Abstract
Background
Research is sparse which examines pathways to suicide, and resilience to suicide, in people who are particularly vulnerable to suicide, for example, prison inmates. The purpose of this study was to examine the ways in which perceptions of self-esteem and coping ability interacted with defeat and entrapment to both amplify suicidal thoughts and feelings, and to act as a buffer against suicidal thoughts and feelings.
Methods
Participants were 65 male prisoners at high risk of suicide. A cross-sectional questionnaire design was used. Questionnaire measures of depression, defeat, entrapment, self-esteem, coping ability and suicidal probability were administered.
Results
For the hopelessness component of the suicide probability measure, high levels of coping ability together with low levels of defeat resulted in the lowest levels of suicidality indicative of a resilience factor. In contrast, low levels of coping skills together with high levels of entrapment were a high risk factor for this hopelessness component of suicide. This pattern of results pertained when controlling for depression levels.
Conclusions
This is the first study to examine interactions between defeat, entrapment and appraisals of self-esteem and coping ability. Therapeutic interventions would benefit from boosting perceptions and appraisals of coping ability, in particular, in people who are at high risk for suicide.
Keywords: Suicide, Prisoners, Defeat, Entrapment, Coping skills, Mental illness
1. Introduction
Suicidal thoughts, behaviours and deaths are a serious health concern [6,14]. The prevalence of suicidal thoughts and behaviours increases dramatically in those with severe mental illnesses. For example, survey results reported that one half of individuals with symptoms of schizophrenia attempt suicide [33]; the risk for suicide deaths in those with bipolar disorder is between 20–30 times greater than that in the general population [38]; and the high prevalence of suicide in those with unipolar depression is well documented [21].
More mental illnesses are experienced by prisoners compared to the general population [15]. Furthermore, prisoners are often vulnerable to suicide in other ways, such as, being homeless, or in financial difficulties, both of which are associated with increased suicidality in general [20,40]. In addition, aspects of the prison environment may intensify suicidality. For example, being incarcerated can lead to fear, a lack of agency, a lack of trust [29], and social isolation [41]. Occupying a single cell has been associated with suicide deaths in prisoners [16]. Consequently, prisoners are at a very high risk of experiencing suicidal thoughts, plans, and behaviours. Indeed suicide deaths have been documented as being from three to eight times higher in prisoners compared to the general population [15,17,36]. Furthermore, this may be an underestimate of the problem of suicidality in prisoners because of limited suicide risk assessment procedures, high vigilance, and restrictions on what prisoners are allowed to bring into their cells [29]. Thus, suicidal ideation may be a more sensitive indicant of suicide risk in prison contexts. Office for National Statistics for England and Wales figures showed that lifetime suicidal ideation for male and female prisoners were 41.5% and 55.5% respectively, whereas lifetime suicide attempts were 23.5% and 40.5% respectively [31]. In a meta-analysis, the odds of death by suicide were found to be 15 times greater in prisoners reporting suicidal ideation [16].
There is increasing evidence that perceptions of being defeated and trapped are strongly linked to suicidality [47]. It is important to determine which psychological factors exacerbate defeat and entrapment. An area of research, which requires expansion, concerns perceptions of coping ability and self-esteem, and the effect of such perceptions on defeat and entrapment. This is important therapeutically because if low levels of self-esteem and coping heighten defeat and entrapment, then this indicates a primary therapeutic target. Conversely, if high levels of self-esteem and coping weaken defeat and entrapment, then this identifies a focus for building suicide resilience [23].
Self-esteem describes feelings of self-worth [34]. There is a robust literature documenting associations between low self-esteem and suicidality in adults [5,8,12,26,37,43,49]. For example, one study reported that in depressed inpatients, those expressing suicidal ideation with a history of suicide attempts had significantly lower self-esteem compared to inpatients who had no such thoughts or histories [37]. Two studies have examined the relationship between self-esteem and suicidality in prisoner populations. The first had a focus on male inmates in the UK which found that self-esteem was significantly lower in prisoners who had made near-lethal suicide attempts (n = 60), compared to those who had not made such attempts (n = 60) [41]. Another study conducted in China reported that depression, low self-esteem, and poor social support were the strongest predictors of suicidal ideation, in that order, but only in female prisoners (n = 201) [49]. Notably, the literature addressing self-esteem in relation to suicidality is sparse for prisoner populations at high risk of suicide. Furthermore, moderation/interaction effects between levels of self-esteem and other key psychological factors, such as, perceptions of defeat and entrapment, in the route to suicidality have received relatively scant attention in the general suicide literature [4,12,26,28,48].
The same issue occurs with coping ability. Coping skills refers to the capacity to offset problems and overcome, or tolerate, stressors [27]. As might be expected, perceptions of having poor coping skills have been linked with suicidal thoughts and behaviours. Work with medical inpatients pointed to an association between high levels of dysfunctional coping skills and high levels of suicidal ideation [30]. Similarly, avoidant coping, i.e., avoiding dealing with stressors, together with the use of substances to cope, was also linked to greater levels of suicidality in homeless young people [25]. Overall, research investigating the relationship between coping skills and suicidality are relatively few. In addition, as with the self-esteem literature, this relationship has been minimally investigated in people who are at high risk of suicide, such as prisoners, nor have moderation/interaction effects between coping ability and defeat and entrapment been sufficiently examined.
Hence, the current study had three aims with a broad focus of understanding suicidal thoughts and behaviours in male prisoners who were most vulnerable to suicide. The first aim was to investigate the impact of low levels of self-esteem and dysfunctional coping abilities on suicidal thoughts and behaviours. The second aim was to examine the extent to which low levels of self-esteem and dysfunctional coping abilities amplified suicidality because they worsen defeat and entrapment. Conversely, the third aim was to determine whether high levels of self-esteem and coping skills buffer perceptions of defeat and entrapment in the pathway to suicidality. Our measure of suicide provided an overall assessment of suicidal thoughts and feelings, but it also allowed an examination of four different components of suicidality. These components reflected suicidal ideation, hopelessness, negative evaluations and hostility. An exploratory goal was to investigate our three aims for each of these components of our suicide measure.
2. Methods
2.1. Design
A cross-sectional questionnaire design was used. The outcome variables were total and sub-scale scores on the Suicide Probability Scale [9]. Predictor variables were defeat and entrapment. Moderator variables were coping and self-esteem. Depression was a control variable.
2.2. Participants
Male volunteers were recruited from a high security prison in England as part of a pilot RCT assessing a cognitive therapy for suicide [39]. Potential participants were identified by prison staff. Participants received no remuneration or privileges for taking part. At the time of recruitment, all participants had to have been identified as being at risk of self-harm or suicide in the past month by prison or prison health care staff according to the Assessment, Care in Custody and Teamwork system of the UK prison service (ACCT). The ACCT system is specific to the prison service in England and Wales. It is the care planning and management system used to identify, monitor, and manage prisoners at risk of suicide or self-harm. No later than 24 hours after the ACCT has been initiated, as part of an ACCT assessment, the at-risk prisoner must be interviewed by a trained ACCT assessor [32].
There were four additional inclusion criteria, namely:
being over 18 years of age;
having sufficient English language ability to understand the participant information sheet and consent form;
having capacity to consent to participation;
and not considered by prison staff to pose a risk to the researcher.
2.3. Measures
The measures were part of a larger battery of tests conducted as part of a pilot randomised control trial assessing cognitive behavioural therapy for suicidality in prisoners [39]. Cronbach’s alpha reliability scores for each measure are presented in Table 1.
Table 1.
Mean scores, standard deviations, sample size (N), Cronbach’s alpha reliability scores, and correlations between key variables.
| M | SD | N | Alpha | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. SPS Total | 86.94 | 20.47 | 63 | .87 | .86** | .86** | .70** | .61** | .72** | .61** | .67** | −.32* | −.70** |
| 2. SPS ideation | 24.48 | 7.89 | 63 | .81 | - | .64** | .51** | .39** | .68** | .59** | .61** | −.33** | −.58** |
| 3. SPS hopelessness | 28.10 | 8.43 | 63 | .76 | - | .54** | .36** | .68** | .64** | .70** | −.16 | −.71** | |
| 4. SPS negative evaluation | 18.43 | 4.43 | 63 | .65 | - | .22 | .51** | .40** | .40** | −.41** | −.49** | ||
| 5. SPS hostility | 15.74 | 5.47 | 61 | .63 | - | .22 | .18 | .20 | −.16 | −.30* | |||
| 6. Depression | 35.11 | 12.33 | 64 | .89 | - | .58** | .70** | −.22 | −.67** | ||||
| 7. Defeat | 54.89 | 14.41 | 63 | .93 | - | .68** | −.01 | −.73** | |||||
| 8. Entrapment | 56.22 | 15.23 | 64 | .92 | - | −.09 | −.69** | ||||||
| 9. Coping skills | 141.41 | 31.49 | 64 | .91 | - | .25 | |||||||
| 10. Self-esteem | 101.52 | 25.71 | 61 | .80 | - |
P ≤ .05;
P ≤ .01. Only the defeat scores were not normally distributed meaning that correlations with this variable were analysed with Spearman’s correlation coefficient. All other correlations used Pearson’s Product Moment correlation coefficient. SPS: Suicide Probability Scale.
2.3.1. Suicidal probability
The Suicide Probability Scale (SPS) [9] is a 36-item questionnaire, which has four sub-scales of hopelessness, suicidal ideation, hostility, and negative self-evaluation. Examples include “When I get mad I throw things”, “I feel so lonely I cannot stand it”. Participants respond to each item using four response-options. This scale provides a total score, and a three-category probability of suicide indicant, based on the profile of sub-scale scores and contextual factors. The total score was used in the current study with a possible range of 30–146.
2.3.2. Depression
The Beck Depression Inventory-second edition (BDI-II) [2] is a 21-item multiple-choice inventory assessing the severity of a range of depressive symptoms (e.g., sadness, pessimism). Items are rated for their severity over the past two weeks using a 4-point scale with a potential range of 0–63.
2.3.3. Self-esteem
The Robson Self Concept Questionnaire (RSCQ) [42] is a 30-item self-report measure, e.g., “I never feel down in the dumps for very long”. A 7-point scale is used giving a possible range of scores from 30–210.
2.3.4. Coping ability
The Coping Inventory for Stressful situations (CISS) [13] is a 48-item measure, e.g., “I can adjust my priorities.” Items are responded to using a 5-point scale ranging from “not at all” to “very much” with a range of 48–240.
2.3.5. Defeat
The defeat scale [19] is a 16-item questionnaire assessing appraisals of defeat including a sense of failed struggle and low social rank (e.g., “I feel that I have not made it in life”). Items are rated on a 5-point scale from ‘Never’ to ‘Always’ for their prevalence during the past week. Scores can range from 0–64.
2.3.6. Entrapment
The entrapment scale [19] is also a 16-item scale assessing feelings of being trapped by internal and external events as well as feelings of a desire to escape (e.g., “I want to get away from myself”). Items are rated on a 5-point scale from ‘Not at all like me’ to ‘Extremely like me’. Scores can range from 0–64.
2.4. Procedure
Participants were asked to read the participant information sheet at least 24 hours prior to signing the consent form. Questionnaires were completed in the order stated above in a private room in the prison, in testing sessions lasting around two hours. This study was approved by a UK NHS ethics committee.
2.5. Analysis strategy
Pearson’s Product Moment or Spearman’s rho correlation coefficients were calculated as appropriate for the data distribution.
Hierarchical multiple regression analysis was used to determine which variables predicted outcome measures as assessed by the suicide probability questionnaire, and its component sub-scales. In the first analysis, the control variable of depressed mood scores was entered into the first step of the regression model, predictor variables of scores on defeat, entrapment, and self-esteem measures were entered into the second step, and moderation effects, which were reflected by interaction/multiplication terms between i defeat and self-esteem, and ii entrapment and self-esteem, were entered into the third step. The second hierarchical regression analysis had the same structure as the first, but coping scores replaced self-esteem. The enter method was used which enters all variables in a step simultaneously [18]. All control and predictor variables were standardised to z scores prior to entry and prior to the calculation of the interaction terms [18]. Outcome variables were checked for distribution normality (skewedness divided by the standard error) [18]. Multi-colinearity was considered problematic if correlations between predictor variables exceeded .8 [18]. The alpha level was set at .05, two-tailed. Data were analysed with IBM SPSS statistics, version 20. Algorithms provided by Dawson et al. were used to plot interaction effects [1,10,11].
3. Results
3.1. Participant characteristics
Participants were 65 male prisoners, aged 22–60 (M = 35.8, SD = 10.95). Most were white (n = 58). Christianity was the most frequent religion (n = 36). The mean number of times that participants had been imprisoned was 3.48 (SD = 6.7). The mean age at which the sample had first been imprisoned was 25.55 (SD = 11.68). The most frequent index offences were sexual crimes (n = 24) and acquisitive offences (n = 22). Psychiatric diagnosis data was drawn from clinical records provided by one consultant psychiatrist at the host prison. Eight participants had no psychiatric diagnoses; 22 had depression; 10 had comorbid depression and anxiety, three were on the schizophrenia disorder spectrum, one had a personality disorder, and the remainder had numerous comorbid symptoms involving severe mental illnesses (e.g., schizophrenia and depression).
3.2. Descriptive data and correlations
The mean scores, standard deviations and correlation coefficients are shown for all key variables in Table 1.
3.3. Regression analyses
The regression analyses tested the predictions that perceptions of low self-esteem and poor coping would be positively associated with suicidality. It was further predicted that low levels of these variables would amplify relationships between defeat and entrapment, and suicidality, and that high levels of these variables would buffer relationships between defeat and entrapment, and suicidality. All outcome variables were normally distributed.
3.4. Self-esteem, defeat, entrapment, and suicidality
The first set of analyses examined whether self-esteem moderated the relationships between defeat and suicidality, and entrapment and suicidality, measured by the suicide probability scale, and the four sub-scales of this measure (Table 2).
Table 2.
Results of the regression models examining predictive effects of self-esteem, defeat, and entrapment on suicide probability and the components of the suicide probability scale for steps which were significant. Coefficients are given only for steps of each model, which were significant.
| Outcome variable | Step | Predictor variables | β | SE β | B | CI (95%) | t |
|---|---|---|---|---|---|---|---|
| SPS - total | 1 F(1, 59) = 64.26, P < .0001, R2 = .52 |
Depression | 15.11 | 1.86 | .72 | 11.34–18.89 | 8.02, P < .0001 |
| 2 F(3, 56) = 5.07, Δ R2 = .10 |
Depression | 7.79 | 2.58 | .37 | 2.63–12.95 | 3.02, P < .01 | |
| Self-esteem | −5.81 | 2.74 | −.28 | −11.30 to −0.33 | −2.12, P < .05 | ||
| Defeat | 2.07 | 2.87 | .10 | −3.63–7.81 | .72 ns | ||
| Entrapment | 2.96 | 2.78 | 0.14 | −2.60–8.53 | 1.07, ns | ||
| SPS hopelessness | 1 F(1, 59) = 57.49, P < .0001, R2 = .49 |
Depression | 6.05 | .80 | .70 | 4.45–7.64 | 7.58, P < .0001 |
| 2 F(3, 56) = 7.05, P < .0001, Δ R2 = .14 |
Depression | 2.56 | 1.05 | .30 | .46–4.66 | 2.45, P < .05 | |
| Self-esteem | −2.66 | 1.11 | −.31 | −4.89 to −0.43 | −2.39, P < .05 | ||
| Defeat | .09 | 1.16 | .01 | −2.24–2.42 | .08 ns | ||
| Entrapment | 2.36 | 1.13 | 0.28 | 0.1–4.62 | 2.09, P < .05 | ||
| SPS ideation | 1 F(1, 59) = 54.34, P < .0001, R2 = .48 |
Depression | 5.59 | .76 | .69 | 4.07–7.10 | 7.37, P < .0001 |
| SPS negative evaluation | 1 F(1, 59) = 20.34, P < .0001, R2 = .26 |
Depression | 2.29 | .51 | .51 | 1.27–3.31 | 4.51, P < .0001 |
SPS: Suicide Probability Scale.
When the suicide probability scale total scores were used as the outcome variable, the first two steps of the model were significant but not the third step containing the interaction/moderator effects (F(1, 54 = 0.34)). Depression and self-esteem were significant predictors. This pattern in the data was repeated to some extent for the hopelessness sub-scale scores where depression, entrapment, and self-esteem were significant predictors, but there were no significant moderation effects at step 3 (F(1, 54 = 0.30)). The suicidal ideation sub-scale outcome resulted in only the first step of the model, containing the depression control variable, being significant (F(3,56 = 2.61) for step 2; F(2,54 = .62) for step 3). Similarly, for the negative self-evaluation sub-scale outcome, only the first step of the model was significant (F(3,56 = 1.09) for step 2). No steps in the regression model were significant for the hostility sub-scale scores (F(1,59 = 2.90) for step 1; F(3,56 = .87) for step 2; F(2,54) = .86 for step 3).
3.5. Coping skills, defeat, entrapment, and suicidality
The second set of analyses followed the first but replaced self-esteem scores with perceived coping skills scores (Table 3).
Table 3.
Results of the regression models examining predictive effects of coping, defeat, and entrapment on suicide probability and the components of the suicide probability scale for steps which were significant. Coefficients are given only for steps of each model, which were significant.
| Outcome variable | Step | Predictor variables | β | SE β | B | CI (95%) | t |
|---|---|---|---|---|---|---|---|
| SPS - total | 1 F(1, 61) = 64.57, P < .0001, R2 = .51 |
Depression | 14.79 | 1.84 | .72 | 11.11–18.48 | 8.04, P < .0001 |
| 2 F(3, 58) = 6.33, Δ R2 = .12 |
Depression | 7.54 | 2.41 | .37 | 2.72–12.36 | 3.13, P < .01 | |
| Coping | −4.50 | 1.68 | −.22 | −7.86 to −1.15 | −2.69, P < .01 | ||
| Defeat | 4.84 | 2.38 | .24 | .08–9.59 | 2.03, P < .05 | ||
| Entrapment | 4.76 | 2.57 | .23 | −.39–9.91 | 1.85, ns | ||
| SPS hopelessness | 1 F(1, 61) = 52.72, P < .0001, R2 = .46 |
Depression | 5.79 | .80 | .68 | 4.19–7.38 | 7.26, P < .0001 |
| 2 F(3, 58) = 5.69, P < .01, Δ R2 = .12 |
Depression | 2.64 | 1.06 | .31 | .53–4.76 | 2.51, P < .05 | |
| Coping | −.53 | .74 | −.06 | −2.00 to −0.95 | −.72, ns | ||
| Defeat | 1.77 | 1.04 | .21 | −.31–3.86 | 1.70, ns | ||
| Entrapment | 2.81 | 1.13 | .33 | 0.55–5.07 | 2.49, P < .05 | ||
| 3 F(2, 56) = 3.16, P = .05, Δ R2 = .04 |
Depression | 1.92 | 1.06 | .23 | −.21–4.05 | 1.81, ns | |
| Coping | −.98 | .80 | −.12 | −2.59–.63 | −1.22, ns | ||
| Defeat | 2.82 | 1.14 | .34 | .53–5.12 | 2.47, P < .05 | ||
| Entrapment | 2.74 | 1.11 | .32 | .51–4.98 | 2.46, P < .05 | ||
| Defeat × coping | 2.62 | 1.19 | .27 | .24–4.99 | 2.21, P < .05 | ||
| Entrapment × coping | −2.05 | .90 | −.24 | −3.86 to −.25 | 2.21, P < .05 | ||
| SPS ideation | 1 F(1, 61) = 52.55, P < .0001, R2 = .46 |
Depression | 5.41 | .75 | .68 | 3.92–6.90 | 7.25, P < .0001 |
| 2 F(3, 58) = 5.51, P < .01, ΔR2 = .12 |
Depression | 2.79 | .99 | .35 | .81–4.78 | 2.82, P < .01 | |
| Coping | −1.86 | .69 | −.24 | −3.24 to −.47 | −2.69, P < .01 | ||
| Defeat | 2.34 | .98 | .30 | .38–4.30 | 2.39, P < .05 | ||
| Entrapment | 1.11 | 1.06 | .14 | −1.02–3.23 | 1.04, ns | ||
| SPS negative evaluation | 1 F(1, 61) = 21.47, P < .0001, R2 = .26 |
Depression | 2.28 | .49 | .51 | 1.3–3.26 | 4.63, P < .0001 |
| 2 F(3, 58) = 3.50, P < .05, ΔR2 = .11 |
Depression | 1.37 | .68 | .31 | 0–2.73 | 2.00, P = .05 | |
| Coping | −1.49 | .48 | −.34 | −2.44 to −.54 | −3.14, P < .05 | ||
| Defeat | .55 | .67 | .12 | −.8–1.9 | .82, ns | ||
| Entrapment | .36 | .73 | .08 | −1.10–1.82 | .49, ns |
SPS: Suicide Probability Scale.
For the total suicide probability scores, the first and second steps of the model were significant, with depression, defeat and poor coping skills being significant predictors. The third step containing the moderation/interaction effects was not significant (F(2,56) = 2.06).
As with the pattern of results for self-esteem, none of the steps in the regression model were significant when the hostility sub-scale scores were entered as the outcome (F(1,59) = 2.90 for step 1; F(3,56) = .63 for step 2; F(2,54) = 51 for step 3). When suicidal ideation sub-scale scores were the outcome, the first two steps of the model were significant. Depression, defeat and coping skills were significant predictors. Step 3 was not significant (F(2,56 = 1.06). For the negative self-evaluation scores, the first two steps of the model were significant. Depression and coping skills, but not defeat or entrapment, were significant predictors. Again, the third step was not significant (F(2,56) = 0.60).
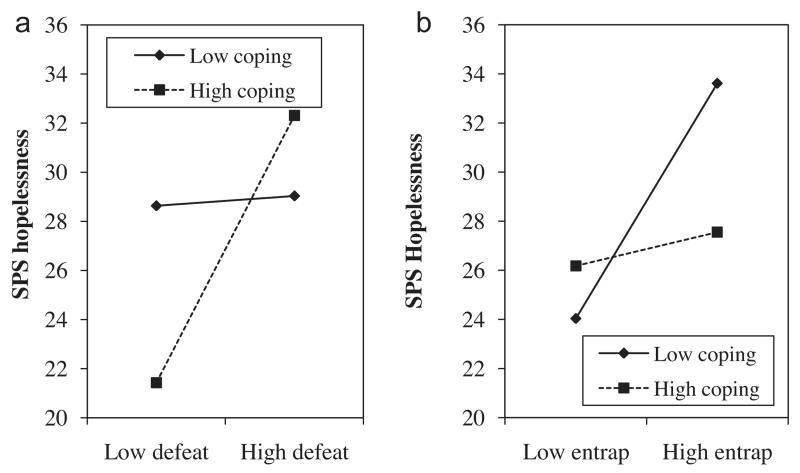
However, for the hopelessness sub-scale scores all three steps of the regression model were significant. There were significant effects for defeat, entrapment, and the interaction/moderation effects between defeat and coping skills, and between entrapment and coping skills. The interaction/moderation effects are depicted in Fig. 1a (defeat) and b (entrapment). Low levels of defeat together with high levels of coping skills appeared to be protective of hopelessness related to suicide probability. Considering perceptions of entrapment, high levels of entrapment coupled with low levels of coping skills seemed to be a risk factor for this hopelessness element of suicide probability.
Fig. 1.
a and b: the moderation effect between defeat and coping skills and the hopelessness sub-scale scores of the suicide probability scale (SPS) is shown in the first figure, a. The moderation effect between entrapment and coping skills and the hopelessness sub-scale scores of the suicide probability scale (SPS) is shown in the second figure, b.
4. Discussion
This is the first study to examine, in a group of individuals who were highly vulnerable to suicidal thoughts and behaviours:
the relationship between self-esteem, coping, and suicidality;
and the extent to which self-esteem and coping moderated defeat and entrapment to both amplify and ameliorate suicidality.
There were four key findings.
First, as expected, low levels of self-esteem were associated with high scores on the suicide probability scale even when controlling for depression. This finding is in accord with previous literature sampling populations across countries, communities, and psychiatric settings [3,8,23,26,37]. Two further studies, found that low levels of self-esteem were associated with suicidality in male [41], and female prisoners [50]. In the current study, the relationship between low self-esteem and suicidality was driven by the hopelessness component of the suicidality measure, but not the hostility, suicidal ideation, or negative evaluation components. No published studies to date have attempted to further examine the components of the suicide probability scale that are affected by low self-esteem in this manner.
Second, contrary to predictions, self-esteem did not moderate defeat and entrapment to either amplify or buffer the effect that these perceptions had on suicidal thoughts and feelings. A review found that results were equivocal concerning the role of high levels of self-esteem as a protective factor, which buffers suicidality [23]. Some studies reporting positive moderation effects have sampled college students [12,26]. It can be questioned whether results from college students can be generalised beyond that population, especially to those who are highly vulnerable to suicidality.
The third finding was that low levels of perceived coping skills predicted the probability of suicidality, again, whilst controlling for depression. Other work has also found relationships between dysfunctional coping skills and suicidality in female prisoners [7,22], psychiatric inpatients [24], patients with physical illnesses [30], and homeless young people [25].
The fourth, and most impactful, finding of the current study concerned interaction/moderation effects of coping skills on the relationship between defeat and entrapment and suicide probability scores. These moderation effects were evident only when the hopelessness component of the suicide probability measure was examined. Perceptions of coping skills affected defeat and entrapment in different ways. High levels of coping ability coupled with low levels of defeat resulted in the lowest levels of suicidality related to hopelessness, which is indicative of a resilience factor [23]. In contrast, high levels of entrapment coupled with low levels of coping skills were a high risk factor for the hopelessness element of the suicide probability scale. An additional important point was that perceived coping skills did not correlate highly with the hopelessness element of the suicidality measure, but it did act as a moderator. This illustrates that it is essential that suicide research expands beyond the examination of main effects to investigate more complex interactive relationships [45].
It is important that the coupling between entrapment and coping was particularly harmful with respect to suicidality, given that the participants were prisoners. It is also important that these effects were observed with the hopelessness component of the suicidality measure because hopelessness, above and beyond depression, has been found to be a high risk factor for suicidal thoughts, behaviours, and death [35,47].
These findings have three clinical implications. First, in terms of assessing suicidality, it is prudent to examine suicidal amplifiers, specifically, a combination of perceptions of entrapment and low coping skills. Second, psychological interventions would benefit from boosting both negative perceptions [45,46] of self-esteem and coping skills, but more importantly the latter, given that negative perceptions of coping skills may amplify entrapment, and positive perceptions of coping skills may counter perceptions of defeat. This last point serves to highlight the clinical importance of considering factors, which confer resilience to suicidality [23]. Third, these patterns of findings pertained even when controlling for depression. This underscores the value of focusing on suicidality in any treatment plan as opposed to focusing on depression alone [44,45].
Four limitations of this study warrant discussion. First, it must be remembered that these findings are based on a sample of prison inmates. Hence, the differential effects of coping skills on defeat and entrapment may have been a function of the prison context. No previous work has examined defeat, entrapment, self-esteem, and coping skills in this interactive manner in a prison context. Consequently, there is no benchmark against which to compare the current findings. However, it should be highlighted that prison contexts overlap with some in-patient psychiatric settings and with those who have reduced mobility. The second limitation is that although we examined sub-components of suicidality our measures did not permit us to investigate different factors contributing to self-esteem. Third, this study was cross-sectional. Thus, causality cannot be inferred. Finally, the sample size was small, meaning that non-significant results may have become significant with a larger sample. However, small samples are not unusual when conducting research with people who are highly vulnerable to suicide and who are difficult to recruit, and for this reason underrepresented in the research literature. Indeed, this kind of data from prison samples is rare.
In conclusion, this study presents a novel contribution to the field of suicide research in four ways. First, the population sample was at high risk of suicidal thoughts and behaviours. Second, the findings indicated that low self-esteem and poor coping ability were associated with suicidality in individuals at high risk of suicide whilst controlling for depression levels. Third, dysfunctional coping skills worsened perceptions of entrapment and, thus, heightened the hopelessness component of the suicide probability measure, but functional coping skills ameliorated perceptions of defeat to lower the hopelessness component of the suicide probability scale. Furthermore, these differential findings were not due to depression. These results are exciting because they illustrate how nurturing positive perceptions of coping abilities have the potential to counter suicidality and improve resilience to suicidality. Moreover, many health professionals are well situated to deliver interventions, which improve coping abilities.
Acknowledgments
We would like to recognize the considerable contribution of our Service User Reference Group (David O’Brien, Natasha Peniston, Angel Delight, and Peer Bhatti) who gave us invaluable advice and support throughout this project. We would also like to thanks Aisha Mirza and Kieran Lord who worked on this project as research assistants and Heather Morrison who aided with recruitment and data collection as a Clinical Support Officer.
Funding
This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-0609-19126). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Footnotes
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Disclosure of interest
The authors declare that they have no competing interest.
References
- [1].Aiken LS, West SG. Multiple regression: testing and interpreting interactions. Sage; London: 1991. [Google Scholar]
- [2]. Beck AT, Steer RA, Brown GK. BDI-II manual. 2nd ed. Harcourt Brace and Company; San Antonio, TX: 1996. [Google Scholar]
- [3].Bhar S, Ghahramanlou-Holloway M, Brown G, Beck AT. Self-esteem and suicide ideation in psychiatric outpatients. Suicide Life Threat Behav. 2008;38(5):511–6. doi: 10.1521/suli.2008.38.5.511. [DOI] [PubMed] [Google Scholar]
- [4].Blankstein KR, Lumley CH, Crawford A. Perfectionism, hopelessness, and suicide ideation: revisions to diathesis-stress and specific vulnerability models. J Rational Emotive Cogn Behav Ther. 2007;25:279–319. [Google Scholar]
- [5].Bryan CJ, Hernandez AM. The functions of social support as protective factors for suicidal ideation in a sample of air force personnel. Suicide Life Threat Behav. 2013;43(5):562–73. doi: 10.1111/sltb.12039. [DOI] [PubMed] [Google Scholar]
- [6].CDC [cited 2014 8-08-2014];Centers for disease control and prevention: morbidity and mortality weekly report 2012. 2012 [Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6101a6.htm?s_cid=mm6101a6_w.
- [7].Chapman AL, Specht MW, Cellucci T. Factors associated with suicide attempts in female inmates: the hegemony of hopelessness. Suicide Life Threat Behav. 2005;35(5):558–69. doi: 10.1521/suli.2005.35.5.558. [DOI] [PubMed] [Google Scholar]
- [8].Chatard A, Selimbegovic L, Konan PND. Self-esteem and suicide rates in 55 nations. Eur J Pers. 2009;23(1):19–32. [Google Scholar]
- [9].Cull J, Gill W. Suicide Probability Scale (SPS) manual. Western Psychological Services; Los Angeles, CA: 1988. [Google Scholar]
- [10].Dawson J. Moderation in management research: what, why, when and how. J Bus Psychol. 2014;29:1–19. [Google Scholar]
- [11].Dawson J, Richter A. Probing three-way interactions in moderated multiple regression: development and application of a slope difference test. J Appl Psychol. 2006;91:917–26. doi: 10.1037/0021-9010.91.4.917. [DOI] [PubMed] [Google Scholar]
- [12].de Man AF, Gutierrez BIB. The relationship between level of self-esteem and suicidal ideation with stability of self-esteem as moderator. Can J Behav Sci. 2002;34(4):235–8. [Google Scholar]
- [13].Endler NS, Parker JDA. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol. 1990;58(5):844–54. doi: 10.1037//0022-3514.58.5.844. [DOI] [PubMed] [Google Scholar]
- [14].EU Death due to suicide by gender. 2012.
- [15].Fazel S, Baillargeon J. The health of prisoners. Lancet. 2011;377(9769):956–65. doi: 10.1016/S0140-6736(10)61053-7. [DOI] [PubMed] [Google Scholar]
- [16].Fazel S, Cartwright J, Norman-Nott A, Hawton K. Suicide in prisoners: a systematic review of risk factors. J Clin Psychiatry. 2008;69(11):1721. [PubMed] [Google Scholar]
- [17].Fazel S, Grann M, Kling B, Hawton K. Prison suicide in 12 countries: an ecological study of 861 suicides during 2003–2007. Soc Psychiatry Psychiatr Epidemiol. 2011;46:191–5. doi: 10.1007/s00127-010-0184-4. [DOI] [PubMed] [Google Scholar]
- [18].Field A. Discovering statistics using SPSS. Sage publications; London: 2005. [Google Scholar]
- [19].Gilbert P, Allan S. The role of defeat and entrapment (arrested flight) in depression: an exploration of an evolutionary view. Psychol Med. 1998;28:585–98. doi: 10.1017/s0033291798006710. [DOI] [PubMed] [Google Scholar]
- [20].Haw C, Hawton K, Casey D. Deliberate self-harm patients of no fixed abode – A study of characteristics and subsequent deaths in patients presenting to a general hospital. Soc Psychiatry Psychiatr Epidemiol. 2006;41(11):918–25. doi: 10.1007/s00127-006-0106-7. [DOI] [PubMed] [Google Scholar]
- [21].Hawton K, Comabella CCI, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147(1–3):17–28. doi: 10.1016/j.jad.2013.01.004. [DOI] [PubMed] [Google Scholar]
- [22].Ireland JL, York C. Exploring application of the Interpersonal-Psychological Theory of Suicidal Behaviour to self-injurious behaviour among women prisoners: proposing a new model of understanding. Int J Law Psychiatry. 2012;35(1):70–6. doi: 10.1016/j.ijlp.2011.11.006. [DOI] [PubMed] [Google Scholar]
- [23].Johnson J, Wood AM, Gooding P, Taylor PJ, Tarrier N. Resilience to suicidality: the buffering hypothesis. Clin Psychol Rev. 2011;31(4):563–91. doi: 10.1016/j.cpr.2010.12.007. [DOI] [PubMed] [Google Scholar]
- [24].Josepho SA, Plutchik R. Stress, coping, and suicide risk in psychiatric-inpatients. Suicide Life Threat Behav. 1994;24(1):48–57. [PubMed] [Google Scholar]
- [25].Kidd SA, Carroll MR. Coping and suicidality among homeless youth. J Adolesc. 2007;30(2):283–96. doi: 10.1016/j.adolescence.2006.03.002. [DOI] [PubMed] [Google Scholar]
- [26].Kleiman EM, Riskind JH. Utilized social support and self-esteem mediate the relationship between perceived social support and suicide ideation. A test of a multiple mediator model crisis. Crisis. 2013;34(1):42–9. doi: 10.1027/0227-5910/a000159. [DOI] [PubMed] [Google Scholar]
- [27].Lazarus RS. Psychological stress and the coping process. McGraw-Hill; New York: 1966. [Google Scholar]
- [28].Lieberman Z, Solomon Z, Ginzburg K. Suicidal ideation among young adults: effects of perceived social support, self-esteem, and adjustment. J Loss Trauma. 2005;10:163–81. [Google Scholar]
- [29].Liebling A, Maruna S. The effects of imprisonment. Willan; Oregon: 2005. [Google Scholar]
- [30].Marusic A, Goodwin RD. Suicidal and deliberate self-harm ideation among patients with physical illness: the role of coping styles. Suicide Life Threat Behav. 2006;36(3):323–8. doi: 10.1521/suli.2006.36.3.323. [DOI] [PubMed] [Google Scholar]
- [31].Meltzer H, Jenkins R, Singleton N, Charlton J, Yar M. Non-fatal suicidal behaviour among prisoners. Statistics OfN; UK: London: 1999. [DOI] [PubMed] [Google Scholar]
- [32].MOJ [cited 2015 20 August];Management of prisoners at risk of harm to self, to others and from others (Safer Custody) 2012 [Available from: http://www.justice.gov.uk/downloads/./psi./psi-64-2011-safer-custody.doc.
- [33].Morgan VA, Waterreus A, Jablensky A, Mackinnon A, McGrath JJ, Carr V, et al. People living with psychotic illness in 2010: the second Australian national survey of psychosis. Aust N Z J Psychiatry. 2012;46(8):735–52. doi: 10.1177/0004867412449877. [DOI] [PubMed] [Google Scholar]
- [34].Mruk C. Self-esteem: research, theory, and practice: towards a positive psychology of self-esteem. Springer Publishing; New York: 1995. [Google Scholar]
- [35].O’Connor RC, Cassidy C. Predicting hopelessness: the interaction between optimism/pessimism and specific future expectancies. Cogn Emotion. 2007;21(3):596–613. [Google Scholar]
- [36].Opitz-Welke A, Bennefeld-Kersten K, Konrad N, Welke J. Prison suicides in Germany from 2000 to 2011. Int J Law Psychiatry. 2013;36(5–6):386–9. doi: 10.1016/j.ijlp.2013.06.018. [DOI] [PubMed] [Google Scholar]
- [37].Palmer CJ. Suicide attempt history, self-esteem, and suicide risk in a sample of 116 depressed voluntary inpatients. Psychol Rep. 2004;95(3):1092–4. doi: 10.2466/pr0.95.3f.1092-1094. [DOI] [PubMed] [Google Scholar]
- [38].Pompili M, Gonda X, Serafini G, Innamorati M, Sher L, Amore M, et al. Epidemiology of suicide in bipolar disorders: a systematic review of the literature. Bipolar Disord. 2013;15(5):457–90. doi: 10.1111/bdi.12087. [DOI] [PubMed] [Google Scholar]
- [39].Pratt D, Tarrier N, Dunn G, Awenat Y, Shaw J, Ulph F, et al. Cognitive behavioural suicide prevention for male prisoners: an exploratory randomised controlled trial. Psychol Med. 2015 doi: 10.1017/S0033291715001348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Richardson T, Elliott P, Roberts R. The relationship between personal unsecured debt and mental and physical health: a systematic review and meta-analysis. Clin Psychol Rev. 2013;33(8):1148–62. doi: 10.1016/j.cpr.2013.08.009. [DOI] [PubMed] [Google Scholar]
- [41].Rivlin A, Hawton K, Marzano L, Fazel S. Psychosocial characteristics and social networks of suicidal prisoners: towards a model of suicidal behaviour in detention. Plos One. 2013;8(7) doi: 10.1371/journal.pone.0068944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Robson P. Development of a new self-report questionnaire to measure self-esteem. Psychol Med. 1989;19(2):513–8. doi: 10.1017/s003329170001254x. [DOI] [PubMed] [Google Scholar]
- [43].Sharaf AY, Thompson EA, Walsh E. Protective effects of self-esteem and family support on suicide risk behaviors among at-risk adolescents. J Child Adolesc Psychiatr Nurs. 2009;22(3):160–8. doi: 10.1111/j.1744-6171.2009.00194.x. [DOI] [PubMed] [Google Scholar]
- [44].Tarrier N, Taylor K, Gooding P. Cognitive-behavioral interventions to reduce suicide behavior. A systematic review and meta-analysis. Behav Modif. 2008;32(1):77–108. doi: 10.1177/0145445507304728. [DOI] [PubMed] [Google Scholar]
- [45].Tarrier N, Gooding P, Pratt D, Kelly J, Awenat Y, Maxwell J. Cognitive behavioural prevention of suicide in psychosis: a treatment manual. Routledge; London, UK: 2013. [Google Scholar]
- [46].Tarrier N, Kelly J, Maqsood S, Snelson N, Maxwell J, Law H, et al. The cognitive behavioural prevention of suicide in psychosis: a clinical trial. Schizophr Res. 2014;156(2–3):204–10. doi: 10.1016/j.schres.2014.04.029. [DOI] [PubMed] [Google Scholar]
- [47].Taylor PJ, Gooding P, Wood AM, Tarrier N. The role of defeat and entrapment in depression, anxiety, and suicide. Psychol Bull. 2011;137(3):391–420. doi: 10.1037/a0022935. [DOI] [PubMed] [Google Scholar]
- [48].Wilke DJ. Predicting suicide ideation for substance users: the role of self-esteem, abstinence, and attendance at 12-step meetings. Addict Res Theory. 2004;12:231–40. [Google Scholar]
- [49].Zhang J, Grabiner VE, Zhou Y, Li N. Suicidal ideation and its correlates in prisoners. A comparative study in China. Crisis. 2010;31(6):335–42. doi: 10.1027/0227-5910/a000055. [DOI] [PubMed] [Google Scholar]
- [50].Zhang J, Liang B, Zhou Y, Brame W. Prison inmates’ suicidal ideation in China: a study of gender differences and their impact. Int J Offender Ther Comp Criminol. 2010;54(6):959–83. doi: 10.1177/0306624X09348200. [DOI] [PubMed] [Google Scholar]