Abstract
Background
Prisoners have an exceptional risk of suicide. Cognitive behavioural therapy for suicidal behaviour has been shown to offer considerable potential, but has yet to be formally evaluated within prisons. This study investigated the feasibility of delivering and evaluating a novel, manualised cognitive behavioural suicide prevention (CBSP) therapy for suicidal male prisoners.
Methods
A pilot randomised controlled trial of CBSP in addition to treatment as usual (CBSP; n=31) compared to treatment as usual alone (TAU; n=31), was conducted in a male prison in England. The primary outcome was self-injurious behaviour occurring within the past six months. Secondary outcomes were dimensions of suicidal ideation, psychiatric symptomatology, personality dysfunction and psychological determinants of suicide, including depression and hopelessness. The trial was prospectively registered (number ISRCTN59909209).
Results
Relative to TAU, participants receiving CBSP therapy achieved a significantly greater reduction in suicidal behaviours with a moderate treatment effect (Cohen’s d=−0.72, 95%CI: −1.71 to 0.09; baseline mean [SD], TAU: 1.39[3.28] vs CBSP: 1.06[2.10], 6 months mean [SD], TAU: 1.48[3.23] vs CBSP: 0.58[1.52]). Significant improvements were achieved on measures of psychiatric symptomatology and personality dysfunction. Improvements on psychological determinants of suicide were non-significant. More than half of participants in the CBSP group achieved a clinically significant recovery by the end of therapy, compared to a quarter of the TAU group.
Conclusions
The delivery and evaluation of cognitive behavioural suicide prevention therapy within a prison is feasible. CBSP therapy offers significant promise in the prevention of prison suicide and an adequately powered randomised controlled trial is warranted.
Keywords: Cognitive Therapy, Suicide Prevention, Prison, Randomised Controlled Trial
INTRODUCTION
The risk of suicide is particularly high amongst prisoners. Male prisoners are five times more likely to die by suicide than the general population (Fazel et al., 2005). Coping with an environment that engenders fear, distrust, and a lack of control, can leave individuals feeling overwhelmed and hopeless, leading some of them to choose suicide as a way to escape (Birmingham, 2003, Liebling and Maruna, 2013). Suicide in prison is of considerable public and social concern (e.g. (Bowcott et al., 2014) and prisoners continue to be prioritised within national suicide prevention strategies (Department of Health, 2002, 2012).
A meta-analysis of cognitive behaviour therapies (CBT) for suicidal behaviour reported such interventions were effective, when designed, tailored, and implemented to focus on suicidality (Tarrier et al., 2008) and CBT is now a recommended treatment for suicidal behaviour (NICE, 2011). However, the potential offered by CBT for suicidal patients located within prison settings is unknown. Structured and systematic approaches to offender behaviour programmes have already been established as effective in reducing other types of prisoner behaviour (Gendreau, 1996, Landenberger and Lipsey, 2005, McGuire, 2002), therefore, it is important to investigate the possible benefits of a CBT-informed structured intervention programme specifically targeting suicidal ideation and behaviour.
International and national policies emphasise imprisonment as an important opportunity to enhance access to interventions aiming to reduce the risk of suicidal behaviour (Department of Health, 2007, Konrad et al., 2007). However, whilst prison settings may present an opportunity to engage with a ‘hard to reach’ sector of society, a number of potential barriers at the contextual level and issues presented by the individual prisoners themselves have to be identified and overcome to allow the acceptable and feasible delivery of any preventative interventions.
The main aim of the Prevention Of Suicide in Prisons (PROSPeR) study, therefore, was to examine the feasibility of delivering and evaluating Cognitive Behavioural Suicide Prevention (CBSP) therapy for individuals identified as presenting a risk to themselves whilst in prison. CBSP was selected as the psychosocial intervention for this study as it is a suicide prevention intervention that has been intentionally derived from an empirically validated theoretical model of suicide (Johnson et al., 2008, Tarrier et al., 2013), and has recently been shown to reduce measures of suicidality in community dwelling participants with a schizophrenia diagnosis (Tarrier et al., 2014).
A further aim of the PROSPeR study was to develop preliminary estimates of the impact of CBSP therapy over the usual care and support offered to suicidal prisoners. We examined three specific hypotheses. First, those who received the CBSP therapy programme would demonstrate significantly greater reductions in the occurrence of suicidal behaviours compared to those receiving usual care and support. Second, the CBSP group would achieve significantly improved scores on psychological measures of suicidality, including suicidal ideation and hopelessness, compared to the usual care group. Third, significant improvements would be experienced by the CBSP group, relative to the usual care group, on measures correlated with suicidal ideation, such as depression, anxiety, self-esteem and psychiatric symptomatology.
METHOD
Study design and participants
In keeping with the guidance for the evaluation of complex interventions (Medical Research Council, 2008), the PROSPeR study was a single-blind (rater) randomised controlled pilot trial. Recruitment into the trial was conducted between 4th January, 2012 and 14th June 2013 at one UK site in the Northwest of England with follow-up assessments taking place between 2nd July 2012 and 14th December 2013. The study sample was recruited from a closed prison establishment with capacity to house approximately 1200 male prisoners. The PROSPeR study was registered as an International Standard Randomised Controlled Trial, ISRCTN59909209, and received approval from the National Research Ethics Committee for Wales (reference 11/WA/0002), the National Offender Management Service’s National Research Committee (reference 16-11) and the Governor of the host prison.
Inclusion criteria were male prisoners aged over 18 years; who had been identified within HM Prison Service’s Assessment, Care in Custody and Teamwork (ACCT) (Ministry of Justice, 2013) system as being at risk of suicidal behaviour within the past month. Eligible prisoners were excluded from the study if they had insufficient knowledge of English to enable adequate participation in the assessment process; were deemed by prison staff to be too dangerous; or unable to provide consent. Current or previous participation in offending behaviour programmes was not an exclusion criterion, as this was considered to be usual treatment for prisoners.
All potential participants were identified by the Safer Custody team within the host prison who held the responsibility for administrating the ACCT system. Individuals identified under the ACCT system were provided with information about the PROSPeR study. After agreement to be contacted, prisoners expressing an interest in the study were then invited to an initial research interview to confirm eligibility. This process of identifying potential participants was conducted independently of the research team. Those participants meeting entry criteria were asked to provide written informed consent to take part in the study and to agree to be subject to a ‘holding order’ to remain within the host prison for the duration of their participation in the trial. Subsequent assessments were completed with a research assistant, independently of trial therapists, at 4 months (post-treatment) and 6 months (follow-up) after the baseline assessment.
Interventions
Treatment as Usual (TAU)
Participants randomised to the TAU group received the usual care and support available to any prisoner identified under the ACCT system had they not participated in the trial. The Prison Service Instruction describing the management of prisoners at risk of harm to self (Ministry of Justice, 2013) clearly prescribed that all prisoners identified under the ACCT system received an assessment of risk when a risk to self was first identified, which then informed a risk management plan of how to keep the individual safe (e.g. levels of monitoring and observation). Subsequently, at least fortnightly, review meetings were arranged by prison officer staff until the risk was considered to be lowered, at which time the individual was discharged from the ACCT system.
Within the risk management plan, a referral could be made to the prison’s Mental Health In-Reach team that offered psychosocial assessment, ongoing monitoring of psychiatric symptoms, medication therapies and nursing support. All participants within the current trial were referred to the In-Reach Team for a psychosocial assessment. At the time of the study, TAU did not include access to a psychological therapy. We did not register use of psychiatric medications, but previous studies have reported that at least a third of suicidal prisoners are routinely prescribed antidepressant medication (Humber et al., 2010, Rivlin et al., 2010).
Cognitive Behavioural Suicide Prevention (CBSP) therapy
In addition to TAU, participants randomly allocated to the CBSP group also received a cognitive therapy informed intervention. The CBSP therapy is a structured, time-limited psychosocial intervention developed to treat individuals experiencing suicidal ideation and / or behaviour (Tarrier et al., 2013). CBSP is informed by the Schematic Appraisals Model of Suicide (Johnson et al., 2008), which identifies (i) information processing biases, (ii) appraisals, and (iii) a suicide schema to be the main components contributing to an individual's experience of suicidality. CBSP draws from established clinical techniques to restructure the three aspects of the SAMS model, including the use of cognitive techniques to encourage participants to evaluate some of their appraisals about themselves, their situation and their future, as well as the use of behavioural techniques to identify and rehearse more helpful responses to distressing situations. The intervention for the current study was manualised and developed from our previously published treatment manual (Tarrier et al., 2013). Briefly, the intervention was modularised into five components:
Attention Broadening
Cognitive Restructuring
Mood Management & Behavioural Activation
Problem-Solving Training
Improving Self-Esteem & Positive Schema.
Delivery of the CBSP therapy programme consisted of up to 20 sessions, delivered twice weekly during the initial phases of therapy, reducing to once weekly sessions when therapeutic engagement had been established. Each session typically lasted for up to 1 hour. Treatment sessions were provided by two trial therapists, of whom both were Clinical Psychologists (doctoral level) with 2 – 5 years’ experience of CBT. Both therapists received initial training to familiarise them to the specifics of the CBSP programme. Ongoing case supervision was provided throughout the trial on a weekly basis, by an experienced Clinical Psychologist who was independent of the research team.
Measures
Adherence measures
To assess participants’ adherence to the CBSP intervention, the trial therapists were asked to rate the participant’s active involvement in the therapy programme on a bespoke rating form based upon existing assessment tools from the offending behaviour programmes (Hollin and Palmer, 2006). For each participant, therapist(s) assessed attendance, promptness, level of participation, mastery of programme content, disruptive behaviour, completion of homework tasks, and an overall evaluation of therapy success. Each of these items was rated on a Likert scale (1=poor to 5=excellent). Additionally, participant attendance was recorded to provide an indicator of engagement in the treatment. Similarly, reasons for non-attendance were monitored. Finally, the therapist(s) maintained a record for each participant of the content of each session, with specific reference to the modules within the treatment protocol.
Outcome measures
Completed suicide occurs too infrequently to be a useful outcome measure; however, suicidal behaviours, thoughts and feelings are common, distressing and, therefore, legitimate outcome measures. This is standard practice as used in previous trials (Tarrier et al., 2014, Tarrier et al., 2008). In accordance with the trial protocol, the primary outcome measure was the number of episodes of suicidal or self-injurious behaviour (SIB) in the past six months assessed by examination of participants’ prison records. Secondary outcome measures included scores on the Beck Scale for Suicidal Ideation (BSSI; (Beck and Steer, 1991) to assess suicidal ideation, and the Suicide Probability Scale (SPS; (Cull and Gill, 1982) to provide an overall estimate of suicidal potential. Both measures have established reliability and predictive validity within prisoner populations (Naud & Daigle, 2010; Perry, Marandos, Coulton and Johnson, 2010; Senior et al., 2007).
Further measures were completed to assess key psychological and psychiatric variables relevant to suicide. Perceptions of pessimism and hopelessness were measured using the Beck Hopelessness Scale (BHS; (Beck and Steer, 1988), levels of depression and anxiety were assessed using the Beck Depression Inventory (BDI-II; (Beck et al., 1996) and the Beck Anxiety Inventory (BAI; (Beck et al., 1988), respectively, and self-esteem was measured using the Robson Self-Concept Questionnaire (RSCQ; (Robson, 1989). The 24-item version of the Brief Psychiatric Rating Scale (BPRS; (Ventura et al., 1993) was administered to assess the presence and severity of psychiatric symptoms, and the Standardised Assessment of Personality – Abbreviated Scale (SAP-AS; (Moran et al., 2003) was used to briefly measure the level of personality dysfunction / disorder. Other assessments were also administered to investigate potential predictors of outcome within further secondary analyses, which are not reported within this paper. Additionally, a range of demographic, clinical and criminological details were collected from participant interviews, clinical and prison records, and the host prison's management information system, subject to participant consent.
Clinically significant recovery
Clinically significant change was calculated on the secondary outcome measures of suicidal ideation and suicide probability. Using standardised procedures (Jacobson et al., 1999), clinical significance was indicated by an improvement in scores from the clinical to the non-clinical range for the measures.
Random assignment and masking
Immediately following completion of baseline assessments, participants were randomly allocated to one of the two treatment groups: TAU or CBSP. Randomisation of participants to the two treatment groups was achieved by referring to a sequence of sealed envelopes provided by the Research Statistician (GD). Treatment allocated was based on pseudo-random number generation, and based on randomly-permuted blocks algorithm (with block sizes randomly varying between 4 and 8).
The randomisation schedules were generated and provided to the study by the Research Statistician, before being kept securely and confidentially by the Trial Administrator who contacted the trial therapists, as appropriate, with the participant's details for those allocated to the CBSP group. Thus, randomisation was independent and the research assistants completing the assessments were blind to group allocation. A number of strategies were developed to achieve and maintain the masking of assessors, such as removing any research assistant involvement in the random assignment process, research assistant and trial therapist to avoid simultaneous use of allocated interview/therapy rooms to preserve blindness to allocation, and participants were encouraged at each assessment not to refer to treatment group allocation.
Statistical Analysis
A sample size of 30 per group gave the trial 80% power to detect an effect size of 0.60 using an independent groups t-test with a two-sided significance level of 0.15. Since this was a preliminary trial, we were prepared to accept a higher type 1 error rate in order to avoid missing promising effects (Stone et al., 2007).
All analyses were conducted using Stata version 11 (StataCorp, 2009). Estimation of treatment effects was based on the intention-to-treat (ITT) principle. Random effects (i.e. random intercepts) models for repeated measures data were fitted to both 4- and 6-month outcome variables, with the baseline value of the outcome variable being used as a covariate. Stata’s xtreg command was used. After preliminary examination of the summary statistics for the outcome variables, treatment effects (differences in outcomes between the two arms of the trial) were assumed to be the same for both follow-up times. Fitting the appropriate random- or mixed-effects model provides an estimate of this common treatment effect. Missing outcome data were assumed to be Missing at Random or MAR, using the terminology of Little and Rubin (Little and Rubin, 2002), i.e. conditional on the data used in the model, whether an observation is missing or not does not depend on its actual value.
Since the primary outcome (SIB) was positively skewed, confidence intervals for the standard errors, and confidence for the treatment effects were estimated by applying a bootstrap procedure (Efron and Tibshirani, 1994) using the percentiles based on the results of 1000 replications (using the trial participant as the sampling unit).
RESULTS
Recruitment and Retention
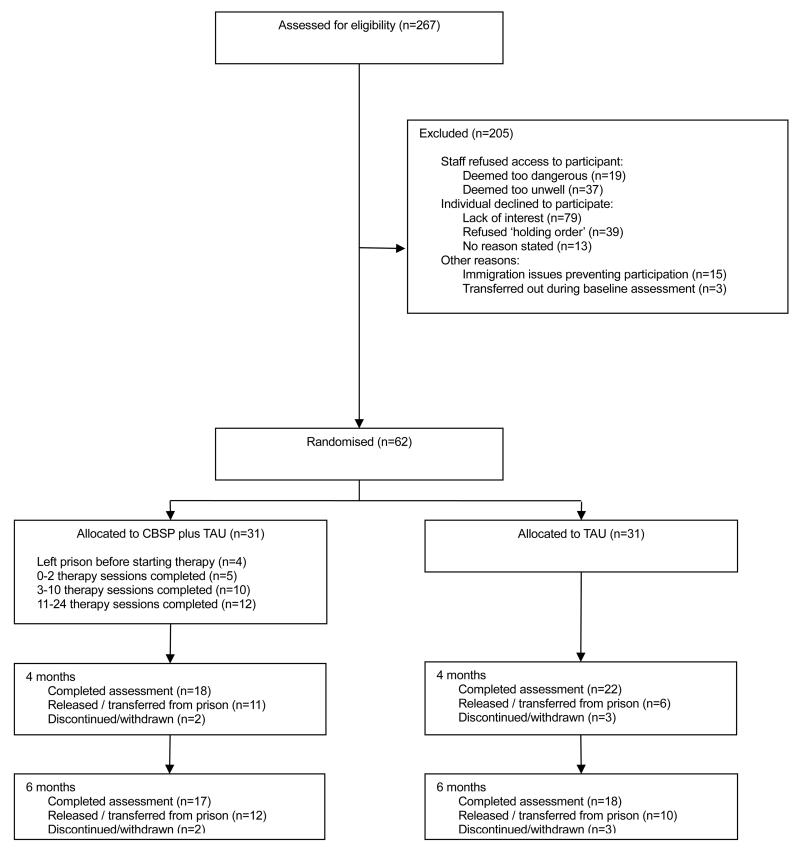
During the two year period of recruitment, 267 prisoners were assessed for suitability for the PROSPeR trial (see Figure 1). Of the 205 who were excluded from the trial, 56 (27%) failed to meet entry criteria (i.e. deemed by prison staff as too dangerous or too unwell to participate), and 131 (64%) declined to participate with 79 (39%) expressing a lack of interest in the trial and 39 (19%) refusing to be placed on a ‘holding order’ to remain in the host prison for 6 months. Fifteen (7%) prisoners were prevented from participating due to legal reasons pertaining to immigration orders, and 3 (1%) were unexpectedly transferred out of the prison whilst undertaking the baseline assessment. Recruitment into the study was successful, with a final sample size slightly larger than the original recruitment target, with 62 participants randomised to the CBSP plus TAU group (n=31) or the TAU alone group (n=31). The follow up rates for the study sample as a whole was 40 out of 62 (65%) at 4 months and 35 (56%) at the 6 months assessments. Five (8%) participants withdrew from the study and we were unable to follow-up 22 (35%) participants who had been unexpectedly released early or transferred to other prisons for security reasons during the course of the trial. Participants that were lost to follow up did not differ significantly from participants that completed the 4 months or 6 months assessment on any of the socio-demographic or custodial characteristics.
Figure 1. CONSORT flow diagram of participant progress through the PROSPeR trial.
Demographic and Clinical characteristics
Baseline characteristics for each group are presented in Table 1. For the overall sample, participant ages ranged from 21 to 60 years with a mean of 35.2 (SD=11.10). Fifty three (85%) participants described themselves as White (UK), 4 (6%) as Black (UK), 3 (5%) as White (non-UK), 3 (5%) as other / not stated. Thirty five (57%) participants were single. According to participants’ self-reports, the mean age of their first custodial sentence was 25.7 years (SD=11.91) with an average of 5.4 (SD=8.95) previous imprisonments. Thirty four (55%) participants were currently serving a prison sentence, 25 (40%) had been remanded into prison custody and the custodial status of 3 (5%) participants was not known.
Table 1. Sociodemographic and Custodial characteristics. Data shown are mean(SD) or n(%).
| CBSP plus TAU (n=31) | TAU alone (n=31) | |
|---|---|---|
|
| ||
| SOCIODEMOGRAPHIC VARIABLES: | ||
|
| ||
| Age (years) | 38.5 (11.3) | 32.0 (10.1) |
|
| ||
| Ethnicity: White, British | 26 (84%) | 27 (87%) |
|
| ||
| Marital status: Single | 19 (61%) | 16 (52%) |
|
| ||
| CUSTODIAL VARIABLES: | ||
|
| ||
| Age first imprisoned (years) | 25.5 (12.7) | 25.9 (11.3) |
|
| ||
| Number of previous imprisonments | 7.5 (11.3) | 3.4 (5.1) |
|
| ||
| Custodial status: | ||
| Sentence | 20 (65%) | 14 (45%) |
| Remand | 9 (29%) | 16 (52%) |
| Other / Not known | 2 (6%) | 1 (3%) |
CBSP=cognitive behavioural suicide prevention, TAU=treatment as usual.
To meet entry criteria to the study, all participants had been managed under the ACCT process during the month prior to entry to the study. Forty four (71%) were under ACCT at the start of their participation in the study, 11 (18%) had been under ACCT less than 2 weeks prior to starting the study, and the remaining 7 (11%) up to a month prior. There was a substantial proportion of previous suicide attempts within the sample, with only nine (15%) participants self-reporting no lifetime history of a suicide attempt, whereas 18 (29%) participants had made a single previous attempt and 35 (57%) had previously attempted suicide on two or more occasions.
On both measures of suicidality, the mean [SD] scores (BSSI=13.8 [10.9], SPS=87.1 [21.2]) indicated a severe level of suicidal ideation and risk amongst the overall sample of participants (Beck and Steer, 1991, Cull and Gill, 1982). Similarly, the mean scores for depression (BDI=34.7 [12.5]) and hopelessness (BHS=11.1 [6.4]) were in the severe ranges (Beck and Steer, 1988, Beck et al., 1996).
Intervention Feasibility
Engagement and Retention in the trial
In total, 276 CBSP therapy sessions were voluntarily attended by participants, with an average of 8.9 (SD=7.42, range 0-20) sessions per participant. Only 16 sessions were refused (participant mean=0.52, SD=0.81) and 46 sessions had to be rearranged due to contextual circumstances beyond the control of the therapist or participant (participant mean =1.48, SD=0.159), such as legal visits, family visits, and security incidents on wings (‘lockdowns’). Twelve (39%) participants received 12 or more sessions, and 10 (32%) participants completed 5 or fewer sessions. Four (13%) participants were allocated to receive the CBSP programme but were unexpectedly released from the prison immediately after randomisation and prior to the first treatment session (see Figure 1).
Adherence to Treatment Protocol
Table 2 shows the list of treatment modules and the frequency of use of each module across the CBSP participants, as judged by the therapist. To foster engagement with the participant, the prioritisation of modules was collaboratively agreed between the participant and therapist. The module most frequently delivered module was Cognitive Restructuring, with almost half (42%) of participants expressing an interest in engaging in this work, with an average of five sessions focussed on directly challenging unhelpful or inaccurate appraisals. The attention broadening technique was used by a quarter (26%) of participants, with those engaging in this work completing an average of six sessions. Problem solving training was delivered to a quarter (23%) of participants and less than a fifth of participants received techniques to improve self-esteem (16%) or mood management (10%).
Table 2. CBSP Individual treatment modules: Number and percentage of participants receiving the module.
| CBSP module | No. of sessions in which module was used (mean, SD) | N (%) of participants receiving module |
|---|---|---|
| Attention Broadening | 6.1 (2.6) | 8 (26%) |
| Cognitive Restructuring | 4.9 (2.3) | 13 (42%) |
| Mood Management | 4.0 (2.7) | 3 (10%) |
| Problem Solving Training | 3.0 (1.2) | 7 (23%) |
| Improving Self-Esteem | 4.4 (2.2) | 5 (16%) |
CBSP = Cognitive Behavioural Suicide Prevention
Therapists’ Ratings of Participant Adherence
Promptness (4.3), attendance (3.6) and level of participation (3.1) in therapy sessions were all rated above the mid-point of the 1 to 5 rating scale, whilst lower ratings were recorded for mastery of programme (2.8) and the completion of homework (2.8). Ratings for disruptive behaviour were very low (1.3). Trial therapist ratings were not recorded for the 4 participants who did not attend a single therapy session.
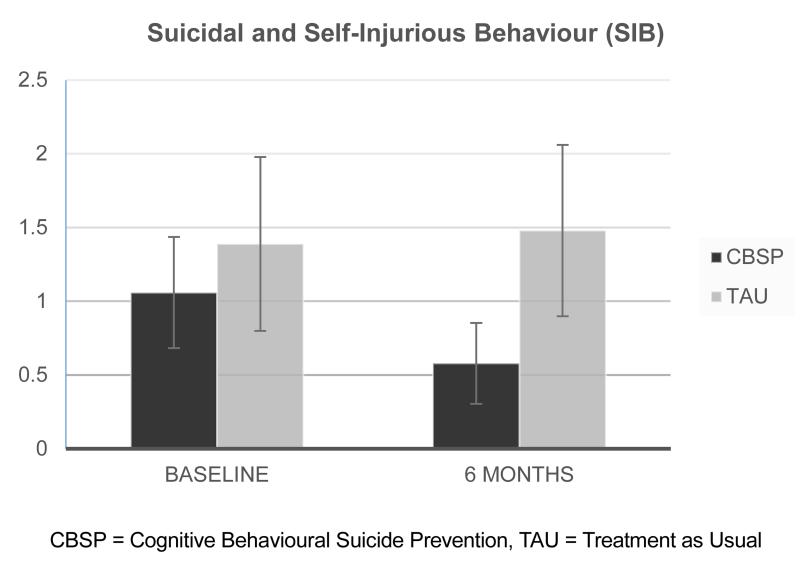
Suicidal and self-injurious behaviours (SIB)
As shown in Figure 2, the mean number of SIBs for the CBSP group (1.06) was initially lower than for the TAU group (1.39). However, at the 6 months assessment the mean number of SIBs for the CBSP group had decreased by almost 50% to 0.58, whereas this figure had changed little (1.48) for the TAU group. As such, the CBSP group engaged in fewer self-injurious behaviours compared to the usual treatment group (treatment effect=−0.72, se=0.47, 95%CI: −1.71 to 0.09, p=0.162). The number of participants who had recently engaged in suicidal or self-injurious behaviours at baseline (CBSP: 12 (39%), TAU: 13 (42%)) reduced for both groups by the follow-up assessment (CBSP: 7 (23%), TAU:7 (23%)). At the six month assessments, no participants within the CBSP group were found to have increased numbers of SIBs relative to baseline, whereas within the TAU group 6 participants had increased numbers of SIBs. All SIB episodes were determined to be adverse events that were not related to the study.
Figure 2. Mean number of Self-Injurious Behaviours.
Self-report measures
The outcomes for each arm of the trial are compared in Table 3. Across measures of suicidal ideation, suicide probability, hopelessness, depression, anxiety, and self-esteem there was a consistent pattern that participants in both the CBSP and TAU groups made improvements between baseline and the follow-up assessments, with greater improvements occurring for the CBSP group although there were no statistically significant effects of treatment. The repeated measures regression modelling did indicate significant improvements in measures of psychiatric symptomatology (BPRS-R; treatment effect=−4.60, se=2.25, 95%CI: −9.02 to −0.19, p=0.04) and personality dysfunction (SAP-AS; treatment effect=−0.79, se=0.39, 95%CI: −1.55 to −0.04, p=0.04).
Table 3. Primary and secondary outcome measures at 4 and 6 months. Data shown are mean (SD).
| Baseline | 4 months | 6 months | ||||
|---|---|---|---|---|---|---|
| CBSP (n=31) | TAU (n=31) | CBSP (n=18) | TAU (n=22) | CBSP (n=17) | TAU (n=18) | |
| Number of SIB episodes in previous 6 months | 1.06 (2.10) | 1.39 (3.28) | N/A | N/A | 0.58 (1.52)a | 1.48 (3.23)a |
| BSSI | 13.2 (10.8) | 14.5 (11.2) | 5.8 (9.9) | 6.7 (10.5) | 6.6 (10.4) | 7.7 (11.4) |
| SPS | 86.9 (19.9) | 87.3 (20.8) | 67.9 (24.3) | 82.6 (23.2) | 67.4 (21.8) | 76.4 (23.8) |
| BHS | 11.4 (6.1) | 10.8 (6.8)b | 6.8 (5.8) | 8.6 (6.6) | 7.9 (7.1) | 7.3 (7.1)c |
| BDI | 34.2 (11.7) | 35.3 (13.4)b | 17.1 (13.0) | 26.6 (15.3) | 20.2 (19.2) | 23.4 (16.6) |
| BAI | 21.7 (13.0) | 21.5 (12.3)b | 12.7 (13.1) | 14.1 (11.1) | 9.5 (11.1) | 12.1 (13.7) |
| RSCQ | 102.8 (21.9) | 100.6 (29.2)b | 117.6 (29.3) | 106.3 (21.7)d | 122.9 (25.5) | 113.7 (31.6) |
| SAPAS | 4.8 (1.7) | 4.2 (1.7)b | 3.8 (1.7) | 4.7 (1.7) | 3.7 (1.8) | 4.3 (1.7) |
| BPRS | 44.6 (11.6) | 46.0 (11.0)b | 35.1 (9.2) | 39.7 (9.6) | 34.9 (6.8) | 41.1 (11.5) |
CBSP=cognitive behavioural suicide prevention, TAU=treatment as usual, SIB=Self-Injurious Behaviours, BSSI=Beck scale for suicidal ideation, SPS=Suicide probability scale, BHS=Beck hopelessness scale, BDI=Beck depression inventory, BAI=Beck Anxiety Inventory, RSCQ=Robson self-concept questionnaire, SAPAS=Standardised Assessment of Personality, Abbreviated Scale, BPRS=Brief Psychiatric Rating Scale, expanded version.
N=31,
N=30,
N=17,
N=21.
Clinically significant recovery
Clinical significant recovery for participants was indicated for total scores of 67 or less on the SPS (Cull and Gill, 1982). At the end of treatment, over half (10/18, 56%) of participants in the CBSP group had achieved a clinically significant recovery compared to a quarter (5/22, 23%) of the TAU group (χ2=4.55, p=0.03), although this group difference was not maintained at follow-up (CBSP:53% v TAU:44%; χ2=0.25, p=0.62).
DISCUSSION
The PROSPeR trial was an exploratory pilot RCT of a novel application of CBSP for individuals at elevated risk of suicide. The results indicated that delivering CBSP within a prison setting is feasible, with the majority of patients commencing therapy and choosing to complete the programme. Further developments to the treatment protocol may be required to better support participants’ learning of new coping techniques and to enhance motivation to complete assignments between therapy sessions. For instance, the completion of homework tasks may be improved if additional support is offered between sessions, perhaps from the prisoner’s personal officer or keyworker. Also, mastery of programme content may be improved by providing participants with a self-help workbook to be reviewed between sessions.
The participant sample was drawn from a population considered to be at elevated risk of suicide and the intervention gave rise to clinically relevant improvements. The importance of this finding is particularly apparent when considered alongside the exceptionally high rates of suicidal behaviour reported by participants, with more than half of the prisoners having previously attempted suicide on two or more occasions. The CBSP therapy was found to be associated with improvements on measures relating to the primary outcome of self-injurious behaviour, as well as measures of psychiatric symptomatology, but this did not generalise to other established psychological correlates of suicide. Whilst it would be inappropriate to emphasise the statistical significance of these findings within the context of a pilot trial (Lancaster et al., 2004), such results are seen as sufficiently encouraging to warrant further investigation of the efficacy of the CBSP intervention.
To our knowledge, this is the first study that has demonstrated an improvement in the cognitive behavioural prevention of suicidal behaviour delivered within a prison setting. Previous investigations of cognitive therapy for suicidal behaviour have been conducted within community settings and treatment guidelines now recommend CBT as an important part of the longer-term management of suicidal and self-injurious behaviour (NICE, 2011). Results from the current study are consistent with previous trials demonstrating significant associations between cognitive therapy and decreases in rates of suicidal behaviour, compared to routine care (Brown et al., 2005, Slee et al., 2008, Tarrier et al., 2014). Since previous studies were conducted in community settings with patients presenting to hospital emergency departments or mental health centres, it now appears that the efficacy of cognitive therapy for suicide could extend into prison settings.
Outside of the primary outcome of actual suicidal behaviour, there has been a mixed set of results concerning the proposed psychological determinants of suicide. Cognitive therapy has been found to be significantly associated with reducing scores on measures of depression, hopelessness, anxiety and self-esteem (Brown et al., 2005, Slee et al., 2008, Tarrier et al., 2014). Contrary evidence has also been reported, where a reduction in suicide behaviour associated with cognitive therapy has been observed without concurrent improvements in these psychological correlates of suicide (Davidson et al., 2006, Morley et al., 2014). Although a pattern of reducing scores for psychological determinants was found in the current study, there was no differential impact of CBSP therapy.
Implications
A number of implications arise from this study, although these must be considered within the limited nature of a pilot trial. The modularised structure of the CBSP programme into short, ‘digestible’ components may have helped to retain participants with poorer cognitive abilities, who are more common amongst prison groups (Social Exclusion Unit, 2002). Whilst the current study drew upon the individualised case formulations for each participant to prioritise the treatment modules, the ideal ordering of the modules could be investigated. Also, CBSP was delivered on a once or twice weekly basis to participants spread across a four month treatment window. In other areas of application, CBT has been found to be preferable when delivered in a more intensive format (Ehlers et al., 2014, Oldfield et al., 2011). Participants’ tolerance of an intensive CBSP approach, and the speed of recovery and potential efficacy, should be investigated since intensive formats may help to minimise the impact of unexpected transfers and discharges during therapy delivery. Similarly, since many offender behaviour programmes are delivered within a group format, the familiarity of this format to prisoners and staff should be considered, especially if this would enable a more cost-effective delivery of CBSP. However, potential drawbacks of a group therapy format may include the loss of an individualistic approach to understanding the participant’s motivation for suicide and the reluctance of some participants to share intimate details with others in fear of potential subsequent victimisation outside the therapy group.
A policy implication of the current study concerns the availability of cognitive behavioural interventions to individuals living in prison identified to be at risk of suicide. The current ACCT system offers a robust risk management process although it remains limited in terms of proactive interventions. The targeted provision of cognitive behavioural therapies for the most vulnerable may help to contribute to the complex challenge of prison suicide prevention.
Limitations
The study has a number of limitations, which would need to be overcome to conduct a more definitive trial. The sample size for the pilot trial was sufficient to enable a preliminary investigation of the potential of the CBSP therapy, although a larger scale trial would be required for more conclusive results. Similarly, the pilot trial was conducted within one site thus limiting the heterogeneity of participants, and so further investigations should be conducted across multiple sites. Generalisability concerns are also raised, for instance, whilst the proportion of participants describing themselves as White British in the current study (85%) was in keeping with previous investigations of suicidal prisoners (e.g. 82%, Hawton et al., 2014), these proportions are notably higher than that observed amongst the general prison population (74%; MoJ, 2014).
Recruiting and retaining suicidal participants into a clinical trial has a tendency to be problematic and challenging. The high proportion (64%) of eligible prisoners who chose not to participate in the current trial presents a serious threat to the feasibility of the intervention. Indeed, treatment refusal and attrition among prisoners is higher than for most other clinical groups with non-completion of treatment endemic to all interventions delivered with prison settings (Wormith & Olver, 2002). Within prisoner groups, typical rates of refusal to enter treatment are up to 70% (Black et al., 2011; Dalton, Majoy & Sharkey, 1998) and treatment drop-outs can be as high as 93% (Gondolf & Foster, 1991). Although our previous trial of CBSP for suicidal people experiencing psychosis (Tarrier et al., 2014) achieved an attrition rate of less than 30%, attrition for the current study (44%) was more in keeping with other trials of CBT for suicide prevention (Morley et al., 2014) and intervention evaluations conducted with prisoner participants (Black et al., 2011; Olver, Stockdale & Wormith, 2011). As such, when conducting future trials, researchers may need to pay even more attention to assessing and enhancing motivation amongst the target group of participants, and prison staff, to facilitate successful recruitment.
Within the pragmatic constraints of a pilot trial, there was no remit to standardise the ‘treatment as usual’ received by all prisoners within this study, including any medication treatments provided by the Mental Health In-Reach team. The nature and content of ‘treatment as usual’ received by individual participants was not registered, although all prisoners were entitled to receive mental healthcare equivalent to that which would be offered to all NHS service users, such as psychotropic medication and nursing support.
Future research
Further research addressing the limitations highlighted above is needed to assess the effectiveness of CBSP for suicidal prisoners. Researchers should consider recruiting participants from multiple sites to investigate if CBSP has differential effects across different types of prisons. The active components of CBSP therapy should be examined by administering a more detailed assessment battery specific to the proposed psychological mechanisms targeted by the intervention, as well as measures of the treatment process. Additionally, such a trial should consider the need to compare CBSP therapy with an active comparison intervention, e.g. supportive counselling or befriending, in order to control for potential non-specific factors. Future investigations should include an economic evaluation in order to estimate the costs of use of health and social care within the custodial settings, and beyond for those released back into the community. Additional metrics on the broader impact of the intervention should also be considered, including violent incidents, prison infractions, adjudications, etc.
Conclusions
The CBSP therapy offers a novel approach that has shown some potential for providing clinical benefit to prisoners in terms of reduced self-injurious behaviour, decreased psychiatric symptomatology and personality dysfunction, and some improvement on the psychological determinants of suicide. This small scale pilot now needs to be replicated within a larger-scale multi-site randomised controlled trial.
FUNDING & ACKNOWLEDGEMENTS
This research was funded by the National Institute of Health Research Research for Patient Benefit Programme (Grant reference number: PB-PG-0609-19126): Prof N Tarrier (PI). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the RfPB programme, NIHR, NHS or the Department of Health.
We would like to acknowledge Chris Wall, Aisha Mirza and Kieran Lord for assistance with data collection and data entry; Chris Wall for administrative support; the Mental Health Research Network (especially Heather Morrison) for their support and assistance; and Peer Bhatti, Claire Daniels, Angel Delight, David O’Brien and Natasha Peniston for their contribution throughout the project as members of the Service User Reference Group (SURG).
Footnotes
CONFLICT OF INTEREST
None.
REFERENCES
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Hopelessness Scale. The Psychological Corporation; San Antonio, Texas: 1988. [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Scale for Suicide Ideation. The Psychological Corporation; San Antonio, Texas: 1991. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. The Psychological Corporation; San Antonio, Texas: 1996. [Google Scholar]
- Birmingham L. The mental health of prisoners. Advances in Psychiatric Treatment. 2003;9:191–199. [Google Scholar]
- Black G, Forrester A, Wilks M, Riaz M, Maguire H, Carlin P. Using initiative to provide clinical intervention groups in prison: a process evaluation. International Review of Psychiatry. 2011;23:70–76. doi: 10.3109/09540261.2010.544293. [DOI] [PubMed] [Google Scholar]
- Bowcott O, Taylor M, Laville S. [Accessed 24 April 2015];England and Wales prisons chief warns of ‘terrible toll’ of inmate suicides. The Guardian. 2014 http://www.theguardian.com/society/2014/oct/21/prisons-uk-chief-hardwick-suicide-prisoners-safety.
- Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Journal of the American Medical Association. 2005;294:563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- Cull J, Gill W. Manual for the suicide probability scale. Western Psychological Services; Los Angeles: 1982. [Google Scholar]
- Dalton R, Majoy S, Sharkey M. Nonattenders and attrition from a forensic psychology outpatient service. International Journal of Offender Therapy and Comparative Criminology. 1998;42:174–180. [Google Scholar]
- Davidson K, Norrie J, Tyrer P, Gumley A, Tata P, Murray H, Palmer S. The effectiveness of cognitive behavior therapy for borderline personality disorder: results from the borderline personality disorder study of cognitive therapy (BOSCOT) trial. Journal of Personality Disorders. 2006;20:450–465. doi: 10.1521/pedi.2006.20.5.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health . National Suicide Prevention Strategy for England. Department of Health; London: 2002. [Google Scholar]
- Department of Health . Improving Health, Supporting Justice: A Consultation Document. A strategy for improving health and social care services for people subject to the criminal justice system. Department of Health; London: 2007. [Google Scholar]
- Department of Health . Preventing Suicide in England: A Cross-government Outcomes Strategy to Save Lives. Department of Health; London: 2012. [Google Scholar]
- Efron B, Tibshirani RJ. An introduction to the Bootstrap. Chapman and Hall; London: 1993. [Google Scholar]
- Ehlers A, Hackmann A, Grey N, Wild J, Liness S, Albert I, Deale A, Stott R, Clark DM. A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. American Journal of Psychiatry. 2014;171:294–304. doi: 10.1176/appi.ajp.2013.13040552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel S, Benning R, Danesh J. Suicides in male prisoners in England and Wales, 1978-2003. Lancet. 2005;366:1301–1302. doi: 10.1016/S0140-6736(05)67325-4. [DOI] [PubMed] [Google Scholar]
- Fazel S, Grann M, Kling B, Hawton K. Prison suicide in 12 countries: an ecological study of 861 suicides during 2003-2007. Social psychiatry and psychiatric epidemiology. 2011;46:191–195. doi: 10.1007/s00127-010-0184-4. [DOI] [PubMed] [Google Scholar]
- Gendreau P. Offender rehabilitation what we know and what needs to be done. Criminal Justice and Behavior. 1996;23:144–161. [Google Scholar]
- Gondolf EW, Foster RA. Pre-program attrition in batterer programs. Journal of Family Violence. 1991;6:337–349. [Google Scholar]
- Hawton K, Linsell L, Adeniji T, Sariaslan A, Fazel S. Self-harm in prisons in England and Wales: an epidemiological study of prevalence, risk factors, clustering, and subsequent suicide. Lancet. 2014;383:1147–54. doi: 10.1016/S0140-6736(13)62118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollin CR, Palmer EJ. Offending behaviour programmes: Development, application and controversies. Wiley; Chichester, England: 2006. [Google Scholar]
- Humber N, Hayes A, Senior J, Fahy T, Shaw J. Identifying, monitoring and managing prisoners at risk of self-harm/suicide in England and Wales. The Journal of Forensic Psychiatry & Psychology. 2010;22:22–51. [Google Scholar]
- Jacobson NS, Roberts LJ, Berns SB, McGlinchey JB. Methods for defining and determining the clinical significance of treatment effects: description, application, and alternatives. Journal of Consulting and Clinical Psychology. 1999;67:300–307. doi: 10.1037//0022-006x.67.3.300. [DOI] [PubMed] [Google Scholar]
- Johnson J, Gooding P, Tarrier N. Suicide risk in schizophrenia: Explanatory models and clinical implications, The Schematic Appraisal Model of Suicide (SAMS) Psychology and Psychotherapy: Theory, Research and Practice. 2008;81:55–77. doi: 10.1348/147608307X244996. [DOI] [PubMed] [Google Scholar]
- Konrad N, Daigle MS, Daniel AE, Dear GE, Frottier P, Hayes LM, Kerkhof A, Liebling A, Sarchiapone M. Preventing suicide in prisons, Part I: Recommendations from the International Association for Suicide Prevention Task Force on Suicide in Prisons. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2007;28:113–121. doi: 10.1027/0227-5910.28.3.113. [DOI] [PubMed] [Google Scholar]
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. Journal of Evaluation in Clinical Practice. 2004;10:307–312. doi: 10.1111/j..2002.384.doc.x. [DOI] [PubMed] [Google Scholar]
- Landenberger NA, Lipsey MW. The positive effects of cognitive–behavioral programs for offenders: A meta-analysis of factors associated with effective treatment. Journal of Experimental Criminology. 2005;1:451–476. [Google Scholar]
- Liebling A, Maruna S, editors. The effects of imprisonment. Willan; Cullompton, England: 2005. [Google Scholar]
- Little RJ, Rubin DB. Statistical analysis with missing data. 2nd edition. Wiley; New York: 2003. [Google Scholar]
- McGuire J. Offender rehabilitation and treatment: Effective programmes and policies to reduce re-offending. Wiley; Chichester, UK: 2002. [Google Scholar]
- Medical Research Council . Developing and evaluating complex interventions: New guidance. Medical Research Council; London: 2008. [Google Scholar]
- Ministry of Justice . PSI 64/2011: Management of prisoners at risk of harm to self, to others and from others. Ministry of Justice; London: [Accessed 23 April 2015]. 2013. http://www.justice.gov.uk/downloads/offenders/psipso/psi-2011/psi-64-2011-safer-custody.doc. [Google Scholar]
- Ministry of Justice . Offender Management Statistics Prison Population 2014. Ministry of Justice; London: 2014. [Google Scholar]
- Moran P, Leese M, Lee T, Walters P, Thornicroft G, Mann A. Standardised Assessment of Personality - Abbreviated Scale (SAPAS): preliminary validation of a brief screen for personality disorder. British Journal of Psychiatry. 2003;183:228–232. doi: 10.1192/bjp.183.3.228. [DOI] [PubMed] [Google Scholar]
- Morley KC, Sitharthan G, Haber PS, Tucker P, Sitharthan T. The efficacy of an opportunistic cognitive behavioral intervention package (OCB) on substance use and comorbid suicide risk: a multisite randomized controlled trial. Journal of Consulting and Clinical Psychology. 2014;82:130–140. doi: 10.1037/a0035310. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence . Self-harm: longer-term management (Clinical guideline CG133) National Institute for Health and Clinical Excellence; London: 2011. [Google Scholar]
- Naud H, Daigle MS. Predictive validity of the suicide probability scale in a male inmate population. Journal of Psychopathology and Behavioral Assessment. 2010;32:333–342. [Google Scholar]
- Oldfield VB, Salkovskis PM, Taylor T. Time-intensive cognitive behaviour therapy for obsessive compulsive disorder: A case series and matched comparison group. British Journal of Clinical Psychology. 2011;50:7–18. doi: 10.1348/014466510X490073. [DOI] [PubMed] [Google Scholar]
- Olver ME, Stockdale KC, Wormith JS. A meta-analysis of predictors of offender treatment attrition and its relationship to recidivism. Journal of Consulting and Clinical Psychology. 2011;79:6–21. doi: 10.1037/a0022200. [DOI] [PubMed] [Google Scholar]
- Perry AE, Marandos R, Coulton S, Johnson M. Screening tools assessing risk of suicide and self-harm in adult offenders: a systematic review. International journal of offender therapy and comparative criminology. 2010;54:803–828. doi: 10.1177/0306624X09359757. [DOI] [PubMed] [Google Scholar]
- Rivlin A, Hawton K, Marzano L, Fazel S. Psychiatric disorders in male prisoners who made near-lethal suicide attempts: case–control study. The British Journal of Psychiatry. 2010;197:313–319. doi: 10.1192/bjp.bp.110.077883. [DOI] [PubMed] [Google Scholar]
- Robson P. Development of a new self-report questionnaire to measure self-esteem. Psychological Medicine. 1989;19:513–518. doi: 10.1017/s003329170001254x. [DOI] [PubMed] [Google Scholar]
- Senior J, Hayes AJ, Pratt D, Thomas SD, Fahy T, Leese M, Bowen A, Taylor G, Lever-Green G, Graham T, Pearson A, Ahmed M, Shaw JJ. The identification and management of suicide risk in local prisons. The Journal of Forensic Psychiatry & Psychology. 2007;18:368–380. [Google Scholar]
- Slee N, Garnefski N, van der Leeden R, Arensman E, Spinhoven P. Cognitive-behavioural intervention for self-harm: randomised controlled trial. British Journal of Psychiatry. 2008;192:202–211. doi: 10.1192/bjp.bp.107.037564. [DOI] [PubMed] [Google Scholar]
- StataCorp . Stata Release 11. College Station, Texas: 2009. [Google Scholar]
- Stone A, Wheeler C, Barge A. Improving the design of phase II trials of cytostatic anticancer agents. Contemporary Clinical Trials. 2007;28:138–145. doi: 10.1016/j.cct.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Gooding P, Pratt D, Kelly J, Maxwell J, Awenet Y. Cognitive Behavioural Prevention of Suicide in Psychosis: A Treatment Manual. Routledge; London: 2013. [Google Scholar]
- Tarrier N, Kelly J, Maqsood S, Snelson N, Maxwell J, Law H, Dunn G, Gooding P. The cognitive behavioural prevention of suicide in psychosis: a clinical trial. Schizophrenia Research. 2014;156:204–210. doi: 10.1016/j.schres.2014.04.029. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Taylor K, Gooding P. Cognitive-behavioral interventions to reduce suicide behavior a systematic review and meta-analysis. Behavior Modification. 2008;32:77–108. doi: 10.1177/0145445507304728. [DOI] [PubMed] [Google Scholar]
- Ventura J, Lukoff D, Nuechterlein K, Liberman R, Green M, Shaner A. Manual for the expanded brief psychiatric rating scale. International Journal of Methods in Psychiatric Research. 1993;3:221–224. [Google Scholar]
- Wormith JS, Olver ME. Offender treatment attrition and its relationship with risk, responsivity, and recidivism. Criminal Justice and Behaviour. 2002;29:447–471. [Google Scholar]