Abstract
Context
The objective of this systematic review was to determine the costs, benefits, and overall economic value of communication campaigns that included mass media and distribution of specified health-related products at reduced price or free of charge.
Evidence Acquisition
Economic evaluation studies from a literature search from January 1980–December 2009 were screened and abstracted following systematic economic review methods developed by The Community Guide. Data were analyzed in 2011.
Evidence Synthesis
The economic evidence was grouped and assessed by type of product distributed and health risk addressed. A total of 15 evaluation studies were included in the economic review, involving campaigns promoting the use of child car seats or booster seats, pedometers, condoms, recreational safety helmets, and nicotine replacement therapy (NRT).
Conclusion
Economic merits of the intervention could not be determined for health communication campaigns associated with use of recreational helmets, child car seats, and pedometers, primarily because available economic information and analyses were incomplete. There is some evidence that campaigns with free condom distribution to promote safer sex practices were cost-effective among high-risk populations and the cost per quit achieved in campaigns promoting tobacco cessation with NRT products may translate to a cost per quality-adjusted life year (QALY) less than $50,000. Many interventions were publicly funded trials or programs, and the failure to properly evaluate their economic cost and benefit is a serious gap in the science and practice of public health.
Context
The Community Preventive Services Task Force (Task Force) recommends health communication campaigns that include mass media and distribution of a health-related product at reduced price or free of charge1 on the basis of strong evidence of effectiveness in promoting healthy behaviors and protecting against disease and injury. The intervention is aligned with some social marketing principles in its adoption of communication campaigns to promote healthy behavior change and the marketing of associated health-related products. The conceptual approach, definition, choice of health-related products, and criteria for study inclusion are covered in detail in the accompanying effectiveness review.2 The objective of this economic review was to determine costs and benefits of the selected interventions considered in the effectiveness review. To the authors’ knowledge, this is the first economic review of health communication interventions that combine mass media and product distribution.
Mass media campaigns are appealing because of their ability to reach large audiences at relatively low costs per person. The expectation is that media campaigns that produce even small improvements at the individual level aggregate to substantial population-level effects. Evaluations of effectiveness of media campaigns in public health have increased both in quantity and quality since the 2000s, but with no commensurate improvement in economic evaluations.3
Evidence Acquisition
General methods of systematic economic reviews followed by The Community Guide are available online at www.thecommunityguide.org/about/economics.html. Briefly, a primary objective of a Community Guide economic review is to assess the economic value of an intervention, determined from cost-benefit or cost-utility (cost per quality adjusted life year [QALY]) estimates. Separate estimates are also derived for the cost of implementing and sustaining the intervention and the economic benefits from expected healthcare cost and productivity loss averted through reduced morbidity and mortality. Methods specific to the present review are detailed below.
The intervention definition and study inclusion criteria for this economic review are described in the effectiveness review.2 Briefly, this multicomponent intervention is conceptualized as a health communication campaign that increases awareness of and demand for a health-related product along with free or discounted distribution of that product. The campaign must use at least one mass media channel; the health-related product must be tangible and have been shown to improve health and the product should not require the services of health professionals for prescription or administration. Studies included in the effectiveness review evaluated the promotion and distribution of six health-related products: child car seats or booster seats, pedometers, condoms, recreational safety helmets, over-the-counter nicotine replacement therapy (NRT), and sun-protection products.
Studies were included in this economic review if they met the intervention definition and provided estimates for one or more of the following: intervention cost; healthcare cost changes; change in productivity at worksites; and change in morbidity and mortality measured in disability- or quality-adjusted life years. Intervention cost measures the monetary value of resources needed to implement and maintain the intervention, composed of the media promotion and product distribution components. The media promotion and product distribution components are separable activities that may be funded at different levels, and studies that provide comparative economic outcomes for different combinations of the two components were included in this economic review. Healthcare cost is the sum of costs related to inpatient and outpatient care, drugs, devices, and emergency room visits. Productivity at the worksite is the individual’s contribution to value of production, generally measured in terms of wage and salary of the individual. The intervention produces economic benefit when healthcare cost is averted or worksite productivity improves. Studies that provide cost-benefit and cost-utility estimates are central to The Community Guide systematic economic review methods: cost-benefit studies provide monetized values of both cost and benefit of the intervention and cost-utility studies provide the cost per quality-adjusted life year (QALY) saved due to intervention.
This economic review also included studies that provided cost-effectiveness based on proximal outcomes that are meaningful within particular intervention areas, such as cost per quit in tobacco control and cost per additional helmet user in preventing head injuries.
The accompanying effectiveness review2 estimated the proportion of product use within populations based on pooled intervention effects reported across different products. Similar pooling of estimates of costs and benefits for the economic review would not be sensible because the magnitudes of costs and benefits associated with the products, such as condoms and recreational helmets, differ. Pooling the economic effects for different types of products distributed might have been feasible had each study reported a standardized measure such as cost per QALY saved or benefit-cost ratio. Given the absence of such reporting, this economic review considered the evidence separately for each type of product distributed.
The literature search covered the period January 1980 through December 2009. Sources of literature searched included those for the effectiveness review2 and additional specialized databases of economic literature at the Center for Review and Dissemination in the University of York, JSTOR, and EconLit. All monetary values reported are in 2009 U.S. dollars, where adjustment for inflation used the Consumer Price Index from the Bureau of Labor Statistics,4 and adjustments for values denominated in foreign currencies used purchasing power parities5 from the World Bank. Data were analyzed in 2011.
Three research questions were posed for this review: (1) What is the cost of intervention including the costs of the media component and the product distribution component? (2) Are there any economic benefits through the intervention’s effects on healthcare cost and/or productivity? (3) How does cost compare to benefit and is the intervention cost-beneficial or cost-effective?
Organization of Review Findings
Each study was reviewed for how well it answered questions about cost and benefit components and overall economic value. Results from included studies and discussions are grouped by type of product distributed and health outcome or health risk addressed by the intervention. Conclusions for groups of studies and overall conclusions are drawn about economic value and evidence gaps.
Search Results
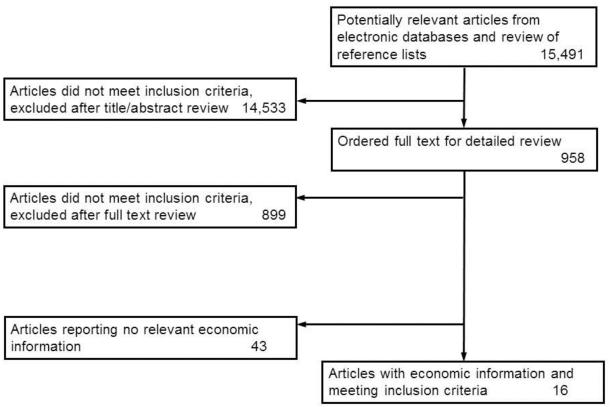
The literature search produced a list of 15,491 references. Initial screening identified 59 candidate studies, and subsequent full text review resulted in 15 unique studies (reported in 16 papers)6-21 with economic information, which were included in this review (Figure 1).
Figure 1.
Flow diagram, showing number of studies identified, reviewed in full text, reasons for exclusion, and total number of included studies.
Evidence Synthesis
Only two12,13 of the 15 included studies performed complete evaluations of economic costs and benefits of health communication campaigns with product distribution. Intervention cost was incomplete in most studies, which did not account for both the cost of media and the cost of product distribution. Four studies9,11,14,18,19 provided the grant amount with little other information. More than three quarters of the studies in this review that provided information about the source of funding were publicly financed. The number of studies for each product in the effectiveness2 and economic reviews is shown in Table 1.
Table 1.
Studies included in economic and effectiveness reviews.
| Product | Studies in economic review |
Studies in both reviews | Studies in effectiveness review |
|---|---|---|---|
| Child car seats (boosters) |
119 | 119 | 2 |
| Pedometers | 19,11 | 19 | 2 |
| Condoms | 46,13,14,16 | 26,14 | 6 |
| Recreational helmets |
58,15,17,18,21 | 415,17,18,21 | 8 |
| Nicotine replacement therapy |
47,10,12,20 | 27,20 | 3 |
| Sun-protection products |
0 | 0 | 1 |
| Total | 15 | 10 | 22 |
Six studies8,10-13,16 were included in the economic review, but not in the effectiveness review. Two8,11 were secondary studies where the primary study was included in the effectiveness review, two12,13 were studies with modeled outcomes, and the remaining two studies10,16 reported intervention cost for various jurisdictions where the interventions were implemented.
Table 2 provides a detailed description of all studies categorized by product type.
Table 2.
Details of included studies
| Study and Year Location Population Design Type of economic analysis |
Intervention components Length of intervention Volunteers and in-kind contributions |
Effectiveness | Intervention cost and components |
Economic benefits considered |
Summary economic outcome |
|---|---|---|---|---|---|
| Child safety seat use | |||||
| St Louis 200819 Oakland County, MI Area Pop: 197,846 Low-income community pop: Not reported Hispanic community pop: 11,355 Pre-Post with Comparison Funded amount |
TV, radio, print, small media, community mobilization, child seats, small group education 15 months Used volunteers |
No difference for low- income community Hispanic community: Before - 9.7% After - 14.9% (Control: Before- 18.2%, After-14.8%) 358 free seats distributed |
$53,209 grant to each of two communities No details about number of vouchers redeemed |
None | None |
| Pedometer distribution | |||||
| Brown 20069 Eakin 200711 Rockhampton, Australia Pop: 60,000 (40,000 adults) Pre-Post with Comparison Funded amount and partial intervention cost |
TV, radio, print, small media, pedometers, phone support, website, small group education, improved municipal signage and footpaths, formative research 2 years Volunteers and in-kind contributions |
No significant effect | Grant plus in-kind contributions: $530,700 Includes paid advertising and event marketing: $17,400, with additional $43,500 in-kind |
None | None |
| Condom distribution | |||||
| Alstead 19996 Seattle, WA Pop size not reported 15-17-year-olds in three communities within Seattle Pre-Post Partial intervention cost |
Radio, small media, community mobilization, condoms, small group education, formative research 7 months Volunteers used |
No significant difference in condom use at last intercourse between those exposed and unexposed to campaign |
$276,617 for formative research, media and placement, professional advertising and vending services plus $15,000 for condoms |
None |
None |
| Kahn 200113 Intervention: Eugene, OR Control: Santa Barbara, CA Target gay men aged 18-27 years (approx 1,100 in area) Pre-Post with Comparison Modeled cost- effectiveness |
(Print, small media, community mobilization, small group education, formative research, condoms) 8 months Modeled 1, 5, 20 years Volunteers used |
27% reduction in risk sex behavior (measured as reduction in unprotected anal sex) Assumed reduction in risk translates directly to same percent reduction in HIV incidence. Authors provide rationale for assumption based in literature. |
$113,641 or $676 per person (For personnel, computers and supplies, publicity and communications, condoms, travel, workspace) |
Health care averted based on lifetime medical care cost for treating HIV infections using estimates from literature |
Societal net savings= intervention cost minus averted medical costs: 1 year: $265K 5 years: $875K 20 years: $1,714K |
| Kennedy 200014 Sacramento, CA About 6,000–10,000 sexually active adolescents Pre-Post with series of surveys Funded amount |
Radio, small media, community mobilization, phone support, small peer-led group education, condoms 1 year |
OR of condom use with main partner at last intercourse: 1.26 OR of condom carrying: 1.27 |
Funding: $335,358 (~$42 per target person) No component details provided |
None |
None |
| Rebchook 200616 Multiple sites, U.S. Young gay men Cross-section of 26 community-based organizations (CBOs) Program budgets |
Print, small media, community mobilization, small group education, formative research NA – data collected during 2002–2005 |
NA | 26 CBOs provided data Annual operating budget: >$171K: 19%; $79,800-$171K: 19%; $22,800- $79,800: 5%; ≤$22,800: 23%; Don’t know: 23% Avg: $112,570; Median: $80,370; Range: $7,980– $394,349 |
NA | NA |
| Recreational helmets distribution | |||||
| Bergman 19908 Seattle, WA Elementary school children and parents (N=56,179) Pre-Post with Comparison Product discount information |
TV, radio, print, small media, community mobilization, helmets, phone support 3 years Volunteers used |
At 16 months: Intervention (Seattle): – 5% to 16%; Control (Portland): 1% to 3%; Difference: 9% |
Only intervention cost was $5K contribution to small media. Usual price of helmets $40–$60. Round 1: $19.95 helmets with coupons (5,155 of 109,450 coupons redeemed) Round 2: $25 helmet sales increasing from 1986-1.5K; 1987- 5K; 1988-22K; Partial 1989-30K |
None | None |
| Levy 200715 Denver, CO Pop. size not reported Skiers and snowboarders in area Pre-Post with Comparison Product discount information |
TV (newscast), print, small media, community mobilization, helmets, formative research 4 ski seasons starting 1998-1999 Volunteers used |
Helmet acceptance among renters: 1998-99:13.8% 2001-2002: 33.5% For control stores, corresponding percentages were 1.38% and 4.48% Observations of helmet days/rental days: 98-99: 2,150/15,567 99-00:55,581/179,705 00-01: 44,351/132,219 01-02: 75,037/224,008 Observed helmet use on slopes by skiers: 98-99: 7.7% to 01-02: 20.3% |
Usual helmet rental cost: $3.74 to $12.46 provided free to renters of package. Based on helmet days from effect size and lower estimate for rental cost, 4-year outlay was $662,425 with annual average of $165,606 |
None | None |
| Rouzier 199517 Grand Junction, CO 8,600 elementary school children and parents Pre-Post Product discount information |
Radio (news), print, small media, community mobilization, helmets, small group education 2 years Volunteers used |
Observed helmet use over 3 years: 1992: 5.6% 1993: 12.5% 1994: 30% |
Phase 1: Helmets purchased for 18.36-$26.01. 1,080 sold for $7.65; 1,080 for $22.95; and 240 for $26.01 Phase 2: 4,000 sold for $19.87 |
None | None |
| Smith 199118 Oakland County, MI 3,100 middle and junior high students and parents from six schools Pre-Post Funded amount and partial intervention cost |
TV, small media, community mobilization, phone support, small group education, formative research 5 months |
Self-reported helmet ownership increased from 5% to 18.5%. From pre to post, parent-reported helmet use 50% of time increased ~2% to ~4% for low-intensity group and ~2% to ~11% for high- intensity group |
Grant $358,355 fully financed intervention. 200 helmets given away in low-intensity group at cost of $14681.28 63 helmets given away in high- intensity group for cost of $4624.80 |
None | None |
| Wood 198821 Victoria, Australia Statewide population Pre-Post Partial intervention cost |
TV, radio, print, small media, reduced price, formative research 1 year Volunteers used |
Metro Melbourne: Observed helmeted: Primary school students: 4.6% in 1983 to 38.6% in 1985 Secondary school students: 1.6% in 1983 to 14.0% in 1985 Adults: 26.1% in 1983 to 42% in 1985 20% reduction in bicycle-related motor vehicle crash head injury in Victoria in 1982-1983 combined, compared to 1984 |
Partial cost provided as cost of TV/radio campaign was $294,286; total cost of rebates for helmets of $745,200 (calculated by reviewers) |
None | None |
| Nicotine replacement therapy (NRT) distribution | |||||
| Bauer 20067 Western NY All callers to quitline Pre-Post with Comparison Cost per additional quitline caller |
Print, small media, community mobilization, phone support, NRT, supplies 3-4 weeks 3 Treated Arms: Arm 1: Newspaper and magazine ad with NRT Arm 2: Newspaper ad Arm 3: Newspaper ad with cigarette look-alike |
Arm 1: Incremental calls – 4724 Quit (7-day abstinence): 22% for those redeeming NRT versus 12% pre-NRT, implying OR=1.77 Arm 2: Incremental calls – 14 Arm 3: Not reported Treated quits: 20% Controls: 24% |
Arm1: $58,487 (For newspaper and magazine ad and NRT) Arm 2: $3,810 for newspaper ad Arm 3: Not reported (For newspaper ad and plastic cigarette at $1.71 each) |
None | Cost per incremental call Arm 1: $12.54. Arm 2: $272.46 Arm 3: $93.48 |
| Cummings 2006a10 (linked to Miller 200522 and Cummings 2006b23) 4 regions of New York Region I: Buffalo area, n=1,099 Region II: 8 counties, n=1,334 Region III: 15 counties, n=2,323 Region IV: NYC, n=35,334 All callers to quitline Pre-Post with Treated Comparison Cost per additional quit |
Radio, print, small media, NRT, phone support 4 regions with varying durations of free NRT and type of media Region I: 2 weeks with earned media Region II: 2 months with earned media and paid radio Region III: 4 weeks with earned media and print ads Region IV: 6 weeks with earned media |
Daily call volume by region Region: Before/After I: 312/63=5.0 II: 393/79=4.97 III: 931/60=15.5 IV: 7,213/552=13.1 Region: Percent quits (risk ratio) Pre-NRT: 12% (1.0) I: 27% (2.9) II: 21% (2.0) III: 24% (2.4) IV: 33% (3.8) |
Intervention cost (per enrollee) by region: I: $52,856 ($48) II: $43,823 ($33) III: $110,382 ($48) IV: $3.08 Mil ($87) |
None | Cost per quit due to NRT by region: I: $312(n=169) II: $349(n=125) III: $396(n=279) IV: $396(n=7770) |
| Fellows 200712 State of Oregon Pop. size not reported All callers to quitline Pre-Post Cost per LYS |
TV, radio, NRT, phone support, counseling 3 months |
Calls to quitline Jan- June (monthly avg): Pre-Patch: 3,214 (136) Patch Period: 6,823 (1,137); Difference: 3,609 (602) Quits defined as 30- day abstinence at 6 months: Pre-Patch: 8.2% Patch:15.7% |
Note: 2 months of paid ads assumed for post- patch period for cost-effectiveness analysis. Pre vs patch period Total cost: $224,5897 vs $256,5552 Media cost: $1,579,056 vs $483,789 NRT+counseling cost: $666,841 vs $2,081,763 |
Quits converted to LYS based on age- specific estimates from literature |
Pre vs. patch period Callers: 6,428 vs 13646 Quits (%): 527 (8.2) vs 2,142 (15.7) LYS: 1,246 vs 4,502 Cost/quit: $4,261 vs $1,197 Incremental cost/quit: NA vs $198 Incremental cost/LYS: NA vs $98 (Bounds of $25 to $402 per LYS based on sensitivity analysis on quit rate, intervention cost, and discount rate) |
| Tinkelman 200720 State of Ohio All callers to quitline Pre-Post with Comparison Partial intervention cost |
NRT, phone support, formative research Multimillion $ media campaign but no details about channels. NRT became available in July 2005; 4-week supply plus another 4 weeks if continuing in program. NRT promoted through media Sept 2005–April 2006 (7 months). |
Call volume per day: increase from 78 per day pre-NRT to 188 post-NRT Quit (7-day abstinence) 10.3% pre NRT and 14.9% post NRT, measured at 6- month follow-up. Post NRT quit rate 11.2% for Counseling Only and 20.2% for Counseling + NRT. |
Pre-NRT (Jul 2004-Apri 2005) media costs $4,620,000; Post-NRT (Sept 2005–Apr 2006) $3,180,000. No cost of NRTs provided. Reviewers assumed difference went to finance free NRT. |
None | None |
Avg, average; K, thousand (000); LYS, life-years saved; NRT, nicotine replacement therapy
Interventions to Promote Booster Seats and Child Car Seats for Injury Prevention
The per capita cost of intervention to increase the use of booster seats could not be estimated because the one included study19 provided only the total funded amount and did not provide an accurate estimate of the study population (Table 2). The intervention was effective only in one of two targeted communities. In the other, the intervention was not cost-effective because the intervention cost was positive, but there was no effect on health outcome.
Interventions to Promote Pedometers to Increase Physical Activity
The study (reported in two papers)9,11 that evaluated the promotion of physical activity with distribution of pedometers found the cost of intervention to be $13.27 per adult resident. This intervention was not cost-effective as there was no change in self-reported physical activity following the intervention.
Condoms and Prevention of Sexually Transmitted Infections
Four studies6,13,14,16 evaluated campaigns with condom distribution to prevent sexually transmitted infections and pregnancies (Table 2). Estimated per capita intervention cost varied widely from $42 among adolescents in a large urban population14 to $676 among young gay men (the MPowerment program) in a small city.13 A survey16 of community-based organizations (CBOs) between 2002 and 2005 reported the median annual budget for the MPowerment program was about $80,370; per capita cost could not be calculated because sizes of target populations were not specified.
The evaluation13 of the Mpowerment program was one of the very few studies that provided a complete accounting for intervention cost and also modeled the economic benefits based on averted medical care cost for HIV. The study assumed the percentage reduction in risk behavior measured by unprotected anal intercourse translated to an equal percentage reduction in HIV incidence. The economic benefit of intervention was estimated as the averted cost of healthcare from HIV infections prevented, based on estimates from the literature. The cost of intervention was drawn from actual program costs and included the key components of promotion and product distribution. All costs were discounted and sensitivity analyses were performed based on: societal and public health agency perspectives; different rates of HIV prevalence; and time horizons of 5 and 20 years. Savings from healthcare cost averted exceeded intervention cost in the first year, and increased over the 5- and 20-year modeled horizons.
On the other hand, another study6 of an intervention among adolescents found no change in condom use at last intercourse. Though per capita cost of intervention could not be calculated from the $276,617 program cost because the size of study population was not specified, the intervention was ineffective and hence could not have been cost-effective.
Given the paucity of studies that provided a complete economic analysis of both costs and benefits and the inconsistent results from cost-benefit and cost-effectiveness studies, a clear conclusion cannot be drawn about the economic value of the intervention.
Recreational Safety Helmets to Prevent Head Injury
Only two18,21 of five8,15,17,18,21 included studies provided details on program costs, and no study provided sufficient information to compute cost-effectiveness (Table 2). All studies evaluated promotion of bicycle helmets except one,15 which was for ski helmets. Three8,15,17 studies provided economic information only for the free or discounted helmet component of the intervention.
These partial estimates are presented here to emphasize that such interventions can be costly when implemented population-wide. One study8 of bicycle helmet promotion among elementary school children reported an increase in sales from 1,500 units to over 22,000 over a 2-year period, during which participating retailers offered the helmets for an average of $40 when the undiscounted prices in the area averaged $95. Another helmet promotion17 among elementary school children achieved an increase from 5.6% to 30.0% in helmet use at a cost of approximately $15,000 for the discount component of the program. The study of helmet promotion among skiers and snowboarders in Colorado15 reported a 16.6% increase in acceptance from 1998–1999 to 2001–2002 when equipment renters were offered a free loaned helmet in their rental package, for an annual outlay of approximately $166,000 for the sponsors.
Two studies reported what may be a reasonably accurate estimate for intervention cost. A 5-month bicycle helmet promotion among 3,100 students from six middle and junior high schools and their parents was fully financed by a $358,355 grant.18 The study found a 15.5 percentage point increase in helmet ownership and some increase in parent-reported helmet use. Based on the grant amount, the per capita cost was about $116 for this 5-month intervention. The other study21 evaluated a helmet promotion campaign implemented in Victoria, Australia, which offered purchase rebates. Partial program cost was provided as $294,286 for TV and radio campaigns and $745,200 for rebates over the approximate 1-year duration of the intervention (the rebate was calculated as an approximate value by the present reviewers). The study noted a substantial increase in helmet use among school children in the Melbourne metro area, as well as a 20% reduction in the incidence of bicycle-related head injury involving motor vehicle crashes in Victoria, when comparing injury data from 1982–1983 and 1984.
Nicotine Replacement Therapy and Tobacco Cessation
Four studies7,10,12,20 evaluated interventions promoting tobacco cessation through quitlines with distribution of NRTs (Table 2). Only one study12 modeled life years saved based on observed quits, indicating a cost per life year saved that probably meets the standard threshold for cost-effectiveness. Free or reduced-cost distribution of NRTs was consistently shown to increase calls to quitlines7,20 while also increasing quit rates12,20 among participants. The number of quits reported in the included studies was based on surveys of the population of callers to quitlines and does not account for quits that occurred within the larger population in response to the media component of the intervention. Similar to interventions for recreational helmets, reduced price and greater availability appear to increase use but also constitute a substantial cost of the intervention.
Results from two state-wide studies12,20 suggest that incremental effectiveness in terms of call volume to quitlines is not sacrificed by relying on cheaper mass media such as earned versus paid media, and radio or print versus TV. However, the effect of the intervention is likely to diminish over time and the use of paid mass media may be necessary to sustain the population-level change in behavior. The first study20 did not report the cost of product purchase and distribution, and the present reviewers assumed that the difference in media expenditures between the periods (about $1.44 million) went substantially to purchase NRTs. Daily call volume to quitlines increased from 78 to 188, and self-reported 7-day abstinence at 6-month follow-up increased from 10.3% to 14.9%. The second study12 evaluated a change in intervention strategy that reduced TV and radio coverage cost from $1.58 million to $0.48 million and increased the outlay for free NRT plus counseling from $0.67 million to $2.08 million. The monthly average calls to quitlines increased from 536 in the pre-NRT period to 1,137 in the free NRT period, a difference of 7,212 per year, and quits increased from 8.2% to 15.7%.
Four variants of campaigns that promoted quitlines along with free NRT distribution operated in New York City (NYC) and three other regions of New York State during 2003–2004.10 The campaign in NYC was longer in duration and offered a more generous 6-week supply of NRT patches to callers. Intervention cost ranged from $33 to $48 for three regions to $87 for NYC, and cost per quit ranged from $312 to $396, with the higher estimate associated with NYC and one other region. A 6-month follow-up evaluation22 of the NYC program reported $3.28 million in program cost, with the NRT product contributing $2.93 million. At 12-month follow-up,23 the cost per quit was $491.
Another study7 of the New York quitline programs evaluated an intervention with three arms: 4-week media campaign promoting the quitline plus free 2-week supply of NRT; a newspaper advertisement to call the quitline for a cessation guide; and a newspaper ad to call the quitline for the guide and a free cigarette look-alike containing no nicotine. Calls to the quitlines increased for all three arms, with the incremental cost per additional call at $12.54 for the first intervention, $93.48 for the cigarette look-alike arm, and $272.46 for the arm without the free product. The authors concluded that the free NRT program was preferable to the newspaper advertisement alone.
The one NRT study12 that modeled long-term outcomes estimated cost per life year saved at $98 which varied between $25 and $402 in sensitivity analysis. These estimates are below the conservative threshold for cost-effectiveness of $50,000 per QALY saved. Cost of intervention for this study was derived as the difference in observed cost of promotion and product distribution in the post-intervention and pre-intervention periods. Quit rates based on intent-to-treat were estimated from a survey of registered callers to the quitline, and quits were translated to life years saved based on age-specific life expectancy for smokers and quitters derived from the literature. A discount rate of 3% was applied to life years saved and sensitivity analysis was performed based on upper and lower CI estimates for intervention cost and quit rates. Likely savings from healthcare cost averted were not included in this model, which could have improved the cost-effectiveness ratio.
Conclusion
The studies included in this review do not provide evidence to reach a conclusion about the economic merit of health communication campaigns that use mass media combined with product distribution. Some evidence suggests that this intervention strategy might be cost-effective in promoting condom use among high-risk populations and in promoting tobacco cessation with NRT products. However, the small body of evidence also includes studies of three instances of interventions with positive cost but no positive effect on health outcomes: child car booster seats to reduce injuries; pedometers to increase physical activity; and another to increase condom use. These instances of the intervention were not cost-effective.
The scarcity of good quality estimates across three categories of information made the determination of the intervention’s economic merits difficult: cost of intervention; cost consequences for healthcare and worksite productivity; and life years or QALY saved. Program costs reported in many studies were often incomplete: in-kind and voluntary contributions were not valued, or the product and distribution cost of this multicomponent intervention simply ignored. Cost consequences for healthcare and intervention effects on worksite productivity were rarely recorded or modeled.
Finally, the effects reported were often based on proximal outcomes specific to the intervention, such as incremental quits among smokers or reduction in unprotected sex. The determination of economic value of the intervention would require modeling these effects to monetary values for a cost-benefit assessment or to QALYs for a cost-effectiveness assessment.
Regarding study populations, although it is difficult to ascertain information on the treated population for mass media interventions, having at least an estimate of the population of interest is useful. This information, missing from some included studies, is needed to convert program costs to a per capita basis, so that similar interventions implemented in different populations can be compared.
A 2006 supplement of the Journal of Health Communication3 included a collection of papers by experts in communication and economics providing guidance and exhortations for improvement in evaluation studies. The supplement included a review of economic evaluations of mass media health interventions24 that determined how well studies published between 1981 and 2005 adhered to standards of good health economics evaluation research. The Hutchinson and Wheeler review24 identified 19 studies published between 1981 and 2005 of interventions in high-income countries that included mass media components. Key findings of the review were: lack of documentation, rigor, and transparency for costs included or excluded; failure to value resources at opportunity cost; omission of capital and overhead costs; retrospective data collection; diversity of outcomes ranging from process outcomes to intermediate outcomes, particular to the health intervention and the rare use of standardized DALY or QALY; and design elements that prevented estimation of incremental cost-effectiveness due to intervention. However, it may be noted that the last two observations are not unexpected for mass media interventions, given the acknowledged problems in designing controlled experiments when exposure to treatment is population-wide. The present review came to very similar findings and conclusions for the focused area of mass media campaigns that include health-related product distribution.
Providing a health-related product at a discount or no charge increases use and associated positive health behavior. Increased product acquisition may be due to removing non-price–related barriers to access; convenience of the distribution network; or price lowering. The importance of price is likely to be greatest where the product constitutes a large part of a population’s income; a program that distributes such a product at a discount or no charge can expect a substantial outlay for the product component of this multicomponent intervention. Yet it may also require substantial funds to finance the distribution infrastructure for even a relatively inexpensive product, such as condoms. Reduced price or no-charge promotions for a relatively expensive product, such as recreational helmets, increases demand, and private sector or government funds must consistently be available to underwrite such costs.
Many interventions were publicly funded trials or programs, and the failure to properly evaluate their economic cost and benefit is a serious gap in the science and practice of public health.
Acknowledgments
The authors acknowledge Kara Contreary and Anilkrishna B. Thota for numerous thoughtful comments and suggestions and Kate W. Harris for expert editorial assistance at various stages in the review and the development of the manuscript; all are in CDC’s Center for Surveillance, Epidemiology, and Laboratory Services. The authors also thank three anonymous reviewers for many helpful comments.
Footnotes
Author affiliations are shown at the time the work was conducted.
The names and affiliations of the Task Force members are at www.thecommmunityguide.org/about/task-force-members.html
Points of view are those of the Community Preventive Services Task Force and do not necessarily reflect those of the CDC.
References
- 1.Community Preventive Services Task Force Recommendation for health communications campaigns that include mass media and health-related product distribution. Am J Prev Med. 2014;47(3):372–4. [Google Scholar]
- 2.Robinson MN, Tansil KA, Elder RW, et al. Social marketing in public health: combining mass media health communication campaigns with health-related product distribution. A Community Guide systematic review. Am J Prev Med. 2014;47(3):360–71. doi: 10.1016/j.amepre.2014.05.034. [DOI] [PubMed] [Google Scholar]
- 3.Special issue on cost-effectiveness analysis. J Health Commun. 2006;11(Suppl 2):1–73. doi: 10.1080/10810730600973987. [DOI] [PubMed] [Google Scholar]
- 4.Consumer Price Index - All Urban Consumers: U.S. Department of Labor, Bureau of Labor Statistics. http://data.bls.gov/PDQ/outside.jsp?survey=cu.
- 5.World Bank World Development Indicators http://data.worldbank.org/indicator.
- 6.Alstead M, Campsmith M, Halley CS, Hartfield K, Goldblum G, Wood RW. Developing, implementing, and evaluating a condom promotion program targeting sexually active adolescents. AIDS Educ Prev. 1999;11(6):497–512. [PubMed] [Google Scholar]
- 7.Bauer JE, Carlin-Menter SM, Celestino PB, Hyland A, Cummings KM. Giving away free nicotine medications and a cigarette substitute (Better Quit (R)) to promote calls to a Quitline. J Public Health Manag Pract. 2006;12(1):60. doi: 10.1097/00124784-200601000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Bergman AB, Rivara FP, Richards DD, Rogers LW. The Seattle children's bicycle helmet campaign. Arch Pediatr Adolesc Med. 1990;144(6):727. doi: 10.1001/archpedi.1990.02150300127033. [DOI] [PubMed] [Google Scholar]
- 9.Brown WJ, Mummery K, Eakin E, Schofield G. 10,000 Steps Rockhampton: evaluation of a whole community approach to improving population levels of physical activity. J Phys Act Health. 2006;3(1):1. [Google Scholar]
- 10.Cummings KM, Fix B, Celestino P, Carlin-Menter S, O'Connor R, Hyland A. Reach, efficacy, and cost-effectiveness of free nicotine medication giveaway programs. J Public Health Manag Pract. 2006;12(1):37. doi: 10.1097/00124784-200601000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Eakin EG, Mummery K, Reeves MM, et al. Correlates of pedometer use: Results from a community-based physical activity intervention trial (10,000 Steps Rockhampton) Int J Behav Nutr Phys Act. 2007;4(1):31. doi: 10.1186/1479-5868-4-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fellows JL, Bush T, McAfee T, Dickerson J. Cost effectiveness of the Oregon quitline “free patch initiative”. Tob Control. 2007;16(Suppl 1):i47. doi: 10.1136/tc.2007.019943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kahn JG, Kegeles SM, Hays R, Beltzer N. Cost-effectiveness of the Mpowerment Project, a community-level intervention for young gay men. J Acquir Immune Defic Syndr. 2001;27(5):482. doi: 10.1097/00126334-200108150-00010. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy MG, Mizuno Y, Seals BF, Myllyluoma J, Weeks-Norton K. Increasing condom use among adolescents with coalition-based social marketing. AIDS. 2000;14(12):1809. doi: 10.1097/00002030-200008180-00017. [DOI] [PubMed] [Google Scholar]
- 15.Levy AS, Hawkes AP, Rossie GV. Helmets for skiers and snowboarders: an injury prevention program. Health Promot Pract. 2007;8(3):257. doi: 10.1177/1524839906292178. [DOI] [PubMed] [Google Scholar]
- 16.Rebchook GM, Kegeles SM, Huebner D. Translating research into practice: The dissemination and initial implementation of an evidence-based HIV prevention program. AIDS Educ Prev. 2006;18(suppl):119–36. doi: 10.1521/aeap.2006.18.supp.119. [DOI] [PubMed] [Google Scholar]
- 17.Rouzier P, Alto WA. Evolution of a successful community bicycle helmet campaign. J Am Board Fam Pract. 1995;8(4):283. [PubMed] [Google Scholar]
- 18.Smith PK. Evaluation report. Michigan Helmet Advisory Committee; Lansing: Increasing bicycle helmet use in Michigan: A school-based intervention pilot program. www.eric.ed.gov/ERICWebPortal/recordDetail?accno=ED351329. [Google Scholar]
- 19.St Louis RM, Parow JE, Eby DW, Bingham CR, Hockanson HM, Greenspan AI. Evaluation of community-based programs to increase booster seat use. Accid Anal Prev. 2008;40(1):295–302. doi: 10.1016/j.aap.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 20.Tinkelman D, Wilson SM, Willett J, Sweeney CT. Offering free NRT through a tobacco quitline: impact on utilisation and quit rates. Tob Control. 2007;16(Suppl 1):i42. doi: 10.1136/tc.2007.019919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wood T, Milne P. Head injuries to pedal cyclists and the promotion of helmet use in Victoria, Australia. Accid Anal Prev. 1988;20(3):177–85. doi: 10.1016/0001-4575(88)90002-4. [DOI] [PubMed] [Google Scholar]
- 22.Miller N, Frieden TR, Liu SY, et al. Effectiveness of a large-scale distribution programme of free nicotine patches: a prospective evaluation. Lancet. 2005;365(9474):1849–54. doi: 10.1016/S0140-6736(05)66615-9. [DOI] [PubMed] [Google Scholar]
- 23.Cummings KM, Hyland A, Fix B, et al. Free Nicotine Patch Giveaway Program: 12-month follow-up of participants. Am J Prev Med. 2006;31(2):181–4. doi: 10.1016/j.amepre.2006.03.027. [DOI] [PubMed] [Google Scholar]
- 24.Hutchinson P, Wheeler J. The cost-effectiveness of health communication programs: What do we know? J Health Commun. 2006;11:7–45. doi: 10.1080/10810730600973862. [DOI] [PubMed] [Google Scholar]