Abstract
Background
Health insurance plans have historically limited the benefits for mental health and substance abuse (MH/SA) services compared to benefits for physical health services. In recent years, legislative and policy initiatives in the U.S. have been taken to expand MH/SA health insurance benefits and achieve parity with physical health benefits. The relevance of these legislations for international audiences is also explored, particularly for the European context.
Aims of the Study
This paper reviews the evidence of costs and economic benefits of legislative or policy interventions to expand MH/SA health insurance benefits in the U.S. The objectives are to assess the economic value of the interventions by comparing societal cost to societal benefits, and to determine impact on costs to insurance plans resulting from expansion of these benefits.
Methods
The search for economic evidence covered literature published from January 1950 to March 2011 and included evaluations of federal and state laws or rules that expanded MH/SA benefits as well as voluntary actions by large employers. Two economists screened and abstracted the economic evidence of MH/SA benefits legislation based on standard economic and actuarial concepts and methods.
Results
The economic review included 12 studies: eleven provided evidence on cost impact to health plans, and one estimated the effect on suicides. There was insufficient evidence to determine if the intervention was cost-effective or cost-saving. However, the evidence indicates that MH/SA benefits expansion did not lead to any substantial increase in costs to insurance plans, measured as a percentage of insurance premiums.
Discussion and Limitations
This review is unable to determine the overall economic value of policies that expand MH/SA insurance benefits due to lack of cost-effectiveness and cost-benefit studies, predominantly due to the lack of evaluations of morbidity and mortality outcomes. This may be remedied in time when long-term MH/SA patient-level data becomes available to researchers. A limitation of this review is that legislations considered here have been superseded by recent legislations that have stronger and broader impacts on MH/SA benefits within private and public insurance: Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) and the Patient Protection and Affordable Care Act of 2010 (ACA).
Implications for Future Research
Economic assessments over the long term such as cost per QALY saved and cost-benefit will be feasible as more data becomes available from plans that implemented recent expansions of MH/SA benefits. Results from these evaluations will allow a better estimate of the economic impact of the interventions from a societal perspective. Future research should also evaluate the more downstream effects on business decisions about labor, such as effects on hiring, retention, and the offer of health benefits as part of an employee compensation package. Finally, the economic effect of the far reaching ACA of 2010 on mental health and substance abuse prevalence and care is also a subject of future research.
Introduction
Background
Historically, private health insurance plans in the U.S. limited mental health and substance abuse (MH/SA) benefits compared to the benefits covered for physical health.1,2 MH/SA benefits were usually controlled through lower quantitative limits on specific services and higher copayments and deductibles.3 Monitoring and gatekeeping the demand for mental health treatment and services was believed to be more difficult than for physical health.4
Various actuarial models from the mid-1990s predicted that federal legislation expanding mental health benefits would increase utilization of those services and insurance premium would increase anywhere from 3.2% to 11.4%.5 This expectation found empirical basis in early results from the Rand Health Insurance Experiment (RAND HIE)6, which demonstrated higher utilization associated with lower patient cost-sharing or out-of-pocket (OOP) cost.
Beginning in the 1990s, federal and state legislations, executive orders and corporate policy changes sought to relax the quantitative and financial limits on behavioral health benefits in group health insurance plans.7,8 Similar expansions in MH/SA benefits in relation to physical benefits were implemented and evaluated by large private and public employers with self-insured plans. Though more recent federal legislation such as the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) and the Affordable Care Act of 2010 (ACA) were enacted, they have not been in effect over a sufficiently long period to produce published evaluations.
The market for voluntary health insurance (private health insurance) in Europe is small given the prevalence of universal public insurance in all but a few countries in Central and Eastern Europe. However, the experience of the U.S. in implementing parity in private insurance benefits for mental health is relevant for Europe. Unequal access to health promotion, prevention and treatment for mental health exists also in Europe’s systems of universal coverage, prompting national legislations such as in the U.K.9 It is noted that the higher out- of- pocket costs required for specialist mental health care constitute disparity in access to mental health relative to physical health services for several Western European countries.10 Further, it is a practice in many European countries to transfer long term care of chronic aspects of mental health out of the health care system and into the social care system with plausibly different eligibility requirements, means testing, and out- of- pocket cost.11 The U.S. enacted policies and laws to require equal access for mental health services and their consequences for cost and health outcomes are thus relevant for Europe irrespective of whether the final payer is private insurance or a public fund. Finally, mental health is integral to both capabilities and the exercise of those capabilities for the well-being of all individuals12 and it is therefore a matter of justice that the objectives of good mental and physical health have equal weight for all national health systems.
Aims of the Study
A recent evidence review,13 conducted for the Community Preventive Services Task Force (CPSTF), found that these interventions that expanded mental health benefits were effective in improving financial protection and increasing appropriate utilization of mental health services for people with mental illness. The CPSTF is an independent, nonfederal, unpaid panel of public health and prevention experts, established in 1996 by the U.S. Department of Health and Human Services to identify population health interventions that are scientifically proven to save lives, increase lifespans, and improve quality of life for the U.S. population. The objective of the present study is to review the evidence of economic effects of the interventions that expanded mental health benefits. In particular, the research questions and the associated economic outcomes of interest are: (1) What is the cost of implementing and administering policies that expand MH/SA health insurance benefits? (2) What is the effect of MH/SA benefits expansion on healthcare cost? (3) What is the effect of the intervention on productivity at the worksite? (4) What is the economic impact of intervention on the plan provider?
Methods
The general methods for conducting systematic economic reviews for the CPSTF can be found at http://www.thecommunityguide.org/about/economics.html. The translation of general methods to the present review is detailed below. A coordination team (team), comprising of subject matter experts on mental health from various organizations as well as systematic review experts, developed an analytic framework and guided a systematic search to identify relevant studies that reported economic information about the intervention. Details about intervention definitions and the analytic framework may be found at http://www.thecommunityguide.org/mentalhealth/benefitslegis.html.
Identification and Selection of Studies
The search covered the period January 1950 to February 2011 and used the following sources: Center for Reviews and Dissemination (CRD) at the University of York, Medline, EconLit, PsycINFO, and Google Scholar. Detailed strategy and criteria for the economic search can be found at http://www.thecommunityguide.org/mentalhealth/SS-benefitslegis-econ.html. Studies that contained economic information were also identified from the search yield for the effectiveness review.13 Studies were included if they: (1) met the definition of intervention; (2) were in English; (3) were conducted in a high income country;14 (4) estimated or modeled at least one of the following: intervention cost; effect on healthcare cost; effect on productivity at work; effect on cost per life year gained or cost per quality/disability adjusted life year saved/averted.
Concepts and Measurements
Interventions are those that expand MH/SA benefits through legislations and policies, regardless of the mechanism (e.g. federal or state law or executive order, administrative rule, employer benefits policy).
Intervention Cost is the dollar value of time and materials used by experts, interest groups, leaders/legislators, and staff in their activities both in favor and in opposition to the policies, and the resources needed to monitor and enforce the policies, once they are in place.
Cost Consequences for Healthcare due to Intervention measure the change in the sum of inpatient and outpatient care costs plus the cost of drugs for MH/SA due to the expansion of benefits. It is usually measured from claims data. The out-of-pocket (OOP) cost to the covered patient was included in the review of effectiveness13 and is not considered here since it is not a cost to the plan.
Healthcare cost can either increase or decrease in response to the benefits expansion. If the current users of MH/SA services increase their use, or other enrollees start to use these services once they became more readily accessible, the cost might increase. On the other hand, if expanded MH/SA benefits improve prevention and treatment and reduce morbidity, healthcare cost might decrease.
Economic Benefits due to Intervention are the societal economic benefits arising from health care costs averted and productivity gains in worksites due to improvements in health. Improvements in health in turn reduce morbidity and mortality and thereby increase quality-adjusted life years (QALY) saved or disability-adjusted life years (DALY) averted.
Plan Cost is the cost consequence to the plan provider due to MH/SA benefits expansion and is calculated from the change in healthcare cost for MH/SA minus deductibles and other out-of-pocket costs paid by the patients. Claims data are used to measure changes in healthcare utilization from the perspective of the plan provider. Claims are classified as mental health or substance abuse treatment based on the diagnosis related group (DRG) code and further classified into inpatient and outpatient categories. Claims for drug benefits are often separate and managed by specialized vendors.
Assessment of Impact on Plan Provider The economic impact of MH/SA benefits expansion from a plan provider’s perspective is assessed by estimating the change in plan cost as a percentage of revenues from premiums. This provides a basis to judge whether any observed change in cost was small or large in relation to revenue and the plan’s ability to absorb the impact of expansion in MH/SA benefits. Operating financials for health insurance plans are generally measured in per member per year (PMPY) terms, where member is the plan-holder who contributes to premiums or for whom the premiums are paid. The plan-holder may opt for single coverage, or for family coverage that includes spouse and children. In this review, the persons covered under a plan are collectively referred to as enrollees. Research and administrative reports generally identified claims with the person for whom expenses are incurred while premiums are reported in per member (plan-holder) terms. This review constructed per person per year (PPPY) estimates for both the cost and revenue sides of the equation, where the person is any enrollee. These standard methods of accounting in insurance operations are similar to concepts and methods in a recent background report developed by the Congressional Research Services to assist legislators in their debate on regulating private health insurance premiums,15 and also in actuarial training materials.16
It is difficult to estimate premium revenues for private group plans because the information is generally proprietary and confidential. The review team drew from multiple sources for premium, plan type, and enrollment data. The US Office of Personnel Management (OPM) provided average premiums (Personal communication with OPM) for various Federal Employee Health Benefits (FEHB) plans and the overall counts for plan-holders and dependents.17 Premiums for private health insurance plans and the percentage distribution of single coverage were obtained from the insurance component of the Medical Expenditure Panel Survey (MEPS-IC).18 MEPS-IC is based on data collected by the Agency for Healthcare Research and Quality (AHRQ) since 1996 through a survey of private and public sector employers. The number of covered dependents on family plans is not available in MEPS-IC and national estimate for employer-sponsored plans from the Current Population Surveys (CPS) of the U.S. Census Bureau19 was used to estimate this variable.
We chose the premium most appropriate for comparison against the source of claims used in the studies to estimate the change in cost of utilization based on: HMO or PPO provider type; claims for plan-holders only, plan-holder plus dependents, or dependents only; geographic area; federal government, state and local government, or private sector employer; size of private employer; and year claims generated. The following rules were followed:
Claims from HMO – HMO premiums were used
Claims from PPO – mixed provider premiums were used
Large employer – used premiums for insurance sponsored by employers with greater than 1000 employees
Years of claims – in pre to post analysis of claims, the premium from the midpoint of the pre to post period was used.
Plan-holder only claims – used premium for single coverage
Plan-holder plus dependent claims – used weighted single and family premium with weights provided by percentage of plan-holders opting for single coverage and the average number of dependents in family coverage
Dependent only claims – used premium for family coverage weighted by average number of dependents in family coverage
All monetary values in this review are reported in nominal U.S. dollars and are not adjusted for inflation. Adjustments for price level alone are not sufficient to draw valid inferences regarding magnitude and direction of change from observations of MH/SA costs that are many years apart because recognized MH/SA conditions and available treatments in the two periods can be very different. Besides, financial consequence to the insurance plans due to expanded benefits is assessed on the basis of the percentage change in claims cost in relation to existing health insurance premium for that period, a ratio that does not involve actual dollar values.
Listing of Economic Evidence
Findings from the Federal Employees Health Benefits (FEHB) studies are discussed first, followed by statewide studies and individual employer studies. The FEHB studies are considered strong because of the plans’ large membership and study sample sizes, the increased MH/SA benefits that resulted from the executive order, and detailed historical claims data that were analyzed for multiple plans. The evidence from statewide mandate studies is considered next because the mandated incremental MH/SA benefits applied to a large population in a defined geographic area. The evidence from individual private and public employers is discussed last because the voluntary nature of their decision to expand MH/SA benefits may reflect unobserved selection biases.
Results
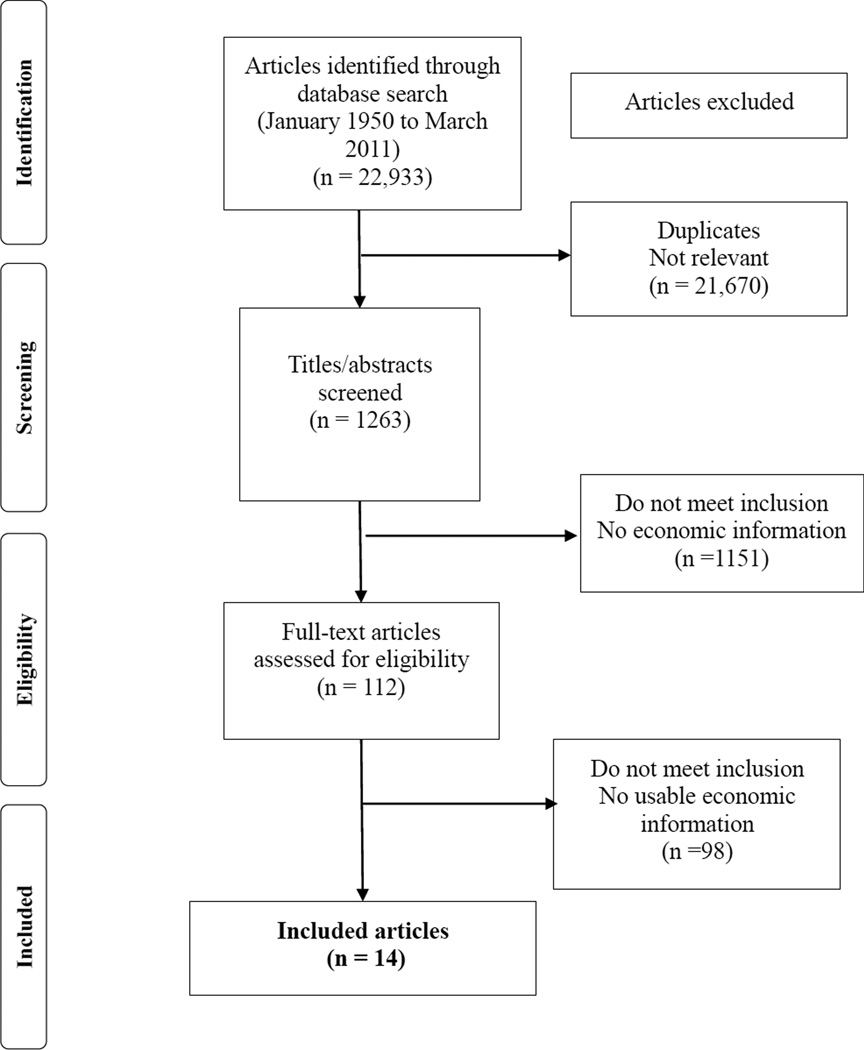
A total of 1263 potentially eligible papers were identified from the search, out of which 112 full text papers were considered after title and abstract screening, to yield 14 papers that met all inclusion criteria based on detailed full text review (Figure 1).20–33 Three papers31–33 are considered a single study because the same core set of authors analyzed the same plans and data, and the conclusions in the last paper drew on results from the previous two. Thus, a total of 12 studies (in 14 papers) were included in the review. An additional unpublished report34 was used to adjust estimates in one23 of the included studies. All included studies were based in the U.S.
Figure 1.
Flow chart of article selection
Intervention cost
No studies reported the economic cost of time and materials that brought about the policy change expanding MH/SA insurance benefits.
Healthcare cost
All but one26 of the studies reported the effect of benefits expansion on healthcare cost, based on estimates from claims for MH/SA treatments. The estimated changes in cost of MH/SA utilization are reported below in the section on Cost Impacts for Plan Providers.
Cost-Benefit and Cost-Effectiveness
No studies reported cost per QALY saved or benefit-to-cost ratios for the intervention. The absence of this evidence is not unexpected since monetized benefits and QALY would have required estimates for morbidity and mortality outcomes due to the intervention, and the review of effectiveness also found no evaluations that attempted or were able to measure health impact attributable to legislation beyond change in utilization and financial protection of the insured.13
Cost Impact on Plan Providers
Federal Employees Health Benefits Program
The Federal Employees Health Benefits (FEHB) Program is the largest employer-sponsored health insurance program in the U.S. Following executive orders, the Office of Personnel Management (OPM) instituted policies requiring that MH/SA benefits be at parity with general medical care with respect to features such as deductibles, copayments, and limits on visits and inpatient days. The first order was executed in 1967 in the pre–managed-care era and the second in 1999 when managed care had become prevalent in the health system.
Four studies of FEHB plans are included, one25 that assessed the effect of the 1967 order and three20,21,23 that evaluated effects of the 1999 order (Table 1). In general, the evidence from the FEHB studies indicates decreases in cost per covered person. The early study25 of benefits expansion from the first executive order reported an increase in cost but this occurred prior to managed care and during a period when adverse selection was a serious problem faced by the major FEHB plans.35 National estimates of weighted single and family premiums for fee for service (FFS) plans for the year 2000 was an average of $2382, the approximate mid-point of the FEHB evaluations (Table 1). Premiums for PPOs were not readily available from OPM. One study23,34 that assessed the impact on all adult enrollees and both MH and SA claims found that plan cost per person per year for MH/SA decreased in six plans (minimum of 0.06% and maximum of 1.03%) and increased in 1 plan by 0.21%, where the percentage changes are calculated with respect to weighted single and family 2000 premiums. Another study20 based on claims for MH/SA for child beneficiaries found that MH/SA cost per child (inclusive of OOP cost) increased by 0.17% in one plan and decreased in six plans, with minimum and maximum decreases of 0.14% and 0.79% respectively with reference to year 2000 premiums for family coverage weighted for number of dependents. The study showed that OOP cost per child user decreased across all 7 plans but it was not possible to obtain change in plan cost per child enrollee from the information provided. The third study21 found that SA plan cost per adult enrollee decreased by 0.013% in terms of year 2000 weighted single and family premiums.
Table 1.
Cost Impact of Benefit Expansion for Federal Employees Health Benefits (FEHB) Program
| Author, Year |
Study Design |
Data source/ Measurement Carveout? |
Benefits Expansion |
Change in Plan Cost PPPY |
Premium for Corresponding year |
Change in Plan Cost PPPY as Percentage of Insurance Premiums PPPY |
|---|---|---|---|---|---|---|
| Goldman 200623,34 | Pre-Post with Comparison | Claims for MH/SA from 1999 to those from 2002 for plan-holders and adult dependents in seven preferred provider organizations (PPO) in the FEHB program. Six plans were carved-out. |
Cost impact of the 1999 executive order | 6 plans, (−$24.50 to −$1.50) per covered person 1 plan, $5.00 per covered person |
$2,382 in year 2000a | 6 plans, (−1.03% to −0.06%) 1 plan, 0.21% |
| Azrin 200720 | Pre-Post with Comparison | Claims associated with children covered under the FEHB program and their utilization of MH/SA services in seven PPOs Six plans were carved-out. |
Cost impact of the 1999 executive order | 1 plan, $5.50 6 plans, (−$25.83 to −$4.56) per covered child (Includes OOP cost) |
$3,266 in year 2000b | 1 plan, 0.17% 6 plans, (−0.79% to −0.14%) (Includes OOP Cost) |
| Azzone 201121 | Pre-Post with Comparison | Claims for SA care only for plan-holders and adult dependents across six PPO plans Five plans were carved-out. |
Cost impact of the 1999 executive order | −$0.31 per covered person | $2,382 in year 2000a | −0.013% |
| Hustead 197825 | Pre-Post | Claims data for the two major carriers, Aetna and Blue Cross/Blue Shield (BC/BS) in 1973 No carve-out. |
First expansion of MH/SA benefits in FEHB | Not applicable | Not applicable | Not applicable |
Weighted single and family premium. Premium data obtained from FEHB-OPM for single (=$2,967) and family (=$6,466) FFS coverage. Covered persons to plan-holders ratio (=1.98) from Federal Civilian Workforce Statistics, The Fact Book 2006 Edition. Assumed 50% opt for single coverage. $2,382 = (2967*0.50+6466*0.50)/1.98
Premium data obtained from FEHB-OPM for family FFS coverage. Covered persons to plan-holders ratio (=1.98) from Federal Civilian Workforce Statistics, The Fact Book 2006 Edition. $3266 = 6466/1.98
Note: Abbreviations: FEHB, Federal Employees Health Benefits; MH/SA, mental health/substance abuse; PPPY, per person per year; SA, substance abuse.
State mandates
The federal Mental Health Parity Act of 1996 (MHPA) had limited scope, in part, because parity applied only to annual and lifetime dollar limits and did not cover SA and its treatment. Several state legislatures enacted their own stronger parity laws immediately after passage of the MHPA and thereafter, only a few of which were evaluated. Included in the economic evidence are two studies that assessed the effect of parity mandates on plan costs for the State of Oregon27 and the State of Vermont28 (Table 2). The Oregon study27 found that the increase in plan cost per person ranged from 0.23% to 0.63% of weighted single and family premiums for mixed provider coverages. The Vermont study28 found that plan cost per person increased by 0.1% in terms of percent of weighted single and family premiums for mixed provider coverage.
Table 2.
Cost Impact of State Mandates for MH/SA Benefits Expansion
| Author, Year | Study Design |
Data source/ Measurement Carveout? |
Benefits Expansion |
Change in Plan Cost PPPY |
Premium for Corresponding year |
Change in Plan Cost PPPY as Percentage of Insurance Premiums PMPY |
|---|---|---|---|---|---|---|
| McConnell 201227 | Pre-Post with Control | MH/SA claims for plan-holders and dependents from 2005 through 2008 from four PPOs. 2 of the 4 PPOs were carved-out |
Benefit expansion in State of Oregon | Increase in plan cost in the four plans ranged from $10.00 to $27.33 per covered person | $4,322 in year 2008a | (0.23% to 0.63%) |
| Rosenbach 200328 | Pre-Post | Claims from 1996 through 1999 from Blue Cross/Blue Shield of Vermont (BC/BS) for plan-holders and dependents. MH/SA was carved out. |
Benefit expansion in State of Vermont | MH costs per covered person increased by $8.52 while that for SA treatment decreased $6.20 per covered person Overall, cost for MH/SA increased by $2.32 per covered person |
$2,294 in year 1999b | 0.1% |
| Lang 201126 | Pre-Post with Control | Cost of averted suicides ascribable to state parity mandates for MH/SA benefits | States with parity mandates | $1.3–$3.1 million per suicide averted. | Not applicable | Not applicable |
Weighted single and family premium. Premiums for mixed provider private health insurance plans in State of Oregon for single (=$4,338) and family ($12,600) coverage and percentage opting for single coverage (=52.6%) obtained from MEPS-IC data. Ratio of covered persons to plan-holders (=1.91) determined from US Census-CPS data for 2008. $4,322 = (4338*52.6/100+12600*(100−52.6)/100)/1.91
Weighted single and family premium. Premiums for mixed provider private health insurance plans in State of Vermont for single (=$2,546) and family (=$6,477) coverage and percentage opting for single coverage (=50.4%) obtained from MEPS-IC data. Ratio of covered persons to plan-holders (=1.96) determined from US Census-CPS data for 2002. $2,294 = (2546*50.4/100+6477*(100−50.4)/100)/1.96
Note: Abbreviations: MH/SA, mental health/substance abuse; MH, mental health; PPPY, per person per year; PPO, preferred provider organization; SA, substance abuse; MEPS-IC, Medical Expenditure Panel Survey-Insurance Component; CPS, Current Population Survey.
Individual employers
Five studies22,24,29–33 assessed the impact on cost for individual large employers that expanded their MH/SA benefits voluntarily or in response to administrative rule (Table 3). In the case of one study,22 this review assumed the cost estimate excluded OOP cost though it was not clearly stated to be so in the study. Details whether plan-holders and dependents are included in the observed claims data and the choice of estimate for premiums used to compute the percentage change in plan cost are available within the table. Of these studies, two22,24 found that plan cost PPPY decreased (6.74% and 0.28% of premiums) and one29 found that it increased by 1.07%. Of the remaining two studies, one30 reported mixed results (0.29% in the HMO and −0.76% in indemnity plans) and the other31–33 found no change in plan cost for the employer.
Table 3.
Cost Impact of MH/SA Benefit Expansion by Individual Employers
| Author, Year |
Study Design |
Data source/ Measurement Carveout? |
Benefits Expansion | Change in Plan Cost PPPY | Premium for Corresponding year |
Change in Plan Cost PPPY as Percentage of Insurance Premiums PPPY |
|---|---|---|---|---|---|---|
| Sturm 199830 | Pre-Post | Claims for MH/SA for plan-holders and dependents from 1995–1997 to estimated costs from management reports for prior years. Plans were carved-out. |
The State of Ohio employee’s health benefits plan | For indemnity plans, the study estimated that cost per covered person covered decreased $15.20 from 1992–1993 to 1996–1997. For HMOs, which started from limited MH/SA benefits, increased from $43.92 in 1993 to $55.92 in the post 1995–1996 year and then declined to $43.68 in 1996–1997, an overall increase of $5.88 per covered person from 1993–1994 to 1996–1997 |
$2,011 in year 1996a | Indemnity plans: −0.76% HMO: 0.29% |
| Sasso 200629 | Pre-Post with Comparison | Claims for MH/SA from plan-holders only. Presence of carve-out not clear |
Voluntary expansion of MH/SA benefits in 1996 by a large Midwestern manufacturing company | The difference in difference change in cost per person from 1995 to 1998 was an increase of $21.84 | $2,034 in 1997b | 1.07% |
| Grazier 200024 | Pre-Post | Claims for MH/SA from plan-holders only from 1990 through 1993 for large corporation’s California-based employees MH/SA was carved out |
Large employer that voluntary expanded MH/SA benefits in 1991 | MH/SA cost per person decreased by $6.27 from 1990 to 1991–1993. | $2,241 in year 1996c | −0.28% |
| Cuffell 199922 | Pre-Post | MH/SA claims from 1991 through 1995 for plan-holders and dependents in PPO. MH/SA carved out |
Effect on plan cost for a large employer that expanded MH/SA benefits in 1993 | Cost per covered life per year decreased by $134.25 from 1991 to 1992–1995. (Net payment assumed to exclude OOP Cost) |
$1,993 in year 1996d | −6.74% |
| Zuvekas 2002, 200531–33 | Pre-Post with Comparison | MH/SA claims for plan-holders and dependents from 1 year pre and 3 years post expansion. MH/SA carved out. |
Large employer that had voluntarily expanded MH/SA benefits | The first two papers31,33 found a large reduction in MH/SA medical cost per person, substantially due to reduced in-patient visits and stays and the later third paper32 found that the pharmacy cost per person increased with substantially more prescriptions for psychotropics. Overall, the study found that the net effect was to leave cost per person unchanged. | $1,993 in year 1996d | 0% |
Weighted total single (=$2,306) and family (=$5,579) premium per plan-holder through state government jobs: East-North-Central Region, MEPS-IC data. Assumed 50% opted for single coverage. Ratio of covered persons to plan-holders determined from US Census-CPS data for 2002 (=1.96). $2,011 = (2306*0.5+5579*0.5)/1.96
Average total single coverage premiums (=$2,034) for mixed-provider plans per plan-holder at private sector firms with =>1K employees in 1997, MEPS-IC data.
Average total single premium (=$2,241) for mixed provider plans per plan-holder in private-sector establishments with =>1K employees that offer health insurance: State of California, MEPS-IC data.
Average total single (=$2,028) and family (=$5,059) premium for mixed-provider plans per plan-holder in firms with =>1K employees and percentage opting for single coverage (=38%), MEPS-IC data. Ratio of covered persons to plan-holders determined from US Census-CPS data for 2002 (=1.96). $1993 = (2028*38/100+5059*(100−38)/100)/1.96
Note: Abbreviations: MH/SA, mental health/substance abuse; PPPY, per person per year; SA, substance abuse; MEPS-IC, Medical Expenditure Panel Survey-Insurance Component; CPS, Current Population Survey.
Cost per averted suicide
The one study26 that reported final morbidity and mortality outcomes estimated the cost per averted suicides ascribable to state parity mandates for MH/SA benefits, where cost was drawn from increase in premiums estimated in the literature. The study estimated that these mandates averted 592 suicides per year nationwide, at a cost of $1.3–$3.1 million per suicide averted.
Summary of Results
There were no studies of MH/SA benefits expansion that reported cost per QALY saved or cost-benefit outcomes. Hence, there was insufficient information to determine whether the interventions were cost-effective or cost-beneficial.
Ten of the eleven studies that evaluated cost impact on health plans were based on data from 1996 onwards, three of which showed decreases in plan cost PPPY while two showed decreases in 6 of the 7 plans they considered. There was no change in cost PPPY for one study while it was mixed (0.29% and −0.76%) in another. Of the three remaining studies, two showed an increase in cost PPPY to be 0.63% or less, and the other an increase of 1.07%, respectively. The evidence from economic evaluation studies indicates that MH/SA benefits expansion did not lead to any substantial increase in cost to health insurance plans, measured as a percentage of premiums.
Discussion
During the period covered in this review, arguments were made for and against parity for MH/SA benefits in the US and the latter included the possibility that plans would face formidable increases in cost. Modeling exercises were conducted in the 1990s, under the aegis of the Congressional Budget office (CBO) and the National Advisory Mental Health Council (NAMHC), to predict the expected cost increases following the expansion of MH/SA benefits towards parity. The history of their predictions is traced36 from the initial estimated increase in premiums of 4.0% predicted to follow the Mental Health Parity Act (MHPA) of 1996 to the lower 3.6% increase predicted from actuarial-economic models and observed experience in 1998. Further evidence from the FEHB experience and several large behavioral carve-outs were then used to calibrate the actuarial-economic model and the impact was further revised downward to a 1.4% increase in premiums.36 The models predicted smaller increases in premiums as a result of incorporating the effects of managed care activities on treatments and the smaller estimates of MH/SA demand elasticity in managed care settings.
With all but one estimated increase below 1% and many plans showing actual decreases in cost PPPY, the evidence from this systematic review indicates that costs are likely to increase far less than the predictions made during and around the time of the MHPA federal law of 1996. In fact, the findings of this review are consistent with the CBO prediction that the MHPAEA of 2008 would result in a 0.4% increase in premiums.37,38 A recent historical review of the processes that led to the MHPAEA of 2008 ascribed the success of its passage partly to data showing there was little to no effect on plan costs due to earlier parity or other benefit expansion.39 The present study echoes the observation with evidence based on a systematic review.
The much smaller increase in cost, if any, observed in the parity studies compared to the predictions from earlier actuarial models merits additional comment. A key difference is that the early actuarial models were based on experience and data that were not moderated by managed care practices while these practices were very much in play within the plans analyzed in the parity studies included in this review. Further, effective pharmacotherapy and its increased use in treatment of MH/SA likely also confounded the pathway from benefits expansion to cost of utilization. In the case of the FEHB, OPM actually encouraged the use of managed care to control cost and all but one of the plans included in the FEHB studies were carved-out to managed behavioral health organizations (MBHOs). As shown in column 3 of tables 2 and 3, carve-outs were also the dominant organization that managed MH/SA in the State and large employer parity studies.
The study26 on state suicide rates is the only study in this body of evidence to provide a cost per unit of health outcome ascribable to MH/SA benefits expansion. Future economic research needs to allow more adequately for concurrent effects of general and medical care inflation on cost, innovations in pharmaceuticals, changes in prescription patterns, and secular trends in the diagnosis and treatment of mental illnesses and SA. Very few studies evaluated the more downstream effects on business decisions about labor, such as effects on hiring, retention, and the offer of health benefits as part of a compensation package. This gap is noted considering that about 60% of the U.S. non-elderly insured have employer-sponsored insurance and laws apply differently across employers of different sizes, as was the case for the federal laws and state mandates included in both the effectiveness review13 and this economic review. One other limitation of the review is that the included studies only considered claims coded for mental health and do not account for physical health claims that may have had an underlying mental health condition. Such patients may have more readily sought appropriate mental health care with the advent of parity.
U.S. Implications for MH/SA Care Provision and Use
Policies on MH/SA benefits in health insurance evolved through a long history of laws and rules at the US federal level, numerous mandates at the state level, and voluntary expansions by large self-insured employers. MH/SA benefits legislation at the federal level culminated in the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA),38 as amended by the Health Care and Education Reconciliation Act of 2010 (commonly jointly referred to as the Affordable Care Act, or ACA). MHPAEA38 extended parity requirements to mental health and substance use disorder benefits provided by plans in the large group health insurance market, applicable to financial requirements such as co-pays and deductibles, and to treatment limitations such as limits on outpatient and inpatient visits.40 The ACA added mental health and substance use disorder protections in addition to those enacted under MHPAEA by requiring that certain plans offer minimum mental health/substance use disorder benefits, including behavioral health treatment, as one of the essential health benefit categories,41 generally expanding the population with health care coverage,42 and eliminating pre-existing condition clauses from most plans.43 The ACA also enhanced Medicaid coverage options for serious and persistent mental illness and applied MHPAEA and essential health benefit requirements to Medicaid alternative benefit plans.44 The likely effect of these changes on the mental health and substance abuse costs of different health insurance plans is the subject of future research.45
Acknowledgements
The authors thank the following members of the Community Guide Branch at CDC: Randy W. Elder, David P. Hopkins, Andrea Baeder, Kate W. Harris, and Onnalee Gomez. The authors also wish to thank Rebecca Kander from the US Office of Personnel Management for assistance obtaining historical estimates for FEHB premium. Comments and suggestions from an anonymous referee were instrumental in improving methods and interpretation. Finally, we acknowledge Task Force member, Ned Calonge, for alerting us to the issue of mental health conditions that present as physical complaints in visits to general practice.
Footnotes
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry.
Contributor Information
Verughese Jacob, Centers for Disease Control and Prevention (CDC).
Shuli Qu, Centers for Disease Control and Prevention (CDC).
Sajal Chattopadhyay, Centers for Disease Control and Prevention (CDC).
Theresa Ann Sipe, Centers for Disease Control and Prevention (CDC).
John A. Knopf, Centers for Disease Control and Prevention (CDC).
Ron Z. Goetzel, Johns Hopkins Bloomberg School of Public Health and Vice President, Truven Health Analytics.
Ramona Finnie, Centers for Disease Control and Prevention (CDC).
Anilkrishna B. Thota, Centers for Disease Control and Prevention (CDC).
References
- 1.Buck JA, Umland B. Covering mental health and substance abuse services. Health Affairs. 1997;16(4):120–126. doi: 10.1377/hlthaff.16.4.120. [DOI] [PubMed] [Google Scholar]
- 2.Jensen GA, Rost K, Burton RP, Bulycheva M. Mental health insurance in the 1990s: are employers offering less to more. Health Affairs. 1998;17(3):201–208. doi: 10.1377/hlthaff.17.3.201. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services. Mental health: A report of the Surgeon General. Rockville, MD: National Institute of Mental Health; 1999. [Google Scholar]
- 4.Frank RG, Koyanagi C, McGuire TG. The politics and economics of mental health 'parity' laws. Health Affairs. 1997;16(4):108–119. doi: 10.1377/hlthaff.16.4.108. [DOI] [PubMed] [Google Scholar]
- 5.Sing M, Hill S, Smolkin S, Heiser N. The costs and effects of parity for mental health and substance abuse insurance benefits. US Department of Health and Human Services, Public Health Service, Substance Abuse and Mental Health Services Administration; 1998. [Google Scholar]
- 6.Manning WG, Wells KB, Buchanan J, Keeler EB, Valdez ROB, Newhouse JP. Effects of mental health insurance: Evidence from the Health Insurance Experiment. A RAND Corporation Report. 1989 http://www.rand.org/pubs/reports/R3815.html. [Google Scholar]
- 7.Propper V, Pomiecko GL. Parity for Mental Health: History and Consequences [Google Scholar]
- 8.NCSL. State Laws Mandating or Regulating Mental Health Benefits. 2004 [Google Scholar]
- 9.Bailey S. EPA-1080–Parity: from rhetoric to reality; future proofing society through mental health. European Psychiatry. 2014;29:1. [Google Scholar]
- 10.World Health Organization. The European Mental Health Action Plan. Çeşme Izmir, Turkey: World Health Organization; 2013. [Google Scholar]
- 11.Knapp M, McDaid D, Mossialos E, Thornicroft G. Mental health policy and practice across Europe. The future direction of mental health care. Open University Press; 2007. [Google Scholar]
- 12.Nussbaum MC. Capabilities as fundamental entitlements: Sen and social justice. Feminist Economics. 2003;9(2–3):33–59. [Google Scholar]
- 13.Sipe TA, Finnie RKC, Knopf JA, et al. The role of mental health benefits legislation in improving mental health: A Community Guide systematic review. In prep. [Google Scholar]
- 14.World Bank. 2014 data.worldbank.org/about/country-classifications/country-and-lending-groups#High_income. [Google Scholar]
- 15.Newsom M, Fernandez B. Private health insurance premiums and rate reviews. 2011 http://digitalcommons.ilr.cornell.edu/cgi/viewcontent.cgi?article=1793&context=key_workplace. [Google Scholar]
- 16.Klugman SA, editor. Understanding actuarial practice. Society of Actuaries; 2012. https://www.soa.org/books/. [Google Scholar]
- 17.Federal civilian workforce statistics: The Fact Book. Washington, DC: U.S Office of Personnel Management; 2006. U.S. Office of Personnel Management. [Google Scholar]
- 18.Medical Expenditure Panel Survey - Insurance Component. [Accessed November 21, 2014];Agency for Healthcare Research and Quality. http://meps.ahrq.gov/mepsweb/survey_comp/Insurance.jsp. [PubMed]
- 19.U.S Census Bureau; [Accessed October 25, 2014]. Current population survey - health insurance coverage. http://www.census.gov/cps/data. [Google Scholar]
- 20.Azrin ST, Huskamp HA, Azzone V, et al. Impact of full mental health and substance abuse parity for children in the Federal Employees Health Benefits program. Pediatrics. 2007;119(2):e452. doi: 10.1542/peds.2006-0673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Azzone V, Frank RG, Normand SLT, Udrey Burnam M. Effect of insurance parity on substance abuse treatment. Psychiatr Serv. 2011;62(2):129–134. doi: 10.1176/appi.ps.62.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cuffel BJ, Goldman W, Schlesinger H. Does managing behavioral health care services increase the cost of providing medical care? J Behav Health Services Res. 1999;26(4):372. doi: 10.1007/BF02287298. [DOI] [PubMed] [Google Scholar]
- 23.Goldman HH, Frank RG, Burnam MA, et al. Behavioral health insurance parity for federal employees. N Engl J Med. 2006;354(13):1378–1386. doi: 10.1056/NEJMsa053737. [DOI] [PubMed] [Google Scholar]
- 24.Grazier KL, Pollack H. Translating behavioral health services research into benefits policy. Med Care Res Rev. 2000;57(2S):53–71. doi: 10.1177/1077558700057002S04. [DOI] [PubMed] [Google Scholar]
- 25.Hustead EC, Sharfstein SS. Utilization and cost of mental illness coverage in the Federal Employees Health Benefits Program, 1973. Am J Psychiatry. 1978;135(3):315–319. doi: 10.1176/ajp.135.3.315. [DOI] [PubMed] [Google Scholar]
- 26.Lang M. The impact of mental health insurance laws on state suicide rates. Health Econ. 2013;22(1):73–88. doi: 10.1002/hec.1816. [DOI] [PubMed] [Google Scholar]
- 27.McConnell KJ, Gast SH, Ridgely MS, et al. Behavioral health insurance parity: Does Oregon's experience presage the national experience with the Mental Health Parity and Addiction Equity Act? Am J Psychiatry. 2012;169(1):31–38. doi: 10.1176/appi.ajp.2011.11020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosenbach M, Lake T, Young C, et al. Effects of the Vermont mental health and substance abuse parity law. DHHS Pub. No. (SMA) 03-3822. Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; 2003. [Google Scholar]
- 29.Sasso AT, Lurie IZ, Lee JU, Lindrooth RC. The effects of expanded mental health benefits on treatment costs. J Ment Health Policy Econ. 2006;9(1):25–33. [PubMed] [Google Scholar]
- 30.Sturm R, Goldman W, McCulloch J. Mental health and substance abuse parity: A case study of Ohio's state employee program. J Ment Health Policy Econ. 1998;1(3):129–134. doi: 10.1002/(sici)1099-176x(1998100)1:3<129::aid-mhp16>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 31.Zuvekas SH, Regier DA, Rae DS, Rupp A, Narrow WE. The impacts of mental health parity and managed care in one large employer group. Health Affairs. 2002;21(3):148–159. doi: 10.1377/hlthaff.21.3.148. [DOI] [PubMed] [Google Scholar]
- 32.Zuvekas SH, Rupp AE, Norquist GS. Spillover effects of benefit expansions and carve-outs on psychotropic medication use and costs. Inquiry. 2005;42(1):86–97. doi: 10.5034/inquiryjrnl_42.1.86. [DOI] [PubMed] [Google Scholar]
- 33.Zuvekas SH, Rupp AE, Norquist GS. The impacts of mental health parity and managed care in one large employer group: A reexamination. Health Affairs. 2005;24(6):1668–1671. doi: 10.1377/hlthaff.24.6.1668. [DOI] [PubMed] [Google Scholar]
- 34.U.S. Department of Health and Human Services. Evaluation of parity in the Federal Employees Health Benefits (FEHB) program: Final Report. 2004 Dec; http://aspe.hhs.gov/daltcp/reports/parity.pdf.
- 35.Francis W. Putting Medicare consumers in charge: Lessons from the FEHBP. AEI studies on Medicare reform. Washington, DC: AEI Press; 2009. [Google Scholar]
- 36.Kirschstein RL. Insurance parity for mental health: cost, access, and quality. Final Report to Congress by the National Advisory Mental Health Council, 2000. 2000 http://www.nimh.nih.gov/about/advisory-boards-and-groups/namhc/reports/nimh-parity.pdf.
- 37.Mark TL, Levit KR, Vandivort-Warren R, Buck JA, Coffey RM. Changes in US spending on mental health and substance abuse treatment, 1986–2005, and implications for policy. Health Affairs. 2011;30(2):284–292. doi: 10.1377/hlthaff.2010.0765. [DOI] [PubMed] [Google Scholar]
- 38.Wellstone P, Domenici P. Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 (H.R. 1424) 2008:117. http://www.gpo.gov/fdsys/pkg/BILLS-110hr1424enr/pdf/BILLS-110hr1424enr.pdf.
- 39.Barry CL, Huskamp HA, Goldman HH. A political history of federal mental health and addiction insurance parity. Milbank Q. 2010;88(3):404–433. doi: 10.1111/j.1468-0009.2010.00605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.U.S. Department of Labor. Fact sheet: The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) 2010 http://www.dol.gov/ebsa/newsroom/fsmhpaea.html.
- 41.Compilation of Patient Protection and Affordable Care Act, section 1302. 2010:59. http://housedocs.house.gov/energycommerce/ppacacon.pdf.
- 42.Compilation of Patient Protection and Affordable Care Act (expanding options for coverage through Exchanges and Medicaid expansions) 2010 http://housedocs.house.gov/energycommerce/ppacacon.pdf.
- 43.Compilation of Patient Protection and Affordable Care Act, section 1201. 2010 http://housedocs.house.gov/energycommerce/ppacacon.pdf.
- 44.Compilation of Patient Protection and Affordable Care Act, section 2001(c) 2010:184. http://housedocs.house.gov/energycommerce/ppacacon.pdf.
- 45.Sarata AK. Mental health parity and the Patient Protection and Affordable Care Act of 2010. Congressional Research Service Report for Congress. 2011 http://www.ncsl.org/documents/health/MHparity&mandates.pdf. [Google Scholar]