Abstract:
Blood cross-matched for patients undergoing cardiac surgery is used infrequently and represents a significant cost. We investigated the ability to predict the need for intraoperative transfusion. We hypothesized that red blood cell volume is a predictor because dilution is the primary cause for transfusion requirement intraoperatively. A total of 401 consecutive patients having cardiothoracic surgery requiring the use of cardiopulmonary bypass were retrospectively analyzed by revision of their perfusion record. This sample included 82% elective, 17% urgent, and 1% emergency procedures. The product of body surface area and preoperative hemoglobin gave us gHb/l/m2, which are the units of the Transfusion Predictor Product (TPPu). Mean patient age was 66.9 ± 10.7 years, and 112 (28%) were women. Mean TPP was 257.2 ± 45.5u. 52 patients (13%) received red blood cells intraoperatively. At less than TPP 211.7u, one standard deviation below the mean value, 32 patients of 69 (46%) received blood transfusion intraoperatively (p < 0.001). At a TPP greater than 211.7u, 20 patients of 322 (6%) had blood transfusion intraoperatively. Patients with a TPP > 211.7u do not require routine cross-matching of blood. Cross-matching for these patients should be individualized on the basis of predicted duration of CPB and/or other types of patient comorbidity.
Keywords: predicting blood usage cardiac surgery
Most patients presenting for cardiac surgery requiring cardiopulmonary bypass routinely have two or more units of blood cross-matched before the surgery. Most of these patients will not require this blood during its “cross-match life” (3 to 4 days from cross-match). We hypothesize that for most of the patients that require blood transfusion intraoperatively, the need arises slowly with gradual dilution. The blood can be obtained safely at that time and be available in 5 to 10 minutes if previous blood grouping and screening for major antibodies has been done.
Cross-matching blood has both a financial cost and a resource cost. Grouping and screening for major antibodies only costs 36% of full group, screen, and cross-match (Aus$41.65 vs Aus$113.40) (1). A chronically underresourced blood pool is further limited by the small, but nonetheless significant, waste of blood set aside for individual patients.
Models for predicting transfusion requirements in cardiac surgical patients have been available for many years (2–5). They generally have been complex and required multivariate computations. Predictive factors have included operative procedure, surgeon, age, sex, height, weight, hematocrit, the presence or absence of diabetes, and albumin levels. Our goal was to find a simple equation that could be easily calculated on admission. This preoperative predictor of the need for transfusion may decrease the necessity to cross-match blood.
The primary cause of blood requirement in the operating theater is hemodilution. Hemodilution can be described as primary and secondary. The volume of diluent given before cardiopulmonary bypass (CPB) by the anesthetist and the prime of the heart lung machine are reasonably constant and predictable. This is the primary dilution that all patients in this study received. Volume given during bypass is relatively dependent on the duration of bypass, which is frequently not predictable. This is the secondary dilution.
It is hypothesized that the main predictor of blood usage is the patient’s total circulating red blood cell (RBC) volume. This volume is what the dilution load, both primary and secondary, will affect. The hemoglobin and the hematocrit frequently are used as the triggers for blood transfusion.
BSA (m2) multiplied by preoperative hemoglobin (g/l) gives us a numerical product we called the Transfusion Predictor Product (TPPu) (gHb/l/m2). The TPP estimates circulating RBC volume and can be used to predict RBC requirements during cardiac surgery. We hypothesize that the TPP could be used as an accurate predictor for blood requirement caused by primary dilution during cardiac surgery requiring CPB. TPP can be easily calculated after the patients’ admission to hospital and a decision about cross matching made.
MATERIALS AND METHODS
All 401 consecutive patients having cardiac surgery requiring CPB in one cardiothoracic surgical unit at the Monash Medical Centre during one calendar year were retrospectively analyzed by review of their perfusion record. Institutional approval was sought but deemed unnecessary. This sample included 82% elective, 17% urgent, and 1% emergency procedures, and there were no exclusions. All patients were adults. There were no deaths in the operating theater. Procedures are listed in Table 1. Six surgeons, six anesthesiologists, and five perfusionists were involved in these procedures.
Table 1.
Procedures.
| Procedure | Number |
|---|---|
| Coronary artery bypass grafts (CABGS) 71% | 285 |
| Aortic valve replacement (AVR) 9.5% | 38 |
| CABGS and AVR 6.2% | 25 |
| Mitral valve repair (MVRep) 3.0% | 12 |
| Mitral valve replacement (MVR) 2.5% | 10 |
| Miscellaneous 7.7% | 31 |
| (i.e., CABGS and MVRep (6), CABGS and MVR (4), AVR and ascending aorta (4), ASD (2), AVR and MVR and CABGS (2), AVR and MVR (2), CABGS and aortic dissection (1), Ross procedure (1), AVR and MVR and TVR (1), aortic valve repair and CABGS (1), Bentall procedure (1), CABGS and ascending aorta (1), CABGS and VSD (1), HOCM repair (1), Left atrial myxoma (1), Left ventricular aneurysm (1), MVR and TVRep (1) |
HOCM, hypertrophic obstructive cardiac myopathy; TVR, tricuspid valve replacement; TVRep, tricuspid valve repair; VSD, ventricular septal defect.
The accurate preoperative measurement of circulating blood volume is difficult. An estimation of circulating volume can be made through calculation of body surface area (BSA), which is determined from the Dubois body surface area nomogram, multiplied by 2.4. In general, a larger patient will have a larger circulating volume. Total circulating RBC volume can be calculated from circulating blood volume multiplied by hematocrit. The preoperative hematocrit is not recorded routinely in our practice; however, pre-operative hemoglobin is.
The BSA and preoperative Hb were obtained from the perfusion record, and TPP calculated (BSA × Hb = TPP). Blood usage data were obtained from the perfusion record and hematology department records. Unless otherwise noted, results are listed as mean ± standard deviation. Statistical methodology included binary logistic regression and one-way analysis of variance.
RESULTS
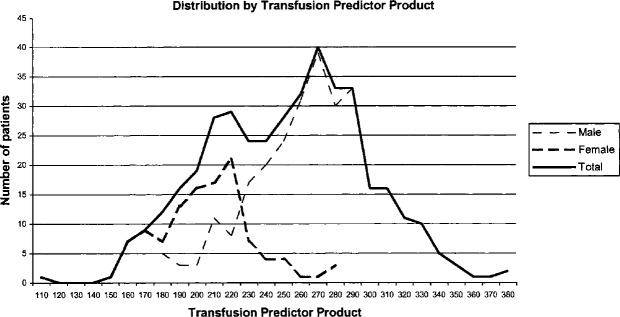
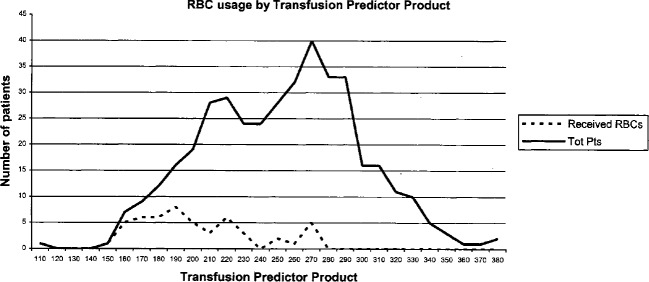
Patient demographics are listed in Table 2. The distribution of TPP for both male and female patients was unimodal and do not appear to be normally distributed (Figure 1). A bimodal distribution related to the graph for all patients is noted. A total of 52 patients (13%) received RBCs during surgery (Figure 2).
Table 2.
Patient demographics.
| Male | Female | Total Sample | |
|---|---|---|---|
| Age | 65.9 ± 10.0 y | 69.4 ± 11.9 y | 66.9 ± 10.7 y |
| Sex | 289 (72.1%) | 112 (27.9%) | 401 |
| BSA (m2) | 1.95 ± 0.16 | 1.64 ± 0.13 | 1.87 ± 0.21 |
| Hb pre-op (g/L) | 141 ± 13 | 128 ± 13 | 137 ± 15 |
| TPP (u) | 275.4 ± 37.0 | 210.1 ± 28.4 | 257.2 ± 45.5 |
| Primary dilution volume (mL) | 2660 ± 463 | 2387 ± 363 | 2584 ± 453 |
| Secondary dilution volume (mL) | 1973 ± 1063 | 1678 ± 1066 | 1887 ± 1077 |
| Received RBCs in OR (%) | 16 (5.5%) | 36 (32%) | 52 (13%) |
| Average transfusion in units | 2.6 ± 1.4 | 2 ± 0.8 | 2.2 ± 1.1 |
OR, operating room.
Figure 1.
Patient distribution by TPP.
Figure 2.
Blood usage by TPP.
Intraoperative blood usage is highly dependent upon TPP (p < 0.001). Similarly, intraoperative blood usage is highly dependent upon duration of CPB (p < 0.001). A TPP of 211.7u is one standard deviation less than the mean. Distribution for blood requirement caused by primary dilution appears to end in approximately this area. We arbitrarily chose this point, a TPP of 211.7u, as our point of review. At measurements greater than this TPP, the requirement for blood is the result of secondary dilution.
A total of 52 patients (13%) required RBC transfusion intraoperatively. Of these, 32 patients had a low TPP (TPP < than 211.7u) and 20 had a high TPP (TPP > than 211.7u). This represents 46.4% and 6% of these respective groups. Of the 69 patients with a low TPP, 32 received blood during surgery (46.4%). All received their first transfusion after institution of CPB, that is, after the primary dilution. On no occasion was blood placed in the prime. Time between start of CPB and first transfusion was 67 ± 60 minutes. Primary dilution volume was 2490 ± 415 mL.
Twenty of the remaining 332 patients (6%) with a TPP of greater than 211.7u received blood during surgery. Time between start of CPB and first transfusion was 95 ± 74.5 minutes. The CPB time for this group of 20 patients was 165 ± 66 minutes, with only one patient having a CPB time of less than 100 minutes (59 minutes). Primary dilution volume was 2825 ± 629 mL. Secondary dilution volume was 2365 ± 1249 mL. This group of 20 patients was further stratified into groups having a long CPB time (>120 minutes) and a short CPB time (≥ 120 minutes; Table 3).
Table 3.
Patients with TPP greater than 211.7u who received a blood transfusion.
| CPB ≤ 120′ | CPB > 120′ | |
|---|---|---|
| CPB time (mins) | 104.8 ± 22.9 | 190.8 ± 61.9 |
| Number of patients | 6 | 14 |
| Females:males | 6:0 | 6:8 |
| Age (years) | 78.7 ± 6.8 | 72.4 ± 7.6 |
| TTP (u) | 223.6 ± 6.3 | 248.6 ± 22.6 |
| Unstable | 2 | 4 |
| Reoperation | 0 | 2 |
| Unstable reoperation | 0 | 4 |
| Time from anesthesia induction to transfusion (min) | 159.5 ± 38.1 | 227.4 ± 73.0 |
| Time from CPB start to transfusion (min) | 54.8 ± 21 | 112.5 ± 82.9 |
This group of 20 patients included six reoperations, five combined valve and CABG operations, and 10 urgent procedures (there is overlap amongst these groups). The five patients who didn’t fit into the above categories included four females with a mean age of 74.2 years. One patient was on bypass for 365 minutes (TPP 262.2u) and was transferred to the intensive care unit on extra corporeal life support and intra-aortic balloon pump support (he was successfully weaned from extra corporeal life support and intra-aortic balloon pump at postoperative day 7). Another patient spent 295 minutes on CPB (TPP 273.6u) after his right ventricle (RV) was ruptured during reoperative sternotomy. Twelve women (60%) comprised this group of 20.
All 20 patients with a TPP greater than 211.7u, who received blood during surgery received it electively during CPB to optimize hematocrit. In all cases there was sufficient time to have the blood cross-matched once it was needed. No blood was required urgently, including for the ruptured RV.
Patients transfused with a TPP of greater than 211.7u and a CPB time less than 120 minutes were all female with a mean age of 78.7 years. Their blood transfusion was caused by both primary dilution and a lower threshold of transfusion because of their age. The largest TPP in this group was 231.2u. Five of this group required no further blood during their hospital stay. The largest transfusion was two units.
Patients transfused with a TPP of greater than 211.7u and a CPB time more than 120 minutes were clearly transfused because of secondary dilution. Time between start of CPB and first transfusion was 113 ± 83 minutes. The CPB time for this group was 191 ± 62 minutes. Secondary dilution volume was 2879 ± 999cc.
Of the 52 patients transfused during surgery, 30 (58%) were further transfused in ICU. A further 111 patients (28%) not transfused during surgery received blood in the first 2 postoperative days. A total of 61% of all patients did not receive blood either intraoperatively or postoperatively. Many factors determine blood requirement in the post-operative phase. These include hemoglobin at the end of surgery, post-operative blood loss, availability of blood, and physician determination. Blood was not required urgently in the ICU. Blood was electively transfused to optimize hemoglobin to levels greater than 10 g/L.
DISCUSSION
Despite the obvious limitation of the retrospective nature of this study and that it was performed in a single surgical unit, we believe that the TPP is an accurate predictor of intraoperative blood requirement for primary dilution of patients undergoing cardiac surgery requiring CPB. Only 14% of all patients presenting for cardiac surgery, those with a TPP less than 211.7u, need to have blood cross-matched preoperatively. This group can be selected, on admission, from their BSA and preoperative Hb. This selection will save time, money, and resources within the hematology department while maintaining patient safety. An argument could be made to add female patients older than 70 years of age with a TPP of up to 235 to this group. A further 5% will need blood whilst in the OR but this can be safely obtained as the need arises. Further provision of blood would be required in the ICU and an algorithm for predicting this is currently being worked on by this group.
REFERENCES
- 1.Australian Government Department of Health and Ageing. Medicare? Benefits Schedule Book, 2004: 552, items 65096 & 65099. [Google Scholar]
- 2.Magovern J, Sakert T, Benckart D, et al. . A model for predicting transfusion after coronary artery bypass grafting. Ann Thorac Surg. 1996;61:27–32. [DOI] [PubMed] [Google Scholar]
- 3.Moskowitz D, Klein J, Shander A, et al. . Predictors of transfusion requirements for cardiac surgical procedures at a blood conservation center. Ann Thorac Surg. 2004;77:626–34. [DOI] [PubMed] [Google Scholar]
- 4.Parr K, Patel M, Dekker R, et al. . Multivariate predictors of blood product use in cardiac surgery. J Cardioth Vasc Anesth. 2003;17:176–81. [DOI] [PubMed] [Google Scholar]
- 5.Karkouti K, Cohen M, McCluskey S, et al. . A multivariable model for predicting the need for blood transfusion in patients undergoing first-time elective coronary bypass graft surgery. Transfusion. 2001;41:1193–203. [DOI] [PubMed] [Google Scholar]