Abstract
We explored the concept of using a Mindfulness-based intervention to reduce perinatal grief among Indian women. Data were collected using mixed methods to explore concept acceptability, receptivity, modality, and feasibility of the intervention. The intervention was piloted and evaluated with measures of perinatal grief, psychosocial wellbeing, religious coping, perceived social provision of support, and mindfulness. The intervention was well received and effective in teaching skills to help women deal with high levels of grief and subsequent mental health challenges. To overcome attendance barriers modification is necessary. Partnership with a local nursing school is critical to enhance sustainability of the intervention.
INTRODUCTION
Perinatal grief following stillbirth is recognized in the literature as a phenomenon characterized by active grief, difficulty coping, and despair due to the great social and psychological impact of perinatal loss (Barr & Cacciatore, 2007; Toedter, Lasker, & Janssen, 2001). Perinatal grief is a unique type of grief due to the experience of the anticipation of birth thwarted at the very moment due to perinatal loss (Kelly, 2007; Rowland & Goodnight, 2009). However, in India, where stillbirth is common, literature regarding women’s perceptions of the stillbirth experience is very limited. Yet, India is one of five countries contributing to half of the 3.2 million stillbirths annually occurring in low and middle-income countries (Bhati, 2014). The vast majority of stillbirths occurring in these settings are intrapartum, resulting from fetal distress and/or obstructed labor (Kramer et al., 2002), when the loss is most devastating (Mehta & Verma, 1990) and can lead to ‘pathologic grief’.
Pathologic grief has been described as a complicated intensification of grief (Horowitz, Bonanno, & Holen, 1993), which may result from maladaptive coping skills, low social support, and intense emotionality immediately following the loss (Bennett, Litz, Maguen, & Ehrenreich, 2008). Anxiety and depression may follow for years to come (Boyle, Vance, Najman, & Thearle, 1996). The psychological burden resulting from stillbirth has significant social impact (Sather, Fajon, Zaentz, & Rubens, 2010).
Our previous study found significantly elevated levels of perinatal grief among women in central, rural India (Roberts, Montgomery, Lee, & Anderson, 2012) and resultant suffering (Roberts, Anderson, Lee, & Montgomery, 2012). Factors that contribute to perinatal grief for women in this setting include traditional social norms, and perceived lack of social support (Roberts, Montgomery et al., 2012). In light of these study results, we realized a critical need for an intervention to help the women better cope with their enormous grief that could only be implemented if it was placed within their social normative context (Roberts, Anderson et al., 2012). As a next step, this data was used to guide the subsequent development of a culturally rooted intervention designed to positively impact their ability to cope, utilizing ‘Mindfulness modalities’.
Mindfulness-based stress reduction (MBSR) is an empirically-supported intervention that has been shown to result in an increased functional quality of life: improved emotional balance and coping with distress (Ludwig & Kabat-Zinn, 2008); decreased state and trait anxiety, depression (Shapiro, Schwartz, & Bonner, 1998) and total mood disturbance (Krasner et al., 2009); improved emotional regulation and increased self-insight (Davis & Hayes, 2011); and restored balance between affective and sensory neural networks (Farb et al., 2010). A meta-analysis of 20 studies utilizing MBSR, done by Grossman, Niemann, Schmidt, and Walach (2004) indicated an overall effect size of 0.5 (p < 0.0001), and suggested that MBSR may be helpful to individuals to cope with both clinical and non-clinical problems. Five facets of Mindfulness are represented in MBSR: observing, describing, acting with awareness, non-judging of inner experience, and non-reacting to inner experience. Most simply stated, Mindfulness is defined as ‘moment-to-moment awareness of one’s experience without judgment,’ which is a state of being rather than a character trait (Davis & Hayes, 2011, p. 198). As such, it can be cultivated with practice.
MBSR harnesses the power of the mind–body connection that is so often ignored in daily living (Kabat-Zinn, 2009). Recent evidence supports neuroplastic changes in the brain as a result of Mindfulness practice (Hölzel et al., 2011). The mind–body connection is an ancient concept that has been revisited by scientists over the past few decades and is now recognized as a bidirectional interaction between the brain and body through autonomic and neuroendocrine pathways. Therefore, the mind–body connection influences both mental and physical health (Taylor, Goehler, Galper, Innes, & Bourguignon, 2010). Moreover, mind–body connection is also an integral premise of Ayurveda, the traditional medical practice of India (Miller, 2013).
This paper presents a pilot study that aimed to explore the feasibility, acceptance, and cultural fit of a brief Mindfulness-based intervention to reduce perinatal grief among poor, rural, central Indian women who have experienced stillbirth. To the best of our knowledge, no prior studies using MBSR or studies to reduce perinatal grief, have been conducted in central, rural, India, where women are highly isolated in their traditional roles.
METHODS
A total of 10 key informant interviews were conducted by the principal investigator, with the help of gender- and culturally-matched research staff. Triangulation of key informant interviews were used to assure multiple relevant perspectives and convergent validation (Berg, 2009), specifically: women of reproductive age who have experienced stillbirth, family members living in the hospital catchment area, and hospital staff who identify themselves as concerned with perinatal grief. A semi-structured interview outline was used to assure consistent exploration of concept acceptability, receptivity, modality, and feasibility of the intervention in this setting, while allowing descriptive exploration (Corbin & Strauss, 2008). A validation focus group was conducted with the assistance of trained research staff (a culturally and gender-matched moderator and co-moderator). The focus group consisted of six women from the hospital catchment area, representing local women of child-bearing age who had experienced stillbirth. Two women were reimbursed for bus fare, the rest of the women had arrived by walking, bullock cart or were already at the hospital for other reasons. All participants were given a small gift to thank them for their time. All interviews were conducted by a trained qualitative interviewer, with the help of gender- and culturally-matched translators for Hindi or Chhattisgarhi, the local dialect. All interviews were audiotaped and transcribed verbatim. Informed consent, as well as pre- and post-tests for the pilot intervention were written in both English and Hindi, translated by a bilingual committee. Independent forward and backward translation was completed, ensuring cultural and functional equivalence, which is of utmost importance (Jones, Lee, Phillips, Zhang, & Jaceldo, 2001), rather than simply literal translation. Verbal translation from Hindi to Chhattisgarhi was employed as needed. The data collected from the interviews were used in the development of the pilot intervention pre- and post-tests and for minor adjustments to the treatment protocol.
None of the women who participated in the qualitative phase of the study participated in the pilot intervention. Hospital staff referred three women who had experienced stillbirth within the last year, who agreed to participate in the pilot intervention. Additional participants were then recruited using snowball sampling techniques (Berg, 2009). A total of 22 women attended the two-session pilot intervention. Given the restricted nature of the women’s lives to engage in activities outside the home, the two-session modality was chosen for this pilot to test Mindfulness concept acceptability and feasibility of MBSR. The basic constructs of MBSR were condensed and introduced over two lengthy sessions, with the intent to deliver the full MBSR intervention in the future if indeed Mindfulness was a good fit and its delivery found to be feasible.
Measures
At baseline, demographics and questions pertaining to obstetric and general medical history as well as autonomy and perinatal grief were included. Pre- and post-tests included measures of psychosocial wellbeing, religious coping, perceived social provision of support and Mindfulness attributes.
To assess feasibility and acceptability of the intervention and study protocol, we recorded participant attendance at intervention sessions or reasons for a missed session. The post-intervention questionnaire provided additional data regarding the acceptability of the program. This questionnaire consisted of a 12-item program evaluation regarding suitability of intervention content, concepts, and feasibility, as well as perceived helpfulness of the intervention. Each item was rated on a Likert-type scale, ranging from (1) strongly disagree, to (5) strongly agree. Additionally, participants were asked a dichotomous question regarding practice of Mindfulness skills between sessions one and two, and if they answered positively, additional information was elicited regarding specific Mindfulness-based skills they had been practicing. Finally, participants were asked for their preferences of the time of year for the intervention with regards to major holidays and harvest seasons.
The following validated scales were used for pre/post-test data collection.
Hopkins Symptoms Check List – 10 (HSCL-10)
The HSCL-10 was translated into Urdu and performed well among a sample of poor, rural Pakistanis with low education levels (Syed, Zachrisson, Dalgard, Dalen, & Ahlberg, 2008), therefore, it was chosen for use among this population who share some similarities with the Syed et al. (2008) sample. The measure’s 10 items are rated on a Likert-type scale ranging from (1) not at all to (4) extremely, with higher scores representing more symptoms of anxiety and depression (Cronbach’s alpha = 0.84).
Satisfaction with Life Scale (SWLS)
Life satisfaction was measured using the 5-item SWLS with items rated on a Likert-type scale ranging from (1) strongly disagree to (7) strongly agree (Diener, Emmons, Larsen, & Griffin, 1985). The resulting summed scores range from 5 to 35, with higher scores representing greater satisfaction with life (Cronbach’s alpha = 0.68). The SWLS is easily understood by respondents and is applicable in divergent life situations and countries (Diener, Inglehart, & Tay, 2013).
Short Form of the Brief Religious Coping Questionnaire (RCOPE)
Religious coping was measured using a 7-item version of the RCOPE scale with six items rated on a Likert-type scale ranging from (0) not at all to (3) a great deal. Positive items are totaled separately from negative items, with each sub-scale totaling three items (Feder et al., 2013). A higher score on each sub-scale represents greater use of positive or negative religious coping (Cronbach’s alphas = 0.58 and 0.70, respectively). Additionally, one overall religious coping item to measure the extent that religion is used to understand or deal with stressful situations (John E. Fetzer Institute, 1999) is rated on a scale of (0) not involved at all to (3) very involved.
Perinatal Grief Scale (PGS)
This is a 33-item questionnaire utilizing a Likert scale ranging from (1) strongly agree to (5) strongly disagree (Potvin, Lasker, & Toedter, 1989; Toedter et al., 2001). Two reverse coded items were reversed before the items were summed for a possible index score of 33–165, with higher scores representing more severe grief (Cronbach’s alpha = 0.95).
Social Provisions Scale (SPS)
The 12-item version was used, which assesses six components of social support received from others as perceived by the respondent (Mosley-Williams, Lumley, Gillis, Leisen, & Guice, 2002). A Likert-type scale ranging from (1) strongly disagree to (4) strongly agree is summed after reversing reverse-coded items for a possible index score of 12–48, with higher scores reflecting more social support (Cronbach’s alpha = 0.70).
Five Facet Questionnaire: Short Form (FFMQ-SF)
The FFMQ-SF utilizes a 5-point Likert scale ranging from (1) never or very rarely true to (5) very often or always true, to assess the five facets of Mindfulness with 24 items (Bohlmeijer, M, Fledderus, Veehof, & Baer, 2011). Each facet is scored independently after reversing reverse-coded items (Cronbach’s alphas ranging from 0.72 for acting with awareness to 0.92 for observing). The five facets of Mindfulness are distinct, and, therefore, cannot be given an index score (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006; Baer et al., 2008; Bohlmeijer et al., 2011).
Procedures
Institutional review board (IRB) approval was received from the study team’s university IRB with care taken to ensure compliance with the ethical guidelines for India. Potential participants were informed that they would be asked questions to obtain demographic information and questions about their experience with grief after stillbirth and the acceptability of the pilot intervention.
Intervention Description
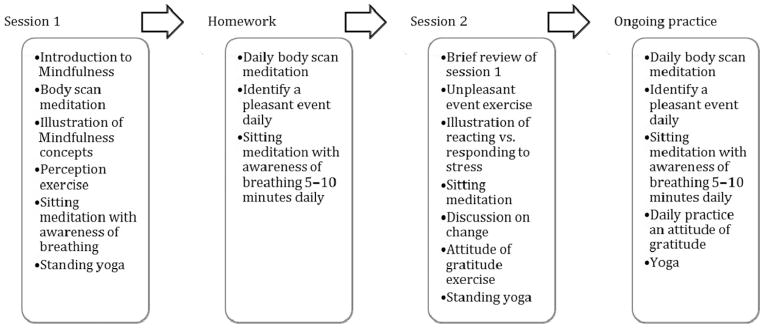
A pilot intervention group was conducted to explore modality of implementation. The pilot intervention (Figure 1) was adapted from the Stress Reduction Clinic Mindfulness-based Stress Reduction (MBSR) Curriculum Guide (Blacker, Meleo-Meyer, Kabat-Zinn, & Santorelli, 2009). The first session of the intervention consisted of: (a) an introduction to Mindfulness; (b) body scan meditation exercise followed by group discussion; (c) an illustrative verbal presentation of Mindfulness concepts; (d) a perception exercise; (e) sitting meditation with awareness of breathing followed by sharing dyads; and (f) concluded with standing yoga. The women were instructed to practice body scan meditation each day, identify at least one pleasant event daily, and try sitting meditation with awareness of breathing 5–10 min/day for the week between sessions. Session two consisted of: (a) a brief review of concepts covered in session one; (b) unpleasant event exercise followed by sharing dyads; (c) reacting vs responding to stress illustration; (d) brief sitting meditation, discussion on change; (e) an attitude of gratitude exercise; and (f) again standing yoga. In conclusion, the women were instructed to continue practicing body scan meditation, identify at least one pleasant event per day, do sitting meditation with awareness of breathing 5–10 min/day, practice yoga, and identify at least one thing to be grateful for each day.
FIGURE 1.
Structure and components of the brief pilot intervention conducted over a 2-week timeframe. This pilot intervention was adapted from a standardized Mindfulness-Based Stress Reduction (MBSR) program.
Data Collection and Analysis
All key informant interviews and the focus group were audio-recorded and transcribed verbatim and then systematically coded by two individuals. Qualitative analysis of the data resulted in a final codebook with 14 codes, which were clustered into nine sub-themes and four themes. Interrater reliability was determined by dividing the number of agreed upon codes by all possible codes, then multiplied by 100 (Kelsey, 1996), which resulted in 94.3% overall agreement.
Quantitative and qualitative data pertaining to the pilot intervention were collected before the first session (pre-test). The second session was followed by the post-test and qualitative program evaluation completed as a structured interview. Thematic analysis was completed on qualitative data. All quantitative data were analyzed with SPSS.
RESULTS
Participants
Phase one
Key informant interviews (n = 10) were conducted with a doctor, a staff nurse, and women of reproductive age that had experienced stillbirth (<1 year–17 years prior). A focus group (n = 6) was conducted with women of reproductive age who had a stillbirth history (<1 year–8 years since event). Most had suffered one stillbirth, some women had suffered stillbirth twice, and two women had suffered four and five stillbirths, respectively. With the exception of the doctor and nurse, all the women were married, living with their husbands and in-laws.
Phase two
In total, 22 village women with a history of stillbirth attended the intervention. Of these women, in the first session, 13 had experienced stillbirth within the last 1–7 years, and two of the women had experienced stillbirth twice. The average time since stillbirth or most recent stillbirth was 19.31 months (SD 21.34). The Perinatal Grief Scale index mean among these women was 106.39 (SD 22.68), well above the normal cutoff score of 91. Of women who had experienced stillbirth, 12 attended the second session, however, only six of these women had attended the first session and were eligible to complete the post-test. All but one of the women had one or more living children, gravida ranged from 1 to 8. Some of the women were not sure of their own age, but their ages ranged approximately 18–35. See Table 1 for demographic details.
TABLE 1.
Sample demographics (n = 13)
| Characteristics | n | (%) |
|---|---|---|
| Age | ||
| 18–25 years | 7 | 54 |
| 26–35 years | 6 | 46 |
| Time since stillbirth | ||
| ≤6 months | 3 | 23 |
| >7 to ≤12 months | 6 | 46 |
| >1 to ≤5 years | 3 | 23 |
| >6 years | 1 | 8 |
| Had antenatal care | ||
| Yes | 8 | 62 |
| No | 5 | 38 |
| Where delivery occurred | ||
| Home | 10 | 77 |
| Facility | 2 | 15 |
| Other | 1 | 8 |
| Gestational age | ||
| 28–39 weeks | 8 | 62 |
| Full term | 5 | 38 |
| Who attended birth | ||
| Relative | 4 | 31 |
| Dai* | 4 | 31 |
| Nurse/Midwife | 3 | 23 |
| Doctor | 1 | 8 |
| None | 1 | 8 |
| Ethnicity | ||
| Scheduled Caste† | 7 | 54 |
| Scheduled Tribe†† | 3 | 23 |
| OBC††† | 3 | 23 |
| Total number of living children | ||
| 0 | 1 | 8 |
| 1–2 | 5 | 39 |
| 3–5 | 7 | 54 |
A Dai is an untrained, traditional birth attendant who conducts deliveries in rural areas (Park, 2009).
Scheduled castes, tribes, and other backward castes; OBC are people groups of the lowest status in the Indian social stratification system (Sachchidananda, 1993).
Feasibility and Acceptance of Intervention and Procedures
The four themes that emerged from the qualitative data were: (1) Grief, (2) Coping Needs, (3) Receptivity, and (4) Feasibility.
The Grief theme was expressed in poignant descriptions of how old the lost child would have been had he or she lived; what the mother thought the child would have been like; and how thinking of the lost child evoked a deep pain that does not resolve with time or having other children. Women reported that the grief interfered with their day-to-day functioning in terms of decreased ability to concentrate on the task at hand and decreased motivation in general. Additionally, they expressed that their health was affected due to poor appetite and sleep interference associated with their grief.
The Coping Needs theme encompassed both positive and negative coping attempts and perceived family support. Distraction was a common means of attempting to cope, which was employed by the women themselves as well as their families. The belief that having another child would assuage their grief caused women to seek pregnancy, despite advice to wait. Prayer and the performance of rituals were employed by some women and their families to help them cope with the loss. Talking to others was identified as a positive, but often unavailable means of coping and was addressed in the subsequent intervention.
The Receptivity theme captured the women’s response to the Mindfulness concept and their willingness to participate. They expressed an understanding of the concept, saw it of value for dealing with mental and emotional pain, embraced the mind–body connection as foundational, and indicated they would participate in the program given the opportunity, as well as recommending it to others.
The Feasibility theme reflected the exploration of possible intervention location, transportation issues, and the women’s autonomy. The village was endorsed repeatedly as the appropriate location for the program. Transportation and permission to attend at the hospital was felt to be problematic. Transportation was not reliably available and was expensive. Permission to attend was likely if the program was delivered in the village where male family members would know where the women were and what they were doing. Additionally, if the Sarpanch (village chief) endorsed the program, their families would not oppose their participation, even if they did not fully support it. Table 2 presents the themes, sub-themes, and exemplar supporting quotes.
TABLE 2.
Qualitative data categories (description of each category and selected exemplifying quotes)
| Theme (Frequency) | Sub-themes | Supporting quotes |
|---|---|---|
| Grief (24) | Grief makes it hard to function | I want to win over this loss, my life was saved, but how can I endure? I don’t feel like doing any work. Many days I suffer, and it interrupts my cooking, etc. The pain comes again and again. |
| Grief affects health | The pain remains, even after another child. I don’t feel like eating food, then I am weak, then there is only sitting and sleep, sleep. | |
| Coping needs (18) | Coping attempts | Praying that no one does Black magic, talking to doctors, it has not helped, time does not help, I’m only waiting to get pregnant again. |
| Family support | They [family] say don’t cry, and give work to keep me busy so I don’t think. I try to think of other things, but every time I think of the baby it is painful. They [family] try to distract me, but it only helps a little. I need to talk so my burden becomes less. |
|
| Receptivity (23) | Mindfulness concept acceptability | I would want to participate, after telling we feel less burdened. Please do the program, I will come. Medicine cannot help this pain, so we need this. Psychological support is first, this is good, then the family should also support. |
| Willingness to participate | This will help us move forward. It will be a good thing. Mind–body connection is very strong, this is helpful, there will be changes. Without this understanding they will sit and cry all day long. |
|
| Feasibility (22) | Intervention location | My family would let me come, my husband could bring me. I came because I lost one child, other women will come also. |
| Transportation | Until today I have never gone to hospital, it must be in our village. If it is in the village or nearby village they [family] will allow us to come. | |
| Permission to attend | We can attend once a week for 2 months, yes. If we have finished the work we are free to go every week. If Sarpanch* gives permission we will participate, no one will stop us then. |
Sarpanch is the village chief.
The Pilot Intervention
The pilot intervention was well attended (n = 22), all participants were engaged, embraced Mindfulness concepts, and endorsed the intervention adaptations as culturally appropriate. Some women who had not heard about the intervention initially, subsequently came to the second session, suggesting both a need and strong interest in the concept of the intervention. All participants at session one indicated a desire to attend the second session, and would attend 8-weekly sessions if given the opportunity to participate in the full intervention. However, only six of the women who attended the first also attended the second session. Women who were unable to attend the second session sent word through other attendees. A number of barriers to attendance were identified: family obligations, harvest, local festivals, and marriage season.
Pre-test Results
The Hopkins Symptoms Check List (HSCL-10) index score mean was 2.88 (SD .78), considerably higher than the 1.75 cutoff score recognized as the normal index. The Satisfaction with Life Scale (SWLS) mean was 23.50(SD 2.17). The mean of the positive religious/spiritual coping sub-scale was 7.9 (SD 1.60) and the negative religious/spiritual coping sub-scale mean was 6.369 (SD 2.28). In response to the overall religious/spiritual coping item asking to what extent religion is involved in understanding or dealing with stressful situations, 62% of the women chose ‘somewhat involved’, 31% chose ‘very involved’, and the remainder chose ‘not at all involved’. None of the women chose response option ‘not very involved.’ The average Social Provision of Support (SPS) index score was 21.83 (SD 5.15). The five facets of Mindfulness sub-scale means were as follows: describe 14.67 (SD 1.75); non-react 14.00 (SD 7.66); non-judge 10.17 (SD 3.92); observe 12.33 (SD 4.92); act with awareness 13.50 (SD 1.97).
Post-test Results
On the post-test, the mean HSCL-10 was 2.13 (SD 0.62) and the mean SWLS 24.67 (SD 3.72). The means of the religious/spiritual coping sub-scales were 7.33 (SD 1.63) and 5.00 (SD 1.27) for positive and negative, respectively. In response to the overall religious/spiritual coping item on post-test 83% (n = 5) of the women chose ‘somewhat involved’. The mean SPS was 26.83 (SD 4.62). The five facets of Mindfulness sub-scale means were as follows: describe 18.00 (SD 2.45); non-react 20.00 (SD 3.95); non-judge 15.00 (SD 4.05); observe 15.83 (SD 3.31); and act with awareness 18.83 (SD 3.65).
Efficacy of the Intervention
Comparison of paired pre- and post-test results of HSCL-10, Brief RCOPE sub-scales, SWLS, SPS, and the five facets of Mindfulness, revealed a significant difference in the desired direction in observing, describing, acting with awareness, and the non-judging facets of Mindfulness. While still elevated, the decrease in HSCL-10 index approached statistical significance. No other significant differences were noted, though all variables changed in the desired direction (see Table 3).
TABLE 3.
Paired t-tests, pre- and post-intervention comparison (n = 6)
| Pre-test
|
Post-test
|
||||||
|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | t (5) | p value (2-tailed) | r | |
| HSCL-10 | 2.88 | 0.31 | 2.13 | 0.26 | 2.46 | 0.057 | 0.46 |
| SWLS | 23.50 | 0.88 | 24.67 | 1.52 | −1.47 | 0.201 | 0.92 |
| Positive RCOPE | 7.00 | 0.78 | 7.33 | 0.67 | −.598 | 0.576 | 0.11 |
| Negative RCOPE | 5.50 | 0.99 | 5.00 | 0.52 | 0.473 | 0.656 | 0.81 |
| Overall RCOPE | 2.00 | 0.00 | 2.17 | 0.17 | −1.00 | 0.363 | – |
| SPS | 21.83 | 2.10 | 26.83 | 1.17 | −2.99 | 0.031* | 0.61 |
| Describe | 14.67 | 0.71 | 18.00 | 1.00 | −3.37 | 0.020* | 0.37 |
| Non-react | 14.00 | 3.13 | 20.00 | 1.61 | −1.96 | 0.107 | 0.30 |
| Non-judge | 10.17 | 1.60 | 15.00 | 1.65 | −2.98 | 0.031* | 0.50 |
| Observe | 12.33 | 2.01 | 15.83 | 1.35 | −3.66 | 0.015* | 0.91 |
| Act aware | 13.50 | 0.80 | 18.83 | 1.49 | −4.00 | 0.010* | 0.46 |
p < 0.05.
Participant Feedback
All participants who attended both sessions (n = 6) indicated daily practice of Mindfulness skills between sessions one and two. All 12 women who participated in the second session completed the program evaluation. Their mean responses, with a possible range of 1–5 indicating strongly disagree to strongly agree, respectively, are reported in Table 4. Among these participants (n = 12) preferences of the time of year for the intervention with regards to major holidays and harvest seasons varied across all 12 months without consensus.
TABLE 4.
Program evaluation responses (n = 12)
| Item | Mean | SD | Variance |
|---|---|---|---|
| The format of the group meeting was comfortable. | 4.08 | 0.29 | 0.08 |
| The duration of the session was about right. | 4.08 | 0.52 | 0.27 |
| This is a good place to have group meetings. | 4.17 | 0.39 | 0.15 |
| The meetings should be held in the village. | 3.92 | 0.79 | 0.63 |
| I learned a lot about stillbirths, grief, and coping. | 4.08 | 0.52 | 0.27 |
| I do not think Mindfulness will help me. | 2.50 | 0.91 | 0.82 |
| It was helpful to be in a group with other women who had a similar experience. | 4.25 | 0.45 | 0.21 |
| I will continue to use Mindfulness techniques. | 4.25 | 0.45 | 0.21 |
| I would like to learn more about Mindfulness. | 4.08 | 0.52 | 0.27 |
| If 8-weekly sessions were available I would participate. | 3.83 | 0.58 | 0.33 |
| My family noticed a difference in my ability to cope. | 3.50 | 1.00 | 1.00 |
| My family would allow me to return for future session. | 4.17 | 0.58 | 0.33 |
DISCUSSION
This study, to the best of our knowledge, is the first to examine feasibility and acceptance of a Mindfulness-based intervention to reduce perinatal grief among poor, rural, central Indian women with a history of stillbirth. As in our previous study, these are women with high levels of perinatal grief and risk of complicated grief (Potvin et al., 1989; Toedter et al., 2001). Perinatal grief, particularly prolonged perinatal grief, such as noted in this sample, puts women at risk for mental health issues, somatic symptoms, and decreased function (Bennett, Litz, Lee, & Maguen, 2005; Horowitz et al., 2003; Roberts, Anderson et al., 2012). This prolonged grief places each of these Indian women at further risk for domestic violence and displacement from her family or community, and other social issues, particularly if she has failed to produce a child, preferably a son (Joshi, Dhapola, & Pelto, 2008).
Stigmatization of mental health and reproductive issues, plus a strong cultural belief in the inter-relatedness of mind, body, and spirit, in addition to a lack of mental health resources (Gupta, 2010), points to Mindfulness as a possible solution. This Mindfulness-based intervention utilizing yoga and meditation was well-suited and well-received among these women suffering with perinatal grief.
Results indicate concept acceptance and clearly acknowledged need and interest by the women for an intervention. High receptivity for the proposed intervention was indicated by enthusiastic response and requests for immediate intervention delivery. However, complete delivery of even this shortened pilot intervention proved problematic. It is challenging for these women to attend weekly sessions, even when provided in the village, within walking distance. Their time is structured by: (a) familial duties; (b) work dictated by environmental variations, such as harvesting; (c) community events, such as weddings and festivals. Additionally, the women lack autonomy: therefore, first and foremost they were required to complete all their daily household chores, and comply with the burden of family demands and obligations. Only after all of these conditions were met, could they even consider attending a session. Despite their desire and expressed intentions to return for the second session, many women were unable to attend due to these intervening events and obligations. At the same time, as news of the intervention spread by word of mouth, women who had not attended the initial session presented for the second session, hoping to participate.
Furthermore, notwithstanding the lack of statistical power and low dose of intervention sessions, preliminary results of this research can be cautiously interpreted as indicating that a Mindfulness-based intervention for reduction of perinatal grief may be effective. Statistically significant changes were noted on paired t-tests for four of the five facets of Mindfulness. Reliability and relationship tests suggest that the tools will adequately measure and show significance in a larger study.
The modified cut-off score of HSCL 1.65 was used to indicate elevated levels of anxiety and depression, as this study population resembled Syed et al.’s (2008) Pakistani population more closely than a Western sample. The SWLS pre-test mean of 23.50, falls in the average score range (20–24), indicating that on average these women felt that their lives were generally satisfactory, though there were some areas where they desired improvement (Diener, 2006). On post-test, the SWLS mean was 24.67, falling between average and high (25–29) scores, which indicates a shift toward feeling that their lives were overall going well (Diener, 2006).
Study limitations include several methodological issues. The study sample was small and lacked statistical power. The pilot intervention was conducted in two lengthy sessions, but was still a low dose in comparison with standard MBSR. Self-report measures, although most often used in comparable studies, may have introduced response bias. Given that the pre- and post-test were only 1 week apart, practice effects may have affected results. Additionally, due to low autonomy, these women may be prone to favorable response bias. However, we believe that using triangulation and saturation as part of our qualitative data collection strategy, helped prevent misinterpretation of the quantitative results.
Several strengths of the study are important. The Mindfulness-based intervention was a good cultural fit. The familiar concept of the mind–body connection and their high need possibly enhanced the participants’ receptivity to the Mindfulness-based intervention. MBSR, which the intervention was based upon, is empirically supported. The qualitative findings add important information regarding how women in rural, central India perceive the need for a Mindfulness-based intervention to reduce perinatal grief and improve coping. Additionally, the qualitative findings add breadth and depth to the quantitative findings.
Within the context of these limitations, the current findings are encouraging and further research is warranted to test alternate delivery methods with a larger sample and longer follow-up. If this proves feasible, expansion of the intervention might be considered.
In addition to improving psychological wellbeing among women suffering from perinatal grief, Mindfulness practice has the potential to be transformative at the community level. MBSR education has been associated with improved attitudes and empathy among physicians, necessary characteristics for patient-centered care (Krasner et al., 2009). Unfortunately, the women who need care, most always lack power to engage the health-care system. Therefore, to increase the effectiveness of health care in these complex settings, hospital staff education regarding the psychosocial issued involved, should be offered in the future. This type of education would hopefully shift the prevailing medical society’s attitude that these women are not experiencing perinatal grief and just need to get on with having another child (Mammen, 1995; Roberts, Anderson et al., 2012). If the medical community elicits the concerns and emotions of their patients who experience a life-changing stillbirth event, women will be allowed to express their feelings, and, perhaps will slowly begin to do so within their families and communities as well. They will, however, require a greater ability to cope more effectively with both short and long-term stressors, which are critical skills for women dealing with perinatal grief and the social repercussions of stillbirth in this context.
CONCLUSION
Mindfulness is a culturally acceptable intervention for poor rural Indian women who have experienced significant grief following stillbirth. While the results with a short version of the intervention are promising, a full-dose MBSR intervention in this setting would not be feasible. Though the women are enthusiastic about the intervention, note that they need it, and want it; the realities of their lives would make the rigorous schedule of MBSR impossible to deliver. However, given the very positive results of this pilot test, we continue wrestling with how best to deliver the intervention to women in the rural Indian context. It is clear that even the shortened version of the intervention remains a challenge, as indeed, village women in a collectivistic society are able to attend group events but not easily so at scheduled weekly intervals.
Informed by the qualitative data, the decision was made to provide childcare to better accommodate the limited autonomy and resources of these women. Also, based on qualitative feedback, future work will entail a mixed format. It appears critical to conduct small group (dyad to triad) follow-up sessions with participants after group sessions and this can be accomplished by partnering with local staff nurses and nursing students doing their community health rotations in the village. The follow-up sessions will be used to reiterate Mindfulness concepts, monitor progress, promote continued practice of Mindfulness skills, and receive feedback. This partnership will be instrumental to the success of implementing and sustaining the intervention in the future. It will also help the nurses learn to better understand the women’s realities and thus be more effective in delivering future care to the women who rarely have the opportunity to interact with nurses that are usually fully hospital-based.
Footnotes
Declaration of Interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Contributor Information
Lisa R. Roberts, Loma Linda University, School of Nursing, Loma Linda, California, USA.
Susanne B. Montgomery, Loma Linda University, School of Behavioral Health, Loma Linda, California, USA.
References
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Barr p, cacciatore j. Problematic Emotions and Maternal Grief. Omega: Journal of Death & Dying. 2007;56(4):331–348. doi: 10.2190/om.56.4.b. [DOI] [PubMed] [Google Scholar]
- Bennett SM, Litz BT, Maguen S, Ehrenreich JT. An exploratory study of the psychological impact and clinical care of perinatal loss. Journal of Loss & Trauma. 2008;13(6):485–510. [Google Scholar]
- Bennett SM, Litz BT, Lee BS, Maguen S. The scope and impact of perinatal loss: current status and future directions. Professional Psychology: Research and Practice. 2005;36(2):180–187. [Google Scholar]
- Berg BL. Qualitative research methods for the social sciences. Boston: Allyn and Bacon; 2009. [Google Scholar]
- Bhati DK. Stillbirths: A high magnitude public health issue in India. South East Asia Journal of Public Health. 2014;3(1):3–9. [Google Scholar]
- Blacker M, Meleo-Meyer F, Kabat-Zinn J, Santorelli S. Stress reduction clinic mindfulness-based stress reduction (MBSR) curriculum guide. Center for Mindfulness in Medicine, Health Care, and Society; Worcester, MA: University of Massachusetts Medical School; 2009. p. 20. [Google Scholar]
- Bohlmeijer EM, Fledderus M, Veehof M, Baer R. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment. 2011;18(3):308–320. doi: 10.1177/1073191111408231. [DOI] [PubMed] [Google Scholar]
- Boyle FM, Vance JC, Najman JM, Thearle MJ. The mental health impact of stillbirth, neonatal death or SIDS: prevalence and patterns of distress among mothers. Social Science & Medicine. 1996;43(8):1273–1282. doi: 10.1016/0277-9536(96)00039-1. [DOI] [PubMed] [Google Scholar]
- Corbin JM, Strauss AL. Basics of qualitative research: techniques and procedures for developing grounded theory. Los Angeles, CA: Sage Publications, Inc; 2008. [Google Scholar]
- Davis D, Hayes JA. What are the benefits of mindfulness? A practice review of psychotherapy-related research. Psychotherapy. 2011;48(2):198–208. doi: 10.1037/a0022062. [DOI] [PubMed] [Google Scholar]
- Diener E. Satisfaction with Life Scale (SWLS) 2006 Understanding the SWLS scores. Retrieved from http://internal.psychology.illinois.edu/~ediener/SWLS.html.
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction with Life Scale. Journal of Personality Assessment. 1985;49(1):71. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Diener E, Inglehart R, Tay L. Theory and validity of life satisfaction scales. Social Indicators Research. 2013;112(3):497–527. [Google Scholar]
- Farb NA, Anderson AK, Mayberg H, Bean J, McKeon D, Segal ZV. Minding one’s emotions: mindfulness training alters the neural expression of sadness. Emotion. 2010;10(1):25. doi: 10.1037/a0017151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feder A, Ahmad S, Lee EJ, Morgan JE, Singh R, Smith BW, et al. Coping and PTSD symptoms in Pakistani earthquake survivors: Purpose in life, religious coping and social support. Journal of Affective Disorders. 2013;147(1–3):156–163. doi: 10.1016/j.jad.2012.10.027. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Gupta VB. Impact of culture on healthcare seeking behavior of Asian Indians. Journal of Cultural Diversity. 2010;17(1):13–19. [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ, Bonanno GA, Holen A. Pathological grief: diagnosis and explanation. Psychosomatic Medicine. 1993;55(3):260. doi: 10.1097/00006842-199305000-00004. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ, Siegel B, Holen A, Bonanno GA, Milbrath C, Stinson CH. Diagnostic criteria for complicated grief disorder. Focus. 2003;1(3):290–298. doi: 10.1176/ajp.154.7.904. [DOI] [PubMed] [Google Scholar]
- John E. Fetzer Institute. Multidimensional measurement of religiousness/spirituality for use in health research. Kalamazoo, MI: Author; 1999. p. 96. [Google Scholar]
- Jones PS, Lee JW, Phillips LR, Zhang XE, Jaceldo KB. An adaptation of Brislin’s translation model for cross-cultural research. Nursing Research. 2001;50(5):300. doi: 10.1097/00006199-200109000-00008. [DOI] [PubMed] [Google Scholar]
- Joshi A, Dhapola M, Pelto PJ. Gynaecological problems: perceptions and treatment-seeking behaviors of rural Gujarati women. In: Koenig M, Jejeebhoy S, Cleland J, Ganatra B, editors. Reproductive health in India: new evidence. New Delhi: Rawat Publications; 2008. pp. 133–158. [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Delta Publishing; 2009. [Google Scholar]
- Kelly ER. Marking short lives: constructing and sharing rituals following pregnancy loss. New York: Peter Lang Publishing; 2007. [Google Scholar]
- Kelsey JL. Methods in observational epidemiology. New York: Oxford University Press; 1996. [Google Scholar]
- Kramer MS, Liu S, Luo Z, Yuan H, Platt RW, Joseph KS. Analysis of perinatal mortality and its components: time for a change? American Journal of Epidemiology. 2002;156(6):493. doi: 10.1093/aje/kwf077. [DOI] [PubMed] [Google Scholar]
- Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302(12):1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300(11):1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- Mammen OK. Women’s reaction to perinatal loss in India: an exploratory, descriptive study. Infant Mental Health Journal. 1995;16(2):94–101. [Google Scholar]
- Mehta L, Verma IC. Helping parents to face perinatal loss. Indian Journal of Pediatrics. 1990;57(5):607–609. doi: 10.1007/BF02728696. [DOI] [PubMed] [Google Scholar]
- Miller MC. Complementary and integrative treatments: expanding the continuum of care. Otolaryngologic Clinics of North America. 2013;46(3):261–276. doi: 10.1016/j.otc.2012.12.003. [DOI] [PubMed] [Google Scholar]
- Mosley-Williams A, Lumley MA, Gillis M, Leisen J, Guice D. Barriers to treatment adherence among African American and white women with systemic lupus erythematosus. Arthritis & Rheumatism. 2002;47(6):630–638. doi: 10.1002/art.10790. [DOI] [PubMed] [Google Scholar]
- Park K. Park’s textbook of preventive and social medicine. 20. Jabalpur, India: Banarsidas Bhanot; 2009. [Google Scholar]
- Potvin L, Lasker J, Toedter L. Measuring grief: A short version of the Perinatal Grief Scale. Journal of Psychopathology and Behavioral Assessment. 1989;11(1):29–45. [Google Scholar]
- Roberts LR, Anderson BA, Lee JW, Montgomery S. Grief and women: stillbirth in the social context of India. International Journal of Childbirth. 2012;2(3):12. doi: 10.1891/2156-5287.2.3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts LR, Montgomery S, Lee JW, Anderson BA. Social and cultural factors associated with perinatal grief in Chhattisgarh, India. Journal of Community Health. 2012;37(3):572–582. doi: 10.1007/s10900-011-9485-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowland A, Goodnight WH. Fetal loss: addressing the evaluation and supporting the emotional needs of parents. Journal of Midwifery & Women’s Health. 2009;54(3):241–248. doi: 10.1016/j.jmwh.2009.02.011. [DOI] [PubMed] [Google Scholar]
- Sachchidananda. Political culture of scheduled castes and tribes: a study in change. In: Roy SB, Ghosh AK, editors. People of India: Bio-cultural dimensions. New Delhi: Inter-India Publications; 1993. p. 456. [Google Scholar]
- Sather M, Fajon AV, Zaentz R, Rubens C. Global report on preterm birth and stillbirth (5 of 7): advocacy barriers and opportunities. BMC Pregnancy and Childbirth. 2010;10(Suppl 1):S5. doi: 10.1186/1471-2393-10-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. Journal of Behavioral Medicine. 1998;21(6):581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- Syed HR, Zachrisson HD, Dalgard OS, Dalen I, Ahlberg N. Concordance between Hopkins Symptom Checklist (HSCL-10) and Pakistan Anxiety and Depression Questionnaire (PADQ), in a rural self-motivated population in Pakistan. BMC Psychiatry. 2008;8:1–12. doi: 10.1186/1471-244X-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor AG, Goehler LE, Galper DI, Innes KE, Bourguignon C. Top-down and bottom-up mechanisms in mind-body medicine: development of an integrative framework for psychophysiological research. Explore: The Journal of Science and Healing. 2010;6(1):29–41. doi: 10.1016/j.explore.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toedter LJ, Lasker JN, Janssen HM. International comparison of studies using the Perinatal Grief Scale: A decade of research on pregnancy loss. Death Studies. 2001;25(3):205–228. doi: 10.1080/07481180125971. [DOI] [PubMed] [Google Scholar]