Abstract
Background
Outcomes following an acute myocardial infarction (AMI) are generally more favorable if pre-hospital delay time is minimized.
Methods
We examined the association of neighborhood household income (nINC) and health insurance status with prehospital delay among a weighted sample of 9700 men and women with a validated, definite, or probable AMI in the Atherosclerosis Risk in Communities (ARIC) community surveillance study (1993-2002). Weighted multinomial regression with generalized estimation equations was used to estimate odds ratios (ORs) and 95% confidence intervals (CIs) and to account for the clustering of patients within census tracts.
Results
Low nINC was associated with a higher odds of long vs short delay (OR, 1.46; 95% CI, 1.09-1.96) and medium vs short delay (OR, 1.43; 95% CI, 1.12-1.81) compared with high nINC in a model including age, sex, race, diabetes, hypertension, presence of chest pain, arrival at the hospital via emergency medical service, distance from residence to hospital, study community, and year of AMI event. Meanwhile, compared with patients with prepaid insurance or prepaid plus Medicare, patients with Medicaid were more likely to have a long vs short delay (OR, 1.87; 95% CI, 1.10-3.19) and a medium vs short delay (OR, 1.76; 95% CI, 1.13-2.74).
Conclusions
Both low nINC and being a Medicaid recipient are associated with longer prehospital delay. Reducing socioeconomic and insurance disparities in pre-hospital delay is critical because excess delay time may hinder effective care for AMI.
Outcomes following acute myocardial infarction (AMI) are typically more favorable if medical treatment is received in a timely manner. Time-dependent treatments for AMI, such as primary percutaneous coronary intervention (PCI) and thrombolysis, are more likely to be given to patients arriving early to the hospital following the onset of symptoms.1,2 Despite efforts to reduce time elapsed between the onset of AMI symptoms and hospital arrival, prehospital delay times have not improved over the years.3-5
Previous research has demonstrated an association between prolonged prehospital delay time following AMI and female sex, black race, advanced age, hypertension, and diabetes.3-7 Meanwhile, shorter prehospital delay times have been reported among patients who experience chest pain and are transported to the hospital by emergency medical service (EMS).3,8-10
A paucity of data exists regarding pre-hospital delay for AMI and socioeconomic status (SES), since SES data (such as education and income) are not generally available in the medical record. However, place of residence is universally collected for the purposes of patient follow-up and billing, allowing linkage to census-based socioeconomic data. Indicators of neighborhood socioeconomic conditions, while often used as surrogates for individual SES, have also been shown to influence a patient's health independent of individual SES.11-13 The independent influence of neighborhood SES may be due to issues of access to care, structural social support, and the built environ-ment.14-17 Meanwhile, health insurance status has been used as a proxy for individual SES in the literature when such information is not available.18,19
The purpose of the present study is to determine whether neighborhood household income (nINC) and health insurance status influence prehospital delay times among patients with AMI. We hypothesized that low nINC, no health insurance, and Medicaid coverage would be associated with longer prehospital delay times among patients with AMI presenting to hospitals with the onset of symptoms preceding admission in 4 geographically defined US study communities.
Methods
The Atherosclerosis Risk in Communities (ARIC) study's community-based surveillance of coronary heart disease (CHD) has been ongoing since 1987, and its methods have been previously described.20,21 Briefly, hospital discharges for AMI among white and black patients aged 35 to 74 years from 4 study communities (Forsyth County, North Carolina; the city of Jackson, Mississippi; northwest suburbs of Minneapolis, Minnesota; and Washington County, Maryland) were retrospectively reviewed.
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) hospital discharge codes 402,410 through 414, 427, 428, and 518.4 were sampled from the participating hospitals serving the 4 study communities. Trained staff abstracted presenting symptoms, medical history, and pertinent laboratory values from eligible medical records. Myocardial infarction (MI) was identified on the basis of chest pain (presence or absence; cardiac or noncardiac origin), cardiac bio-markers (abnormal, equivocal, normal, or incomplete as compared with laboratory standards) and electrocardiographic evidence (evolving diagnostic, diagnostic, evolving ST-T, equivocal, or other evidence based on Minnesota codes) and classified as definite, probable, suspect, no MI, or unclassifiable.22 All analyses were weighted to account for the sampling of ICD-9-CM hospital diagnosis codes.21 Events classified as definite or probable were combined and included in the present analyses. Multiple hospitalizations for the same patient occurring within 28 days were linked, and only the first occurrence was considered in this analysis.
Between 1993 and 2002, 9560 definite or probable hospitalized MIs occurred in the ARIC community surveillance study area. Address data, our source of nINC, was not available in ARIC community surveillance prior to 1993, and therefore all events since 1987 could not be included in this analysis. Included were events occurring in white and black patients in Mississippi and North Carolina. In Maryland and Minnesota, analyses were restricted to whites because the black population in these communities was small and not sufficient to provide race-specific estimates. Events with delay times exceeding 3 days (n=802) were excluded from this analysis, since this investigation is focused on acute onset events. Also excluded were 669 events without delay time recorded in the medical record, 1172 events that were hospital transfers, and 171 events with missing insurance status. A final study sample of 6746 (9700 weighted) hospitalized MI events over the 10-year period was used in the analyses.
Prehospital delay time was defined as the time elapsed between symptom onset and hospital arrival.23 Time of symptom onset was abstracted from the medical records by trained abstractors per ARIC study protocol.24 Prehospital delay time was obtained from the medical record as previously described3 and classified into 3 clinically meaningful categories of short (<2 hours), medium (2-12 hours), and long (12-72 hours) delay.
Address data abstracted from the medical record were sent to a commercial vendor for geocoding. Accuracy of the vendor has been previously assessed and found to be high.25 Of the data submitted, 93% were exact address matches, and 95% were geocoded to the level of the census tract. Geocoded cases were linked with year 2000 US census socioeconomic data. Since a higher percentage of addresses could be matched to the level of the census tract and because socioeconomic data aggregated at the level of the census tract and block group result in almost identical socioeconomic gradients with a variety of health outcomes,26,27 we used census tract level data in the reported analyses. We used US census tract median household income to characterize nINC, since it and other related measures of deprivation have been demonstrated to produce similar results as more complicated indexes.27-29 The distribution of median household income across all census tracts in the 4 study communities were grouped into the following tertiles: low (<$33 533), medium ($33 533-$50 031), and high (≥$50032). Health insurance was categorized as prepaid (ie, health plan, health maintenance organization) or prepaid and Medicare, Medicare only, Medicaid, Medicare and Medicaid, other (ie, government insurance and workers' compensation), or no insurance.
The distance from residence to hospital was calculated as the spherical distance between the latitude and longitude coordinates of the patient address and the location of the hospital. The conversion calculation from degrees and minutes to kilometers accounted for the curvature of the earth. Distance from residence to hospital was not normally distributed and log transformed in all analyses.
Weighted multinomial regression implemented with generalized estimation equations was used to estimate odds ratios (ORs) and 95% confidence intervals (CIs) and to account for the clustering of patients within census tracts (SAS-callable SUDAAN, release 9.0.1; Research Triangle Institute, Research Triangle Park, North Carolina). The odds of long delay compared with short delay were estimated, in addition to the odds of medium delay compared with short delay. The following potentially confounding factors were abstracted from the medical record and included in the full model: age, sex, race, diabetes, hypertension, presence of chest pain, arrival at the hospital via EMS vs other mode of transportation, distance from residence to hospital (inkilometers), ARIC study community, and year of AMI event. Effect modification of the association between SES measures and delay by age, sex, race, diabetes, hypertension, EMS use, and study community was assessed using a Wald χ2 test. Given the large sample size, P< .05 was considered statistically significant.
Result
The study population was 33% female, 25% black, and 42% arrived at the hospital via EMS. Overall, 66% and 33% had current or history of hypertension and diabetes, respectively, and 94% reported chest pain as an acute cardiac symptom beginning before hospital arrival (Table 1). Regarding prehospital delays, 36% of patients arrived at the hospital within 2 hours of symptom onset, 42% arrived within 2 to 12 hours, and 22% arrived within 12 to 72 hours. Patient sociodemographic and medical history characteristics are given in Table 1, stratified by prehospital delay category. Those arriving within 2 hours were more likely to be male and white and to have arrived at the hospital by EMS than were those with longer delays.
Table 1. Characteristics of Patients With Definite or Probable AMI,a Overall and by Delay Category: ARIC Community Surveillance Study (1993-2002).
| Characteristic | Overall (n = 9700) |
Prehospital Delay | ||
|---|---|---|---|---|
|
| ||||
| <2 h (n = 3511) |
2-12 h (n = 4064) |
>12 h (n = 2125) |
||
| Household income, median, US$ | 42 342 | 43 437 | 41 804 | 41 561 |
| Age, mean, y | 60.6 | 59.9 | 61.0 | 60.8 |
| Distance traveled, mean, km | 5.3 | 5.2 | 5.5 | 5.3 |
| Health insurance status, % | ||||
| Prepaid, prepaid and Medicare | 68.6 | 70.3 | 68.0 | 66.1 |
| Medicaid and Medicare | 5.6 | 5.0 | 5.9 | 6.2 |
| Medicare | 11.3 | 10.5 | 11.8 | 11.8 |
| Medicaid | 3.5 | 2.7 | 3.9 | 4.2 |
| Other | 3.4 | 3.3 | 3.0 | 4.5 |
| No insurance | 7.6 | 8.3 | 7.3 | 7.1 |
| Female vs male, % | 33.2 | 30.6 | 33.9 | 36.2 |
| Black vs white, % | 25.1 | 22.8 | 25.5 | 28.2 |
| Current or history of hypertension, % | 65.7 | 62.2 | 67.2 | 68.5 |
| Current or history of diabetes, % | 32.5 | 28.6 | 33.5 | 37.3 |
| Symptoms included chest pain, % | 93.5 | 94.2 | 95.0 | 89.4 |
| Arrived at hospital by EMS, % | 41.6 | 53.1 | 38.0 | 29.4 |
Abbreviations: AMI, acute myocardial infarction; ARIC, Atherosclerosis Risk in Communities; EMS, emergency medical service.
Weighted to account for sampling strategy.
Among patients with low nINC, 44% had prepaid or prepaid and Medicare insurance. Patients with low nINC were more likely than other patients either to be uninsured or to have Medicaid and/or Medicare. Of patients from low nINC areas, 60% were black and 42% were female. On average, low nINC patients lived closer to the hospital than patients not living in low nINC areas, and 78% and 42% of patients living in low nINC areas had hypertension and diabetes, respectively (Table 2).
Table 2. Characteristics of Patients With Definite or Probable AMI,a by nINC Category: ARIC Community Surveillance Study (1993-2002).
| Characteristic | nINC Category | ||
|---|---|---|---|
|
| |||
| Low | Medium | High | |
| Age, mean, y | 59.4 | 61.3 | 60.9 |
| Distance traveled, mean, km | 3.4 | 6.2 | 6.4 |
| Health insurance status, % | |||
| Prepaid, prepaid and Medicare | 43.9 | 75.9 | 85.5 |
| Medicaid and Medicare | 12.2 | 3.3 | 1.5 |
| Medicare | 18.6 | 9.6 | 5.7 |
| Medicaid | 8.4 | 1.4 | 0.9 |
| Other | 4.5 | 2.9 | 3.0 |
| No insurance | 12.4 | 6.9 | 3.4 |
| Female vs male, % | 42.0 | 29.9 | 28.0 |
| Black vs white, % | 59.5 | 12.5 | 3.9 |
| Current or history of hypertension, % | 78.2 | 61.4 | 57.7 |
| Current or history of diabetes, % | 41.5 | 30.5 | 25.6 |
| Symptoms included chest pain, % | 92.8 | 93.1 | 94.6 |
| Arrived at hospital by EMS, % | 39.1 | 43.0 | 42.5 |
Abbreviations: AMI, acute myocardial infarction; ARIC, Atherosclerosis Risk in Communities; EMS, emergency medical service; nINC, neighborhood household income.
Weighted to account for sampling strategy.
There was no evidence of significant effect modification of the nINC/health insurance–delay time association by race or sex or other selected sociodemographic and medical history variables. Thus, these variables were assessed as covariates in this analysis, and no race- or sex-specific results are presented.
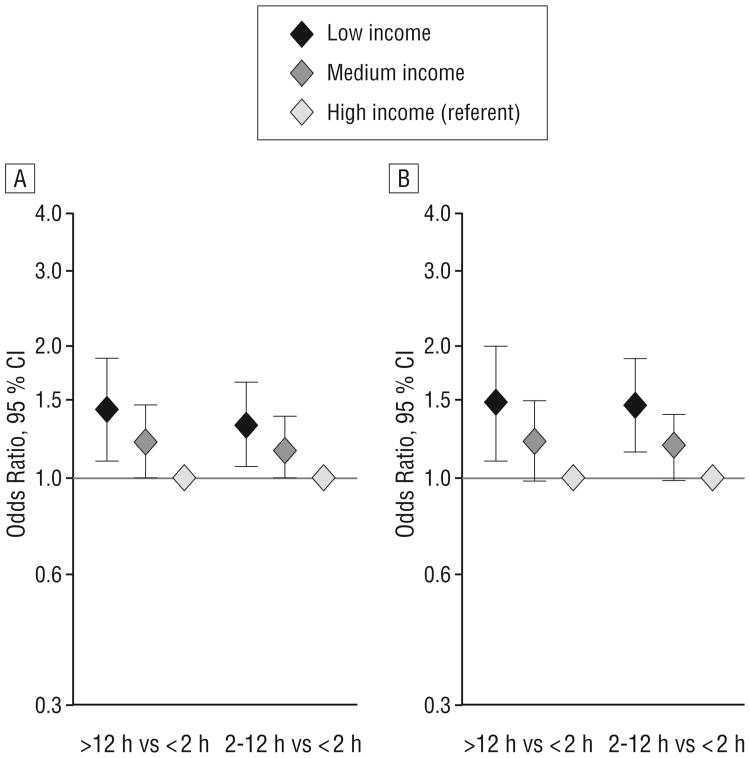
Low nINC was associated with a higher odds of long vs short delay (OR, 1.43; 95% CI, 1.10-1.86) and medium vs short delay (OR, 1.32; 95%CI,1.07-1.63)compared with high nINC in a model including age, sex, race, and study community (Figure 1A). These associations persisted after additionally controlling for health insurance status, diabetes, hypertension, EMS use, chest pain, year of AMI event, and distance from residence to hospital (Figure 1B).
Figure 1.
Odds ratios of prehospital delay in patients with acute myocardial infarction by median household income. A, Basic model: multivariate analysis adjusted for age, sex, race, and study community. B, Adjusted model: basic model plus adjustment for health insurance, diabetes, hypertension, chest pain, emergency medical service use, year of event, and distance from residence to hospital. CI indicates confidence interval.
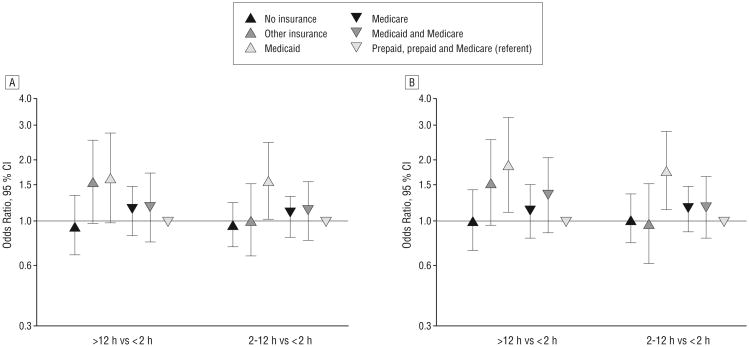
Associations of insurance status with delay time were less consistent. In the minimally adjusted model (Figure 2A), there was generally no significant variation in delay time by insurance status. An exception was that patients with Medicaid were more likely to have a medium vs short delay than were patients with prepaid insurance or prepaid plus Medicare. In models that controlled for additional covariates, compared with patients with prepaid insurance or prepaid plus Medicare, patients with Medicaid were more likely to have a long vs short delay (OR, 1.87; 95% CI, 1.10-3.19) and a medium vs short delay (OR, 1.76; 95% CI, 1.13-2.74) (Figure 2B). Further adjustment for history of angina, AMI, or revascularization did not significantly change the results (data not shown).
Figure 2.
Odds ratios of prehospital delay in patients with acute myocardial infarction by health insurance status. A, Basic model: multivariate analysis adjusted for age, sex, race, and study community. B, Adjusted model: basic model plus adjustment for health insurance, diabetes, hypertension, chest pain, emergency medical service use, year of event, and distance from residence to hospital. CI indicates confidence interval.
We performed supplemental analyses in which hospitalized AMI events were further classified by type of AMI (ST segment elevation myocardial infarction [STEMI] or non-STEMI).30 There was no statistically significant effect modification by type of AMI, nor did its inclusion in models appreciably impact odds ratios (results not shown).
Comment
Receipt of time-dependent AMI treatments within therapeutic windows can lead to better health outcomes following AMI. American College of Cardiology and American Heart Association guidelines recognize that differences in delay time between patients may be due to mode of transportation to the hospital and the ability of the receiving hospital to provide the appropriate treatment; however, they state that “the goal is to keep total ischemic time within 120 minutes.”31(e100) Reperfusion therapy (thrombolytic therapy or percutaneous coronary intervention) is ideally implemented within 12 hours of admission.32
We found that living in a low-income neighborhood and being a Medicaid recipient were independently associated with longer prehospital delay. Researchers have acknowledged socioeconomic barriers to both deciding to seek care and arriving promptly to the hospital following onset of AMI symptoms.7,8,33 One of the hypothesized pathways whereby neighborhood socioeconomic conditions are thought to influence health is through its association with material and infrastructure resources available in the community which serve to strengthen the effects of social stratification.16,34 While neighborhood socioeconomic conditions have been associated with both risk of and mortality following AMI,34,35 its effects on pre-hospital delay for AMI have not been explored prior to this investigation.
With regard to health insurance status, McGinn et al3 found that in the ARIC surveillance communities from 1993 to 2000, delay time did not differ between patients with and without health insurance. However, gaps exist between types of health insurance in terms of reimbursement, receipt of medical procedures, prescription of medication, and health outcomes, including mortality.36,37 For example, Medicaid coverage is extended to certain patients below the federal poverty level38 and has been shown to be negatively associated with delay time.39
Our investigation, therefore, explored subtypes of health insurance. Contrary to our hypothesis, patients with AMI without health insurance were not likely to have a longer delay than patients with prepaid or prepaid and Medicare insurance. In our study, patients with no insurance had a similar nINC distribution as patients with Medicare insurance. Therefore, it is possible the no insurance category comprises misclassified Medicare recipients as well as patients with no health insurance coverage, a proportion of whom have the financial resources to pay for medical care.39 Our findings for Medicaid are consistent with previous research that found that Medicaid recipients experience longer prehospital delay compared with patients with other types of insurance.8,39,40
Most patients (94%) included in our study reported experiencing chest pain. Other studies indicate that chest pain is a commonly reported clinical feature among hospitalized patients with AMI, with estimates ranging from 67% to 95%.6,41,42
A strength of this study is its population-based community surveillance design, which minimizes selection bias by allowing for a representative sample of validated, hospitalized AMI events from the study communities. The ARIC study is currently the only CHD community surveillance study encompassing 4 diverse US communities with a biracial study population that includes male and female subjects who represent a broad age range. A limitation of this study is the retrospective nature of the data collection. The retrospective surveillance design relies on relatively limited socioeconomic patient information in hospital records. However, we were able to use available health insurance status information as an albeit crude proxy for resources to cover medical expenses; furthermore, Medicaid eligibility is based on federal poverty guidelines and thus, provides an indicator of unfavorable individual SES in this population. In addition, we are unable to elucidate the possible processes concerning the association between low nINC (and Medicaid recipient status) and increased prehospital delay. For example, our investigation was only able to capture overall prehospital delay (ie, the time elapsed between onset of symptoms and hospital arrival). However, “decision delay” (ie, the time following the onset of symptoms that patients spend weighing their options and deciding whether to go to the hospital) is thought to be a major component of prehospital delay time.43 Lack of access to transportation, telephone service, slower EMS response times, and living alone are other factors that may also negatively affect prehospital delay time or prohibit the patient from arriving at the hospital at all. Having more detailed information on both decision delay and various transport delays would be optimal because it would allow for more effectively targeted interventions to reduce prehospital delay. In addition, individuals with AMI dying before hospital arrival were not included in the analysis. Individuals declared deceased on hospital arrival or who died during transport to the hospital are not admitted and thus do not have a prehospital delay time nor a validated AMI event. It is possible that such individuals predominantly live in similar nINC areas or are overrepresented in select insurance categories, which may be a source of selection bias in this study.
Reducing socioeconomic and insurance disparities in prehospital delay is critical because excess delay time may hinder effective care for AMI. Prolonged prehospital delay among patients from low nINC areas and among Medicaid recipients suggests a need for increased recognition of and rapid response to AMI symptoms within these populations. Interventions that have been considered include the following: community education and awareness campaigns,44 targeted interventions by health care professionals aimed at reducing prehospital delay among patients with known CHD,45-47 and promoting EMS use throughout the community.48
Future research aimed at identifying neighborhood structural or organizational factors that could be the target of a public health intervention to improve access to care and patients' response to AMI symptoms is warranted.
Acknowledgments
Funding/Support: This research was supported by contract 1R01HL080287 from the National Heart, Lung, and Blood Institute (NHLBI) and was also funded in part by National Institutes of Health, NHLBI, and National Research Service Award training grant 5-T32-HL007055-30 (Ms Foraker). The ARIC study is carried out as a collaborative study supported by NHLBI contracts N01-HC-55015, N01-HC-55016, N01-HC-55018, N01-HC-55019, N01-HC-55020, N01-HC-55021, and N01-HC-55022.
Footnotes
Author Contributions: Study concept and design: Foraker, Rose, Goff, and Rosamond. Acquisition of data: Foraker, Rose, and Wood. Analysis and interpretation of data: Foraker, Rose, McGinn, Suchindran, Goff, Whitsel, Wood, and Rosamond. Drafting of the manuscript: Foraker and Rose. Critical revision of the manuscript for important intellectual content: Foraker, Rose, McGinn, Suchindran, Goff, Whitsel, and Rosamond. Statistical analysis: Foraker, Rose, and Suchindran. Obtained funding: Rose and Rosamond. Administrative, technical, and material support: Rose and Whitsel. Study supervision: Rose.
Financial Disclosure: None reported.
Previous Presentation: This study was presented as an abstract (February 28, 2007) and poster (March 2, 2007) at the 47th Cardiovascular Disease Epidemiology and Prevention Conference; February 28–March 3, 2007; Orlando, Florida.
Additional Contributions: We thank the staff and participants of the ARIC study for their important contributions.
References
- 1.Krumholz HM, Anderson JL, Brooks NH, et al. American College of Cardiology/American Heart Association Task Force on Performance Measures; Writing Committee to Develop Performance Measures on ST-Elevation and Non-ST-Elevation Myocardial Infarction. ACC/AHA clinical performance measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Performance Measures on ST-Elevation and Non-ST-Elevation Myocardial Infarction) Circulation. 2006;113(5):732–761. doi: 10.1161/CIRCULATIONAHA.106.172860. [DOI] [PubMed] [Google Scholar]
- 2.Ryan TJ, Antman EM, Brooks NH, et al. 1999 update: ACC/AHA Guidelines for the Management of Patients With Acute Myocardial Infarction: Executive Summary and Recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) Circulation. 1999;100(9):1016–1030. doi: 10.1161/01.cir.100.9.1016. [DOI] [PubMed] [Google Scholar]
- 3.McGinn AP, Rosamond WD, Goff DC, Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987-2000. Am Heart J. 2005;150(3):392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994-1997) in, prehospital delay in patients with acute myocardial infarction: the second National Registry of Myocardial Infarction. Arch Intern Med. 1999;159(18):2141–2147. doi: 10.1001/archinte.159.18.2141. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg RJ, Yarzebski J, Lessard D, Gore Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: the Worcester Heart Attack study. Arch Intern Med. 2000;160(21):3217–3223. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg RJ, Steg PG, Sadiq I, et al. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry) Am J Cardiol. 2002;89(7):791–796. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 7.Sheifer SE, Rathore SS, Gersh BJ, et al. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation. 2000;102(14):1651–1656. doi: 10.1161/01.cir.102.14.1651. [DOI] [PubMed] [Google Scholar]
- 8.Goff DC, Jr, Feldman HA, McGovern PG, et al. Rapid Early Action for Coronary Treatment (REACT) Study Group. Prehospital delay in patients hospitalized with heart attack symptoms in the United States: the REACT trial. Am Heart J. 1999;138(6, pt 1):1046–1057. doi: 10.1016/s0002-8703(99)70069-4. [DOI] [PubMed] [Google Scholar]
- 9.Meischke H, Larsen MP, Eisenberg MS. Gender differences in reported symptoms for acute myocardial infarction: impact on prehospital delay time interval. Am J Emerg Med. 1998;16(4):363–366. doi: 10.1016/s0735-6757(98)90128-0. [DOI] [PubMed] [Google Scholar]
- 10.Grossman SA, Brown DFM, Chang Y, et al. Predictors of delay in presentation to the ED in patients with suspected acute coronary syndromes. Am J Emerg Med. 2003;21(5):425–428. doi: 10.1016/s0735-6757(03)00106-2. [DOI] [PubMed] [Google Scholar]
- 11.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robert SA. Neighborhood socioeconomic context and adult health: the mediating role of individual health behaviors and psychosocial factors. Ann N Y Acad Sci. 1999;896:465–468. doi: 10.1111/j.1749-6632.1999.tb08171.x. [DOI] [PubMed] [Google Scholar]
- 13.Yen IH, Kaplan GA. Neighborhood social environment and risk of death: multilevel evidence from the Alameda County Study. Am J Epidemiol. 1999;149(10):898–907. doi: 10.1093/oxfordjournals.aje.a009733. [DOI] [PubMed] [Google Scholar]
- 14.Diez-Roux AV, Nieto FJ, Caulfield L, Tyroler H, Watson R, Szklo M. Neighbourhood differences in diet: the Atherosclerosis Risk in Communities (ARIC) Study. J Epidemiol Community Health. 1999;53(1):55–63. doi: 10.1136/jech.53.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am J Public Health. 2006;96(2):325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaix B, Rosvall M, Merlo J. Neighborhood socioeconomic deprivation and residential instability: effects on incidence of ischemic heart disease and survival after myocardial infarction. Epidemiology. 2007;18(1):104–111. doi: 10.1097/01.ede.0000249573.22856.9a. [DOI] [PubMed] [Google Scholar]
- 17.Diez-Roux AV, Evenson KR, McGinn AP, et al. Availability of recreational resources and physical activity in adults. Am J Public Health. 2007;97(3):493–499. doi: 10.2105/AJPH.2006.087734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schechter MS, Shelton BJ, Margolis PA, Fitzsimmons SC. The association of socioeconomic status with outcomes in cystic fibrosis patients in the United States. Am J Respir Crit Care Med. 2001;163(6):1331–1337. doi: 10.1164/ajrccm.163.6.9912100. [DOI] [PubMed] [Google Scholar]
- 19.Morgan MA, Behbakht K, Benjamin I, Berlin M, King SA, Rubin SC. Racial differences in survival from gynecologic cancer. Obstet Gynecol. 1996;88(6):914–918. doi: 10.1016/s0029-7844(96)00342-0. [DOI] [PubMed] [Google Scholar]
- 20.The ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129(4):687–702. [PubMed] [Google Scholar]
- 21.Armstrong D, Wing S, Tyroler HA. Race differences in estimates of sudden coronary heart disease mortality, 1980-1988: the impact of ill-defined death. J Clin Epidemiol. 1996;49(11):1247–1251. doi: 10.1016/s0895-4356(96)00217-x. [DOI] [PubMed] [Google Scholar]
- 22.White AD, Folsom AR, Chambless LE, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years' experience. J Clin Epidemiol. 1996;49(2):223–233. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 23.Alonzo AA. The impact of physician consultation on care-seeking during acute episodes of coronary heart disease. Med Care. 1977;15(1):34–50. doi: 10.1097/00005650-197701000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Atherosclerosis Risk in Communities Study. ARIC Protocol 3: Surveillance Component Procedures, Version 4.1. Chapel Hill, NC: Collaborative Studies Coordinating Center; Mar 1998, [Accessed January 23, 2008]. http://www.cscc.unc.edu/aric/visit/Surveillance_Procedures_-_Coronary_Heart_Disease.1_3.pdf. [Google Scholar]
- 25.Whitsel EA, Rose KM, Wood JL, Henley AC, Liao D, Heiss G. Accuracy and repeatability of commercial geocoding. Am J Epidemiol. 2004;160(10):1023–1029. doi: 10.1093/aje/kwh310. [DOI] [PubMed] [Google Scholar]
- 26.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156(5):471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 27.Krieger N, Jarvis TC, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the public health disparities geocoding project. Am J Public Health. 2003;93(10):1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Diez-Roux AV, Kiefe CI, Jacobs DR, et al. Area characteristics and individual level socioeconomic position indicators in three population-based epidemiologic studies [published correction appears in Ann Epidemiol. 2001;30(4):924] Ann Epidemiol. 2001;11(6):395–405. doi: 10.1016/s1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- 29.Diez-Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 30.Watkins S, Thiemann D, Coresh J, Powe N, Folsom AR, Rosamond W. Fourteen-year (1987 to 2000) trends in the attack rates of, therapy for, and mortality from non-ST-elevation acute coronary syndromes in four United States communities. Am J Cardiol. 2005;96(10):1349–1355. doi: 10.1016/j.amjcard.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 31.Antman EM, Anbe DT, Armstrong PW, et al. American College of Cardiology; American Heart Association Task Force on Practice Guidelines; Canadian Cardiovascular Society. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocar-dial Infarction) [published corrections appear in Circulation. 2005;111(15):2013-2014; and Circulation. 2007;115(15):e411] Circulation. 2004;110(9):e82–e292. [PubMed] [Google Scholar]
- 32.Ryan TJ, Anderson JL, Antman EM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) Circulation. 1996;94(9):2341–2350. doi: 10.1161/01.cir.94.9.2341. [DOI] [PubMed] [Google Scholar]
- 33.Ghali JK, Cooper RS, Kowatly I, Liao Y. Delay between onset of chest pain and arrival to the coronary care unit among minority and disadvantaged patients. J Natl Med Assoc. 1993;85(3):180–184. [PMC free article] [PubMed] [Google Scholar]
- 34.Stjärne MK, Fritzell J, De Leon AP, Hallqvist J. Neighborhood socioeconomic context, individual income and myocardial infarction. Epidemiology. 2006;17(1):14–23. doi: 10.1097/01.ede.0000187178.51024.a7. [DOI] [PubMed] [Google Scholar]
- 35.Chang WC, Kaul P, Westerhout CM, Graham MM, Armstrong PW. Effects of socioeconomic status on mortality after acute myocardial infarction. Am J Med. 2007;120(1):33–39. doi: 10.1016/j.amjmed.2006.05.056. [DOI] [PubMed] [Google Scholar]
- 36.Wang NE, Gisondi MA, Golzari M, van der Vlugt TM, Tuuli M. Socioeconomic disparities are negatively associated with pediatric emergency department aftercare compliance. Acad Emerg Med. 2003;10(11):1278–1284. doi: 10.1197/s1069-6563(03)00499-8. [DOI] [PubMed] [Google Scholar]
- 37.Calvin JE, Roe MT, Chen AY, et al. Insurance coverage and care of patients with non-st-segment elevation acute coronary syndromes. Ann Intern Med. 2006;145(10):739–748. doi: 10.7326/0003-4819-145-10-200611210-00006. [DOI] [PubMed] [Google Scholar]
- 38.Rosenbaum S. Medicaid. N Engl J Med. 2002;346(8):635–640. doi: 10.1056/NEJM200202213460825. [DOI] [PubMed] [Google Scholar]
- 39.Brown DL, Schneider DL, Colbert R, Guss D. Influence of insurance coverage on delays in seeking emergency care in patients with acute chest pain. Am J Cardiol. 1998;82(3):395–398. doi: 10.1016/s0002-9149(98)00338-5. [DOI] [PubMed] [Google Scholar]
- 40.Gurwitz JH, Goldberg RJ, Malmgren JA, et al. Hospital transfer of patients with acute myocardial infarction: the effects of age, race, and insurance type. Am J Med. 2002;112(7):528–534. doi: 10.1016/s0002-9343(02)01072-0. [DOI] [PubMed] [Google Scholar]
- 41.Goldberg R, Goff DC, Jr, Cooper L, et al. Age and sex differences in presentation of symptoms among patients with acute coronary disease: the REACT trial: Rapid Early Action for Coronary Treatment. Coron Artery Dis. 2000;11(5):399–407. doi: 10.1097/00019501-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Canto JG, Shlipak MG, Rogers WJ, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283(24):3223–3229. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 43.Taylor DM, Garewal D, Carter M, Bailey M, Aggarwal A. Factors that impact upon the time to hospital presentation following the onset of chest pain. Emerg Med Australas. 2005;17(3):204–211. doi: 10.1111/j.1742-6723.2005.00724.x. [DOI] [PubMed] [Google Scholar]
- 44.Kildemoes HW, Kristiansen IS. Cost-effectiveness of interventions to reduce the thrombolytic delay for acute myocardial infarction. Int J Technol Assess Health Care. 2004;20(3):368–374. doi: 10.1017/s0266462304001205. [DOI] [PubMed] [Google Scholar]
- 45.Dracup K, Alonzo AA, Atkins JM, et al. Working Group on Educational Strategies To Prevent Prehospital Delay in Patients at High Risk for Acute Myocardial Infarction. The physician's role in minimizing prehospital delay in patients at high risk for acute myocardial infarction: recommendations from the National Heart Attack Alert Program. Ann Intern Med. 1997;126(8):645–651. doi: 10.7326/0003-4819-126-8-199704150-00010. [DOI] [PubMed] [Google Scholar]
- 46.Dracup K, McKinley S, Riegel B, Mieschke H, Doering LV, Moser DK. A nursing intervention to reduce prehospital delay in acute coronary syndrome: a randomized clinical trial. J Cardiovasc Nurs. 2006;21(3):186–193. doi: 10.1097/00005082-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 47.Blank FSJ, Smithline HA. Evaluation of an educational video for cardiac patients. Clin Nurs Res. 2002;11(4):403–416. doi: 10.1177/105477302237453. [DOI] [PubMed] [Google Scholar]
- 48.Osganian SK, Zapka JG, Feldman H, et al. REACT Study Group; Rapid Early Action for Coronary Treatment. Use of emergency medical services for suspected acute cardiac ischemia among demographic and clinical patient subgroups: the REACT trial: Rapid Early Action for Coronary Treatment. Prehosp Emerg Care. 2002;6(2):175–185. doi: 10.1080/10903120290938517. [DOI] [PubMed] [Google Scholar]