Abstract
Background: Tuberculosis (TB) and human immunodeficiency virus (HIV) co-infection remains high in Rwanda. Since one-stop TB-HIV services were implemented to manage TB-HIV co-infection, their functioning and impact on TB treatment outcomes have not been assessed.
Objective: To evaluate one-stop TB-HIV services in Rwanda by comparing the TB treatment outcomes before and after their implementation in Kicukiro and Rulindo districts.
Methods: This descriptive retrospective study used a quantitative questionnaire to determine the functioning of Rwanda's one-stop TB-HIV services. In-depth interviews and focus group discussions with health care providers, heads of facilities and co-infected patients were held to seek their opinion about the functioning of the services.
Results: The one-stop TB-HIV services at all 12 health facilities visited were functioning according to the approved criteria. However, TB treatment outcomes after the intervention were not statistically different from those before the intervention. Qualitative data showed a positive impact on the quality of service, particularly a reduction in waiting times and appointments that were better respected as a result of the efficient functioning of the services.
Conclusion: One-stop TB-HIV services have improved the quality of service in Kicukiro and Rulindo districts. However, the services need to be strengthened programmatically to improve TB treatment outcomes.
Keywords: services integration, LMICs, programme evaluation
Abstract
Contexte : Une co-infection par la tuberculose (TB) et le virus de l'immunodéficience humaine (VIH) reste fréquente au Rwanda. Depuis que des services TB-VIH à guichet unique ont été mis en œuvre afin de prendre en charge cette co-infection TB-VIH, leur fonctionnement et leur impact sur les résultats du traitement de la TB n'ont pas été évalués.
Objectif : Evaluer les services TB-VIH à guichet unique du Rwanda, en comparant les résultats du traitement de la TB avant et après leur mise en œuvre, dans les districts de Kicukiro et Rulindo.
Méthodes : Un étude descriptive rétrospective et un questionnaire quantitatif ont permis de connaître le fonctionnement du service TB-VIH à guichet unique ; des entretiens approfondis et des discussions en groupes focaux avec les prestataires de soins, les directeurs des structures et les patients co-infectés ont permis de connaître leur opinion à propos du fonctionnement.
Résultats : Après la mise en œuvre des services TB-VIH à guichet unique, les 12 structures de santé visitées fonctionnaient selon les critères établis. Cependant, les résultats du traitement de la TB n'ont pas été significativement différents avant et après l'intervention. Les données qualitatives ont mis en évidence un effet positif de l'intervention sur la qualité de service, notamment sur la réduction du temps d'attente, et sur un meilleur respect des rendez-vous en réponse au bon fonctionnement du service.
Conclusion : Les services TB-VIH à guichet unique ont amélioré la qualité des services dans les districts de Kicukiro et Rulindo. Cependant, le service doit être renforcé en termes de programme afin d'améliorer les résultats du traitement de la TB.
Abstract
Marco de referencia: La frecuencia de coinfección por el bacilo de la tuberculosis (TB) y el virus de la inmunodeficiencia humana (VIH) sigue siendo alta en Rwanda. Desde que se introdujeron los servicios de ‘ventanilla única’ de atención de la TB y la infección por el VIH con el fin de atender a los pacientes aquejados de coinfección no se ha llevado a cabo una evaluación de su funcionamiento ni de su impacto sobre los desenlaces terapéuticos de la TB.
Objetivo: Evaluar los servicios de ventanilla única de atención de la TB y la infección por el VIH en Rwanda, mediante la comparación de los desenlaces del tratamiento antituberculoso antes y después de la introducción de los servicios en los distritos de Kicukiro y Rulindo.
Métodos: Fue este un estudio descriptivo retrospectivo, en el cual se administró un cuestionario cuantitativo con el fin de conocer el funcionamiento de los servicios de ventanilla única; se practicaron entrevistas exhaustivas y debates en grupos de opinión dirigidos a los profesionales de salud, los gestores de establecimientos y los pacientes aquejados de coinfección con el objeto de conocer sus opiniones sobre el funcionamiento de los servicios.
Resultados: Después de la introducción de los servicios de ventanilla única de atención de la TB y la infección por el VIH, los 12 establecimientos visitados funcionaban de conformidad con los criterios fijados. Sin embargo, los desenlaces del tratamiento antituberculoso después de haber iniciado la intervención no fueron estadísticamente mejores que los resultados anteriores a la misma. Los datos cualitativos pusieron en evidencia un efecto positivo de la intervención sobre la calidad del servicio, sobre todo con respecto al tiempo de espera y al cumplimiento de las citas, como resultado del buen funcionamiento del servicio.
Conclusión: El sistema de ventanilla única de atención de la TB y la infección por el VIH ha mejorado la calidad de los servicios prestados en los distritos de Kicukiro y Rulindo. Sin embargo, se precisa un refuerzo programático encaminado a mejorar los desenlaces del tratamiento antituberculoso.
Of the 33.2 million persons infected worldwide with the human immunodeficiency virus (HIV), one third are estimated to be co-infected with Mycobacterium tuberculosis. In 2008, there were an estimated 1.4 million new cases of tuberculosis (TB) among persons with HIV infection, and TB accounted for 26% of acquired immune-deficiency syndrome (AIDS) related deaths. The relative risk of TB among HIV-infected persons, compared with that among non-HIV-infected persons, ranges from 20- to 37-fold, depending on the severity of the HIV epidemic. In 2008, 1.4 million TB patients globally were tested for HIV, and 81 countries, of which many are located in sub-Saharan Africa, tested more than half of their TB patients for HIV. Only 4% of all HIV-infected persons were screened for TB in the same year. The decentralisation of HIV treatment services and the strengthening of their integration with TB services are essential.1
In Rwanda, the TB-specific fatality rate is 7.5% and TB is the most common opportunistic infection among people living with HIV/AIDS (PLWHA). However, the number of TB cases has doubled during the last 10 years, and almost 40% are HIV-positive.2 A study conducted at the Gisenyi hospital in Gisenyi, Rwanda, on TB-HIV integration between June 2005 and July 2006 showed that 55% of TB out-patients did not know their HIV status, and that once tested, 29% were co-infected.2,3 Rwanda has implemented a ‘one-stop TB-HIV service’ approach, one of the strategies recommended by the World Health Organization (WHO) for collaborative TB-HIV activities to address the burden of TB and HIV.4,5 It took one year for the TB-HIV collaborative activities policy to be drafted and approved in 2005, and the implementation of one-stop TB-HIV services was meant to start early in 2006.6
The approach adopted by Rwanda includes: 1) providing HIV counselling and testing (HCT) to TB patients in TB clinics; 2) treating and caring for co-infected patients in the TB clinic; 3) transferring HIV-infected patients to an HIV clinic at the end of TB treatment to continue antiretroviral treatment (ART) and care; 4) systematic screening of all HIV patients for TB at clinic appointments; and 5) contact tracing for TB patients via home-based visits and HIV testing or TB screening for family members.
This article describes the rate of compliance with these criteria and their effect on TB treatment outcomes among TB-HIV patients in Kicukiro and Rulindo districts in Rwanda. Both Kicukiro and Rulindo districts are concerned with the implementation of one-stop TB-HIV services, as recommended by the Rwandan National TB Programme, by complying with all the above-mentioned criteria. This was undertaken after an evaluation of the collaborative TB-HIV services showed that scale-up was necessary.6
STUDY POPULATION AND METHODS
Setting and study population
This descriptive retrospective study used quantitative and qualitative approaches to assess the one-stop TB-HIV services by comparing the periods before and after their implementation. The study was carried out in Rulindo district in Northern Province and Kicukiro district in Kigali City, which respectively represent rural and urban areas of Rwanda. Of the 29 health facilities (HFs) available in both districts, 12 (42%) facilities with one-stop TB-HIV services were visited. All the TB-HV records for 2001–2010 were reviewed. Nurses in charge of the services and heads of facilities were included in the study due to their responsibility in the services, and TB-HIV patients were included as beneficiaries of the services. All other staff and all patients with infections other than TB-HIV were excluded. All treatment outcomes were reviewed, excluding transfers out, as these were followed up in other HFs during the study period.
Data collection
The TB registers, ART registers and patients' ART and TB files were reviewed for data on HCT, cotrimoxazole preventive therapy (CPT) and ART initiation, TB screening and testing, CD4 evolution and TB treatment outcomes through one questionnaire per site with head nurses of the one-stop TB-HIV services.
Focus group discussions (FGDs) with 6–12 mixed sex co-infected patients were conducted to collect data about their appreciation of the quality and challenges of the one-stop TB-HIV services. In-depth interviews (IDI) were also conducted to capture the perceptions of the nurses in charge and the heads of the HFs on the services, as well as lessons to share and areas for improvement.
Data were collected for the period from January 2001 to December 2010 by two trained data collectors. FGDs and interviews were recorded in addition to field note-taking, and IDIs and FGD field notes were expanded with transcriptions before the next field study. Both quantitative and qualitative data were collected from July to December 2011.
Data analysis
Quantitative data were verified and entered into Epi Info 3.5.1 (US Centers for Disease Control and Prevention, Atlanta, GA, USA). Data were exported to Microsoft Excel (Microsoft Corp., Redmond, WA, USA) and then to SPSS 16.0 (SPSS Inc., Chicago, IL, USA) for analysis. To determine HCT coverage among TB patients, TB screening and testing among PLWHA, CPT and ART initiation and CD4 count evolution, descriptive statistics were computed. To compare TB treatment outcomes between before and after the implementation of the one-stop TB-HIV services, a χ2 test was computed. Results were significant, at P < 0.05, through a comparison between the before and after service implementation periods.
Qualitative data were manually analysed with content coding from the main themes of the FGDs and IDIs. All ideas were categorised around the corresponding codes to be able to determine the saturation of the respondents' ideas and opinions about the one-stop TB-HIV services. Finally, triangulation was carried out between quantitative and qualitative findings to come up with the final discussion, conclusion and recommendations.
Ethical approval was obtained from the University of Rwanda School of Public Health; authorisation to access health services data was obtained from the Rwanda Ministry of Health.
RESULTS
Quantitative results
Of the 12 HFs visited, nine were health centres (HCs) and three were hospitals. Data from registers, ART files and TB treatment cards were reviewed for 600 patients in Kicukiro and 3095 patients in Rulindo, and the questionnaires were administered at the 12 health facilities to capture aggregated data on the functioning of the services. The unit of analysis was the health facility; no demographics were collected.
In Kicukiro, the six HFs did not initiate the one-stop TB-HIV services at the same time. The Kicukiro HC started in 2006, the Kabuga HC in 2007, the Gikondo HC and Masaka HC in 2009 and the Carrefour clinic and Rwanda Military Hospital in 2010. In Rulindo, all six HCs began in 2009 and all were functional in both districts. All HFs were supported by the Rwandan Ministry of Health in TB-HIV services management. All the head nurses of Rulindo were trained in 2009, but in Kicukiro the head nurses were trained at different times between 2007 and 2012. In all 12 HFs, TB-HIV patients followed in the one-stop TB-HIV service received combined TB and HIV services in a single location, i.e., the TB clinic.
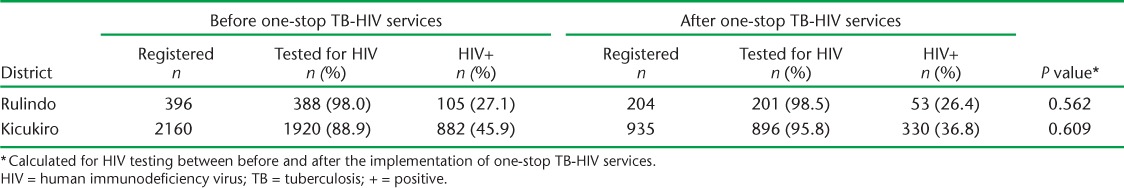
In all 12 HFs, following the service implementation, HCT was undertaken for presumed TB cases and for TB patients who did not know their HIV status. Prior to implementation, no patients with presumed TB had been counselled and tested for HIV, but respectively 2324 (74.8%) and 2401 (54.4%) received HCT in Rulindo and Kicukiro following implementation. Almost all TB patients underwent HCT before and after the service implementation; the difference was not statistically significant (Table 1).
TABLE 1.
HIV counselling and testing for TB cases
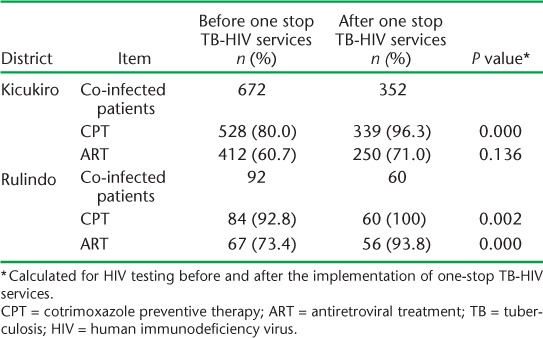
CPT initiation increased from 80% before to 96.3% after implementation in Kicukiro (P = 0.000) and from 92.8% to 100% in Rulindo (P = 0.002). ART initiation increased from 60.7% to 71% in Kicukiro (P = 0.136) and from 73.4% to 93.8% in Rulindo (P = 0.000) (Table 2).
TABLE 2.
CPT and ART initiation among co-infected patients before and after the intervention
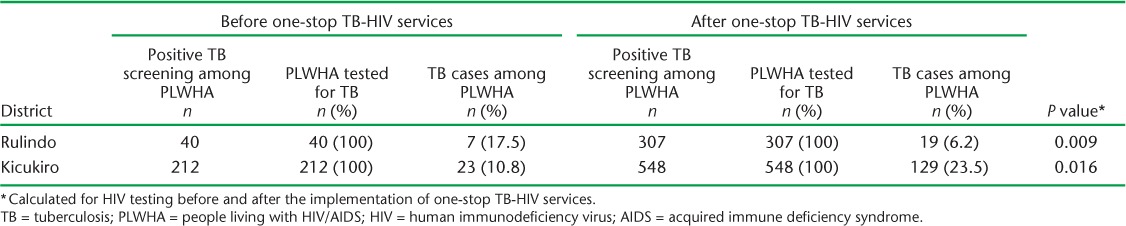
TB screening was systematic in all 12 facilities. Among HIV-infected clients with a positive TB screen (defined as those who responded ‘yes’ to any of the five screening questions posed) before the one-stop TB-HIV services in Rulindo district, all 40 positively screened were tested for TB, and 7 (17.5%) were diagnosed with active TB. After the service, among 307 positively screened patients, 307 (100%) were tested, and 19 (6.2%) were found to be TB-positive. In Kicukiro district, before the service, all 212 positively screened patients were tested for TB and 23 (10.8%) were diagnosed with active TB. After the service, all 548 positively screened patients were tested and 129 (23.5%) were diagnosed with active TB (Table 3).
TABLE 3.
TB testing and TB prevalence among PLWHA, 2006–2010
Prior to implementation of the one-stop TB-HIV services, the CD4 counts increased from 240 cells/μl at the beginning of TB treatment to 360 cells/μl at the end. After implementation they increased from 200 cells/μl to 350 cells/μl in both districts.
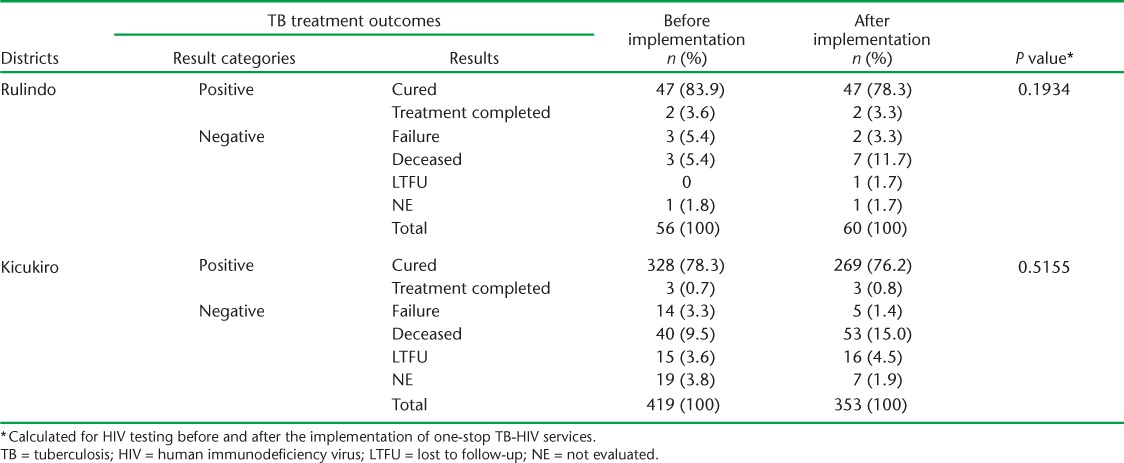
Comparing the two periods, there was no difference in proportions of positive (cured or treatment completed) and negative (deceased, lost to follow-up, treatment failure or not evaluated) TB treatment outcomes in Rulindo (P = 0.193) or Kicukiro (P = 0.516) (Table 4).
TABLE 4.
TB treatment outcomes among co-infected patients before and after the implementation of one-stop TB-HIV services, 2001–2010
Qualitative results
To evaluate the perceptions and opinions of the HF staff and patients of the one-stop TB-HIV services, one IDI with the head of facility, one with the nurse in charge, and one FGD with co-infected patients was conducted per health facility, for a total of 24 IDIs and 12 FGDs.
All the respondents reported that they were happy with the implementation of the one-stop TB-HIV services because the patients were offered services quickly and in a single location, which had a positive impact on service quality.
Before TB infection, we were considered like other patients with all what you know about it; but now, all services are offered once and in one service. The service nurse takes care of us at high level and we have become friends.
(FGD participant)
The nurses in charge and the heads of facilities reported that the combined approach also prevented co-infected patients from infecting other PLWHA who are already weak. However, the respondents highlighted some reasons why patients did not experience improvements in their general status after anti-tuberculosis treatment, such as insufficient nutrition, lack of financial support, etc.
You can have these drugs for both TB and HIV and stay in a critical status because to improve you need also to eat well in quality and in quantity like flour and sugar, et cetera, to make CD4 counts increase.
(FGD participant)
Health facility-related challenges included staff turnover after training, a lack of designated staff for the service (nurses and data manager), community health workers (CHWs) who were not motivated, problems in the infrastructure, etc.
At the end, you see that the only one who is trained is self estimated as the most important person at the facility, which ends up with a high turnover of the trained staff, because they are still looking for the most incentivised work.
(IDI participant)
DISCUSSION
We conducted this study to assess the functioning of one-stop TB-HIV services by comparing TB treatment outcomes among TB-HIV patients before and after implementation of these services in Rwanda.
All the one-stop TB-HIV services were working according to the determined criteria, but they had not been implemented at the same time. The implementation of the services might depend on the commitment, resources and infrastructures of the HFs, and especially their infection control design. Many countries are still facing this building challenge,7 and efforts have been deployed by the Rwandan Ministry of Health to address it. Nurses have been trained, but the high turnover of trained staff has worsened the situation. This is a big challenge in health systems strengthening in resource-limited settings.8
The proportion of patients offered HCT increased significantly after the service implementation, in particular in Rulindo, a rural area. There are many factors behind the low uptake of HIV testing in urban areas, such as age, sex, employment status, HF level and previous HCT.9 HCT serves as an entry point to HIV/AIDS care and treatment10 or to co-infection enrolment.11 Current Rwandan figures show that 99% of all forms of TB cases know their HIV status—a big achievement.12
CPT and ART initiation increased after the service implementation in both districts, in particular in Rulindo district. The early initiation of ART among TB patients saves the lives of many co-infected patients,11,13–15 as HIV is an important predictor of mortality among co-infected patients.16 Current Rwandan figures show that respectively 98% and 90% of co-infected patients are on CPT and ART, another achievement across the region.12
HFs were performing well in TB screening, a general situation in sub-Saharan Africa, where 48–100% of HIV-positive patients are screened for TB.16 After a positive TB screen, testing was performed for all eligible patients, irrespective of HF location or level. This is common in sub-Saharan Africa, where sputum smear microscopy is widely available at all levels and X-ray is available in secondary and tertiary level facilities.17
Although the CD4 cell count increased during anti-tuberculosis treatment, there was no increase after service implementation and this would be a good predictor of death. One of the reasons why TB patients do not experience an improvement in their immunological status or even die during treatment, irrespective of HIV status, is malnutrition,10,18 especially in vulnerable groups.1,15 In addition to early initiation of ART, counselling for effective adherence and nutritional support would improve the CD4 counts and prevent the high mortality rate among co-infected patients.9,16,19
Both positive and negative anti-tuberculosis treatment outcomes were statistically the same before and after the intervention in the two districts. Some of the reasons highlighted for this included the lack of sufficient food for the patients, a lack of permanent trained staff in the service in some HFs, lack of staff motivation and fear of being infected by TB. However, there were many positive outcomes, such as a reduction in waiting times, adherence to the programme, respect for privacy and specific staff in charge of the service. We expect to see treatment outcomes improve, as many challenges were addressed and this could serve as lessons learnt for similar settings.2,11,14,20
Study limitations
Our study has several limitations. Poor documentation remains a big challenge in Rwanda6 and other sub-Saharan African countries.20,21 The analysis was based on the existing records of HFs, which had missing data and outcome ascertainment. The inability to control for confounders in the facilities visited affected the capacity to determine the impact of the programme. Very few facilities were visited, and few data were recorded due to funding limitations. This analysis nonetheless represents a real picture of the programme in the districts visited, and informs the policy on room for improvement towards better TB treatment outcomes.
CONCLUSION
The implementation of one-stop TB-HIV services in Rwanda has improved service quality in terms of a reduction in waiting times and an increase in patient adherence, as confirmed by both patients and HF staff. Study participants suggested several strategies to improve TB treatment outcomes, such as better infrastructure, staff retention, data management, ongoing training on ART and TB for a sufficient number of staff, strengthening the involvement of community health workers in TB activities, especially in urban areas, nutritional support for all TB-HIV patients and involvement of private HFs in TB activities.
As this study assessed only 12 HFs in two districts, a further nationwide study would provide a more accurate snapshot of the situation, as TB-HIV patients are normally few.
Acknowledgments
The paper was developed by AN for his Master's dissertation.
The authors acknowledge the financial support for data collection from the Rwanda Biomedical Center, TB and Other Respiratory Diseases Division, Kigali, Rwanda, under the leadership of M Gasana. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official view of the donors.
We thank all the visited health facilities staff and the patients who participated in this study.
Footnotes
Conflicts of interest: none declared.
References
- 1.Getahun H, Gunneberg C, Granich R, Nunn P. HIV infection-associated tuberculosis: the epidemiology and the response. Clin Infect Dis. 2010;50(Suppl 3):S201–S207. doi: 10.1086/651492. [DOI] [PubMed] [Google Scholar]
- 2.Gasana M, Vandebriel G, Kabanda G et al. Integrating tuberculosis and HIV care in rural Rwanda. Int J Tuberc Lung Dis. 2008;12(Suppl 1):S39–S43. [PMC free article] [PubMed] [Google Scholar]
- 3.Gasana M, Vandebriel G, Kabanda G et al. Tuberculosis in Rwanda: challenges to reaching the targets. Bull World Health Organ. 2007;85:383–384. [Google Scholar]
- 4.World Health Organization. WHO policy on collaborative TB/HIV activities: guidelines for national programmes and other stakeholders. Geneva, Switzerland: WHO; 2012. WHO/HTM/TB/2012.1. [PubMed] [Google Scholar]
- 5.World Health Organization. Interim policy on collaborative TB/HIV activities. Geneva, Switzerland: WHO; 2004. WHO/HTM/TB/2004.330. WHO/HTM/HIV/2004.1. [Google Scholar]
- 6.Pevzner E S, Vandebriel G, Lowrance D W, Gasana M, Finley A. Evaluation of the rapid scale-up of collaborative TB/HIV activities in TB facilities in Rwanda, 2005–2009. BMC Public Health. 2011;11:550. doi: 10.1186/1471-2458-11-550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bock N N, Jensen P A, Miller B, Nardell E. Tuberculosis infection control in resource-limited settings in the era of expanding HIV care and treatment. J Infect Dis. 2007;196(Suppl 1):S108–S113. doi: 10.1086/518661. [DOI] [PubMed] [Google Scholar]
- 8.Laserson K F, Wells C D. Reaching the targets for tuberculosis control: the impact of HIV. Bull World Health Organ. 2007;85:377–381. doi: 10.2471/06-035329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sendagire I, Schreuder I, Mubiru M, van der Loeff M S, Cobelens F, Konde-Lule J. Low HIV testing rates among tuberculosis patients in Kampala, Uganda. BMC Public Health. 2010;10:177. doi: 10.1186/1471-2458-10-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howard A A, El-Sadr W M. Integration of tuberculosis and HIV services in sub-Saharan Africa: lessons learned. Clin Infect Dis. 2010;50(Suppl 3):S238–S244. doi: 10.1086/651497. [DOI] [PubMed] [Google Scholar]
- 11.Harris J B, Hatwiinda S M, Randels K M et al. Early lessons from the integration of tuberculosis and HIV services in primary care centers in Lusaka, Zambia. Int J Tuberc Lung Dis. 2008;12:773–779. [PubMed] [Google Scholar]
- 12.Rwanda Biomedical Center. Tuberculosis facts information summary, 2014. Kigali, Rwanda: Rwanda Biomedical Center; 2015. [Google Scholar]
- 13.Hermans S M, Leth F, Manabe Y C et al. Earlier initiation of antiretroviral therapy, increased tuberculosis case finding and reduced mortality in a setting of improved HIV care: a retrospective cohort study. HIV Med. 2012;13:337–344. doi: 10.1111/j.1468-1293.2011.00980.x. [DOI] [PubMed] [Google Scholar]
- 14.Koole O, Colebunders R. Reducing mortality from HIV infection and tuberculosis. Lancet Infect Dis. 2011;11:494–495. doi: 10.1016/S1473-3099(11)70094-9. [DOI] [PubMed] [Google Scholar]
- 15.Manosuthi W, Chottanapand S, Thongyen S, Chaovavanich A, Sungkanuparph S. Survival rate and risk factors of mortality among HIV/tuberculosis-coinfected patients with and without antiretroviral therapy. J Acquir Immune Defic Syndr. 2006;43:42–46. doi: 10.1097/01.qai.0000230521.86964.86. [DOI] [PubMed] [Google Scholar]
- 16.Mugusi F M, Mehta S, Villamor E et al. Factors associated with mortality in HIV-infected and uninfected patients with pulmonary tuberculosis. BMC Public Health. 2009;9:409. doi: 10.1186/1471-2458-9-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saito S, Howard A A, Reid M J et al. TB diagnostic capacity in sub-Saharan African HIV care settings. J Acquir Immune Defic Syndr. 2012;61:216–220. doi: 10.1097/QAI.0b013e3182638ec7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gustafson P, Gomes V F, Vieira C S et al. Clinical predictors for death in HIV-positive and HIV-negative tuberculosis patients in Guinea-Bissau. Infection. 2007;35:69–80. doi: 10.1007/s15010-007-6090-3. [DOI] [PubMed] [Google Scholar]
- 19.Schön T, Idh J, Westman A et al. Effects of a food supplement rich in arginine in patients with smear positive pulmonary tuberculosis—a randomised trial. Tuberculosis (Edinb) 2011;91:370–377. doi: 10.1016/j.tube.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Okot-Chono R, Mugisha F, Adatu F, Madraa E, Dlodlo R, Fujiwara P. Health system barriers affecting the implementation of collaborative TB-HIV services in Uganda. Int J Tuberc Lung Dis. 2009;13:955–961. [PubMed] [Google Scholar]
- 21.Uyei J, Coetzee D, Macinko J, Guttmacher S. Integrated delivery of HIV and tuberculosis services in sub-Saharan Africa: a systematic review. Lancet Infect Dis. 2011;11:855–867. doi: 10.1016/S1473-3099(11)70145-1. [DOI] [PubMed] [Google Scholar]


