Abstract
Background: In India, the National Health Mission has provided one mobile medical unit (MMU) per district in the state of Punjab to provide primary health care services for difficult-to-reach populations.
Objectives: To determine the number of patients with presumptive tuberculosis (TB) and the number of TB cases detected and treated among patients who used the MMU services from May to December 2012 in Mohali district, Punjab, India.
Methods: A cross-sectional study was conducted and registers of the out-patient, laboratory, radiology, and TB departments of the MMU were reviewed to determine the number of persons presumed to have TB and the number of persons diagnosed with TB.
Results: Of 8346 patients who attended the MMUs, 663 (8%) had symptoms suggestive of TB. Among those with TB symptoms, 540 (81%) were evaluated for pulmonary TB using sputum examination or chest X-ray. In total, 58 (11%) patients had clinical or laboratory evidence of pulmonary TB, of whom 21 (36%) started anti-tuberculosis treatment.
Conclusion: As MMUs are an integral part of the general public health system, these units have the potential to detect TB cases among difficult-to-reach populations. Additional research is required to optimise the diagnosis of TB at MMUs and to increase rates of TB treatment initiation.
Keywords: tuberculosis, mobile, chest X-ray, India, remote populations
Abstract
Contexte : En Inde, la Mission nationale santé a fourni une unité médicale mobile (MMU) par district dans l'état du Penjab afin d'offrir des services de soins de santé primaires aux populations difficilement accessibles.
Objectifs : Déterminer le nombre de patients présumés atteints de la tuberculose (TB) et le nombre de cas de TB détectés et traités parmi les patients qui ont utilisé les services de la MMU de mai à décembre 2012 dans le district de Mohali de l'état du Penjab, Inde.
Méthodes : Une étude transversale a été réalisée et l'étude des registres des consultations, du laboratoire, de la radiologie et des services de TB de la MMU a permis de compter le nombre de personnes présumées atteintes de TB et le nombre de personnes ayant eu un diagnostic de TB.
Résultats : Un total de 8346 patients ont fréquenté la MMU, dont 663 (8%) avaient des symptômes suggérant une TB. Parmi ces derniers, 540 (81%) ont bénéficié d'une recherche de TB pulmonaire grâce à un examen de l'expectoration ou à une radiographie pulmonaire. Au total, 58 (11%) patients ont eu des preuves cliniques ou biologiques de TB pulmonaire, dont 21 (36%) ont mis en route un traitement de la tuberculose.
Conclusion : Comme les MMU font partie intégrante du système de santé publique général, ces unités ont le potentiel de détecter les cas de TB parmi les populations « difficiles à atteindre ». De plus amples recherches sont requises afin d'optimiser le diagnostic de la TB dans les MMU pour accélérer la mise en route du traitement de la TB.
Abstract
Marco de referencia: En la India, la National Health Mission ha suministrado una unidad médica móvil (MMU) a cada distrito del estado del Punjab, con el objeto de prestar servicios de atención primaria de salud a las poblaciones de difícil acceso.
Objetivos: Determinar el número de pacientes con presunción clínica de tuberculosis (TB) y el número de casos de TB diagnosticados y tratados en el grupo de pacientes que acudieron a las MMU de mayo a diciembre del 2012 en el distrito de Mohali del estado del Punjab, en la India.
Métodos: Se llevó a cabo un estudio transversal, en el cual se examinaron los registros de los servicios de consulta externa, laboratorio, radiología y los departamentos de TB de las MMU, con el propósito de calcular el número de personas con presunción de TB y el número de casos de TB diagnosticados.
Resultados: Durante el período del estudio acudieron a las MMU 8346 personas, de las cuales 663 refirieron síntomas indicativos de TB (8%). Se investigaron 540 personas por TB pulmonar (81%) mediante la baciloscopia del esputo o la radiografía de tórax. Se encontraron pruebas clínicas o de laboratorio de TB pulmonar en 58 pacientes (11%) y se inició el tratamiento antituberculoso en 21 de ellos (36%).
Conclusión: Puesto que las MMU forman parte integrante del sistema general de salud pública, estas estructuras pueden detectar los casos de TB en las poblaciones de difícil acceso. Se precisan nuevas investigaciones que contribuyan a optimizar el diagnóstico de la TB en estas unidades y a conseguir que una mayor proporción de pacientes inicie el tratamiento antituberculoso.
In many countries, public health departments are using innovative strategies to improve the reach and accessibility of health services for a variety of conditions.1–9 India is a low- to middle-income country, with approximately 30% of the population earning below the international poverty line (US$<1.25 per day).10 Despite a well-developed public health system, many populations in India remain either underserved or without access to the health services available from the public health facilities.11–14 To enhance access to care and create an equitable distribution of health services across the country, the government of India created the National Rural Health Mission (NHRM). The NRHM has undertaken many initiatives to provide health care to underserved populations, including providing one mobile medical unit (MMU) in each district to increase the accessibility of public health services, especially in remote or difficult-to-reach locations. MMUs are vehicles equipped with basic diagnostic and treatment facilities that can move from one place to another, and which can provide opportunities for early, improved detection of a multitude of health conditions, particularly those of public health importance.
Tuberculosis (TB) is a major public health problem in India.15,16 Although TB diagnosis and treatment are available at all government health facilities through the Revised National Tuberculosis Control Programme (RNTCP),17 some at-risk populations are unable to access these TB services, thus remaining undetected and untreated.13 As MMUs are now an integral part of the general health system, offering services to remote or difficult-to-reach populations, they can be used to increase access to TB diagnostic and treatment services in the communities they serve. However, the results of MMUs for specifically screening, diagnosing and linking TB patients to treatment services have not been documented.
We undertook an operational research study among people using the medical services of an MMU in Punjab, India. As this was the first time that the MMU was being used for the screening and diagnosis of TB patients in India, it was anticipated that some challenges would be encountered. We therefore sought to identify and document 1) the proportion of people accessing the MMU medical services who were found to have presumptive TB; 2) the proportion of presumptive TB patients diagnosed with TB by the MMU; 3) the proportion of people diagnosed with TB who started treatment; and 4) the challenges faced during screening.
METHODOLOGY
Study design
This was a population-based descriptive cross-sectional study.
Setting
The study was conducted in the Mohali district (population 1 million) in the northern state of Punjab, India. In 2012, 67 378 new sputum smear-positive patients were diagnosed and 100 966 patients with TB were treated in the state of Punjab.16 MMU field visits were conducted to underserved communities in remote and vulnerable areas (e.g., urban slums, brick kilns and construction sites) where it was assumed that the population had difficulty in accessing health services.
Services provided by MMUs in Mohali district
Each MMU, with a staff of two medical officers, one nurse, one laboratory technician and one radiographer, is under the overall administrative control of the Chief Medical Officer of the district. The routine services provided by the MMU are general out-patient medical consultations, laboratory investigations (e.g., haemoglobin, total leukocyte count, differential leukocyte count, non-fasting blood sugar and urinalysis), electrocardiography, radiography and pharmacy. While medical consultations are provided free of charge, nominal charges are levied for diagnostic investigations (Indian Rs. 125, US$1.90). All services provided by the MMU are documented in an out-patient department (OPD) register, a laboratory register and a drug dispensing register.
As part of this demonstration project and prior to the scheduled visit of the MMU, the public health field workers (auxiliary nurse midwife and accredited social health activist) informed the local communities about the MMU visit. Persons with a cough of >2 weeks were given sputum containers and requested to go to the MMU with an early morning sputum sample. On the day of the MMU visit to the community, the MMU staff welcomed those persons who were identified and any person who presented for care. Each MMU visit began at 8 am and ended at approximately 2 pm, or until the last person waiting in the queue was evaluated. The MMU medical staff were trained to recognise presumptive TB, order appropriate diagnostic investigations (e.g., posteroanterior and lateral chest radiographs [CXR], and sputum smear microscopy), and link persons with TB disease to the RNTCP treatment services. The laboratory technician of the MMU was trained to perform Ziehl-Neelsen (ZN) sputum smear microscopy and to maintain a laboratory register according to RNTCP guidelines.17
Study period and study population
During the period of observation, from May 2012 to December 2012, all persons from Mohali district who had used the services from the MMU were included in the analysis.
All persons attending the MMU were screened for TB with a standardised medical examination and interview. All patients with signs and symptoms suggestive of pulmonary TB (e.g., prolonged cough >2 weeks, night sweats, fever, unexplained weight loss) were referred for sputum smear microscopy and CXR in the MMU. The CXRs were inspected for image quality by the radiographer before presentation to the medical officer for review and clinical diagnosis. If an abnormality was discovered, the second officer reviewed the film for concurrence. If the medical officer's reading was found to be discordant, the film was reviewed by the Chief Medical Officer for final decision. Because conventional radiography is limited in specificity, clinical suspicion was high for these individuals; all patients with abnormalities consistent with pulmonary TB were screened by sputum smear microscopy.
All sputum smear-positive patients were referred to the medical officer in charge of the nearest health facility for initiation of anti-tuberculosis treatment in accordance with RNTCP guidelines.17 Patients who were sputum smear-negative and had CXR features suggestive of TB were re-examined by a clinician and a radiologist for classification as clinical TB at the district or subdistrict level. Patients with sputum smear-negative TB or with symptoms or CXR evidence suggestive of TB were also offered anti-tuberculosis treatment.
Definitions, variables and sources of data
Persons presumed to have TB were defined as all patients with cough of ⩾2 weeks with/without any other associated symptoms, or any patient referred for TB investigations. We categorised the patients into three groups: 1) sputum smear-positive TB patients were all those who were positive for acid-fast bacilli (AFB) by ZN staining based on at least one sputum smear microscopy; 2) sputum smear-negative pulmonary TB patients were all those who were AFB-negative, but had CXR features suggestive of pulmonary TB; and 3) persons with symptoms and radiological features suggestive of TB on CXR but who did not undergo sputum smear examinations were labelled ‘presumed clinical TB’.
Demographic (age, sex) and clinical information were abstracted from the MMU OPD register, laboratory register, RNTCP TB registers, treatment cards, radiographic reports and monthly peripheral health institution (PHI) reports of the MMU using a standardised data collection instrument. At the conclusion of the study, we documented any logistical and programmatic challenges through informal interviews with all MMU staff. Key themes were identified, categorised and summarised.
Data management and analysis
Data collection forms were double-entered into a master database created in EpiData software version 3.1 (Odense, Denmark). There were no instances of discordance from the double data entry. Simple frequencies and percentages were tabulated for all variables. Pearson's χ2 tests were used to compare differences in proportions between groups. We compared four groups of patients receiving care at the MMU: those presumed to have TB, those evaluated for TB, those diagnosed with TB and, among those diagnosed, those started on anti-tuberculosis treatment. A P value of < 0.05 was considered statistically significant.
Ethics clearance
The study protocol was reviewed and approved by the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease (Paris, France) and the Institutional Ethics Committee of the National Tuberculosis Institute, Bangalore, India. Permission for the study was also obtained from the Director Health Services and the State TB Officer, Punjab.
RESULTS
During the study period, there were a total of 127 field screening days at 127 different locations. The MMU staff attended to a total of 8346 persons (average persons screened per visit, n = 66). Among these, 663 (8%) were determined to have symptoms suggestive of pulmonary TB. Of those with TB symptoms, 540 (81%) were further evaluated for TB: 186 (34%) with sputum smear examination only, 97 (18%) with both sputum examination and CXR and the remaining 257 (48%) with only CXR. Of those evaluated, 34 TB patients were diagnosed by sputum smear microscopy and CXR; 17 (50%) started anti-tuberculosis treatment. Among those evaluated with CXR alone (without sputum smear examination), 24 patients had radiographic features suggestive of TB and 4 (17%) started anti-tuberculosis treatment. In total, 58 patients were diagnosed with TB either due to sputum smear positivity or because of CXR evidence suggestive of TB (Figure).
FIGURE.
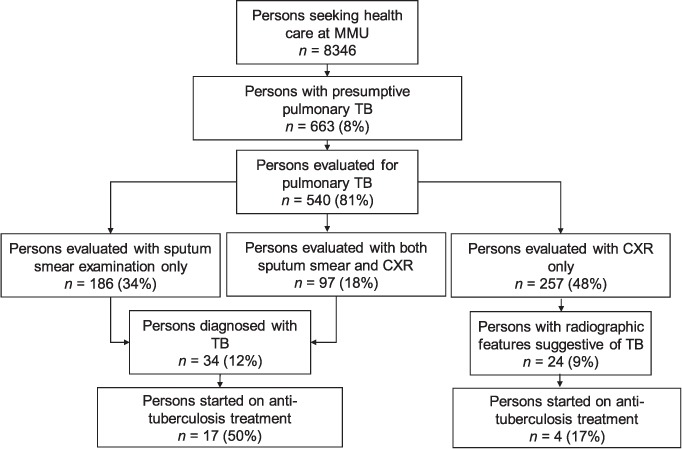
Screening and diagnosis of pulmonary TB among persons using medical care from MMU in Mohali district, Punjab, India (May–December 2012). MMU = mobile medical unit; TB = tuberculosis; CXR = chest X-ray.
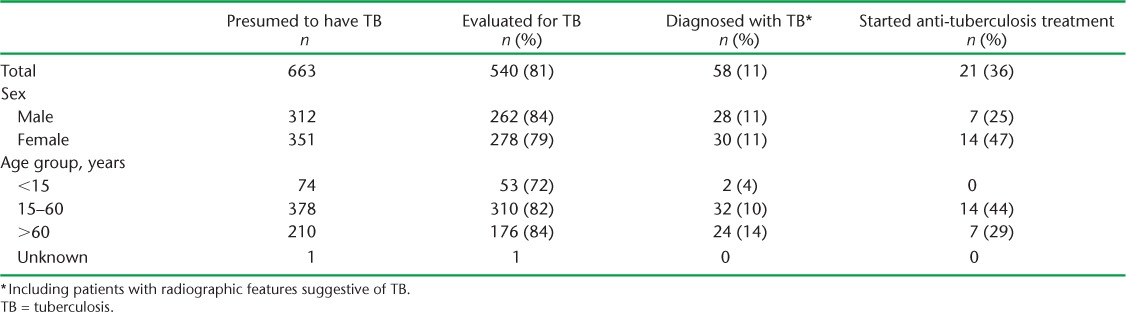
The demographic characteristics of patients with symptoms suggestive of TB are provided in Table 1. Although the proportion of males investigated for TB was greater (84% vs. 79%, P = 0.05), the proportion of males who started anti-tuberculosis treatment was smaller (25% vs. 47%, P < 0.05) compared to females. Fewer children (aged <15 years) were investigated for TB compared to other age groups (P < 0.05). Following a diagnosis of TB, no patients aged <15 years and less than a third of patients aged >60 years started treatment.
TABLE 1.
Demographic characteristics of patients with presumptive TB: status of evaluation, diagnosis and treatment of TB
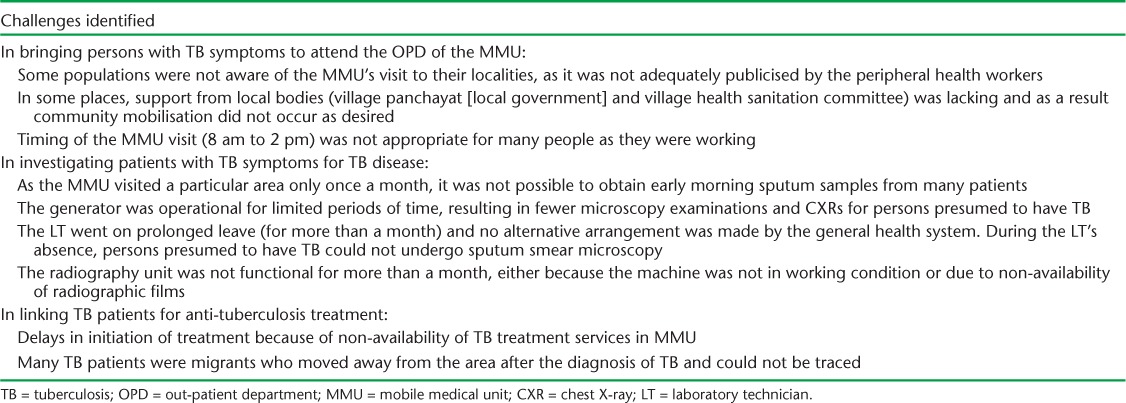
Challenges in screening hard-to-reach populations for TB through MMUs are summarised in Table 2. These included staffing and supply shortages, marketing and scheduling challenges and tracing migrant populations.
TABLE 2.
Challenges identified in screening hard-to-reach populations for TB through mobile medical units in Mohali, Punjab, India, 2012
DISCUSSION
This is the first study from India to describe case-finding activities using MMUs to target hard-to-reach populations for TB screening and treatment. Approximately 8% of patients screened by the MMU had symptoms suggestive of TB, and nearly four out of five persons with TB symptoms underwent additional investigations for TB (18% with both sputum smear microscopy and CXR, 48% with CXR alone and 34% with sputum smear microscopy alone). About 1 in 10 persons presumed to have TB were diagnosed with TB and, of these, only 1 in 3 started anti-tuberculosis treatment.
These findings have three key programmatic implications. First, the RNTCP has a policy for universal access to TB care, by which it aims to ‘reach the unreached’ through quality TB diagnostic and treatment services.13,18 As the philosophy of operating MMUs has a similar aim, it follows that the RNTCP-specified TB diagnostic and treatment services should be made available through the NRHM MMUs across the country. Our finding that 8% of the MMU attendees had clinical features suggestive of TB was much higher than the 2–3% found among those attending other public health facilities,6 a clear indication that the populations served by MMUs are in need of TB services. Second, sputum smear microscopy and CXR (the essential components of the RNTCP's TB diagnostic algorithm) can be made available through the facilities and resources already available through MMUs. To make these services more functional, some minimal expenditure (e.g., training, laboratory consumables) will be required. In addition, good coordination between RNTCP staff and the staff of the MMU will be essential to ensure continuity of appropriate care. Third, the study highlights potential operational challenges that may be encountered when conducting population-based field screening for TB using MMUs. Not all patients presumed to have TB underwent all the TB diagnostic tests, and loss to follow-up in this process was nearly 20%. It was difficult to evaluate all persons presumed to have TB as per RNTCP recommendations, because sputum smear microscopy is the primary test in the algorithm, followed by CXR. In this setting, sputum smear microscopy could not be undertaken for nearly half of those presumed to have TB due to the temporary absence of the laboratory technician or because of logistical challenges in obtaining an early morning sputum sample as part of a mobile field-based operation. This resulted in TB diagnosis based on clinical symptoms and CXR, a method previously reported as problematic.19,20 Finally, there were further losses to follow-up after the diagnosis of TB was made because the linkages for treatment services could not be properly established. If TB screening and treatment are to be integrated into MMU practice, formal guidelines must be established with sufficient resource allocation to overcome these challenges.
This study does have some limitations. First, as is the case with all studies that require data abstraction from routine surveillance and medical records, the quality of the data may be limited. Surveillance registries and medical records are not designed for study purposes but rather to document clinical encounters and report illnesses of public health importance. Although all the registries and records used were subjected to routine health system supervision and monitoring, data transcription errors were possible. Second, we did not ascertain whether the costs of the tests were a potential barrier to receiving screening at the MMU. Third, we did not compare the relative yield of diagnosing TB among persons receiving services in generalised clinics of Punjab. Comparing the MMU results with generalised clinics would enhance the analytical design of the study. Fourth, as we did not follow the patients over time, there was no time limit to assess initiation of treatment. It is possible that some patients may have been diagnosed and treated later in time or elsewhere. Finally, the challenges narrated in Table 2 were not collected in a structured manner; they are simply a compilation of feedback and perceptions of key MMU staff at the conclusion of the study. Despite this limitation, we believe these perceptions highlight relevant programmatic challenges that are important for translating our findings into public health action.
CONCLUSION
Despite observing some operational and logistical challenges under mobile field conditions (i.e., providing all diagnostic tests necessary to confirm TB diagnosis and to start anti-tuberculosis treatment), we believe that through the development of standardised guidelines, training and appropriate resource allocation, including multiple day visits for each community, MMUs have the potential to detect TB among difficult-to-reach populations in India.
Acknowledgments
The authors wish to thank the Civil Surgeon of Mohali district, and all of the medical officers and paramedical staff of the mobile medical units (MMU), the Revised National Tuberculosis Control Programme (RNTCP) and contractual staff, for their sincere efforts in collecting data for study and organising the data entry.
The study was conducted as a part of a year-long TB Operations Research Training Course designed to build operational research capacity within the Government of India's RNTCP. This training project was conceived and implemented jointly by the Central TB Division (Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India), The National TB Institute (Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India, Bangalore, India), the World Health Organization (WHO) India Country Office, the International Union Against Tuberculosis and Lung Disease (The Union) SouthEast Asia Regional Office, New Delhi, India, and the US Centers for Disease Control and Prevention, Division of TB Elimination, Atlanta, GA, USA. Funding support was provided in part by The Union from Global Fund Round 9, and by WHO-India through the United States Agency for International Development funding. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions or policies of the WHO, The Union, the CDC or the Central TB Division of the RNTCP, India.
Footnotes
Conflicts of interest: none declared.
References
- 1.Long Z, Hill C, Bennet J, Vavasis A, Oriol N E. Mobile clinic in Massachusetts associated with cost savings from lowering blood pressure and emergency department use. Health Aff (Millwood) 2013;32:36–44. doi: 10.1377/hlthaff.2011.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Omboni S, Carabelli G, Ghirardi E, Carugo S. Awareness, treatment, and control of major cardiovascular risk factors in a small-scale Italian community: results of a screening campaign. Vasc Health Risk Manag. 2013;9:177–185. doi: 10.2147/VHRM.S40925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Story A, Aldridge R W, Abubakar I et al. Active case finding for pulmonary tuberculosis using mobile digital chest radiography: an observational study. Int J Tuberc Lung Dis. 2012;16:1461–1467. doi: 10.5588/ijtld.11.0773. [DOI] [PubMed] [Google Scholar]
- 4.Lamel S A, Haldeman K M, Ely H, Kovarik C L, Pak H, Armstrong A W. Application of mobile teledermatology for skin cancer screening. J Am Acad Dermatol. 2012;67:576–581. doi: 10.1016/j.jaad.2011.11.957. [DOI] [PubMed] [Google Scholar]
- 5.Murthy K R, Murthy P R, Kapur A, Owens D R. Mobile diabetes eye care: experience in developing countries. Diabetes Res Clin Pract. 2012;97:343–349. doi: 10.1016/j.diabres.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 6.Kawichai S, Celentano D, Srithanaviboonchai K et al. NIMH Project Accept (HPTN 043) HIV/AIDS community mobilization (CM) to promote mobile HIV voluntary counseling and testing (MVCT) in rural communities in Northern Thailand: modifications by experience. AIDS Behav. 2012;16:1227–1237. doi: 10.1007/s10461-011-0099-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eang M T, Satha P, Yadav R P et al. Early detection of tuberculosis through community-based active case finding in Cambodia. BMC Public Health. 2012;12:469. doi: 10.1186/1471-2458-12-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zucker D M, Choi J, Gallagher E R. Mobile outreach strategies for screening hepatitis and HIV in high-risk populations. Public Health Nurs. 2012;29:27–35. doi: 10.1111/j.1525-1446.2011.00970.x. [DOI] [PubMed] [Google Scholar]
- 9.Hill C, Zurakowski D, Bennet J et al. Knowledgeable Neighbors: a mobile clinic model for disease prevention and screening in underserved communities. Am J Public Health. 2012;102:406–410. doi: 10.2105/AJPH.2011.300472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The World Bank. National Poverty Data—India. Washington, DC, USA: The World Bank Group; 2013. 2013. http://data.worldbank.org/country/india. Accessed November, 2015. [Google Scholar]
- 11.Khatri G R, Frieden T R. Controlling tuberculosis in India. N Engl J Med. 2002;347:1420–1425. doi: 10.1056/NEJMsa020098. [DOI] [PubMed] [Google Scholar]
- 12.Falzon D, Jaramillo E, Wares F, Zignol M, Floyd K, Raviglione M C. Universal access to care for multidrug-resistant tuberculosis: an analysis of surveillance data. Lancet Infect Dis. 2013;13:690–697. doi: 10.1016/S1473-3099(13)70130-0. [DOI] [PubMed] [Google Scholar]
- 13.Sachdeva K S, Kumar A, Dewan P, Kumar A, Satyanarayana S. New vision for Revised National Tuberculosis Control Programme (RNTCP): universal access—‘reaching the unreached’. Indian J Med Res. 2012;135:690–694. [PMC free article] [PubMed] [Google Scholar]
- 14.Satyanarayana S, Nair S A, Chadha S S et al. From where are tuberculosis patients accessing treatment in India? Results from a cross-sectional community based survey of 30 districts. PLOS ONE. 2011;6:e24160. doi: 10.1371/journal.pone.0024160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Global tuberculosis control: WHO report 2010. Geneva, Switzerland: WHO; 2010. WHO/HTM/TB/2010.7. [Google Scholar]
- 16.India Ministry of Health and Family Welfare. Tuberculosis India 2012. New Delhi, India: Central Tuberculosis Division, Directorate General of Health Services, Ministry of Health and Family Welfare; 2013. Annual Report of the Revised National Tuberculosis Control Programme. [Google Scholar]
- 17.India Ministry of Health and Family Welfare. Technical and operational guidelines for tuberculosis control, Revised National Tuberculosis Control Programme. New Delhi, India: Central Tuberculosis Division, Directorate General of Health Services, Ministry of Health and Family Welfare; 2005. [Google Scholar]
- 18.India Ministry of Health and Family Welfare. Universal Access to TB Care—a practical guide for programme managers. New Delhi, India: Central Tuberculosis Division, Directorate General of Health Services, Ministry of Health and Family Welfare; 2010. [Google Scholar]
- 19.Del Portillo-Mustieles E C, Laniado-Laborín R. Active case finding of pulmonary tuberculosis through screening of respiratory symptomatics using sputum microscopy: is it time to change the paradigm? Tuberc Res Treat. 2013;2013:312824. doi: 10.1155/2013/312824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koppaka R, Bock N. How reliable is chest radiography? In: Frieden T, editor. Toman's tuberculosis. Geneva, Switzerland: World Health Organization; 2004. pp. 14–22. [Google Scholar]


