Abstract
India mainly uses passive case finding to detect tuberculosis (TB) patients through the Revised National Tuberculosis Control Programme (RNTCP). An intensified case finding (ICF) intervention was conducted among vulnerable communities in two districts of Karnataka during July–December 2013; 658 sputum smear-positive TB cases were detected. The number of smear-positive cases detected increased by 8.8% relative to the pre-intervention period (July–December 2012) in intervention communities as compared to an 8.6% decrease in communities without the ICF intervention. ICF activities brought TB services closer to vulnerable communities, moderately increasing TB case detection rates.
Keywords: SORT IT, India, active case finding, marginalised groups, Project Axshya
Abstract
L'Inde recourt en majorité à la détection passive des cas de patients avec la tuberculose (TB) à travers le Programme national révisé de Lutte contre la Tuberculose. Une intervention de recherche intensifiée de cas (ICF) a été réalisée au sein de communautés vulnérables dans deux districts de Karnataka entre juillet et décembre 2013 ; 658 cas de TB à frottis positif ont été détectés. Le nombre de cas à frottis positif a augmenté de 8,8% par comparaison à la période précédant l'intervention (juillet–décembre 2012) dans les communautés bénéficiaires comparées aux 8,6% de diminution dans les communautés témoins. Des activités de recherche de cas intensifiées ont amené les services de TB plus près des communautés vulnérables, ce qui a accru modérément le taux de détection des cas de TB.
Abstract
En la India se da preferencia a la estrategia de búsqueda pasiva con el fin de detectar los casos de tuberculosis (TB) en el marco del Programa Nacional Revisado. Se llevó a cabo una intervención de búsqueda intensificada de casos en las comunidades vulnerables de dos distritos de Karnataka de julio a diciembre del 2013 y se detectaron 658 casos de TB con baciloscopia positiva. El número de casos con baciloscopia positiva aumentó un 8,8% con respecto al período anterior a la intervención (de julio a diciembre del 2012) en las comunidades de la intervención, en comparación con una disminución de 8,6% en las comunidades que no recibieron la intervención. Las actividades de intensificación de la búsqueda de casos llevaron los servicios de atención de la TB a las comunidades vulnerables y aumentaron de manera moderada las tasas de detección de la enfermedad.
India's Revised National Tuberculosis Control Programme (RNTCP) relies primarily on passive case finding to detect new cases of tuberculosis (TB). The new sputum case detection rate in Karnataka, a state in southern India, was 58% in 2013.1 One designated microscopy centre (DMC) exists for every 100 000 population in the plains, and in hilly areas the state government establishes one DMC per 50 000 population. About 24% of Karnataka's population is specifically classified by the Census of India as belonging to lower (scheduled) castes, and 7% belong to the tribal groups. Low socio-economic status and marginalisation is correlated with TB, requiring interventions to increase TB case detection rates.
Through Round 9 of the Global Fund to Fight AIDS, Tuberculosis and Malaria, Project Axshya helps expand the reach and effectiveness of the RNTCP, engaging communities to improve TB services for vulnerable populations. An intensified case finding (ICF) intervention was initiated under Project Axshya in 16 districts, covering 56% of Karnataka's population (34 million),2 including 54% of its lower caste and 45% of its tribal population. This study focuses on ICF activities in two districts, Kolar in the southern part of the state and Bidar in the northern part of the state, selected purposively to capture geographical spread. Areas were mapped so that a predominantly vulnerable population (20 DMCs, intervention area, population ~2 million) received the ICF intervention whereas the remainder (11 DMCs, non-intervention area, population ~1.1 million) did not.
To evaluate the effect of ICF on TB case detection, we reviewed routine programme data and compared changes in 1) the number of presumptive TB patients examined, and 2) smear-positive patients detected and treated in the intervention and non-intervention areas before the intervention (July–December 2012) and after implementing the intervention (July–December 2013).
ASPECT OF INTEREST
Under the intervention, vulnerable populations were mapped and selected in both districts in consultation with the District TB Officer. Individuals in vulnerable communities were visited in their homes and informed about TB and the RNTCP services. If people with presumptive TB were identified, they were linked to the RNTCP by patient referral and/or collecting and transporting sputum samples to the nearest DMC. This activity was expanded to areas where vulnerable communities predominantly live: slums, tribal areas, quarries and communities reported to have high human immunodeficiency virus (HIV) prevalence.
Trained community volunteers (n = 26) reached out to 1000 households, or at least 3000 individuals, per month per district. They visited households at well-planned times to maximise outreach per household. During the counselling process (~10–15 mins), consent was obtained from the household members, and information about TB as well as information, education and communication (IEC) material was shared by volunteers. Questions from household members were answered by volunteers.
The study was approved by the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France, and the Catholic Health Association of India, Secunderabad, India, Research Ethics Board.
To calculate the estimated additional yield from ICF activities, we calculated the difference in the number of persons screened and the number of TB cases diagnosed and treated during the intervention period compared to the same time period one year earlier for both the intervention areas and the non-intervention areas. The data were extracted from the RNTCP laboratory register, the TB treatment register and reporting formats under Project Axshya. EpiData software (v3.1 for entry and v2.2.2.182 for analysis, EpiData Association, Odense, Denmark) was used for double data entry, validation and analysis.
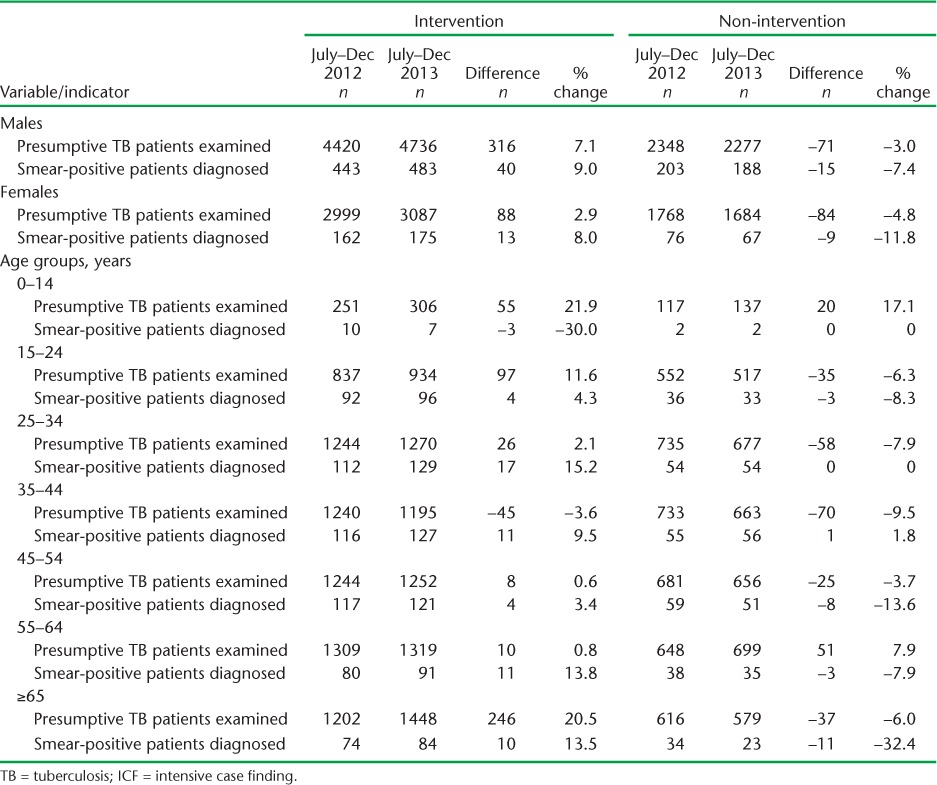
Of 115 119 households mapped in the intervention areas, 8468 (7%) were visited during the intervention period. This activity is being continued, and all households will be covered within 2 years. As seen in Table 1, there was an overall increase in the number of patients examined (+5.6%), diagnosed (+8.8%) and treated (+6.1%) in the intervention areas relative to the pre-intervention period. In contrast, there was an overall decline in case detection in the non-intervention areas. There was no difference in case detection rates by age and sex (Table 2).
TABLE 1.
Number of persons with presumptive TB and smear-positive cases diagnosed and treated under an ICF intervention in two districts of Karnataka, India, July–Dec 2012 and July–Dec 2013
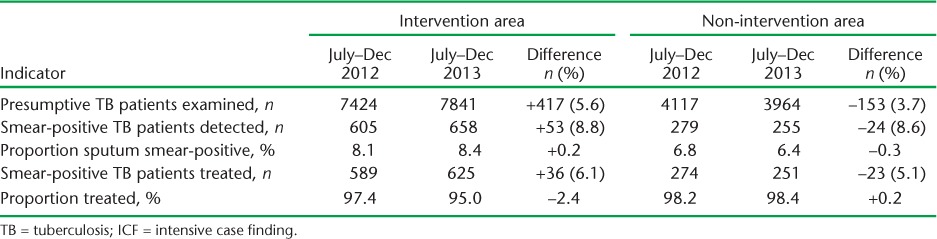
TABLE 2.
Number of persons with presumptive TB and smear-positive cases diagnosed stratified by age and sex under an ICF intervention in two districts of Karnataka, India, July– Dec 2012 and July–Dec 2013
DISCUSSION
This study shows that an innovative, community-based, education/case finding intervention increased the number of TB cases detected and treated and brought TB diagnostic and treatment services closer to vulnerable communities, boosting awareness about RNTCP services. These findings reflect preliminary results, as only 7% of the mapped houses were covered during the intervention period, and the activity is ongoing.
In studies such as these, the question is frequently raised as to how we can attribute the entire effect to the intervention in question, given the possibility of other interventions or changes in population size which might have contributed to increased case detection. We are not aware of any such interventions in the study area, and can thus attribute the increased case finding predominantly to the ICF intervention. This interpretation is further substantiated by the declining trends in the non-intervention areas. As the study is cross-sectional in design, we cannot elucidate all the reasons for this decrease, which presents a limitation.
Community-based ICF interventions implemented elsewhere in India and other countries have shown similar results; this reflects the replicability and scalability of such interventions.3–5 An intervention in Orissa, India, increased case detection by 11%.3 A similar ICF activity conducted in Ethiopia doubled the pulmonary TB case notification rate, from 64 to 127/100 000 population/year.4 In the results of the FIDELIS (Fund for Innovative DOTS Expansion through Local Initiatives to Stop TB) project in China, which massively mobilised school students for case finding, the case detection in intervention counties increased by a factor of 3.5 relative to the pre-intervention period.5
There were some limitations to our study. While our approach demonstrated a potential for improved case detection in the short term, we do not know if these trends are sustainable; we will need to re-examine the results once all the mapped households in the intervention area are covered. We did not collect data to determine whether this strategy led to earlier detection of TB cases and thereby reduced transmission, or if it improved treatment outcomes for patients—the ultimate objectives of ICF. There was a small decrease in the proportion started on treatment in the intervention areas. We are not aware of specific reasons for this decrease and this needs further research. Maintaining the increased detection rates observed in this study would likely require routine ICF interventions for vulnerable communities and increased access to DMCs. Alternatively, door-to-door counselling visits may lead to moderate behavioural change, help in case detection and be more cost-effective than special programmes or campaigns, as shown in Cambodia.4 Future studies should assess the cost-effectiveness of such interventions to determine the optimal periodicity of such interventions before making scale-up decisions. Given these encouraging initial results and to address the above limitations, a larger study is being planned.
In conclusion, ICF using family counselling mechanisms and community-based TB screening led to a modest increase in the numbers of smear-positive TB cases diagnosed among vulnerable communities in Karnataka, India.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR). The model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union) and Médecins Sans Frontières (MSF). The specific SORT IT programme that resulted in this publication was jointly developed and implemented by The Union South-East Asia Regional Office, New Delhi, India, the Centre for Operational Research, The Union, Paris, France, and the Operational Research Unit (LUXOR), MSF, Brussels Operational Center, India.
Funding for the operational research course was made possible by the support of the American People through the United States Agency for International Development (USAID). The funders had no role in the study design, data collection, analysis and interpretation of data, the decision to publish or the preparation of the manuscript. The contents of this paper do not necessarily reflect the views of USAID, the United States Government or The Union. In accordance with the WHO's open-access publication policy for all work funded by the WHO or authored/co-authored by WHO staff members, the WHO retains the copyright of this publication through a Creative Commons Attribution IGO license (http://creativecommons.org/licenses/by/3.0/igo/legalcode) which permits unrestricted use, distribution and reproduction in any medium provided the original work is properly cited.
Footnotes
Conflicts of interest: none declared.
References
- 1.Indian Ministry of Health and Family Welfare. TB India 2013. Revised National Tuberculosis Control Programme: annual status report. New Delhi, India: Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare; 2013. http://www.tbcindia.nic.in/ Accessed November 2015. [Google Scholar]
- 2.Indian Ministry of Home Affairs. Directorate of Census Operations–Karnataka, 2011. Bangalore, India: Ministry of Home Affairs, Directorate of Census Operations; 2012. http://censuskarnataka.gov.in/ Accessed November 2015. [Google Scholar]
- 3.Parija D, Patra T K, Kumar A M et al. Impact of awareness drives and community-based active tuberculosis case finding in Odisha, India. Int J Tuberc Lung Dis. 2014;18:1105–1107. doi: 10.5588/ijtld.13.0918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yassin M A, Datiko D G, Tulloch O et al. Innovative community-based approaches doubled tuberculosis case notification and improved treatment outcome in Southern Ethiopia. PLOS ONE. 2013;8:e63174. doi: 10.1371/journal.pone.0063174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eang M T, Satha P, Yadav R P et al. Early detection of tuberculosis through community-based active case finding in Cambodia. BMC Public Health. 2012;12:469. doi: 10.1186/1471-2458-12-469. [DOI] [PMC free article] [PubMed] [Google Scholar]


