Abstract
Although many studies have addressed adverse outcomes in children of parents with alcohol abuse/dependence, less is known about the possible long-term effects of more normative patterns of parental alcohol consumption, including drinking at lower risk levels and heavy episodic or binge drinking. The extent of harm from parental drinking may therefore be underestimated. With this research proposal, we describe a project that aims to assess possible long-term adverse effects of parental drinking by combining survey and nationwide registry data. Advantages of a longitudinal general population cohort design include that it allows for detailed information on parental drinking through survey data and identification of possible negative long-term health and social outcomes from exposure to parental drinking 1–19 years after exposure through continuously updated nationwide registers. The rich information available from combining survey and registry data allows us to take into account important confounders, mediators, and moderators.
Keywords: parental drinking, harm to children, longitudinal, cohort, registry
Introduction
Alcohol contributes to harm both the drinkers and those close to them. The global burden of disease from alcohol estimates all deaths and disability-adjusted life years lost,1 but since research on harm from alcohol usually focuses only on health problems in the drinkers, the global burden from alcohol may be underestimated. Although alcohol's harm to others has received less attention in, we now see a growing interest in estimating “second-hand” effects from alcohol.2–5 Beyond the importance of obtaining better assessments of the overall health and social burden attributable to alcohol, a better understanding of alcohol's harms to others may serve to legitimatize effective alcohol control policies6 and particularly so when vulnerable groups, such as children, suffer harms from others’ drinking. In this research proposal, we describe a project that addresses possible long-term adverse effects of parental drinking.
Studies have shown that children of parents with alcohol abuse/dependence are at increased risk of various negative outcomes, such as violence,7,8 family separation,7 teenage pregnancy,7 substance use problems,9–13 mental health problems,13–19 poor academicperformance,20,21 unemployment,7 and becoming dependent on social welfare benefit from a young age.7 However, recent systematic reviews have shown that much less is known about how children are affected by parental alcohol consumption other than clinically diagnosed alcohol problems, including drinking at lower risk levels and heavy episodic or binge drinking, hereafter referred to as subclinical drinking.14,15
While persons with alcohol abuse/dependence are more likely than others to experience harm from own drinking, light and moderate drinkers also account for a substantial proportion of the health burden due to alcohol use.16 Tus, drinking carries a risk of harm to the drinker at all consumption levels. We do not know whether this also applies to harms to children from parental drinking. What we know is that alcohol consumption, also in the absence of dependence or abuse may change how parents behave around their children: alcohol consumption influences the central nervous system, can cause changes in mood, impaired cognition, increased impulsiveness, and aggressiveness, which may contribute to poorer parenting.17 Parents may become less attentive to their children’s needs and be more likely to misinterpret and misjudge communication, actions, and situations under the influence of alcohol and to initiate conflict or violence.18,19 As we know little about the effects on children from subclinical parental drinking,14,15 questions regarding the possible long-term effects of subclinical parental drinking on children’s psychosocial functioning and possible dose–response relationships remain unanswered.
Due to various methodological limitations, most of the previous studies of harm to children from parental drinking have limited capacity for drawing causal inferences from associations between exposure and outcome, particularly regarding long-term outcomes. First, cross-sectional surveys applying a retrospective design may offer information about associations between current problems and childhood or adolescent exposure to parental heavy drinking.20 However, such studies rely on retrospective and often long-term recalls of exposure and they are likely to fail in obtaining subclinical exposure and important time-dependent confounders. Second, studies based solely on registry data are suitable for studying the effect of registered exposures, such as parental alcohol disorder treatment, on registered outcomes, such as unemployment in their children. However, such a design does not provide the opportunity to study the effects of subclinical parental drinking on outcomes in their children.7,21 Third, prospective cohort studies offer the best observational study design to assess causal associations, but follow-up time in these studies is often limited to only a few years,14 implying that long-term adverse effects are less likely to be detected. Attrition that causes selection bias may be a further problem in such studies.22,23 A recent scoping review of cohort studies on parental drinking and adverse outcomes in children noted that limitations in the large literature available makes it difficult to address a possible causal role of parental drinking on children’s adverse outcomes.14 Similarly, a systematic review of prospective cohort studies on the influence of parental drinking on children’s drinking concluded that, while more parental drinking is associated with more drinking in children, the existing evidence does not warrant causal inference.15 The limitations described earlier underscore the need for well-designed studies that can shed light on the possible adverse long-term effects in children of exposure to various parental drinking patterns.
This research proposal describes the background and study design for a project that aims at overcoming some of the aforementioned limitations in the existing literature on the adverse effects of parental drinking. To accomplish this, we use a prospective cohort study design that combines survey data from the general population on exposure measures that identify parental drinking ranging from absenteeism to normative patterns of parental drinking and abuse/dependence and registry data on outcome measures in children.
Scientific aims
The main objective is to study the possible long-term effects of parental drinking on psychosocial adjustment in their children, using a large cohort of parents and children in the general population for which both survey data on exposure to parental drinking and registry data on outcome measures in children are available.
Methods
Setting
Norway has a long tradition of a restrictive alcohol policy. Limited availability of alcoholic beverages, high alcohol taxes, and a comprehensive alcohol monopoly system are regarded as pillars of the Nordic alcohol policy.24 Even though the Norwegian alcohol policy has been liberalized during the past few decades, it is still fairly restrictive compared to other Western countries.25,26
The alcohol consumption in Norway is also fairly low – at least compared to other European countries.27 The drinking culture has traditionally been characterized by relatively infrequent drinking during weekdays and higher consumption during weekends and holidays.28 With this drinking pattern, it is possible that many adolescents have experienced change in their parents’ behavior because of drinking. Indeed, a relatively large proportion (43%–48%) of Norwegian adolescents report having seen one or both parents intoxicated by alcohol.18
Design
To address the aims of this project, we link survey data from a large cohort, including both the adult population and the youth population in one Norwegian county (the Nord-Trøndelag Health Study/HUNT), with several national registries. This approach allows us to follow adolescents (Young-HUNT participants) over time to study the effects of parental drinking (obtained from HUNT participants) on negative long-term outcomes (obtained from various registries) in children. Norwegian registers provide information at the individual level and cover virtually all the inhabitants in Norway. The personal identification numbers (PIN) assigned to all residents enables linkage of data from different registers at the individual level. HUNT participants provided their PIN, which allows for linkage of information from HUNT and Young-HUNT, with registry data at the individual level.23,29,30 Data on the exposure, parental drinking, are obtained from HUNT, and data on the long-term outcomes are obtained from the national registers. Available data allows us to examine the impact of three possible outcomes: mental health, substance use, and employment. Several research papers will be written on each outcome.
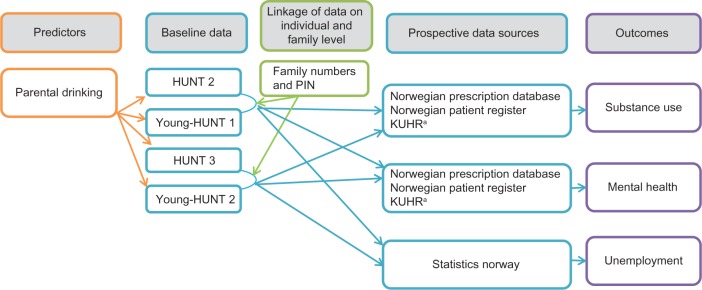
Linkage of triads: data on mother, father, and child(ren) in a family
In addition to PIN, each family in Norway has a unique family number. The family number is available from the national registry and enables linkage of data among mother, father, and children, as long as the child is still living with one or both parents at baseline. Families consist of persons who are married, registered partners, partners living together and/or parent(s), or unmarried children living in the same household.31 Figure 1 illustrates the predictors, baseline data, linkage of data, and prospective data sources used to investigate the various outcomes.
Figure 1.
Overview over predictors, baseline data, linkage of data, and prospective data sources used to investigate outcomes.
Note: aControl and reimbursement to practitioners in primary health care for seeing and treating patients.
Data sources
HUNT
The HUNT study includes longitudinal data from one of the largest general population samples in the world.29 It was carried out in three waves (HUNT 1, 2, and 3) in Nord-Trøndelag County, Norway. The demographic structure of Nord-Trøndelag is fairly representative of the Norwegian population.29 Exceptions are lower average income and smaller proportion with higher education compared with the Norwegian population. The majority of the county's inhabitants live in small towns and rural settings. All adolescents (aged 13–19 years) were invited to participate in Young-HUNT, and all adults (20 years and older) were invited to participate in HUNT, the adult version of the study. This research project uses data from HUNT 2 (n = 66,140, response rate: 71.2%29), Young-HUNT 1 (n = 8433, response rate: 82.7%23), HUNT 3 (n = 50,807, response rate: 54.1%30), and Young-HUNT 3 (n = 7716, response rate: 73.7%23; Table 1). A wide range of variables on demographic characteristics, physical and mental health, social support, and substance use are included in the HUNT and Young-HUNT surveys. For more detailed information about HUNT and Young-HUNT, see publications from the HUNT Research Center.23,29,30 In this research project, information from HUNT and Young-HUNT constitutes the exposure measure, parental drinking. Relevant confounding factors such as parental mental health and mediating factors such as adolescent drinking are also included.
Table 1.
Overview over survey data collection and the period from which registry data were used.
| SURVEY DATA | TIME PERIOD DATA COLLECTION |
|---|---|
| Adult cohort I (HUNT 2) |
1995–1997 (adults of 20 years or older) |
| Adolescent cohort I (Young-HUNT 1) |
1995–1997 (adolescents 13–19) |
| Adult cohort II (HUNT 3) |
2006–2008 (adults of 20 years or older) |
| Adolescent cohort II (Young-HUNT 3) |
2006–2008 (adolescents 13–19) |
| REGISTRY DATA | TIME PERIOD FOR REGISTRY DATAa |
| The Norwegian prescription database | 2004–2014 |
| The Norwegian patient registry | 2008–2014 |
| KUHR databaseb | 2006–2014 |
| Statistics Norway | 2004–2014 |
Notes:
The time period from which registry data were extracted varies because: (1) they were established at different times, (2) for some, data quality was not considered sufficient for the first years after the registry was established, and/or (3) linkage at individual level was not possible for the first years after the registry was established
Control and reimbursement to practitioners in primary health care for seeing and treating patients.
The national registers
The outcome data on psychosocial adjustment are obtained from the national registers. Norway’s national registers include prospectively collected information on all inhabitants. Mental health problems will be identified through several registers, which provide measures of a wide range of problems such as anxiety, depression, and stress-related disorders. Substance use problems, such as alcohol abuse, prescription drug abuse, and opioid dependence, will be identified though several registers. Employment problems, such as benefits for unemployment and long-term sickness absence, will be identified though one registry. Information in the national registers are generally of high quality; missing data is rare and attrition negligible.22 The data available in the respective registers are described in greater detail later.
This project includes the following Norwegian registries: (1) the Norwegian Prescription Database (NorPD), (2) the Norwegian Patient Registry (NPR), (3) Control and reimbursement to practitioners in primary health care for seeing and treating patients (KUHR), and (4) Data on socioeconomic status from registers administered by Statistics Norway include the Norwegian Social Insurance Administration Registries (FD trygd), the National Registry (Folkeregisteret), The National Education Database, and the Income Registry (Table 1).
The NorPD includes detailed information on all drugs prescribed (reimbursed or not) and dispensed at pharmacies to individual patients living outside institutions, ie, in ambulatory care. Data have been collected from all Norwegian pharmacies on a monthly basis since January 2004.32 The detailed information includes data on patient, prescriber, drug, and pharmacy. For this project, the following patient information is included: encrypted PIN, year of birth, year of death, and gender. For the prescriber, only the prescriber ID is included. For prescriptions, prescription ID and the date the patient received the prescription drugs at a pharmacy is included. Drug classification is based on the Anatomical Therapeutic Chemical (ATC) Classification System, and Defined Daily Dose (DDD) offers information on the doses prescribed.33 In the ATC system, the drugs are classified into groups at five different levels. In this research project, drugs acting on the nervous system (drug group N) are the relevant drugs, and can be studied on group level (eg, opioids or benzodiazepines) and substance level (eg, methadone or diazepam). A DDD is defined as the assumed average maintenance dose per day for a drug used on its main indication in adults. Data from NorPD will be used to identify the use of prescription drugs for mental health or substance use problems.
The NPR includes information on admission to hospitals and specialist health care. The information includes dates of admission and discharge and primary and secondary diagnosis. Data from NPR will identify long-term outcomes such as hospital admissions and inpatient or outpatient treatment for mental health or substance use problems. Codes for International Classification of Diseases, 10th Revision (ICD-10) are used. For this project, the following are relevant: diagnoses on ICD-10-group F, mental and behavioral disorders, certain diagnoses from group G, diseases of the nervous system, such as migraine, other headaches and sleep problems since they may be triggered by mental problems, and unspecific mental problems recorded in ICD group Z.
Data from primary health care will be drawn from the KUHR database (control and reimbursement to practitioners in primary health care for seeing and treating patients). The database includes codes for International Classification of Primary Care (ICPC) and can inform about the cause of contact between patient and primary health care and the date for the visit. Data from KUHR will be used to identify diagnoses and treatment for mental health or substance use problems. These are recorded under group P (psychological), and examples include feeling anxious/nervous/tense (P01), feeling depressed (P03), sleep disturbance (P06), acute alcohol abuse (P16), medication abuse (P18), and drug abuse (P19).
The Norwegian Social Insurance Administration Registries (FD trygd) is administered by Statistics Norway. It includes the start and end dates for the receipt of benefits for long-term sickness absence (>15 days), disability pension, unemployment, and social welfare. The diagnoses associated with sickness absence and disability are available as ICPC codes. The register covers the entire Norwegian population from 1992, and it is continuously updated.
Additional background and socioeconomic information administered by Statistics Norway includes family numbers, marital status, education, and income. The data will be used to (1) identify if the child(ren) lived with one (if so, which one) or both parents when the HUNT data was gathered and (2) control for confounding variables.
Study population and size
To study the effect of exposure to parental drinking on long-term outcomes in children, a large data source is necessary. Young-HUNT 1 and 3 include information of ~17,000 adolescents.23 The estimated number of triads (adolescent, mother, and father) is ~7500. This estimate is based on the previous studies which included ~4000 triads from HUNT 2 and Young-HUNT 1.34 Since the participation rate was somewhat lower in HUNT 3 and Young-HUNT 3, we expect that the HUNT 3 wave will provide data from ~3500 triads.
With respect to power, the size of the study is large enough to detect even small differences in increased risk of negative outcomes related to substance use, mental health, and unemployment. As an example, we considered the use of antidepressants. In 2004–2013, 3.0%–3.6% of the inhabitants of Central Norway in the age group 20–24 years were dispensed antidepressants annually.35 Corresponding to this prevalence in NorPD, we estimate that with a total population of 7500 young adults followed for an average of seven years, the risk is higher for those who report to have seen their parents drunk often compared to those who have never/rarely seen their parents drunk; OR: 1.23, with 95% CI: 1.03–1.46, P < 0.05.
Exposure
Parental drinking, as measured in HUNT 2 and 3, is the exposure variable. Parental alcohol consumption is measured by (1) asking the parents about the frequency of drinking during a typical month, (2) the number of alcohol units consumed during a typical two-week period, specifying how many units of (a) beer, (b) wine, and (c) liquor the respondent would typically drink in this time period, and (3) The CAGE screening instrument36,37 that contains four items related to psychological and social cues of heavy drinking during the respondents’ life time and is scored on a dichotomous scale where a cutoff value of ≥2 indicates alcohol misuse. CAGE has shown good psychometric properties across countries.37–39 The exposure measure identifies a range of parental drinking patterns, from abstinence and low-risk drinking to heavy episodic drinking and alcohol misuse. In addition to the parents' report on own drinking, Young-HUNT includes information on if, and how often, the adolescents have seen their parents intoxicated. The response options range from “never” to “a few times per week.”
Outcomes
Mental health
Data from several registers will identify mental health problems. NorPD will be used to identify prescription drug use for mental health issues, eg, antidepressants (ATC codes N06A), and hypnotics, and sedatives (ATC codes N05B and N05C). NPR will identify the treatment for mental health problems in specialist health care, such as mood (affective) disorders (ICD-10 F30–F39) and neurotic, stress-related, and somatoform disorders (ICD-10 F40-F48). KUHR will be used to identify the treatment for mental health issues in primary health care, such as diagnoses for sleep disturbance (ICPC code P06), feeling depressed (ICPC code P03), or feeling anxious/nervous/tense (ICPC code P01).
Substance use
Data from several registers will be used to identify substance use problems. NorPD includes information on prescription drugs prescribed and dispensed to treat substance use problems, such as medicinal treatment for alcohol dependence (ATC codes N07BB) and opioid dependence (ATC codes N07BC). NPR identifies the treatment in specialist health care for mental and behavioral disorders due to psychoactive substance use (ICD-10 F10–F19), such as disorders due to alcohol (F10) and cannabinoids (F12). KUHR identifies problems with substance use identified after contact with primary health care, such as chronic alcohol abuse (ICPC code P15), acute alcohol abuse (ICPC code P16), prescription drug abuse (ICPC code P18), and drug abuse (ICPC code P19).
Unemployment and income compensation
Data from FD trygd will identify young adults who received benefits for unemployment, long-term sickness absence, disability, or who required social welfare assistance.
Confounders, mediators, and moderators
To understand the mechanisms behind parental drinking in the general population and negative long-term outcomes in adolescents, we took into account important confounders, mediators, and moderators, which are available in HUNT, Young-HUNT, and the registers. A particular emphasis is placed on gender, social inequality, and parents’ mental health.7,11,40 The likely causal mechanisms underlying the adverse effects of parental drinking differ for the various types of outcomes, and various theoretical approaches guide the identification of relevant confounding, mediating, and moderating factors for the three types of psychosocial outcomes.
Ethical perspectives
Study participants in HUNT and Young-HUNT provided informed consent, which includes permission to link survey data to register data. For the purpose of this study, encrypted numbers replace the PIN and family numbers before the researchers receive the data file. The research group will not have access to the PIN and keys for linkage. Linkage of HUNT, Young-HUNT, and registry data does not expose study participants to more questions or any form of interventions, which may be experienced as intrusive or unpleasant.
The linked dataset will include an extensive amount of information on each person participating in the study. The more the information available on each person, the higher the possibility that persons can be identified. Although researchers do not use the wide range of data available on each study participant to identify persons, it is theoretically possible to misuse data this way. When applying for data it was therefore important to ask only for the information necessary to answer the research questions in the project. The research group initiated a dialog with several registry owners to discuss which variables were necessary to address the research questions and how to balance getting sufficiently detailed information without asking for more than necessary. Levels of detail were reduced in cases where it was not necessary to address the aims of the project. For instance, when asking for information on ICD-10 diagnosis extracted from the NPR, we do not need all the details about diagnoses. For example, it is sufficient to know that a patient is diagnosed with a depressive episode (F32), we do not need to know what kind of depressive episode, eg, F32.0, F32.1, F32.2, and so on, is diagnosed. Similarly, it was not necessary to include information on geography to address the project aims. Thus, apart from knowing that study participants lived in Nord-Trøndelag when they participated in HUNT and Young-HUNT, information on geographic location is not included.
The research project is approved by the Regional Committees for Medical and Health Research Ethics (REK), the Norwegian Social Science Data Services (NSD) and The Norwegian Data Protection Authority. HUNT research center and the registry owners have approved applications for access to data that are necessary to carry out the research project.
Methodological Considerations, Main Strengths, and Weaknesses
Some limitations should be taken into account when future results from the proposed research project are interpreted. For instance, for adolescents who had dropped out of school, the participation rate is low in Young-HUNT.23 Because they are more likely than their peers to have problems, the prevalence of problems is likely underreported. Similarly, it is likely that parents who choose not to participate in HUNT have more problems compared with those who participate.41 Participation rates in general population surveys have declined during the past 30 years with even steeper declines in the recent years.42 This is the case for the HUNT waves too. Nevertheless, the lowest participation rate of 54% can be considered acceptable. Another limitation is that findings from the study may not be generalized to countries with different drinking cultures and countries with different practices for parental drinking in the presence of children and adolescents. Therefore, the importance of the drinking culture context should be addressed in similar studies in countries with different drinking patterns.
Some registers first became available in 2004 and 2006. Therefore, we have access to outcome data on the participants from Young-HUNT 3 from the time of survey data collection, but outcome data on the participants from Young-HUNT 1 is first available seven to nine years after they completed the survey. Further, Young-HUNT 3 participants (2006–2008) contributed fewer person-years to the study. This was taken into account in statistical analyses. Further, while information in the national registries is generally of high quality, changes in how information is entered into the registers can cause gaps in time series and/or make information before and after the changes incompatible.
The research project has several notable strengths. HUNT, Young-HUNT, and registry data are population based, HUNT and Young-HUNT have a high participation rate,23,30 and attrition in the registers is negligible.22 Advantages of combining survey and registry data for studying long-term outcomes in adolescents from parental drinking in the general population include that it allows for identifying a range of parental drinking patterns and long-term outcomes in the adolescents. The combined survey and registry data provide rich information on areas that are often associated with parental drinking, such as parental mental health, unemployment, education, and other socioeconomic characteristics.43 If these factors are not taken into account, we cannot estimate how much they influence the outcomes of interest. Further, many longitudinal studies on parental drinking and outcomes in children only include a few years with follow-up.12,44–47 For several outcomes, the time from exposure to onset of a problem can take several years. For instance, the association between exposure to parental drinking and unemployment cannot be studied until working age is reached. The chance of identifying such problems increases over time. Further, there are fewer problems with attrition in longitudinal registry studies than in longitudinal survey studies.22
In small samples studies, random error will make effect estimation less precise. Therefore, it is difficult to conclude whether or not a small or moderate effect of parental drinking on later negative outcomes is due to chance. Since the proposed study has a very large sample size, our estimates have more statistical precision, which allows us to report effect sizes with some degree of confidence. Previous publications on HUNT triads23,35 also suggest that our project has sufficient statistical precision for effect estimation, even in complex statistical models.
Several studies include data from only one parent. This may introduce biases, particularly in cases where the nonparticipating parents drinking behavior deviates substantially from that of the participating parent. In these cases, the overall parental drinking exposure is over- or underrated and the exposure-outcome association consequently biased. Thus, including information on both parents is a strength. Further, several studies include data on parental drinking reported either by parents or the adolescents.14 For a more thorough understanding of the association between parental drinking and negative long-term outcomes in children as young adults, it is important to know both how often and how much both parents drink and how often the adolescents see their parents intoxicated. In this study, both aspects are included. While we believe that self-report survey is a good approach to identify the frequency and quantity of parental drinking in the general population, mapping substance use with surveys has its limitations. For instance, those who drink a lot are underrepresented and those who participate may underreport how much they drink.28,48 However, generalizations of relationships are less vulnerable to sample effects than are generalizations of prevalence.49 Thus, as most of the papers resulting from this project focus on bivariate and multivariate associations between exposure and outcome variables, the response rate is not likely to bias the results. Further, controlling for confounding variables is more important to advance understanding of causal mechanisms than representative sampling.50
Implications
There is a growing concern about alcohol-related harms to others than the drinker.2–4 The society's obligations to protect individuals from harms caused by others are generally acknowledged as legitimate reasons for implementing control policies and regulations.6 For instance, limits on blood alcohol concentration and other measures to prevent harms from drunken drivers are effective, widely used, and accepted control measures16,51 that are explicitly reasoned on the principle of protecting “third parties.” Another example based on this principle is regulations of smoking in bars and restaurants. In the same vein, results from this project can be important for informing alcohol policy. A better understanding of the extent of parental drinking, and how it may have adverse health and social consequences for their children, may serve as a strong additional argument for implementing effective strategies to prevent harmful drinking among parents.
Acknowledgments
We are grateful to Kristoffer Burski for valuable input and comments about KUHR.
Footnotes
FUNDING: Authors disclose no funding sources.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
ACADEMIC EDITOR: Gregory Stuart, Editor in Chief
PEER REVIEW: Five peer reviewers contributed to the peer review report. Reviewers' reports totaled 1983 words, excluding any confidential comments to the academic editor.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Author Contributions
Contributed to the study design: IOL, SS, MH, IR, ISM, EES, AB, TN, GSB. Wrote the first draft of the manuscript: IOL. Contributed to the writing of the manuscript: AB, IR, EES, ISM, SS, MH, TN, GSB. Jointly developed the structure and arguments for the paper: IOL, IR, AB, ISM, EES, SS, MH, TN, GSB. Made critical revisions and approved the final version: IR, IOL, AB, EES, ISM, SS, MH, TN, GSB. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–33. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 2.Giesbrecht N, Cukier S, Steeves D. Collateral damage from alcohol: implications of ‘second-hand effects of drinking’ for populations and health priorities. Addiction. 2010;105(8):1323–5. doi: 10.1111/j.1360-0443.2009.02884.x. [DOI] [PubMed] [Google Scholar]
- 3.Room R, Ferris J, Laslett A-M, Livingston M, Mugavin J, Wilkinson C. The drinker’s effect on the social environment: a conceptual framework for studying alcohol’s harm to others. Int J Environ Res Public Health. 2010;7(4):1855–71. doi: 10.3390/ijerph7041855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Casswell S, You RQ, Huckle T. Alcohol’s harm to others: reduced wellbeing and health status for those with heavy drinkers in their lives. Addiction. 2011;106(6):1087–94. doi: 10.1111/j.1360-0443.2011.03361.x. [DOI] [PubMed] [Google Scholar]
- 5.Connor J, Casswell S. Alcohol-related harm to others in New Zealand: evidence of the burden and gaps in knowledge. N Z Med J. 2012;125(1360):11–27. [PubMed] [Google Scholar]
- 6.Skog OJ. The prevention paradox revisited. Addiction. 1999;94(5):751–7. doi: 10.1046/j.1360-0443.1999.94575113.x. [DOI] [PubMed] [Google Scholar]
- 7.Christoffersen MN, Soothill K. The long-term consequences of parental alcohol abuse: a cohort study of children in Denmark. J Subst Abuse Treat. 2003;25(2):107–16. doi: 10.1016/s0740-5472(03)00116-8. [DOI] [PubMed] [Google Scholar]
- 8.Rossow I. Suicide, violence and child abuse: a review of the impact of alcohol consumption on social problems. Contemp Drug Probl. 2000(27):397. [Google Scholar]
- 9.Brunnberg E, Eriksson C, Tinnfält A. Att ha minst en förälder som missbrukar alkohol: Om psykisk ohälsa och utvärderade interventioner Only in Swedish [Having At Least One Parent Who Abuses Alcohol: On Mental Illness and Evaluated Interventions] 2007. http://oru.diva-portal.org/smash/get/diva2:138277/FULLTEXT01.pdf.
- 10.Latendresse SJ, Rose RJ, Viken RJ, Pulkkinen L, Kaprio J, Dick DM. Parenting mechanisms in links between parents’ and adolescents’ alcohol use behaviors. Alcoholism. 2008;32(2):322–30. doi: 10.1111/j.1530-0277.2007.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haugland SH, Holmen TL, Ravndal E, Bratberg GH. Parental alcohol misuse and hazardous drinking among offspring in a general teenage population: gender-specific findings from the Young-HUNT 3 study. BMC Public Health. 2013;13(1):1140. doi: 10.1186/1471-2458-13-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haugland SH, Strandheim A, Bratberg G. Is high-risk use of intoxicants more common among adolescents who have seen their parents intoxicated? Tidsskrift for den Norske laegeforening. 2012;132(4):410–3. doi: 10.4045/tidsskr.11.0623. [DOI] [PubMed] [Google Scholar]
- 13.Jacob T, Windle M, Seilhamer RA, Bost J. Adult children of alcoholics: drinking, psychiatric, and psychosocial status. Psychol Addict Behav. 1999;13(1):3. [Google Scholar]
- 14.Rossow I, Lambert F, Keating P, McCambridge J. Parental drinking and adverse outcomes in children – a scoping review of cohort studies. Drug Alcohol Rev. 2015 doi: 10.1111/dar.12319. Published online August 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rossow I, Keating P, Felix L, McCambridge J. Does parental drinking influence children’s drinking? A systematic review of prospective cohort studies. Addiction. 2015 doi: 10.1111/dar.12319. Published online: 16 OCT 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Babor TF, Caetano R, Casswell S, et al. Alcohol: No Ordinary Commodity: Research and Public Policy. Oxford: Oxford Univsersity Press; 2010. [DOI] [Google Scholar]
- 17.Morland J. Medisin og vitenskap-Tema alkohol-Biologiske virkningsmekanismer og noen kliniske effekter av alkohol [Biological mechanisms of action in alcohol use] Tidsskr Nor Laegeforen. 2003;123(2):180–4. [PubMed] [Google Scholar]
- 18.Rossow I, Moan IS, Natvig H. Nære pårørende av alkoholmisbrukere: hvor mange er de og hvordan berøres de? Only in Norwegian. [Persons with Close Relations to Alcohol Abusers: How Many They are and How They Affected?] SIRUS; Oslo: 2009. [Google Scholar]
- 19.Torvik F, Rognmo K. Barn av foreldre med psykiske lidelser eller alkoholmisbruk: omfang og konsekvenser. Only in Norwegian. [Children of Parents with Mental Illness or Alcohol Abuse: Extent and Consequences] Vol. 2011. Oslo, Norway: Norwegian Institute of Public Health; 2011. p. 4. [Google Scholar]
- 20.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 21.Christoffersen MN, Poulsen H, Nielsen A. Attempted suicide among young people: risk factors in a prospective register based study of Danish children born in 1966. Acta Psychiatr Scand. 2003;108(5):350–8. doi: 10.1034/j.1600-0447.2003.00165.x. [DOI] [PubMed] [Google Scholar]
- 22.Lyngstad TH, Skardhamar T. Nordic register data and their untapped potential for criminological knowledge. Crime Justice. 2011;40(1):613–45. [Google Scholar]
- 23.Holmen TL, Bratberg G, Krokstad S, et al. Cohort profile of the Young-HUNT Study, Norway: a population-based study of adolescents. Int J Epidemiol. 2013;43(2):536–44. doi: 10.1093/ije/dys232. [DOI] [PubMed] [Google Scholar]
- 24.Österberg E. Finnish attitudes to alcohol policy in 2005. J Subst Use. 2007;12(6):419–26. [Google Scholar]
- 25.Brand DA, Saisana M, Rynn LA, Pennoni F, Lowenfels AB. Comparative analysis of alcohol control policies in 30 countries. PLoS Med. 2007;4(4):e151. doi: 10.1371/journal.pmed.0040151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karlsson T, Österberg E. A scale of formal alcohol control policy in 15 European countries. Nordisk Alkohol Och Narkotikatidskrift. 2001;18:117–28. [Google Scholar]
- 27.Skretting A, Lund KE, Bye EK. Rusmidler i Norge 2013. 2014. The Norwegian Institute fr Alcohol and Drug Research, Editor. [Google Scholar]
- 28.Horverak Ø, Bye EK. Det norske drikkemønsteret: en Studie basert på intervjudata fra 1973–2004. Only in Norwegian. [Enligsh title: The Norwegian Drinking Pattern: A Study Based on Interview Data From 1974 to 2004] Vol. 2007. Oslo: Statens istitutt for rusmiddelforskning; p. 248s. [Google Scholar]
- 29.Holmen J, Midthjell K, Krüger Ø, et al. The Nord-Trøndelag Health Study 1995–97 (HUNT 2): objectives, contents, methods and participation. Norsk Epidemiologi. 2003;13(1):19–32. [Google Scholar]
- 30.Krokstad S, Langhammer A, Hveem K, et al. Cohort profile: the HUNT Study, Norway. Int J Epidemiol. 2013;42(4):968–77. doi: 10.1093/ije/dys095. [DOI] [PubMed] [Google Scholar]
- 31.SSB . Standard for gruppering av familiar og hushald. Only in Norgwegian. [Standard for Grouping of Families and Households 2002] SSB; Kongsvinger: 2002. [Google Scholar]
- 32.Furu K. Establishment of the nationwide Norwegian Prescription Database (NorPD) – new opportunities for research in pharmacoepidemiology in Norway. Norsk Epidemiologi. 2008;18(2):129–36. [Google Scholar]
- 33.WHO . WHO Collaborating Centre for Drug Statistics Methodology ATC Classification Index with DDDs 2010. Oslo, Norway: Norwegian Institute of Public Health; 2010. [Google Scholar]
- 34.Rognmo K, Torvik FA, Ask H, Røysamb E, Tambs K. Paternal and maternal alcohol abuse and offspring mental distress in the general population: The Nord-Trondelag Health Study. BMC Public Health. 2012;12(1):448. doi: 10.1186/1471-2458-12-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.The Norwegian Institute of Public Health The Norwegian Prescription Database. 2014. Available at: http://www.norpd.no.
- 36.Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252(14):1905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 37.Skogen JC, Øverland S, Knudsen AK, Mykletun A. Concurrent validity of the CAGE questionnaire. The Nord-Trøndelag Health Study. Addict Behav. 2011;36(4):302–7. doi: 10.1016/j.addbeh.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 38.Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131(10):1121–3. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- 39.Wu SI, Huang HC, Liu SI, et al. Validation and comparison of alcohol-screening instruments for identifying hazardous drinking in hospitalized patients in Taiwan. Alcohol Alcohol. 2008;43(5):577–82. doi: 10.1093/alcalc/agn036. [DOI] [PubMed] [Google Scholar]
- 40.Homlong L, Rosvold EO, Sagatun A, Wentzel-Larsen T, Haavet OR. Living with mentally ill parents during adolescence: a risk factor for future welfare dependence? A longitudinal, population-based study. BMC Public Health. 2015;15(1):413. doi: 10.1186/s12889-015-1734-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Torvik FA, Rognmo K, Tambs K. Alcohol use and mental distress as predictors of non-response in a general population health survey: the HUNT study. Soc Psychiatry Psychiatr Epidemiol. 2012;47(5):805–16. doi: 10.1007/s00127-011-0387-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17(9):643–53. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 43.Ellis DA, Zucker RA, Fitzgerald HE. The role of family influences in development and risk. Alcohol Health Res World. 1997;21:218–26. [PMC free article] [PubMed] [Google Scholar]
- 44.Little K, Hawkins MT, Sanson A, et al. The longitudinal prediction of alcohol consumption-related harms among young adults. Subst Use Misuse. 2012;47(12):1303–17. doi: 10.3109/10826084.2012.699577. [DOI] [PubMed] [Google Scholar]
- 45.Little K, Hawkins MT, Sanson A, et al. Longitudinal predictors of alcohol-related harms during the transition to adulthood. Aust Psychol. 2013;48(4):270–80. [Google Scholar]
- 46.Fisher LB, Miles IW, Austin SB, Camargo CA, Colditz GA. Predictors of initiation of alcohol use among US adolescents: findings from a prospective cohort study. Arch Pediatr Adolesc Med. 2007;161(10):959–66. doi: 10.1001/archpedi.161.10.959. [DOI] [PubMed] [Google Scholar]
- 47.Homish GG, Edwards EP, Eiden RD, Leonard KE. Analyzing family data: a GEE approach for substance use researchers. Addict Behav. 2010;35(6):558–63. doi: 10.1016/j.addbeh.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Johnson TP. Sources of error in substance use prevalence surveys. Int Sch Res Notices. 2014(2014):21. doi: 10.1155/2014/923290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Aaberge R, Laake P. Om statistiske teoriar for tolking av data. Only in Norwegian. [On theories for statistical interpretation of data] Tidsskr Samfunnsforsk. 1984;25(2):165–86. [Google Scholar]
- 50.Rothman KJ, Gallacher JE, Hatch EE. Why representativeness should be avoided. Int J Epidemiol. 2013;42(4):1012–4. doi: 10.1093/ije/dys223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hingson R, Heeren T, Winter M. Effects of recent 0.08% legal blood alcohol limits on fatal crash involvement. Inj Prev. 2000;6(2):109–14. doi: 10.1136/ip.6.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]