Abstract
Uptake of vaccination against seasonal influenza is suboptimal in most countries, and campaigns to promote vaccination may be weakened by clustering of opinions and decisions not to vaccinate. This clustering can occur at myriad interacting levels: within households, social circles, and schools. Given that influenza is more likely to be transmitted to a household contact than any other contact, clustering of vaccination decisions is arguably most problematic at the household level. We conducted an international survey study to determine whether household members across different cultures offered direct advice to each other regarding influenza vaccination and whether this advice was associated with vaccination decisions. The survey revealed that household members across the world advise one another to vaccinate, though to varying degrees, and that advice correlates with an increase in vaccination uptake. In addition, respondents in Japan, China, and the US were less likely to offer advice to older adults than to the young, despite older adults being the target age group for vaccination in both far eastern countries. Furthermore, advice was not primarily directed to household members within the age groups advised to vaccinate by national health policies. In Japan, advice was offered more to ages outside of the policy guidelines than inside. Harnessing the influence of household members may offer a novel strategy to improve vaccination coverage across cultures worldwide.
Introduction
The probability of contracting a highly contagious pathogen such as seasonal influenza critically depends on the level of exposure to others who are infected. This level of exposure is determined by the number and nature of contacts between individuals. Household members have frequent and often prolonged interactions with each other (1). An estimated 30% of influenza is spread within households (2), and living in a household with an infected person is the largest risk factor for contracting influenza (2,3,4). Accordingly, household-based interventions are important for curtailing outbreaks in surrounding communities (2,5). Health policy interventions that promote influenza vaccination uptake are important worldwide because vaccination levels in most countries are significantly lower than the 75% recommended by the WHO, even among the elderly, the age-class most likely to be vaccinated (6). There is substantial heterogeneity in influenza vaccine coverage between countries and across age groups, suggesting that culture-specific factors may contribute to disease burden and influence the effectiveness of health communication within each country.
Close contacts, such as those occurring in a household, may increase exposure to infection but can also influence healthcare decision-making (7). Consequently, household contacts may drive complex interdependent dynamics of vaccination decisions and disease transmission (8). Indeed, spatial clustering of opinions about whether to vaccinate when overlaid with epidemiological dynamics may reduce vaccine effectiveness in the entire population (9, 10). Spatial clustering of opinions can occur via three mechanisms: 1) induction (direct and indirect influence of others' opinions and behaviors), 2) homophily (association with individuals because of their similar opinions or behaviors), and 3) confounders (environmental determinants of similar opinions or behaviors) (11). Quantifying vaccine opinion clustering within households and understanding the associated cultural factors might help to explain low vaccination uptake and could lead to improvements in public health messages to mitigate future influenza epidemics.
There is reason to expect cultural differences in opinion clustering within households. For example, Hofstede has shown that eastern cultures display greater collectivism while western cultures display greater individualism (12). Thus, a reasonable hypothesis is that members of a collectivist culture in the east would be more influenced by household members than members of an individualist culture in the west, which encourages independent decisions. In addition, people of certain ages might have different amounts of influence in eastern and western cultures. For example, the Confucian tradition in eastern cultures emphasizes respect to the elderly, where the elderly are ones to give, but not to receive, advice. Vaccination decisions may also be influenced by an array of country-specific factors, such as geographic location, government vaccination recommendation, and healthcare systems.
Here we quantify the extent of household clustering of vaccination uptake and advice-giving in eight countries: Brazil, China, France, Israel, Japan, South Africa, the U.K., and the U.S. The eight countries were selected to provide a range with regard to the following factors:
general cultural differences: far eastern (Japan and China), western (U.S., U.K. and France), and other countries (Brazil, Israel and South Africa);
healthcare system types, including single-payer (UK), mostly private insurance with some federal provision (US), and mostly state-funded with supplemental private insurance and individual co-payments (France) (13);
influenza vaccination uptake rates, ranging from over 70% for the elderly in Brazil (14) to under 40% for the elderly in Japan, Israel, South Africa (15);
influenza vaccination national recommendations, including countries that recommend vaccination for only elderly (Brazil, France, Japan, UK), only elderly and children (China), all ages (Israel, US), and no specific age groups (South Africa);
geographical position (northern and southern hemispheres).
We compare the tendency to advice across countries and age groups, and we examine the impact of advice on respondent vaccination decisions. We examine the age of respondents and household members because some countries vary their vaccine recommendations by age.
We conclude that the direct influence of household members advising one another to vaccinate may significantly affect the overall vaccination uptake within many countries. Additionally, the scale and age-dependency of this household influence varies substantially worldwide, suggesting that effective health communication must be country-specific and culturally sensitive.
Methods
Data collection
The survey was conducted on the Internet, and respondents were recruited by the commercial survey company Research Now (RN). We recruited 4023 participants from eight countries to complete a survey on attitudes and behaviors regarding seasonal influenza. We excluded 63 respondents who answered the survey outside the country of residence listed in the RN database, in case they changed their country of residence since registering with RN. Two respondents took the survey twice, and we excluded their second responses. Six respondents claimed to be less than 18 years old and were excluded. These exclusions resulted in 3952 responses. Single-person households were also excluded from analysis, except for demographics and overall vaccination rates. The first author performed the data cleaning.
Respondents who completed the survey were compensated at the normal rate provided by RN. Participants were recruited via email and the survey was only made available online. RN contacted pre-subscribed panelists via email informing them of the survey. The survey link brought the respondent directly to the survey in the primary language of their location (Portuguese for Brazil, Simplified Chinese for China, French for France, Hebrew for Israel, Japanese for Japan, British English for South Africa, British English for UK, American English for US). Respondents could change the survey language to any of the seven alternatives on the landing page. The survey materials and the translations were written by the authors and research assistants (acknowledged) who were fluent in the respective language. The translations were also reverse-translated by different research assistants (acknowledged) who were fluent in the respective languages and who were not involved in design of the original survey to ensure that the survey meaning was preserved. Pilot versions of the survey were conducted to gauge the response rates for each country and to ensure the survey flow was correct.
Prior to the start of data collection, we requested 500 complete responses per country from RN. Data from China (N=499), France (N=497), Japan (N=501), United Kingdom (N=496) and United States (N=473) were collected in 2013 between September 13 and September 23, before the start of the influenza season. Data from Israel (N=500) were collected in 2013 between October 1 and October 5 to avoid a major Israeli holiday. Data from Brazil (N=490) and South Africa (N=496) were collected in 2014 between March 10 and March 18, before the start of the southern hemisphere flu season. Only complete surveys were included in the final data counts and analysis. The complete response rates per country ranged from 2% (China) to 20% (Japan), with a median of 10.5%.
We placed quotas on survey uptake during recruitment to obtain a representative sample (Table 1). For all countries in the northern hemisphere, a quota was set to include 50% males and 50% females. For France, Japan, UK and US, a quota was set to include 20% of participants 50 years or older. In China, a quota was set to include 30% of participants 35 years or older, due to lack of older Internet panelists above age 50. In Israel no age quotas were set due to shortage of Internet panelists. In Brazil, a quota was set to include 10% of participants 50 years or older, due to lack of older Internet panelists. In South Africa no quotas were set due to shortage of Internet panelists.
Table 1.
Summary of survey demographics, household (HH) vaccination advice results, and cultural/socio-economic indices.
| Brazil | China | France | Israel | Japan | S. Africa | UK | US | |
|---|---|---|---|---|---|---|---|---|
| Female (%) | 52 | 51 | 53 | 59 | 53 | 61 | 52 | 53 |
| Age <50 years (%) | 90 | 93 | 79 | 71 | 77 | 83 | 81 | 78 |
| Mean Household Size | 4 | 3.4 | 2.5 | 3.4 | 2.6 | 3.7 | 2.7 | 2.5 |
| Mean HH Size excluding single-person HH | 4.2 | 3.6 | 3.1 | 3.6 | 3.1 | 3.9 | 3 | 3 |
|
| ||||||||
| HH with respondent giving advice (%) | 46 | 35 | 14 | 15 | 29 | 23 | 14 | 29 |
| Collectivism index | 62 | 80 | 29 | 46 | 54 | NA | 11 | 9 |
| GINI score | 52 | 47 | 31 | 38 | 38 | 63 | 32 | 45 |
We obtained IRB approval prior to conducting the surveys. All consent forms were translated and back-translated as per survey protocol above and were approved by all respondents prior to completion of the survey.
Survey questionnaire
Respondents gave their age, gender, and reported whether or not they had received an influenza vaccine during the previous season. Respondents were asked to list all members of their household excluding themselves (up to eight). For each household member, respondents were asked for their age, gender, and the nature of the respondent's relationship to them (selected from: spouse/partner, child, parent, grandparent, brother or sister, other family member, friend, other non-family member). Only respondents with other household members are included in the analyses (Table 1).
Respondents stated whether or not they had attempted to influence each household member in their decision to vaccinate the previous year, selecting one choice from the following three answers:
“Yes, I tried to convince this person to get vaccinated,”
“Yes, I tried to convince this person to NOT get vaccinated,” and
“No, I did not try to convince this person either way.”
Respondents then stated whether the same household member had tried to influence their decision to vaccinate as follows, selecting one choice from the following three answers:
“Yes, this person tried to convince me to get vaccinated,”
“Yes, this person tried to convince me to NOT get vaccinated,” and
“No, this person did not try to convince me either way.”
Finally, respondents stated whether the advice from the other household member had influenced their decision to be vaccinated as follows, selecting one choice from the following three answers:
“Yes, this person influenced my decision to be vaccinated,”
“Yes, this person influenced my decision NOT to be vaccinated,”
“No, this person did not influence my decision either way.”
Analysis details
We coded respondent vaccination as 1 if the respondent vaccinated the previous year and 0 if the respondent did not vaccinate or did not know whether or not they had vaccinated. We coded advice (household member to respondent or vice versa) as 1 if the advisor told the advisee to vaccinate and 0 otherwise. Age groups were coded as nominal variables using the following groups: 1–17, 18–39, 40–59, and 60+ years. We excluded relationship type from the analyses given that relationship was correlated with age (e.g., parents were older, children were younger).
For significance testing of interactions and main effects, we performed chi-square model comparison tests. For interaction tests, we compared a model with all interactions to a model excluding the single interaction of interest. For main effect tests, we compared a model with all significant interactions and the non-interacting main effect of interest to the same model but without the non-interacting main effect. The same approach was used in all of our regression analyses. We used a conservative alpha of 0.01.
For several analyses we also conducted post-hoc regression contrasts, which were Wald tests on linear combinations of parameters from the regression model including only the significant interactions and main effects.
Results
Household demographics and vaccination tendencies
Household size and composition from our sample did not vary dramatically across countries. Across all countries, the most common household member relationship types were the child, spouse, and parent of the respondent (Figure 1). The household sizes reported in the survey align well with those reported in national-level data, which range from 2.5 in France to 3.7 in South Africa. Survey respondents from Brazil, China, France, Japan, and the UK produced a slightly higher household size than reported in national-level data. Respondents from Israel, South Africa, and the US produced a slightly lower household size than reported in national-level data. The small differences are likely due to limitations of our sampling procedure, as we were only able to apply loose age quotas for most countries.
Figure 1.
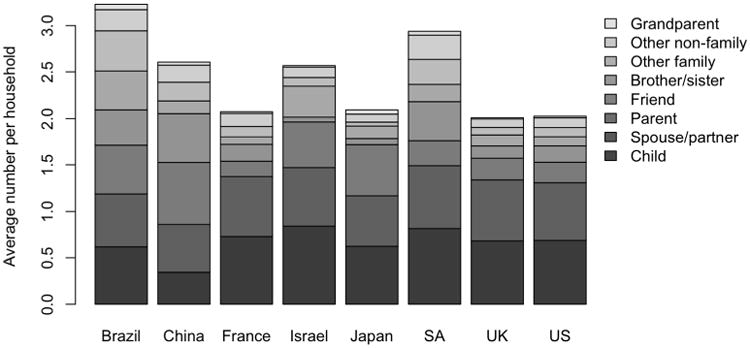
Average numbers of other household members (excluding the respondent), by relationship type.
Respondent advice tendencies
We performed a series of logistic regressions with “advice from the respondent to a household member” (to vaccinate vs. to NOT vaccinate or no advice) as the dependent variable. Predictors included country of household, respondent age group, household member age group, and all two-way interactions. Data regarding household members under 1 year old as recipient of advice were excluded from this analysis given that in certain countries these children are not eligible for the flu vaccine (e.g., in the US, children under 6 months are not eligible). Overall, the tendency to give vaccination advice depends on country of residence and the ages of both the adviser and advisee. The country and household member age interaction was significant, χ2(21)=136.33, p<0.001. Neither the respondent age and household member age interaction, χ2 (6)=15.63, p=0.02, nor the country and respondent age interaction, χ2(14)=15.08, p=0.32, was significant. The main effect of respondent age was significant, χ2(2)=18.68, p<0.001.
The main effect of respondent age group was due to greater proportions of advice being given by older respondents. Respondents aged 18-39 advised on average 17.5% of household members, compared to respondents aged 40-59 advising 19.4%, and respondents 60+ advising 21.5%. We compared each age group to the other with pair wise contrasts and using adjusted alpha of 0.05/3=0.0167. Advice tendency differed between respondents aged 18-39 and both older age groups—those aged 40-59, t(8242)=3.25, p=0.001, and those aged 60+, t(8242)=3.51, p<0.001. However, advice tendency did not differ between the two older age groups, t(8242)=1.81, p=0.07. The greater propensity for older individuals to offer advice regarding vaccination may be due to a greater chance that older individuals offer advice in general (for example, older individuals are more likely to be parents), or because they are more aware of seasonal influenza vaccination because of national-level programs aimed mostly at elderly individuals.
The interaction between county and household member age appears to stem from differences between countries in advice giving to the youngest versus oldest household members (Figure 2). Thus, for selected countries we compared advice tendencies to ages 1-17 and to ages 60+. In both tests we considered three countries, which were selected post-hoc to examine the largest differences between the youngest and oldest age groups. To adjust our alpha level, we divided 0.05 by the number of equivalent such tests: 0.05 divided by 58 (ways to choose 3 countries from 8) times 6 (ways to choose two age groups from 4), or 0.05/(58*6)=0.00014. These tests indicated that respondents in China, Japan, and the U.S. advised children and adolescents aged 1–17 years more than adults aged 60+ years, t(8242)=6.7, p<0.0001, and conversely, respondents in France, Israel, and the UK advised the adults aged 60+ years more than children and adolescents aged 1–17 years, t(8242)=4.48, p<0.0001).
Figure 2.
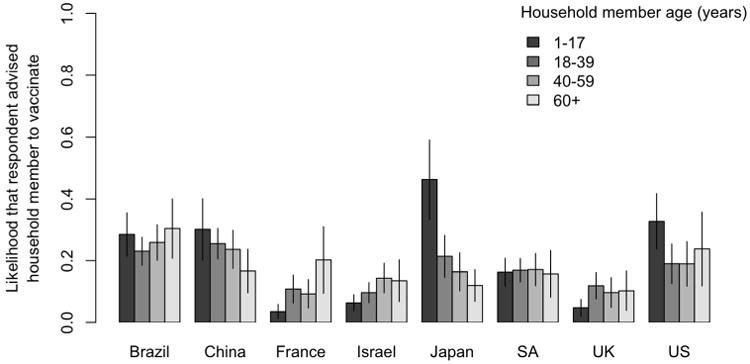
Likelihood of respondent advising a household member to vaccinate by country of residence and age of the household member being advised (or not advised). Vertical lines indicate 95% confidence intervals.
An alternative way to interpret the above interaction is to examine differences in advice tendency across countries, separately for older and younger advisees. The tendency to advise younger household members appeared lower for European and Near East countries, including France, Israel, and the UK, but the same effect for older household members was weak. The former contrast concerning advisees ages 1-17 was significant, t(8242)=12.13, p<0.0001, but the latter concerning advisees 60+ was not significant, t(8242)=2.26, p=0.02.
Effects of advice from household members on respondent vaccination
The next analysis focused on respondent vaccination status the previous year. Predictors included advice from any household member to respondent (to vaccinate vs. to NOT vaccinate or no advice), country, and age of respondent
Overall, the tendency of the respondent to vaccinate depends on the country of residence, respondent age and whether they were advised by a household member to be vaccinated. The household member advice by country interaction was significant (Figure 3A), χ2(7)=21.93, p=0.003, as was the country by respondent age interaction, χ2(14)=44.45, p<0.001. The household member advice by respondent age interaction was not significant, χ2(2)=2.61, p=0.27. These interactions suggest that the impact of household member advice on the eventual decision to vaccinate varies across countries, and the dependency of vaccination rates on age also varies across countries.
Figure 3.
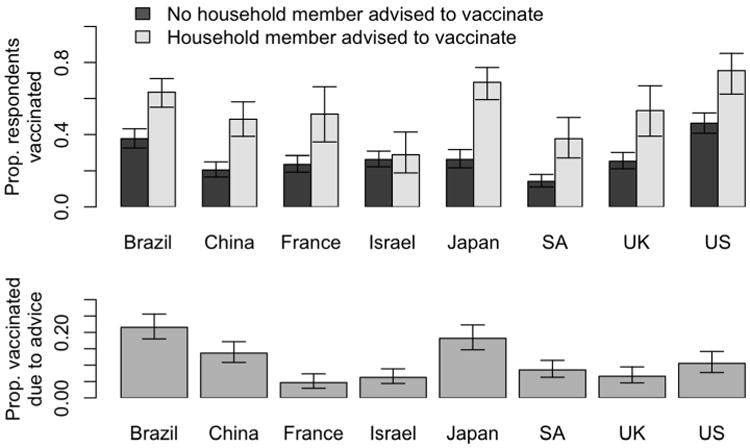
(A) Proportion of respondents who vaccinated by their country of residence and whether or not at Least one household member advised them to vaccinate (top). (B) Proportion of respondents who vaccinated because they were advised by a household member, separately per country (bottom). Error bars indicate 95% confidence intervals
Contrasts revealed that the interaction between country and advice is due to respondents in all countries except Israel showing a positive effect of advice on vaccination status (Figure 3A). Using an adjusted alpha of 0.05/7=0.007, all simple main effects of advice, per country, were significant, except for Israel.
Japan showed the greatest impact of advice, where the odds of a respondent vaccinating are 6.3 times greater for respondents who received advice from household member(s) than for respondents without such advice. The smallest effect (aside from Israel) is in Brazil, where the odds are still 2.9 times greater for respondents receiving advice.
The influence of household members on vaccination decisions may occur through persuasive conversations about whether to receive the influenza vaccine, or it may occur through observation and imitation of others within the household who vaccinate (16, 17). To evaluate how much of the influence from advice is due to direct persuasion, we calculated the proportion of respondents in each country who reported having vaccinated specifically because of the advice given by the household member (Figure 3B). The largest influence of advice is seen in Brazil and Japan, where 18% and 22% of respondents, respectively, said they vaccinated due to the advice of a household member. The lowest proportions are in France (5%), Israel (6%), and the UK (7%). The countries in which advising is less common (UK, France, and Israel) are also the countries in which the decision to be vaccinated is less likely to be influenced by household advice.
Relations to country-specific vaccination policies
In this final analysis, we assessed the extent to which patterns of household advice align with age-specific recommendations of the respective national health authorities regarding vaccination prioritization. The dependent variable was “advice from the respondent to a household member” (to vaccinate vs. to NOT vaccinate or no advice), and predictors included country, whether the household member's age group is targeted by the health authorities to be vaccinated, and the interaction effect. For illustration, in the UK people 65 years and older are targeted for vaccination. Hence, a household member in the UK who is 30 years old would be coded as 0, and a household member who was 70 years old would be coded as 1. We excluded South Africa from the analysis, which has no current age-specific vaccination policy. We also excluded the US and Israel, which both recommend vaccination to all age groups.
The interaction between country and target age group was significant, χ2(4)=17.64, p=0.001. Using an adjusted alpha of 0.05/5=0.01, we found that all simple main effects of advice, per country, were nonsignificant, except for Japan, which was significant, t(5026)=-2.91, p=0.004 (Figure 4). Interestingly, in Japan advice giving stood in direct opposition to public policy. Hence, national level recommendations are either not reflected or are in direct contrast to patterns of household advice.
Figure 4.
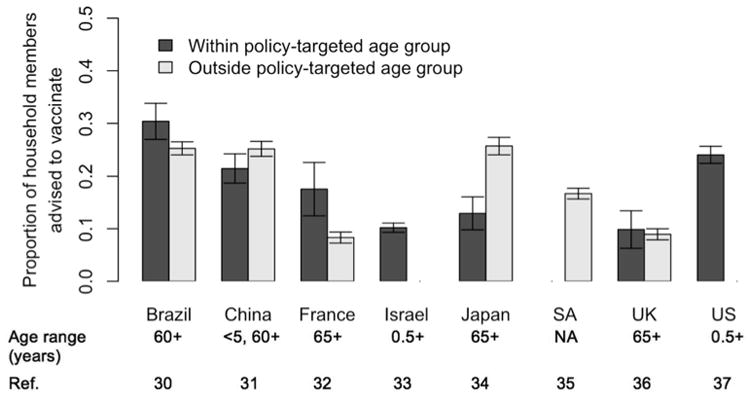
For each country, the proportion of household members that a respondent advised to vaccinate and whether they were within (black) or outside (grey) the age group advised to receive influenza vaccination by the national health authorities. Age-specific vaccine recommendations are provided below each country name. Note: South Africa has no current age-specific vaccination policy.
Discussion
Our results suggest that households are sources for information regarding vaccination against seasonal influenza. Therefore, public health messaging may be acting directly, reaching those individuals for whom the messages are targeted, and indirectly, reaching household members of individuals who discuss the messages with their household. Achieving both effects through public health messaging (e.g., via advertising campaigns), may be analogous to mass vaccination itself, the benefits of which are realized through direct protection of the vaccinated individuals as well as indirect protection through reduced transmission, especially within the household (2, 3, 4).
Our results suggest that the impact of indirect communication of public health messages depends on the country and culture that individuals live in. While the size and age distributions of households do not vary substantially between the countries that we surveyed, the level of communication about vaccination does differ. Cultural differences may dictate the overall willingness of household members to advise each other on vaccination decisions. For instance, public health messages that promote advising the elderly to vaccinate in China and Japan might not be successful due to reluctance to advice elders in East Asian culture (18).
Cross-national differences in the willingness to advise household members could be attributable to cultural differences or to attitudes toward healthcare decision-making and toward state-mandated healthcare policy. While it is difficult to disentangle these effects, our results suggest that cultural differences do play a role. An important example is Japan, where despite vaccination being recommended for elderly individuals, young household members were more likely to receive advice than older household members. This was also true to a smaller degree in China. By contrast, the countries with low levels of advice giving in Europe and the Near East, who also have centralized state-funded healthcare systems, tended to provide advice to older individuals, the focus of the state's vaccine policy. The U.K. recently piloted a seasonal influenza vaccination program aimed at toddlers and adolescents, with parents showing strong support for childhood vaccination (19). As the program is expanded nationally, parental awareness and advice-giving to older teens will prove critical to the scheme's success.
The East-West differences in vaccination toward younger and older household members have two potential explanations. First, advice may serve as an index of general positive attitudes towards the advisee, as it indicates that the advisor cares about protecting the health of the advisee. Despite popular assumptions, a recent meta-analysis on east-west difference in attitudes towards the elderly reveals that eastern countries hold more negative views of the elderly than western countries (20). Thus, the lack of advice giving towards the elderly in Japan and China may reflect a negative attitude towards elderly household members among Japanese and Chinese participants, especially when compared to their western counterparts (excluding the U.S.). An alternative explanation is that Asians are more obedient and respectful of their elderly family members than their Western counterparts due to filial piety (18). Hence, younger Asians may be less likely to engage in behaviors towards the elderly, such as advice-giving, that imply greater power and status of the actor.
Countries with age-related seasonal influenza vaccination policies will also have health-related policies, such as targeting those with chronic conditions who are most at risk of influenza-related complications. Through awareness of these policies, individuals may be more likely to vaccinate to protect a fellow household member who is identified as at risk. This behavior would lead to household clustering of vaccination behaviors through both indirect induction and confounding.
The interaction between age of household member advisee and country suggests a complex landscape of advice-giving based on cultural norms as well as health policy awareness and vaccination availability. As such, designated cultural dimensions such as Individualism/Collectivism as proposed by Hofstede and colleagues (22, 23) may not fully explain our results. Indeed, we examined the relationship between Hofstede's collectivism index (22) and the percentage of respondents advising household members (Figure 5). We found a modest positive relationship between collectivism and advice, r=0.59, p=0.16.
Figure 5.
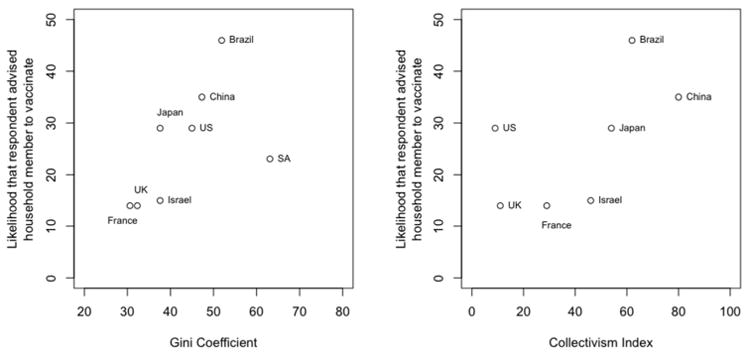
For each country, the Gini Coefficient (left) (26, 27) and Collectivism Index (right) (16) plotted against the mean likelihood of respondents from that country advising a household member to vaccinate.
Similarly, we observed a modest positive relationship between advice and the Gini coefficient (24), r=0.55, p=0.12, suggesting that people in countries with greater social inequality were more likely to give advice. Although both correlations suggest a positive trend, we interpret these data cautiously given the evident lack of statistical power. In addition, the notable outliers underscore the complexity of cultural explanations for health advising. Exploring these nuances in further detail is a topic for future research.
Limitations
We note two main limitations of our study. First, while online surveys provide a fast and efficient means to obtain international participants, they may suffer from selection bias and accessibility issues when compared to telephone or face-to-face interviews (25). Nevertheless, Internet panels compare favorably to samples collected from common alternative survey strategies, such as college-based recruitment (26). Further, reviews suggest no systematic differences in effects between Internet-based samples and non-Internet based samples (27, 28), although some evidence suggests that results from hard to reach-sub populations that do respond well to Internet surveys may suffer from weak generalizability (29). As mentioned above, we used quotas to mitigate age and gender bias in our sample. However, for some countries this was not possible, leading to an over-representation of respondents under 50. We partially mitigated this possible bias by explicitly accounting for age of respondent in the analyses.
A second limitation is that we did not qualify the word “advice” in the survey, leaving this open to the respondents' interpretations. In particular for advice giving to the youngest age class, respondents may have different opinions regarding whether they “gave advice” to their child, for example, or “chose whether the child should receive the vaccine”. Thus, when “advise” is interpreted broadly as “tried to exert influence over”, there may be even more adults who do indeed advise their children to vaccinate.
Conclusion
Our results show that vaccination advice shared within the household impacts the decision to vaccinate, although the nature of this advice and the scale of impact on vaccination vary across countries and cultures. Hence, campaigns aimed at encouraging household advice, specifically using culture-specific messages and strategies, have the potential to increase vaccination rates.
Acknowledgments
The authors thank Hilary Atkins, Michal Hall side, Atila Iamarino, Yoko Ibuka, Paula Luz, Martial Ndeffo Mbah, Claudio Struchiner and Dan Yamin for survey translation and reverse-translation. We also thank Wang Zhang for translation and for comments on the manuscript. We are grateful to funding from the NIH (grant U01-GM105627-01), the NSF (grants SES-1227390 and SES-1227306), and the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Immunisation at the London School of Hygiene and Tropical Medicine in partnership with Public Health England (PHE).
Financial support for this study was provided in part by funding from NIH (grant U01-GM105627-01), NSF (grants SES-1227390 and SES-1227306) and National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Immunisation at the London School of Hygiene and Tropical Medicine in partnership with Public Health England (PHE). The funding agreement ensured the authors' independence in designing the study, interpreting the data, writing, and publishing the report. The views expressed are those of the authors and not necessarily those of the NIH, NSF, NHS, NIHR, UK Department of Health or PHE.
References
- 1.Mossong Joël, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS medicine. 2008;5.3:e74. doi: 10.1371/journal.pmed.0050074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferguson Neil M, et al. Strategies for mitigating an influenza pandemic. Nature. 2006;442.7101:448–452. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cauchemez S, et al. A Bayesian MCMC approach to study transmission of influenza: application to household longitudinal data. Statistics in medicine. 2004;23.22:3469–3487. doi: 10.1002/sim.1912. [DOI] [PubMed] [Google Scholar]
- 4.Longini Ira M, et al. Estimating household and community transmission parameters for influenza. American Journal of Epidemiology. 1982;115.5:736–751. doi: 10.1093/oxfordjournals.aje.a113356. [DOI] [PubMed] [Google Scholar]
- 5.Wu Joseph T, et al. Reducing the impact of the next influenza pandemic using household-based public health interventions. PLoS medicine. 2006;3.9:e361. doi: 10.1371/journal.pmed.0030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.http://www.who.int/immunization/sage/1_WHA56_19_Prevention_and_control_of_influenza_pandemics.pdf. Accessed 31st July 2014.
- 7.Bauch Chris T, Galvani Alison P. Socialfactors in epidemiology. Science. 2013;342.6154:47–49. doi: 10.1126/science.1244492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Funk Sebastian, Salathé Marcel, Jansen Vincent AA. Modelling the influence of human behaviour on the spread of infectious diseases: a review. Journal of the Royal Society Interface. 2010;7.50:1247–1256. doi: 10.1098/rsif.2010.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salathé Marcel, Bonhoeffer Sebastian. The effect of opinion clustering on disease outbreaks. Journal of The Royal Society Interface. 2008;5.29:1505–1508. doi: 10.1098/rsif.2008.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eames Ken TD. Networks of influence and infection: parental choices and childhood disease. Journal of The Royal Society Interface. 2009;6.38:811–814. doi: 10.1098/rsif.2009.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christakis Nicholas A, Fowler James H. Social contagion theory: examining dynamic social networks and human behavior. Statistics in medicine. 2013;32.4:556–577. doi: 10.1002/sim.5408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hofstede G. Values survey module 1994 manual. University of Limburg, Maastricht, The Netherlands: Institute for Research on Intercultural Cooperation; 1994. [Google Scholar]
- 13.Durand-Zaleski Isabelle. The health system in France. EUROHEALTH-LONDON. 2008;14.1:3. [Google Scholar]
- 14.Ropero-Álvarez Alba M, et al. Expansion of seasonal influenza vaccination in the Americas. BMC Public Health. 2009;9.1:361. doi: 10.1186/1471-2458-9-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.http://ecdc.europa.eu/en/press/events/Documents/ECDC-WHO-influenza-meeting-Brown-3.pdf. Accessed 16th Jan 2015
- 16.Hurley Susan L, Chanter Nick., editors. Perspectives on Imitation: Mechanisms of imitation and imitation in animals. Vol. 1. MIT Press; 2005. [Google Scholar]
- 17.Pingle Mark. Imitation versus rationality: An experimental perspective on decision making. The Journal of Socio-Economics. 1995;24.2:281–315. [Google Scholar]
- 18.Ng SH. Social psychology in an ageing world: Ageism and intergenerational relations. Asian Journal of Social Psychology. 1998;1.1:99–116. [Google Scholar]
- 19.Thors Valtyr, Moulsdale Phoebe, Finn Adam. Parental Views on Childhood Influenza Vaccination. The Pediatric infectious disease journal. 2014;33.3:334–335. doi: 10.1097/INF.0000000000000236. [DOI] [PubMed] [Google Scholar]
- 20.North Michael Steven. From jurassic to classic and east to west, an inconvenienced youth: Explaining, measuring, and reducing age bias. PRINCETON UNIVERSITY; 2013. Diss. [Google Scholar]
- 22.Hofstede Geert, et al. Values survey module 2008. 2008 URL: http://www.geerthofstede.nl/media/253/VSM08English.doc (Stand 30.06. 2010)
- 23.Hofstede Geert, Hofstede Gert Jan, Minkov Michael. Cultures and organizations: Software of the mind: Intercultural cooperation and its importance for survival. McGraw-Hill; USA, New York: 2010. [Google Scholar]
- 24.https://www.cia.gov/library/publications/the-world-factbook/rankorder/2172rank.html. Accessed 16th Jan 2015
- 25.Wright KB. Researching Internets-based populations: Advantages and disadvantages of online survey research, online questionnaire authoring software packages, and web survey services. Journal of Computer-Mediated Communication. 2005;10(3):00–00. [Google Scholar]
- 26.Paolacci G, Chandler J. Inside the Turk Understanding Mechanical Turk as a Participant Pool. Current Directions in Psychological Science. 2014;23(3):184–188. [Google Scholar]
- 27.Germine L, Nakayama K, Duchaine BC, Chabris CF, Chatterjee G, Wilmer JB. Is the Web as good as the lab? Comparable performance from Web and lab in cognitive/perceptual experiments. Psychonomic bulletin & review. 2012;19(5):847–857. doi: 10.3758/s13423-012-0296-9. [DOI] [PubMed] [Google Scholar]
- 28.Gosling SD, Vazire S, Srivastava S, John OP. Should we trust web-based studies? A comparative analysis of six preconceptions about internet questionnaires. American Psychologist. 2004;59(2):93. doi: 10.1037/0003-066X.59.2.93. [DOI] [PubMed] [Google Scholar]
- 29.Miller PG, Sønderlund AL. Using the internet to research hidden populations of illicit drug users: a review. Addiction. 2010;105(9):1557–1567. doi: 10.1111/j.1360-0443.2010.02992.x. [DOI] [PubMed] [Google Scholar]
- 30.Luna Expedito JA, Gattás Vera L. Effectiveness of the Brazilian influenza vaccination policy, a systematic review. Revista do Instituto de Medicina Tropical de. São Paulo. 2010;52.4:175–181. doi: 10.1590/s0036-46652010000400002. [DOI] [PubMed] [Google Scholar]
- 31.Feng Luzhao, et al. Seasonal influenza vaccine supply and target vaccinated population in China, 2004–2009. Vaccine. 2010;28.41:6778–6782. doi: 10.1016/j.vaccine.2010.07.064. [DOI] [PubMed] [Google Scholar]
- 32.Mereckiene Jolita, et al. Differences in national influenza vaccination policies across the European Union, Norway and Iceland 2008-2009. 2010 doi: 10.2807/ese.15.44.19700-en. [DOI] [PubMed] [Google Scholar]
- 33.http://www.health.gov.il/english/topics/pregnancy/vaccination_of_infants/pages/default.aspx. Accessed July 31st 2014.
- 34.Iwasa Tsubasa, Koji Wada. Reasons for and against receiving influenza vaccination in a working age population in Japan: a national cross-sectional study. BMC public health. 2013;13.1:647. doi: 10.1186/1471-2458-13-647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Duque Jazmin, McMorrow Meredith L, Cohen Adam L. Influenza vaccines and influenza antiviral drugs in Africa: are they available and do guidelines for their use exist? BMC public health. 2014;14.1:41. doi: 10.1186/1471-2458-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.http://www.nhs.uk/Conditions/vaccinations/Pages/who-should-have-flu-vaccine.aspx. Accessed July 31st 2014.
- 37.http://www.cdc.gov/media/pressrel/2010/r100224.htm. Accessed July 31st 2014.


