Abstract
Aim:
To evaluate the effect of intravenous (IV) clonidine premedication for the bloodless surgical field in patients undergoing middle ear or nasal surgery comparing three different doses.
Subjects and Methods:
This prospective randomized, clinical trial was performed on 90 normotensive patients belonging to American Society of Anesthesiologists grade I/II, aged 18–60 years, of either sex, undergoing routine middle ear or nasal surgery. These patients were divided into three Groups A, B, and C with 30 patients in each according to the dose of IV clonidine used as premedicant that is 3, 4, and 5 µg/kg, respectively. The hypotensive period commenced 10 min after the start of surgery till the surgeon's request for no hypotension required any longer. The target mean blood pressure for producing bloodless surgical field was 60–70 mmHg. During the hypotensive period, the surgeons were asked to rate the bleeding severity score on a six-point scale from 0 (no bleeding) to 5 (severe bleeding).
Statistical Analysis Used:
ANOVA, Chi-square test, Z-test, standard deviation and P value.
Results:
IV clonidine premedication in a dose of 4 and 5 µg/kg reduces bleeding and provides a clear field for surgery. It also reduces the requirement of isoflurane, fentanyl, and metoprolol for controlled hypotension. However, clonidine 5 µg/kg was not more effective than clonidine 4 µg/kg in producing these effects rather was associated with some side effects.
Conclusion:
IV clonidine premedication in a dose of 4 µg/kg is safe and effective for producing a bloodless surgical field in the middle ear and nasal surgery.
Keywords: Bloodless surgical field, controlled hypotension, intravenous clonidine
INTRODUCTION
Middle ear and nasal surgery are a delicate and time-consuming procedure requiring a bloodless surgical field. To achieve these hypotensive techniques are widely used in anesthesia.[1] Clonidine, which is widely being accepted as anesthetic adjuvant acts by a central α2 adrenergic mechanism reducing sympathetic nervous system output. Besides its antihypertensive effect, it also diminishes requirements for inhaled anesthetics and enhances the effects of sedative, anxiolytic, and analgesic drugs,[2] decreases pressor response to laryngoscopy and intubation,[3] postoperative nausea, vomiting[4] and shivering.[5]
So, this study was undertaken to evaluate the effect of intravenous (IV) clonidine premedication for bloodless surgical field in patients undergoing middle ear or nasal surgery in three different doses.
SUBJECTS AND METHODS
After approval from the Institutional Ethical Committee, written informed consent was obtained from 90 normotensive patients (American Society of Anesthesiologists I/II), aged 18–60 years, of either sex, undergoing routine middle ear or nasal surgery. Patients with heart disease, porphyria, liver or kidney dysfunction, history of allergy, obesity (weight >80 kg), pregnant and lactating women were excluded from the study. Patients were assigned to three groups of 30 each. Group A received IV clonidine 3 µg/kg while Groups B and C received IV clonidine 4 µg/kg and 5 µg/kg respectively, 15 min prior to induction of anesthesia. Two separate IV access were secured. Intraoperative monitoring was done through electrocardiograph, pulse-oximeter for saturation (SpO2), noninvasive blood pressure monitor, and capnograph for measuring end-tidal carbondioxide (EtCO2) using Philips MP30 monitor. Patients were premedicated with IV ranitidine 50 mg, ondansetron 4 mg, midazolam 1 mg along with IV clonidine 3, 4, and 5 µg/kg according to group assigned. Following preoxygenation for 3 min, anesthesia was induced with IV fentanyl 2 µg/kg and thiopentone 5 mg/kg. Tracheal intubation was facilitated with suxamethonium 2 mg/kg. Anesthesia was maintained with O2 and N2O 50:50, isoflurane up to 1.5 Vol% to maintain EtCO2 between 30 and 40 mmHg. Atracurium 0.5 mg/kg bolus followed by 0.5 mg/kg/h infusion was administered to maintain neuromuscular blocked. Fluid replacement was based on 4.2.1 rule. To aid in achieving a bloodless surgical field, the patients were placed in a 15° flower position, and the surgeons were asked to inject 1% lidocaine with epinephrine 1:100,000 solution at the surgical site before tissue dissection.
The surgical time was defined as "time from the first infiltration of local anesthetic to the completion of mucosal or skin closure". The hypotensive period commenced 10 min after the start of surgery till the surgeon's request for no hypotension required any longer. The hemodynamic endpoint of anesthetic management was the maintenance of mean blood pressure (MBP) at 60–70 mmHg for producing bloodless surgical field. Direct control of MBP was attained with inspired concentration increments of isoflurane up to maximum of 1.5 Vol % as needed. After 10 min if it was unsuccessful, IV fentanyl 1 µg/kg was added. If both the drugs failed to provide the desirable hypotension, IV metoprolol 0.5 mg was given and repeated as required to a maximum dose of 5 mg. If MBP decreased to <50 mmHg, isoflurane was reduced by 0.25%, to a maximum of 0.5%. If hypotension still persisted, a fluid bolus of 250 ml was infused over 15 min and was repeated as necessary.
On completion of surgery, nitrous oxide and isoflurane were discontinued, and lungs were ventilated with 100% oxygen. Residual neuromuscular blockade was antagonized with neostigmine 2.5 mg and glycopyrrolate 0.5 mg and trachea were extubated following usual extubation criteria. Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), MBP, SpO2, and EtCO2 were recorded before premedication, baseline value, just after premedication, 5 min after premedication, 10 min after premedication, during laryngoscopy and intubation, 3 min after laryngoscopy and intubation, 5 min after laryngoscopy and intubation, every 5 min interval till first 30 min, thereafter at every 10 min interval throughout the surgery.
During the hypotensive period, the surgeons were asked every 15 min to rate the bleeding severity score according to the six-point scoring scale:[6]
0 - No bleeding
1 - Slight bleeding; no suctioning of blood required
2 - Slight bleeding; occasional suctioning required Surgical field not threatened
3 - Slight bleeding; frequent suctioning required Bleeding threatened surgical field a few seconds after suction was removed
4 - Moderate bleeding; frequent suctioning required Bleeding threatened surgical field directly after suction was removed,
-
5 - Severe bleeding; constant suctioning required Bleeding appeared faster than could be removed by suction
Surgical field severely threatened and surgery not possible.
Isoflurane, fentanyl and metoprolol requirement, duration of surgery and hypotensive period and side effects like bradycardia (defined as HR ≤50 bpm), inadvertent hypotension (defined as mean arterial pressure <50 mmHg) if any, were observed, recorded, and treated accordingly.
RESULTS
All the three groups were comparable with respect to age, weight, sex, type of surgeries, duration of surgery, and hypotensive period [Tables 1–3].
Table 1.
Patient characteristics (mean±SD)
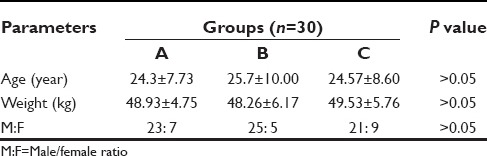
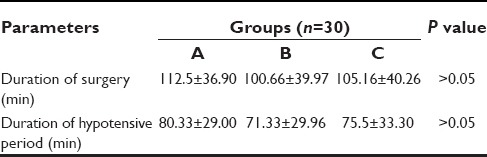
Table 3.
Total duration of surgery and hypotensive period in different groups (mean±SD)
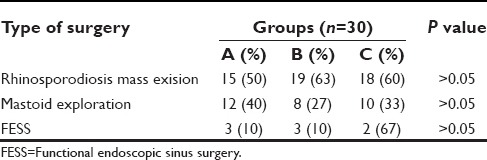
The most commonly performed surgery in all the three groups was rhinosporidiosis excision [Table 2].
Table 2.
Type of surgeries in different groups (number [%])
The groups were comparable as regards to baseline hemodynamic variables as well.
In inter-group comparison, significant fall in mean HR, SBP, DBP and MBP was observed in patients of Groups B and C as compared to Group A (P < 0.05).
The number of patients with bleeding severity score of 1 was significantly more in Groups B (37%) and C (40%) as compared to Group A (17%) [Table 4].
Table 4.
Bleeding severity score (number [%])
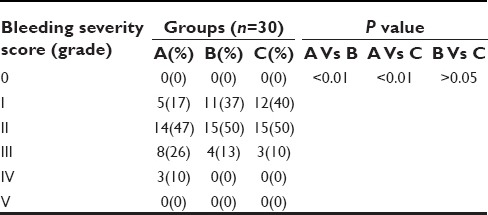
Number of patients with bleeding severity score of 3 and 4 were significantly lesser in Groups B (13%) and C (10%) as compared to Group A (36%) [Table 4].
In none of the patients of any group, bleeding severity score of 0 or 5 was observed [Table 4].
Mean isoflurane requirement was significantly more (P < 0.001) in Group A (1.003 ± 0.28 Vol%) as compared to Group B (0.69 ± 0.23 Vol%) and C (0.68 ± 0.18 Vol%) [Table 5].
Table 5.
Isoflurane, fentanyl and metoprolol requirement (mean±SD or n [%])
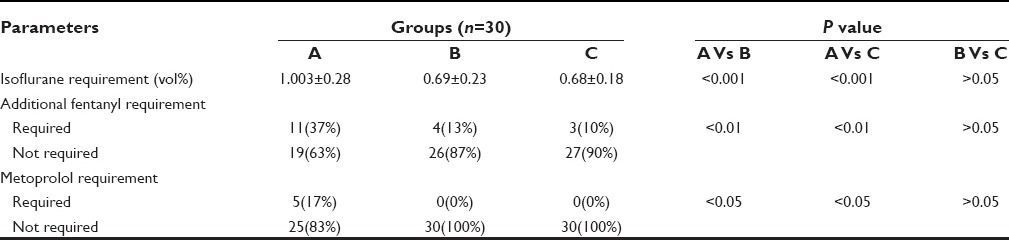
Additional dose of fentanyl was required by 37% patients of Group A as compared to 13% and 10% patients of Groups B and C respectively (P < 0.01) [Table 5].
Metoprolol was required by 17% patients of Group A, whereas none of the patients in Groups B and C required metoprolol (P < 0.05) [Table 5].
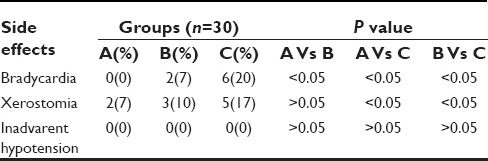
Incidence of side effects (transient bradycardia and xerostomia) was significantly more Group C as compared to Groups A and B. Inadvertent hypotension was not observed in any of the patient among the three groups [Table 6].
Table 6.
Side effects (number [%])
DISCUSSION
In our study, significant fall in mean HR, SBP, DBP, and MBP was observed in patients receiving clonidine 4 and 5 µg/kg as compared to 3 µg/kg. These findings were similar to the findings of Lee et al.,[1] Welfringer et al.,[7] Nishina et al.,[8] and Kerdawy et al.[9]
The decrease in HR after clonidine administration is due to the reduction of the sympathetic outflow along with the simultaneous increase of parasympathetic tone of central origin and influence of clonidine on neurons which receive baroreceptor afferents.[10]
Clonidine interacts with catecholaminergic neuronal system, which modulates tonic and phasic BP control and reduces the release of norepinephrine from nerve endings both centrally and peripherally causing a reduction in arterial pressure.[11]
The effects of clonidine on hemodynamic variables are dose-related and increasing the dose to more than 4 µg/kg dose not further enhance efficacy.[12]
Number of patients with bleeding severity score of 3 and 4 were significantly lesser in 4 µg/kg and 5 µg/kg group as compared to 3 µg/kg group. These findings were similar to the findings of Jabalameli et al.[6] and Welfringer et al.[7] It may be due to hemodynamic attenuation with clonidine, as diminished sympathetic outflow results from central α2 adrenoceptor stimulation thus reducing bleeding.
Isoflurane, fentanyl, and metoprolol requirement were significantly less in patients receiving clonidine 4 µg/kg and 5 µg/kg as compared to 3 µg/kg. These findings were similar to the findings of Jabalameli et al.,[6] El-Kerdawy et al.,[9] Howie et al.[13] and Hackmann et al.[14] This may be due to pharmacological properties of clonidine including analgesic and antihypertensive effects.
Transient bradycardia was significantly more in patients receiving clonidine 5 µg/kg as compared to other two groups. This finding was similar to the finding of Welfringer et al.[7]
CONCLUSION
IV clonidine 4 µg/kg and 5 µg/kg significantly reduce bleeding and provides a clear field for surgery. It also reduces the requirement of isoflurane, fentanyl, and metoprolol for controlled hypotension. However, clonidine 5 µg/kg was not more effective than clonidine 4 µg/kg in producing these effects rather was associated with some side effects.
Hence, we conclude, that the use of intravenous clonidine premedication in a dose of 4 µg/kg is safe and effective for producing a bloodless surgical field in middle ear and nasal surgery without any significant side effects.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lee J, Lovell AT, Parry MG, Glaisyer HR, Bromley LM. I.v. clonidine: Does it work as a hypotensive agent with inhalation anaesthesia? Br J Anaesth. 1999;82:639–40. doi: 10.1093/bja/82.4.639. [DOI] [PubMed] [Google Scholar]
- 2.Bloor BC, Flacke WE. Reduction in halothane anesthetic requirement by clonidine, an alpha-adrenergic agonist. Anesth Analg. 1982;61:741–5. [PubMed] [Google Scholar]
- 3.Mikawa K, Nishina K, Maekawa N, Takao Y, Asano M, Obara H. Attenuation of the catecholamine response to tracheal intubation with oral clonidine in children. Can J Anaesth. 1995;42:869–74. doi: 10.1007/BF03011033. [DOI] [PubMed] [Google Scholar]
- 4.Handa F, Fujii Y. The efficacy of oral clonidine premedication in the prevention of postoperative vomiting in children following strabismus surgery. Paediatr Anaesth. 2001;11:71–4. doi: 10.1046/j.1460-9592.2001.00615.x. [DOI] [PubMed] [Google Scholar]
- 5.Mao CC, Tsou MY, Chia YY, Chow LH, Chan KH, Lee TY. Pre-anesthetic oral clonidine is effective to prevent post-spinal shivering. Acta Anaesthesiol Sin. 1998;36:137–42. [PubMed] [Google Scholar]
- 6.Jabalameli M, Hashemi SM, Soltani HA, Hashemi SJ. Oral clonidine premedication decreases intraoperative bleeding in patients undergoing endoscopic sinus surgery. J Res Med Sci. 2005;I:25–30. [Google Scholar]
- 7.Welfringer P, Manel J, Garric J. Clonidine premedication and isoflurane anesthesia to reduce bleeding in otologic surgery. Ann Fr Anesth Reanim. 1992;11:125–31. doi: 10.1016/s0750-7658(05)80001-2. [DOI] [PubMed] [Google Scholar]
- 8.Nishina K, Mikawa K, Maekawa N, Obara H. The efficacy of clonidine for reducing perioperative haemodynamic changes and volatile anaesthetic requirements in children. Acta Anaesthesiol Scand. 1996;40:746–51. doi: 10.1111/j.1399-6576.1996.tb04522.x. [DOI] [PubMed] [Google Scholar]
- 9.El-Kerdawy HM, Zalingen EE, Bovill JG. The influence of the alpha2-adrenoceptor agonist, clonidine, on the EEG and on the MAC of isoflurane. Eur J Anaesthesiol. 2000;17:105–10. doi: 10.1046/j.1365-2346.2000.00610.x. [DOI] [PubMed] [Google Scholar]
- 10.Kumar A, Bose S, Bhattacharya A, Tandon OP, Kundra P. Oral clonidine premedication for elderly patients undergoing intraocular surgery. Acta Anaesthesiol Scand. 1992;36:159–64. doi: 10.1111/j.1399-6576.1992.tb03444.x. [DOI] [PubMed] [Google Scholar]
- 11.Raval DL, Mehta MK. Oral clonidine premedication for attenuation of haemodynamic response to laryngoscopy and intubation. Indian J Anaesth. 2002;46:124–9. [Google Scholar]
- 12.Kulka PJ, Tryba M, Zenz M. Dose-response effects of intravenous clonidine on stress response during induction of anesthesia in coronary artery bypass graft patients. Anesth Analg. 1995;80:263–8. doi: 10.1097/00000539-199502000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Howie MB, Hiestand DC, Jopling MW, Romanelli VA, Kelly WB, McSweeney TD. Effect of oral clonidine premedication on anesthetic requirement, hormonal response, hemodynamics, and recovery in coronary artery bypass graft surgery patients. J Clin Anesth. 1996;8:263–72. doi: 10.1016/0952-8180(96)00033-5. [DOI] [PubMed] [Google Scholar]
- 14.Hackmann T, Friesen M, Allen S, Precious DS. Clonidine facilitates controlled hypotension in adolescent children. Anesth Analg. 2003;96:976–81. doi: 10.1213/01.ANE.0000052713.72875.13. [DOI] [PubMed] [Google Scholar]


