Abstract
Infrared (IR) imaging is a collection of non-invasive imaging techniques that utilize the IR domain of the electromagnetic spectrum for tissue assessment. A subset of these techniques construct images using back-reflected light, while other techniques rely on detection of IR radiation emitted by the tissue as a result of its temperature. Modern IR detectors sense thermal emissions and produce a heat map of surface temperature distribution in tissues. Thus, the IR spectrum offers a variety of imaging applications particularly useful in clinical diagnostic area, ranging from high-resolution, depth-resolved visualization of tissue to temperature variation assessment. These techniques have been helpful in the diagnosis of many medical conditions including skin/breast cancer, arthritis, allergy, burns, and others. In this review, we discuss current roles of IR-imaging techniques for diagnostic applications in dermatology with an emphasis on skin cancer, allergies, blisters, burns and wounds.
Keywords: skin, skin cancer, burn wounds, infrared imaging, thermography, digital infrared thermal imaging (DITI), optical coherence tomography (OCT)
1. Introduction
Skin is the largest organ of the human body and serves as a barrier between the surrounding environment and the body's internal organs. With its multi-layered structure, skin protects the body from any potential attacks by pathogens in the surrounding atmosphere. Compromising integrity of this barrier or imbalance in the skin composition could lead to various skin injuries or conditions ranging from pruritus, rashes, scars to allergies and cancers. More importantly, several skin conditions are often symptoms of more serious systemic complications and must be examined promptly for early diagnosis [1-3].
The first step of diagnosis for such conditions usually involves visual inspection and non-invasive imaging. However, while there is normally a direct line-of-sight available for the stratum corneum of the skin, interrogating deeper layers requires more sophisticated techniques. Biopsy and microscopy may allow clinicians to examine the tissue and diagnose conditions, however, such techniques are invasive, time consuming and result in unnecessary scars. Ongoing advancements in photonics and in-depth understanding of light-tissue interactions have resulted in the development of several modern non-invasive imaging techniques. We discuss current trends and developments in infrared (IR) imaging techniques and their applications for diagnosis of dermal diseases and skin conditions.
2. Infrared imaging
Visible spectrum is a small portion of the electromagnetic radiation, to which the human eye is sensitive. However, longer wavelengths such as the IR spectrum are extremely useful in visualizing the structure as well as function of the deeper layers of the skin. While the IR spectrum covers wavelengths from 0.7 -1000 μm, only the initial narrow band of the spectrum is used for IR imaging. This spectrum is further divided into three sub-ranges such as near-IR (0.75 -2.5 μm), mid-IR (2.5 – 5 μm) and far-IR (5 -15 μm). The depth of penetration for imaging is largely dependent on the interaction of light with chromophores such as water and hemoglobin present in the skin. The light attenuation due to water in the near-IR range is minimal, thus offering greater depth of penetration; however, high absorption of light in the mid-IR range due to tissue water content results in significant light attenuation. Additionally, due to lack of tunable sources, fiber optic delivery systems and sensitive detectors, very few imaging techniques operate in the mid-IR range. Therefore, most of the biomedical IR imaging modalities utilize the near-IR spectrum for structural as well as functional imaging. Imaging in the far-IR range is predominantly emissive and focuses on recording thermal emissions of tissue.
Optical Coherence Tomography (OCT) is one of the imaging techniques that utilize near-IR radiation. The primary advantages of OCT are high speed, superior resolution and depth-resolved visualization. OCT is a modern imaging technique that uses non-ionizing near-IR radiation (800-1300 nm) for high-resolution (<15 μm), cross-sectional imaging of tissue. It is an optical analogue of ultrasound technology, which operates on the principle of low-coherence interferometry and depicts cross-sections of biological tissues based on the echo time delay of back-reflected light [4]. OCT is a label-free, contactless, non-invasive modality, which has been found to be extremely useful in scientific research and in clinical applications. Due to scattering nature of tissue, the depth of penetration of OCT is typically in range of 1-2 mm, which makes it suitable for structural evaluation of the skin. Various sub-types of OCT have been used for evaluation of skin cancers [5-7], burns scars and wounds [8, 9]. Various techniques such as optical clearing [10] or mechanical compression [11, 12] have been implemented to improve the penetration depth.
In addition to OCT, near-IR imaging has been used for detection of cutaneous melanin in pigmented skin disorders [13]. Melanin is one of the important endogenous chromophores, which plays a role in many benign and malignant skin disorders such as melanoma. Its autofluorescence under near-IR excitation has been utilized for detection of cutaneous melanin in the skin.
Far-IR imaging, also called thermal IR imaging, uses detectors such as bolometers to detect the infrared emissions from the objects under investigation. These detectors absorb the emissions from the object, which causes their temperature to change. This change in temperature causes change in electrical output as a result of some physical property of the sensor material such as temperature-dependent resistance. Thermal IR imaging has been used for non-contact evaluation of burn wound depths [14], sports-related injuries [15], or as an adjunctive screening method for breast cancer [16, 17].An overview of the IR spectrum used in imaging techniques and their dermatological applications are shown in Figure 1.
Figure 1.
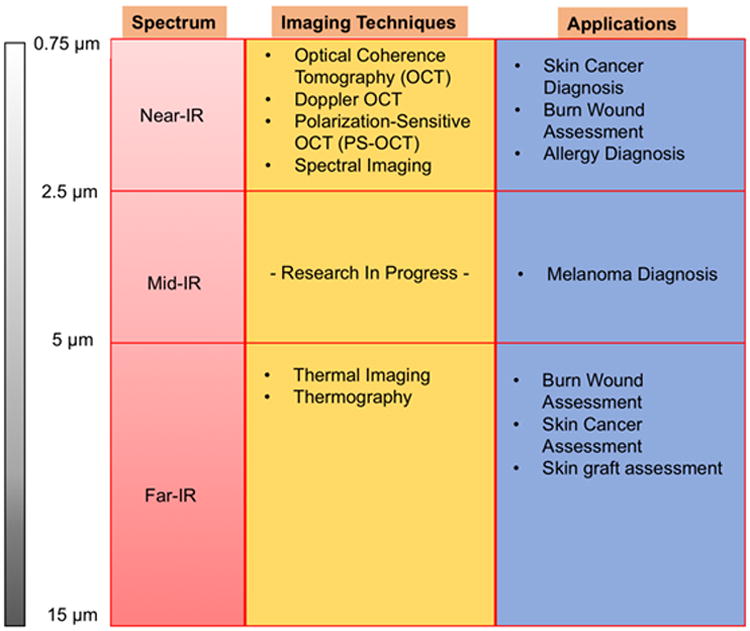
Summary of IR imaging techniques and their dermatological applications.
3. Applications of infrared imaging for diagnosis in various skin conditions
A) Skin cancer
Due to its ability to metastasize, the most serious form of skin cancer is considered to be melanoma [18]. Early detection is crucial to improve survival in patients with this disease. Non-invasive imaging systems that enable accurate quantitative detection of melanoma are important for reducing morbidity and mortality, as well as the cost of care associated with this disease [19].
Melanoma lesions have been observed to be warmer than the surrounding healthy tissue [20]. By using heating or cooling stimulation, it has been demonstrated that the average thermal signature of melanomas is different than that for the healthy skin [21, 22]. For skin cancer, preliminary assessment thermal imaging can be used as non-invasive, non-contact and safe technique. IR instrumentation advancements, dynamic IR imaging and modern digital signal processing algorithms enabled scientists to analyze spatio-temporal thermal behavior of the skin - an important leap in the cancer diagnosis field [23].
In the recent years, use of thermal imaging techniques for the detection and differentiation of skin cancer stages have gained exceptional interest. Most studies follow the protocol of basal study for patient preparation and acclimatization. The anatomic region of interest is exposed to a provocation test (usually cold stimulation), which induces an autonomic vasoconstriction reflex in normal structures. Therefore the thermal contrast due to the differences in the vasculature of the different skin regions can be observed. Melanoma typically possesses a faster temperature recovery than healthy, non-irradiated skin. Nevertheless, some other non-pathological structures are also detectable by IR imaging, (e.g. scars, vessels, arteriovenous anastomoses and injuries), thus requiring a multi-study comparison in order to discriminate the tumor signal [18, 19,23-25].
Recent statistical analyses reveal that thermal conductivity and the variation in thickness, blood perfusion as well as specific heat of certain skin layers lead to significant changes in the skin surface temperature, which can influence the detectability of dynamic IR imaging and frequency modulated thermal wave imaging during diagnosis of small volume melanoma [26, 27].
OCT for skin cancer detection
Basal cell carcinoma (BCC) is the most common subtype of cancer in the United States [28]. Suspicious lesions are normally biopsied for histopathological evaluation leaving behind unwanted scars and making the diagnosis lengthy and expensive. Recently, Polarization-Sensitive OCT (PS-OCT) - an extension of conventional OCT showed a strong potential for non-invasive assessment of skin lesions exhibiting possibility of BCC [7]. Collagen matrix in the healthy skin is birefringent – an optical property of material that results in two different refractive indices that depend on polarization of the incident light. Skin cancer results in disruption of collagen distribution and alignment, thus destroying the birefringence of the collagen matrix [29-31]. PS-OCT can detect the loss of skin birefringence [32, 33] and could enable identification of BCC lesions [7].
B) Allergy
Human skin color is produced by skin pigments that have spectral absorption properties in the visible range. The saturation levels of melanin and hemoglobin are the main contributors to the skin color and are important in dermatological diagnosis. Allergic dermatitis is characterized by allergic skin inflammation and can be induced by an allergic response to chemical substances brought on by environmental contamination [34]. Spectrophotometric assessments of allergic dermatitis can be performed in the near-IR wavelength range for the evaluation of water content [35]. Stamatas et al. proposed a visible and near-IR spectral imaging method for evaluating erythema and edema in which the values of apparent concentrations of oxyhemoglobin and water were calculated based on an algorithm that takes into account spectral contributions of deoxy-hemoglobin, melanin, and scattering [36]. Nishino et al. proposed a long-wavelength near-IR spectral imaging technique for the assessment of allergic dermatitis to detect and visualize intracutaneous differences caused by the activation mechanisms of different types of allergic dermatitis [35]. Recent studies show that IR thermography is a promising tool for screening the presence of digital dermatitis in dairy cows [37] suggesting that thermal and IR imaging is a multi-purpose method for all kinds of allergic mammal skin responses.
C) Blisters
People with various bullous disorders exhibit blister formations. Autoimmune blistering diseases cause impaired adhesion among epidermal cells [38]. Blisters and vesicles are easily diagnosed clinically, however, evaluating the exact pathology of the blister is where using optical imaging technologies may support clinical diagnosis [39]. Liquid nitrogen- and mechanically induced subepidermal blisters appeared as dark areas under the elevated, hypereflective/backscattering epidermis [39-41]. Explorative studies show that OCT can visualize blisters, epidermis and epidermo-dermal junctions in vivo, thus representing a range of relevant morphologies that match histopathology [38, 42].
D) Skin Burns and wounds
Thermography for skin burn assessment
It is important to evaluate the surface and the depth of skin burn, especially in the case of a severe burn as the thorough evaluation enables the appropriate choice of treatment. Clinical assessment is currently the most frequently applied method in burn depth evaluation. Unfortunately, the use of this method results in a high number of false diagnoses. For most burn surgeons, burn depth is better defined by the time to heal, which can be linked to the risk of developing hypertrophic scarring. Digital IR thermal imaging, also known as thermography, detects IR radiation, which is used to determine the emitting surface's temperature by producing a temperature-sensitive pattern on the imaged surface. Zhu et al, showed in 1990 that IR thermography was superior to subjective burn wound assessment [43]. Recent works by Medina-Preciado et al., showed significant difference in the thermal pattern of superficial skin and deep skin burn wounds, which are especially difficult to assess clinically [44].
Other noninvasive techniques such as laser doppler imaging (LDI) have also been used in the prediction of burn wound severity and result in a higher sensitivity (97%) and specificity (100%) when performed within three days of the burn injury [45]. However, even though LDI is accurate in assessing burn wounds, it is also more expensive and has a steeper learning curve than digital IR imaging [44]. Another advantage of digital IR thermography is its ability to image large skin surface areas, which can aid in identifying regions with different burn depths and estimate the size of the grafts needed for deep skin burns.
OCT for burn wounds assessment
Proliferation phase of wound healing involves formation of new blood vessels while the remodeling phase involves scar formation and collagen deposition at the wound site to increase the skin mechanical stability and strength. These stages could be monitored and assessed for quantitative evaluation of healing process using OCT in a non-contact manner. Gong et al [46] performed PS-OCT imaging of the burn scars and measured the attenuation coefficient of the scar tissue for its comparison with that of the surrounding healthy skin. The attenuation coefficient serves as a marker for the composition of scar or skin and therefore could be used for objective assessment of scars. Additionally, the same research group [47] also measured the magnitude of birefringence of scars using three-dimensional PS-OCT. Scar tissue typically lacks the birefringence a healthy skin tissue possesses owing to lack of alignment of the newly deposited collagen [33]. Restoration of such birefringence is a marker for better alignment of collagen and could be monitored using PS-OCT.
4. Limitations of Thermal and infrared imaging
Several biomedical imaging modalities operating in the IR spectrum have been developed in the recent years for diagnostic applications (Figure 1). IR imaging techniques offer high scanning speeds, superior imaging resolution and pose no health hazards as they use non-ionizing radiations. While the IR spectrum has been found to be beneficial for dermatological diagnostic applications, the primary limitation of the IR imaging is the finite depth of penetration, usually confined to 2-3 mm. For skin affected by hypertrophic scarring, sclerosis, or scabs resulting from wounds, this shallow range poses a challenge. Also, native fluorophores such as oxygenated hemoglobin, which absorbs IR, further affect the imaging range adversely.
Additionally, while the IR imaging techniques provide insight into the structural details of the skin; lack of cellular and molecular-level specificity limits the use of these techniques to preliminary diagnosis of skin diseases. Further tests are still necessary for in-depth, comprehensive evaluation of disease symptoms. Novel approaches, such as multimodality imaging are being actively investigated to overcome such limitations [48].
Thermography, or thermal imaging has been used as a diagnostic tool in veterinary medicine [49-51]; however it is a relatively new technique for clinical application. The accuracy of detection of temperature variations, spatial resolution and reliability is still unclear, making the modality adjunctive instead of a primary diagnostic tool.
5. Conclusion
We highlighted most of the prominent imaging techniques and modalities operating in the IR region for examination of various skin conditions and for diagnosis of dermal diseases. Due to advantages such as depth-resolved, faster imaging at superior resolutions, IR-based diagnostic techniques are being increasingly preferred over invasive procedures for preliminary evaluation. In case of skin cancer diagnosis, techniques such as OCT have shown significant promise for better assessment of skin lesions and for preventing unneeded biopsies of benign lesions. Far-IR imaging techniques such as thermography or digital IR thermal imaging have the potential to become valuable tools for non-contact, biopsy-free burn wound assessment.
Research in IR imaging techniques has gained significant momentum in the recent years. Development of IR-based novel modalities may result in faster and more reliable diagnosis and could lead to decreased healthcare costs.
Acknowledgments
The authors thank Dr. Alfred T. Lane of the Stanford Department of Dermatology for his support in this review. The work described was supported by the National Center for Research Resources and the National Center for Advocacy Translational Sciences, National Institutes of Health, through UL1 TR000093 (formerly UL1 RR025744) and SPARK, Spectrum - the Stanford Center for Clinical and Translational Research and Education; the Stanford NIH/NCCR Clinical Translational Science Award grant number TL1 RR025742, and author AD was supported by the Baltic-American Freedom Foundation.
Footnotes
Conflict of interest: The authors declare no conflict of interest.
References
- 1.Patel LM, Lambert PJ, Gagna CE, Maghari A, Lambert WC. Cutaneous signs of systemic disease. Clin Dermatol. 2011;29:511–522. doi: 10.1016/j.clindermatol.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 2.Cedeno-Laurent F, Obstfeld AE, Boni A, Lipoff JB. Lupus-like eruption as the presenting sign of acute myeloblastic leukemia. Lupus. 2015 doi: 10.1177/0961203315611497. [DOI] [PubMed] [Google Scholar]
- 3.Rizzo R, Mancini E, Santoro A. Skin and chronic kidney disease. G Ital Nefrol. 2014;31 [PubMed] [Google Scholar]
- 4.Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, et al. Optical coherence tomography. Science. 1991;254:1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strasswimmer J, Pierce MC, Park BH, Neel V, De Boer JF. Polarization-sensitive optical coherence tomography of invasive basal cell carcinoma. Journal of biomedical optics. 2004;9:292–298. doi: 10.1117/1.1644118. [DOI] [PubMed] [Google Scholar]
- 6.Gambichler T, Orlikov A, Vasa R, Moussa G, Hoffmann K, et al. In vivo optical coherence tomography of basal cell carcinoma. J Dermatol Sci. 2007;45:167–173. doi: 10.1016/j.jdermsci.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 7.Duan L, Marvdashti T, Lee A, Tang JY, Ellerbee AK. Automated identification of basal cell carcinoma by polarization-sensitive optical coherence tomography. Biomed Opt Express. 2014;5:3717–3729. doi: 10.1364/BOE.5.003717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gong P, Es'haghian S, Harms KA, Murray A, Rea S, et al. Optical coherence tomography for longitudinal monitoring of vasculature in scars treated with laser fractionation. Journal of Biophotonics. 2015 doi: 10.1002/jbio.201500157. [DOI] [PubMed] [Google Scholar]
- 9.Liew YM, Mclaughlin RA, Gong P, Wood FM, Sampson DD. In vivo assessment of human burn scars through automated quantification of vascularity using optical coherence tomography. Journal of biomedical optics. 2013;18:061213. doi: 10.1117/1.JBO.18.6.061213. [DOI] [PubMed] [Google Scholar]
- 10.Tuchin VV. Optical clearing of tissues and blood using the immersion method. Journal of Physics D: Applied Physics. 2005;38:2497. [Google Scholar]
- 11.Gurjarpadhye AA, Vogt WC, Liu Y, Rylander CG. Effect of Localized Mechanical Indentation on Skin Water Content Evaluated Using OCT. Int J Biomed Imaging. 2011;2011:817250. doi: 10.1155/2011/817250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rylander CG, Milner TE, Baranov SA, Nelson JS. Mechanical tissue optical clearing devices: enhancement of light penetration in ex vivo porcine skin and adipose tissue. Lasers Surg Med. 2008;40:688–694. doi: 10.1002/lsm.20718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han X, Lui H, Mclean DI, Zeng H. Near-infrared autofluorescence imaging of cutaneous melanins and human skin in vivo. Journal of biomedical optics. 2009;14:024017. doi: 10.1117/1.3103310. [DOI] [PubMed] [Google Scholar]
- 14.Medina-Preciado JD, Kolosovas-Machuca ES, Velez-Gomez E, Miranda-Altamirano A, Gonzalez FJ. Noninvasive determination of burn depth in children by digital infrared thermal imaging. Journal of biomedical optics. 2013;18:061204. doi: 10.1117/1.JBO.18.6.061204. [DOI] [PubMed] [Google Scholar]
- 15.Hildebrandt C, Raschner C, Ammer K. An overview of recent application of medical infrared thermography in sports medicine in Austria. Sensors (Basel) 2010;10:4700–4715. doi: 10.3390/s100504700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rassiwala M, Mathur P, Mathur R, Farid K, Shukla S, et al. Evaluation of digital infra-red thermal imaging as an adjunctive screening method for breast carcinoma: a pilot study. Int J Surg. 2014;12:1439–1443. doi: 10.1016/j.ijsu.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 17.Vreugdenburg TD, Willis CD, Mundy L, Hiller JE. A systematic review of elastography, electrical impedance scanning, and digital infrared thermography for breast cancer screening and diagnosis. Breast Cancer Res Treat. 2013;137:665–676. doi: 10.1007/s10549-012-2393-x. [DOI] [PubMed] [Google Scholar]
- 18.Bonmarin M, Le Gal FA. Lock-in thermal imaging for the early-stage detection of cutaneous melanoma: a feasibility study. Comput Biol Med. 2014;47:36–43. doi: 10.1016/j.compbiomed.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 19.Herman C. The role of dynamic infrared imaging in melanoma diagnosis. Expert Rev Dermatol. 2013;8:177–184. doi: 10.1586/edm.13.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brasfield RD, Laughlin JS, Sherman RS. Thermography in the Management of Cancer. Ann N Y Acad Sci. 1964;121:235–247. doi: 10.1111/j.1749-6632.1964.tb13699.x. [DOI] [PubMed] [Google Scholar]
- 21.Di Carlo A. Thermography and the possibilities for its applications in clinical and experimental dermatology. Clin Dermatol. 1995;13:329–336. doi: 10.1016/0738-081x(95)00073-o. [DOI] [PubMed] [Google Scholar]
- 22.Cetingul MP, Herman C. A heat transfer model of skin tissue for the detection of lesions: sensitivity analysis. Phys Med Biol. 2010;55:5933–5951. doi: 10.1088/0031-9155/55/19/020. [DOI] [PubMed] [Google Scholar]
- 23.Herman C, Cetingul MP. Quantitative visualization and detection of skin cancer using dynamic thermal imaging. J Vis Exp. 2011 doi: 10.3791/2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kateb B, Yamamoto V, Yu C, Grundfest W, Gruen JP. Infrared thermal imaging: a review of the literature and case report. NeuroImage. 2009;47(Suppl 2):T154–162. doi: 10.1016/j.neuroimage.2009.03.043. [DOI] [PubMed] [Google Scholar]
- 25.Santa Cruz GA, Bertotti J, Marin J, Gonzalez SJ, Gossio S, et al. Dynamic infrared imaging of cutaneous melanoma and normal skin in patients treated with BNCT. Appl Radiat Isot. 2009;67:S54–58. doi: 10.1016/j.apradiso.2009.03.093. [DOI] [PubMed] [Google Scholar]
- 26.Bhowmik A, Repaka R, Mulaveesala R, Mishra SC. Suitability of frequency modulated thermal wave imaging for skin cancer detection-A theoretical prediction. J Therm Biol. 2015;51:65–82. doi: 10.1016/j.jtherbio.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 27.Godoy SE, Ramirez DA, Myers SA, Von Winckel G, Krishna S, et al. Dynamic infrared imaging for skin cancer screening. Infrared Physics & Technology. 2015;70:147–152. [Google Scholar]
- 28.Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167–179. [PMC free article] [PubMed] [Google Scholar]
- 29.Everett MJ, Schoenenberger K, Colston BW, Jr, Da Silva LB. Birefringence characterization of biological tissue by use of optical coherence tomography. Opt Lett. 1998;23:228–230. doi: 10.1364/ol.23.000228. [DOI] [PubMed] [Google Scholar]
- 30.Jacques SL, Roman JR, Lee K. Imaging superficial tissues with polarized light. Lasers Surg Med. 2000;26:119–129. doi: 10.1002/(sici)1096-9101(2000)26:2<119::aid-lsm3>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 31.Jacques SL, Ramella-Roman JC, Lee K. Imaging skin pathology with polarized light. Journal of biomedical optics. 2002;7:329–340. doi: 10.1117/1.1484498. [DOI] [PubMed] [Google Scholar]
- 32.Yasuno Y, Makita S, Sutoh Y, Itoh M, Yatagai T. Birefringence imaging of human skin by polarization-sensitive spectral interferometric optical coherence tomography. Opt Lett. 2002;27:1803–1805. doi: 10.1364/ol.27.001803. [DOI] [PubMed] [Google Scholar]
- 33.De Boer J, Srinivas S, Malekafzali A, Chen Z, Nelson J. Imaging thermally damaged tissue by Polarization Sensitive Optical Coherence Tomography. Opt Express. 1998;3:212–218. doi: 10.1364/oe.3.000212. [DOI] [PubMed] [Google Scholar]
- 34.Bae MJ, Shin HS, Choi DW, Shon DH. Antiallergic effect of Trigonella foenum-graecum L. extracts on allergic skin inflammation induced by trimellitic anhydride in BALB/c mice. J Ethnopharmacol. 2012;144:514–522. doi: 10.1016/j.jep.2012.09.030. [DOI] [PubMed] [Google Scholar]
- 35.Nishino K, Fujiyama T, Hashizume H, Nakauchi S. Detection and visualization of intracutaneous allergic type-specific elements using long-wavelength near-infrared hyperspectral imaging. Skin Res Technol. 2013;19:e157–166. doi: 10.1111/j.1600-0846.2012.00622.x. [DOI] [PubMed] [Google Scholar]
- 36.Stamatas GN, Kollias N. Noninvasive quantitative documentation of cutaneous inflammation in vivo using spectral imaging - art. no. 60780P. Photonic Therapeutics and Diagnostics II. 2006;6078:P780–P780. [Google Scholar]
- 37.Alsaaod M, Syring C, Dietrich J, Doherr MG, Gujan T, et al. A field trial of infrared thermography as a non-invasive diagnostic tool for early detection of digital dermatitis in dairy cows. Veterinary Journal. 2014;199:281–285. doi: 10.1016/j.tvjl.2013.11.028. [DOI] [PubMed] [Google Scholar]
- 38.Mogensen M, Morsy HA, Nurnberg BM, Jemec GB. Optical coherence tomography imaging of bullous diseases. J Eur Acad Dermatol Venereol. 2008;22:1458–1464. doi: 10.1111/j.1468-3083.2008.02917.x. [DOI] [PubMed] [Google Scholar]
- 39.Welzel J, Lankenau E, Birngruber R, Engelhardt R. Optical coherence tomography of the human skin. J Am Acad Dermatol. 1997;37:958–963. doi: 10.1016/s0190-9622(97)70072-0. [DOI] [PubMed] [Google Scholar]
- 40.Choo IH, Lee DY, Oh JS, Lee JS, Lee DS, et al. Posterior cingulate cortex atrophy and regional cingulum disruption in mild cognitive impairment and Alzheimer's disease. Neurobiol Aging. 2010;31:772–779. doi: 10.1016/j.neurobiolaging.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 41.Welzel J, Reinhardt C, Lankenau E, Winter C, Wolff HH. Changes in function and morphology of normal human skin: evaluation using optical coherence tomography. Br J Dermatol. 2004;150:220–225. doi: 10.1111/j.1365-2133.2004.05810.x. [DOI] [PubMed] [Google Scholar]
- 42.Wozniak K, Kazama T, Kowalewski C. A practical technique for differentiation of subepidermal bullous diseases: localization of in vivo-bound IgG by laser scanning confocal microscopy. Arch Dermatol. 2003;139:1007–1011. doi: 10.1001/archderm.139.8.1007. [DOI] [PubMed] [Google Scholar]
- 43.Zhu WP, Xin XR. Study on the distribution pattern of skin temperature in normal Chinese and detection of the depth of early burn wound by infrared thermography. Ann N Y Acad Sci. 1999;888:300–313. doi: 10.1111/j.1749-6632.1999.tb07964.x. [DOI] [PubMed] [Google Scholar]
- 44.Medina-Preciado JD, Kolosovas-Machuca ES, Velez-Gomez E, Miranda-Altamirano A, Gonzalez FJ. Noninvasive determination of burn depth in children by digital infrared thermal imaging. J Biomed Opt. 2013;18:061204. doi: 10.1117/1.JBO.18.6.061204. [DOI] [PubMed] [Google Scholar]
- 45.Kim KH, Pierce MC, Maguluri G, Park BH, Yoon SJ, et al. In vivo imaging of human burn injuries with polarization-sensitive optical coherence tomography. J Biomed Opt. 2012;17:066012. doi: 10.1117/1.JBO.17.6.066012. [DOI] [PubMed] [Google Scholar]
- 46.Gong P, Mclaughlin RA, Liew YM, Munro PR, Wood FM, et al. Assessment of human burn scars with optical coherence tomography by imaging the attenuation coefficient of tissue after vascular masking. Journal of biomedical optics. 2014;19:21111. doi: 10.1117/1.JBO.19.2.021111. [DOI] [PubMed] [Google Scholar]
- 47.Gong P, Chin L, Es'haghian S, Liew YM, Wood FM, et al. Imaging of skin birefringence for human scar assessment using polarization-sensitive optical coherence tomography aided by vascular masking. Journal of biomedical optics. 2014;19:126014. doi: 10.1117/1.JBO.19.12.126014. [DOI] [PubMed] [Google Scholar]
- 48.Rossi AM, Sierra H, Rajadhyaksha M, Nehal K. Novel approaches to imaging basal cell carcinoma. Future Oncol. 2015 doi: 10.2217/fon.15.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rushton JO, Tichy A, Nell B. Introduction of the use of thermography and thermometry in the diagnosis of uveitis in horses: a pilot project. Vet Rec Open. 2015;2:e000089. doi: 10.1136/vetreco-2014-000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pavelski M, Silva DM, Leite NC, Junior DA, De Sousa RS, et al. Infrared Thermography in Dogs with Mammary Tumors and Healthy Dogs. J Vet Intern Med. 2015 doi: 10.1111/jvim.13597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Turner TA. Diagnostic thermography. Vet Clin North Am Equine Pract. 2001;17:95–113. doi: 10.1016/s0749-0739(17)30077-9. [DOI] [PubMed] [Google Scholar]


