Abstract
Context:
Tracheo-bronchial aspiration is the most invalidating condition which can happen to patients affected by dysphagia, especially when caused by central neurologic disorders; the associated pneumonia episodes represent the most frequent cause of death in these patients. Oro-pharyngo-esophageal scintigraphy (OPES) allows both functional imaging and semiquantitative evaluation of the subsequent phases of swallowing.
Case Report:
We evaluated by means of OPES a woman who had previously undergone high-dose external beam radiation therapy for a nasopharyngeal carcinoma, which determined tissue fibrosis and progressive dysphagia.
Conclusion:
In this patient with dysphagia, OPES was a simple, inexpensive, noninvasive, and reliable technique that allowed to show the presence of bolus aspiration and quantified tracheobronchial aspirate.
Keywords: Dysphagia, inhalation into tracheobronchial tree, management of aspiration, oro-pharyngo-esophageal scintigraphy
Introduction
Pathophysiologic studies of dysphagia have involved physicians from various specialties such as neurologists, gastroenterologists, otolaryngology, radiologists, and nuclear medicine physicians. Tracheobronchial aspiration is a common complication of dysphagia.
Tracheobronchial aspiration can be life-threatening by itself (because of suffocation) or as a consequence of an associated pneumonia ab ingestis. Aspiration is believed to be due to an alteration of oral and pharyngeal phases of swallow, related to neuromuscular incoordination and defective reflexes of cranial nerves IX, X, XI, and XII. Anatomic and pathophysiologic alterations of the upper aerodigestive tract such as fistulae, diverticulae, or changes resulting from surgery or radiation are other known causes of dysphagia.
Aspiration may cause various clinical signs as choking or coughing during swallowing, chronic cough, voice changes such as hoarseness, pneumonia, and bronchial asthma.[1,2]
There are few diagnostic examinations that allow to study a condition of dysphagia.
Videofluoroscopy is considered the gold standard method. It enables to evaluate alterations of anatomic structures and swallowing during dynamic acquisition; it can also allow to study all the phases of swallowing using liquid or solid foods. It is, particularly, indicated in cases of abnormalities of the mouth and esophagus and helps in detecting compensatory strategies in situations of pathological swallowing to reduce the entity of tracheobronchial aspiration.
Fibro-optic endoscopic examination to evaluate swallowing
It is a simple examination, well tolerated and inexpensive; moreover, it is useful to evaluate the patient enticed. It enables to provide anatomic and functional details of swallowing, particularly about the pharyngeal phase. It is able to precisely evaluate cough reflex. The main disadvantage of this examination is represented by the fact that it is not able to give detailed information about oral and esophageal phases.[3,4] Fibro-optic endoscopic examination to evaluate swallowing (FEES) enables to visualize the sites of bolus accumulation and possible related anatomical alterations. Furthermore, lesions of the pharyngeal tract can easily be biopsied during FEES for histopathologic analysis.
Oro-pharyngo-esophageal scintigraphy (OPES) provides accurate functional and semi-quantitative analyses of swallowing. Moreover, functional analysis gives information on multiple swallows, retention of the bolus in the oro-pharyngeal cavity, bolus fragmentation, gastro-esophageal reflux, tracheobronchial aspiration, and dysmotility of the esophageal tract.
Semi-quantitative analysis of swallowing includes measurement of transit times and retention indices by drawing regions of interest in the oral cavity, pharyngeal region and esophagus. Furthermore, tracheobronchial aspirate, when present, can easily be quantified.[5,6,7]
Case Presentation
We describe here the case of a 75-year-old woman who had undergone high-dose external bean radiotherapy (70 Gy) in 2007 for a nasopharingeal carcinoma; she, subsequently, developed a progressive dysphagia with cough and repeated episodes of pneumonia, associated with weakness of her upper right limb. The patient with a history of repeated inhalations documented by FEES was referred to our center to perform OPES, because of worsening of dysphagia and cough.
The scintigraphic study was carried out with the patient in orthostatic position, her face being turned by about 80° in front of a dual-head, large-field-of view gamma camera (Infinia Hawkeye, GE Healthcare), equipped with a low-energy, high-resolution parallel-hole collimator; the energy window was set at 140 KeV peak (±10%).
The patient was given a single 5 ml bolus of water labeled with 37 MBq of 99mTc-nanocolloids (Nanocoll, GE, Milan, Italy). Dynamic acquisition was recorded with 8 images/s (0.125 s/frame) for 1 min, using a 64 × 64 matrix and zoom 1. At the end of dynamic acquisition, a static image was acquired to search for tracheobronchial aspirate. The field of view of the gamma camera included the oral cavity down to the epigastric area. The functional semi-quantitative parameters analyzed were: Oral, pharyngeal and esophageal transit times, oro-pharyngeal and esophageal retention indices, the percentage of tracheo-bronchial aspirate.
OPES showed massive tracheo-bronchial inhalation, with retention of the radioactive bolus in both lungs; both oral and pharyngeal transit times were prolonged and the oro-pharyngeal retention index was increased. The static view of neck-chest demonstrated significant trachea-bronchial aspiration [Figure 1a]. In order to better characterize the massive aspiration, the study was completed with a neck-thorax single-photon emission computerized tomography/computerized tomography (SPECT/CT) acquisition, with the following parameters: 360° rotation (180° each head) in the step-and-shoot mode (60 frames, 20 s/frame, matrix of 128 × 128 and zoom factor 1.00). The CT study was performed with a 128 × 128 matrix, zoom 1, 25 mA and 140 KeV, acquiring 120 views (1/3°, 360°).
Figure 1.
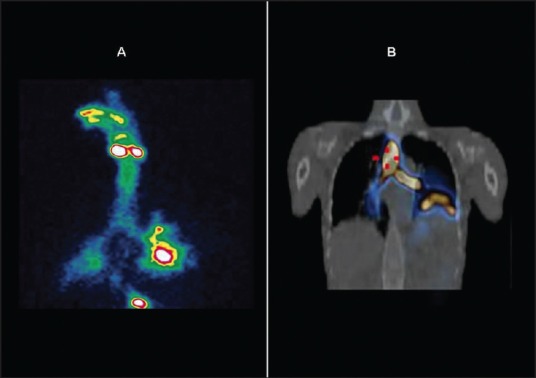
(Panel A) - Massive bilateral tracheobronchial aspiration, particularly on the left tracheo-bronchial tree, planar study. (Panel B) - Single-photon emission computerized tomography/computerized tomography study (coronal fused image). Note the upper elevation of left diaphragm due to pneumonitis ab ingestis and consequent atelectasia
The fused SPECT/CT images spatially outlined the pulmonary aspiration and showed the elevation of the left diaphragm as a consequence of inhalation [Figure 1b].
Based on clinical considerations and on results of FEES and OPES, the patient underwent positioning of a cuffed tracheostomy tube, with subsequent improvement of symptoms. A control OPES performed 7 days after such procedure showed absence of inhalation in the tracheo-bronchial tract, associated, however, with the presence of slightest aspiration in the right bronchus visualized only in the delayed acquisition after 60 min [Figure 2a].
Figure 2.
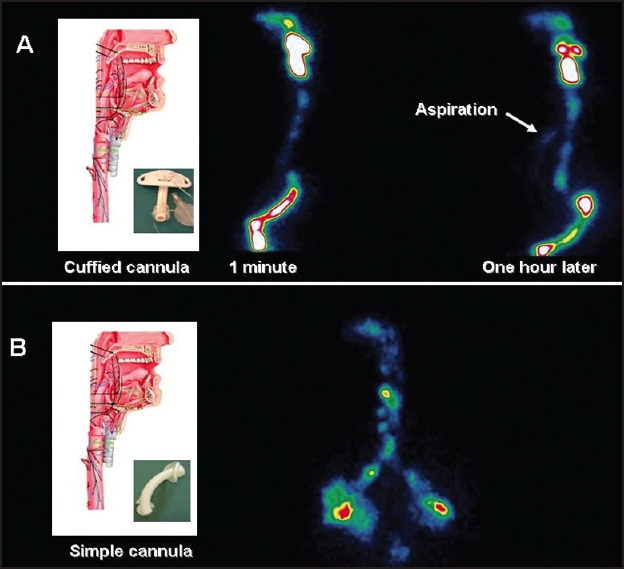
(Panel A) - Early (on the left) and delayed acquisition (on the right) with evidence of aspiration in the tracheo-bronchial tract. (Panel B) - Massive tracheobronchial aspiration after standard tracheostomy tube
The patient was then submitted to speech rehabilitation therapy for 1-month, with stimulation exercises of laringeal sensitivity and breathe-deglutition coordination.
At the end of rehabilitation therapy, the patient developed mucosal ulceration due to a cuffed tracheostomy tube and was then submitted to positioning a standard tracheostomy tube (not cuffed). OPES performed 1-week later showed again massive tracheobronchial aspiration [Figure 2b].
The impossibility of providing the patient with an adequate diet, associated with the high risk of aspiration, has brought to the choice of a total laryngectomy for functional purposes.
A new OPES performed subsequently did not detect any tracheobronchial aspiration [Figure 3].
Figure 3.
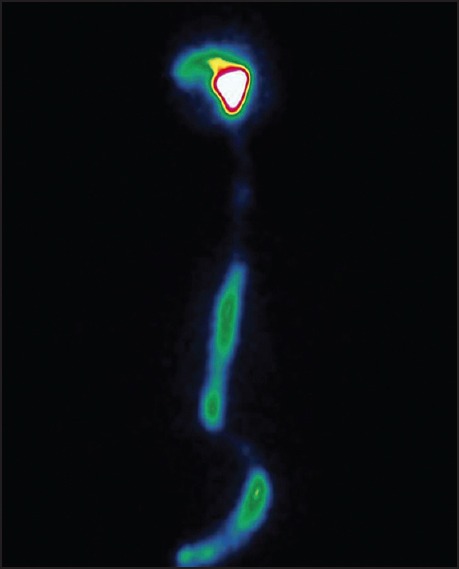
No evidence of tracheobronchial aspiration after functional laryngectomy. Retention of the bolus in the distal esophagus
Discussion
In postsurgical or neurological patients with suspected tracheobronchial aspiration, the occurrence of inhalation is established most reliably and comprehensively by conventional imaging techniques. Videofluoroscopy and FEES evaluation of swallowing are still the gold-standard for determining deglutition impairment. Is however well established that both techniques are inadequate for determining the extent of the respiratory tree penetrated and the amount of material aspirated, that constitute critical factors for the development of pneumonia. OPES it allows a much more accurate calculation of the semi-quantitative parameters in the different stages of swallowing, such as transit time and especially the retention indices of the bolus, and can detect the extensiveness of aspiration below the glottis, giving also possibility for a semi-quantitative measurement of aspirate. The use of SPECT/CT views can improve identification and characterization of the anatomic structures involved.
The clinical role of OPES is therefore to be recognized in its ability to identify swallowing abnormalities, and to provide not only diagnostic information but also evaluation of response to medical and/or surgical treatment, supplying important information for planning treatment and to adopt some different rehabilitative strategies in patients management.[8]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Palmer JB, Drennan JC, Baba M. Evaluation and treatment of swallowing impairments. Am Fam Physician. 2000;61:2 453–62. [PubMed] [Google Scholar]
- 2.Pikus L, Levine MS, Yang YX, Rubesin SE, Katzka DA, Laufer I, et al. Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. AJR Am J Roentgenol. 2003;180:1613–6. doi: 10.2214/ajr.180.6.1801613. [DOI] [PubMed] [Google Scholar]
- 3.Butler SG, Stuart A, Leng X, Rees C, Williamson J, Kritchevsky SB. Factors influencing aspiration during swallowing in healthy older adults. Laryngoscope. 2010;120:2147–52. doi: 10.1002/lary.21116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hey C, Pluschinski P, Stanschus S, Euler HA, Sader RA, Langmore S, et al. A documentation system to save time and ensure proper application of the fiberoptic endoscopic evaluation of swallowing (FEES®) Folia Phoniatr Logop. 2011;63:201–8. doi: 10.1159/000316314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mariani G, Boni G, Barreca M, Bellini M, Fattori B, AlSharif A, et al. Radionuclide gastroesophageal motor studies. J Nucl Med. 2004;45:1004–28. [PubMed] [Google Scholar]
- 6.Fattori B, Grosso M, Ursino F, Matteucci F, Mancini V, Rizza E, et al. Clinical applications of oro-pharyngo-oesophageal scintigraphy in the study of dysphagia. Acta Otorhinolaryngol Ital. 2007;27:192–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Shaw DW, Williams RB, Cook IJ, Wallace KL, Weltman MD, Collins PJ, et al. Oropharyngeal scintigraphy: A reliable technique for the quantitative evaluation of oral-pharyngeal swallowing. Dysphagia. 2004;19:36–42. doi: 10.1007/s00455-003-0033-7. [DOI] [PubMed] [Google Scholar]
- 8.Argon M, Secil Y, Duygun U, Aydogdu I, Kocacelebi K, Ozkilic H, et al. The value of scintigraphy in the evaluation of oropharyngeal dysphagia. Eur J Nucl Med Mol Imaging. 2004;31:94–8. doi: 10.1007/s00259-003-1276-0. [DOI] [PubMed] [Google Scholar]


