Sir,
Crimean-Congo haemorrhagic fever (CCHF) is a tick-borne viral disease with average mortality rate of 30-50 per cent1. In India, presence of CCHF was first time confirmed in Gujarat State during a nosocomial outbreak in 20112,3. Since then, numerous outbreaks and sporadic cases of this disease have been reported from different districts of Gujarat State4,5,6. Studies conducted at the National Institute of Virology (NIV), Pune, had reported the presence of anti-CCHF IgG antibodies in domestic animals from Sirohi district, Rajasthan State. However, in the last four years none of the referred human samples were found positive3,4,5,6.
On March 18, 2014, blood sample of a suspected CCHF case was referred to NIV, Pune, for aetiology confirmation. This suspected CCHF case was a 45 yr old male, shepherd by profession, residing at Veravilapur village, Sirohi district, Rajasthan. He was presented on March 14, 2014, with complains of abdominal discomfort since last six days and vomiting since one day along with history of intermittent fever since 15 days. He had moderate fever without chills and was associated with arthralgia, generalized body ache, constipation, decreased urine output, bleeding from nose, haematuria and bleeding per rectum. He was a known case of HBsAg reactivity, and was transferred from Rajasthan State to Civil hospital, Ahmadabad, Gujarat.
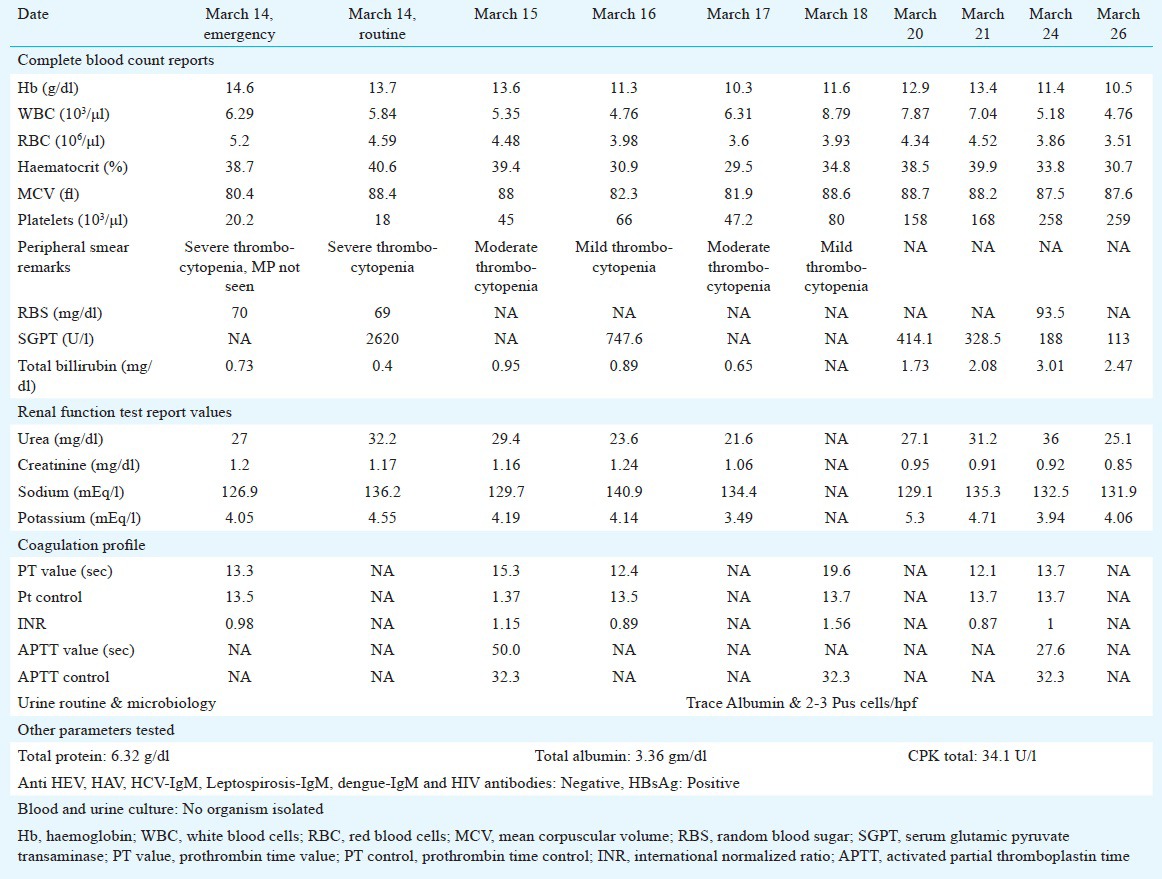
On admission, patient had thrombocytopenia (20,000/μl). Serum creatinine was 1.2 mg/dl, prothrombin time 15.3 sec, International Normalized Ratio (INR) 1.15, and activated partial thromboplastin time (APTT) was 50.0 sec (Table). There was impairment of liver function test in the form of markedly elevated liver enzymes of serum glutamic-pyruvic transaminase (SGPT: 2620 U/l) with normal serum total bilirubin (0.40 mg/dl) and normal renal function. Parameters of complete blood count were in the normal range (Table).
Table.
Day-wise clinical laboratory findings of Crimean-Congo haemorrhagic fever (CCHF) case in 2014
The differential diagnosis of CCHF at the pre-haemorrhagic stage is more difficult. As the disease progresses, clinical features become clearer and diagnosis becomes easier. The sample was differentially tested for some aetiological agents (hepatitis viruses, Leptospira and dengue viruses) which are endemic in the region and mimic the clinical illness of CCHF. Apart from HBsAg, patient was negative for viral markers (i.e. anti-HEV IgM, anti-HAV IgM, anti-HCV IgM). Anti-HIV antibodies, anti-Leptospira IgM and IgG antibodies, dengue IgM antibody, blood and urine culture were negative.
The patient did not have any recent travel history to Gujarat State; but had close contact with livestock. Whole blood of the patient was collected on March 15, 2014 (2nd day of admission) and March 19, 2014 (6th day of admission). On day 19, urine sample was also collected. The patient's serum and urine samples were processed for CCHF virus specific real-time RT-PCR5,7. Anti-CCHF IgM antibodies were tested in serum samples using commercial CCHF IgM ELISA Kit (Vector-Best, Novosibirsk, Russia). Real-time RT-PCR results were found positive for both serum samples collected on day 15th [threshold cycle (Ct) =27] and on 19th day (Ct=34)]. On 19th day urine sample showed Ct=38. Both serum samples (of 15th and 19th days) were positive for IgM antibodies against CCHF virus. Real-time reverse-transcription RT-PCR data showed high CCHF viral copy number. On 19th post illness day, the urine sample also showed low level of CCHF viral RNA.
As soon as the sample was laboratory confirmed as CCHF case, the patient was put in strict isolation. For treatment, oral ribavirin was administered on day 3 after admission on clinical suspicion at the dosage recommended by the World Health Organization8,9,10, along with the supportive and replacement therapy with blood products. The patient responded to the treatment and recovered completely, and was discharged on request on March 27, 2014 (14th day of admission).
Livestock trade and movements of domestic animals infested with infected ticks might be the reason in distribution of infected ticks to newer areas, and eventually spread of CCHFV. As CCHF mimics a wide range of common illnesses caused by different aetiological agents which are endemic in India, differential diagnosis should be done based on clinical biochemical, haematological, bacteriological and virological findings. These include Kyasanur forest disease, hepatitis, Neisseria meningitidis infection, leptospirosis, borreliosis, typhoid, rickettsiosis, dengue and malaria. However, malaria diagnosis can be excluded in cases of suspected viral haemorrhagic fever (VHF)11.
In conclusion, there is a need to initiate active serosurvey of CCHF among human population, and domestic animals in Rajasthan. This will be helpful in understanding the prevalence of this disease in Rajasthan State which eventually will alert the State health authorities.
Acknowledgment
The authors thank the Head of the department of Medicine, Dr A. N. Shah and Head of department of Microbiology, B.J. Medical College, Civil Hospital, Ahmadabad, Gujarat, for sharing the information and transporting specimen for investigation.
References
- 1.Ergonul O. Crimean-Congo haemorrhagic fever. Lancet Infect Dis. 2006;6:203–14. doi: 10.1016/S1473-3099(06)70435-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mourya DT, Yadav PD, Shete AM, Gurav YK, Raut CG, Jadi RS, et al. Detection, isolation and confirmation of Crimean-Congo hemorrhagic fever virus in human, ticks and animals in Ahmadabad, India, 2010-2011. PLoS Negl Trop Dis. 2012;6:e1653. doi: 10.1371/journal.pntd.0001653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yadav PD, Raut CG, Patil DY, Majumdar TD, Mourya DT. Crimean-Congo hemorrhagic fever: current scenario in India. Proc Natl Acad Sci India Sect [B] 2014;84:9–18. doi: 10.1007/s40011-013-0197-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoogstraal H. The epidemiology of tick-borne Crimean-Congo hemorrhagic fever in Asia, Europe, and Africa. J Med Entomol. 1979;15:307–417. doi: 10.1093/jmedent/15.4.307. [DOI] [PubMed] [Google Scholar]
- 5.Yadav PD, Raut CG, Mourya DT. Re-occurrence of Crimean-Congo haemorrhagic fever in Ahmedabad, Gujarat, India (2012): a fatal case report. Indian J Med Res. 2013;138:1027–8. [PMC free article] [PubMed] [Google Scholar]
- 6.Yadav PD, Gurav YK, Mistry M, Shete AM, Sarkale P, Deoshatwar AR, et al. Emergence of Crimean-Congo hemorrhagic fever in Amreli district of Gujarat State, India, June to July 2013. Int J Infect Dis. 2014;18:97–100. doi: 10.1016/j.ijid.2013.09.019. [DOI] [PubMed] [Google Scholar]
- 7.Drosten C, Gottig S, Schilling S, Asper M, Planning M. Rapid detection and quantification catuib of RNA of Ebola and Marburg viruses, Lassa virus, Crimean-Congo hemorrhagic fever virus, Rift Valley fever virus, dengue virus, and yellow fever virus by real-time reverse transcription-PCR. J Clin Microbiol. 2002;40:2223–30. doi: 10.1128/JCM.40.7.2323-2330.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. [accessed on March 18, 2014]. Available from: http://www.who.int/mediacentre/factsheets/fs208/en .
- 9.Bodur H, Erbay A, Akinci E, Onguru P, Bayazit N, Eren SS, et al. Effect of oral ribavirin treatment on the viral load and disease progression in Crimean-Congo hemorrhagic fever. Int J Infect Dis. 2011;15:e44–7. doi: 10.1016/j.ijid.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Mardani M, Jahromi MK, Naieni KH, Zeinali M. The efficacy of oral ribavirin in the treatment of Crimean-Congo hemorrhagic fever in Iran. Clin Infect Dis. 2003;36:1613–8. doi: 10.1086/375058. [DOI] [PubMed] [Google Scholar]
- 11.Zeller H. Laboratory diagnosis of Crimean-Congo hemorrhagic fever. In: Ergonul O, Whitehouse CA, editors. Crimean-Congo hemorrhagic fever: a global perspective. Amsterdam: Springer; 2007. pp. 233–43. [Google Scholar]


