Abstract
Background: Co-morbidities in adulthood is a significant problem and is associated with obesity during adolescent.
Methods: This 3-months randomised controlled trial was aimed at determining the effectiveness of having internet-based intervention (obeseGO!) toward obesity among adolescents in Kuala Lumpur. Forty seven students were assigned randomly to the obeseGO! (intervention) group for internet-based intervention i.e., information on healthy lifestyle and diet were provided via the internet. Fifty students were assigned to the control group, where pamphlets containing health education were provided to these students. The measurement of body mass index (BMI), waist circumference, and the body fat percentage was taken at baseline and after 12 weeks of intervention.
Results: The multivariate analysis of variance (MANOVA) analysis found that obeseGO! had a small effect in reducing BMI, waist circumference and body fat percentage.
Conclusion: The internet-based obesity intervention program may be an effective medium for promoting healthy diet and physical activity among the obese adolescents.
Keywords: adolescent, internet, internet, obesity, body mass index, clinical trial
Introduction
Overweight and obesity are now on the rise, especially in developing counties. This can lead to increased burden of health care and poor quality of life. The main reasons behind the rise in these health problems include increasing consumption of fast foods, convenient or ready-to-eat meals, soft drinks, junk foods and sweets among adolescents and deviations in the physical patterns of adolescents - from playing at the field to playing computer games, watching television and surfing the internet.
WHO stated that the problem of adolescent obesity is global. The prevalence of obesity in Thai adolescents has increased from 12.2% to 15.6% in 2010 to 2012 (1), whereas, in China, the prevalence of obesity has reached 4.8%. However, in Indonesia, the prevalence of obesity was low at only 1.2% in 2001, whereas, in Cambodia, it was 2.6% in 2008 (2). The Malaysia National Health Morbidity Survey reported that the prevalence of obesity in Malaysia increased from 5.3% in 2006 to 6.1% in 2011 (3).
In this high-technology era, most of the adolescents have a sedentary lifestyle that includes watching television, playing internet games or surfing. Therefore, the best health promotion and education can be designed by using the ‘screen’ as a medium.
In 2005, the Ministry of Information and Communication in Malaysia reported that 94.8% of the adolescents use internet. Grayson (4) further stated that adolescents spend about 6 hours 21 minutes per day in media use, including watching TV and videos, listening to radio, tape and MP3, playing games, and surfing the Internet. Comparatively, they spend only about 43 minutes of the day in reading books, newspaper or magazines. Adolescents live in a media-saturated environment for 44.5 hours of media per week. Therefore, internet can be an effective medium for the adolescents to help them reduce their weight provided that they use the internet wisely.
In the US, the use of internet has increased among the adolescents, particularly among those aged 12–17 years, as roughly 73% of them reportedly surf internet. Around 92% of the adolescents surf the internet to read or send emails but only 26% use the internet to look for health information. A study by Borzekowskia and Rickert (5) found that 46% of the internet users used internet to gain health information. Many studies have shown that internet-based health promotion strategies can help adolescents to increase exercise and improve nutrition habits, leading to weight loss. A quasi-experimental study of 40–45 minutes of internet and video sessions for 1 month found that those who completed more than half of the sessions increased their exercises and decreased the percentage of dietary fats (6). Another study (7) showed that the internetbased lifestyle behaviour modification among adolescents found that body fat was significantly lower after six months of intervention. Weight loss can be achieved till adulthood with long-term weight loss and maintenance of healthier lifestyle (8).
Nowadays, adolescents spent most of their times, other than school hours, in front of their screens for playing games, watching movies and surfing the internet. Thus, internetbased interventions were suggested to help the adolescents establish a healthy dietary style and incorporate physical activities. The prevention of adolescent obesity needs an attitude of willingness by the adolescents for carrying out healthy behaviours. By providing health-related activities in websites, adolescents who spend most of their time in front of their screens can benefit from them and improve their knowledge and attitude toward a healthy lifestyle. Therefore, the aim of the research was to determine the effectiveness of obeseGO! intervention among the adolescents.
Methods
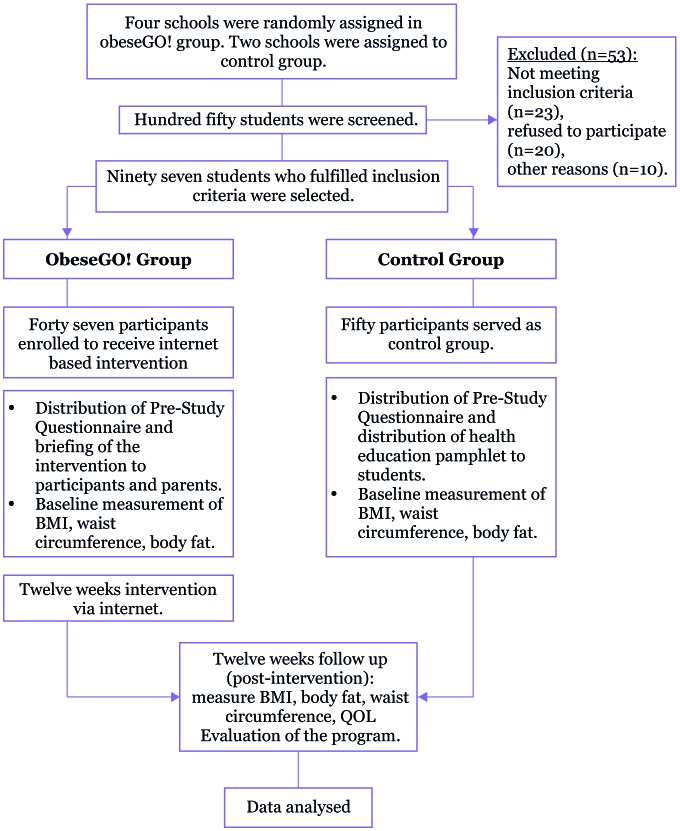
This school-based cluster randomised controlled trial was conducted within a 12-week period. A total of 196 secondary schools were chosen for the study. Of them, six schools were randomly selected using simple randomisation. Of the randomly selected schools, four schools were allocated to the intervention group whereas the other two schools served as control groups as shown in Figure 1.
Figure 1:
Study flowchart
Participants
From the six selected schools, only those students who satisfied the following criteria were selected for the study. The students should be of 16 years of age (adolescents), have a body mass index (BMI) of more than 25 kg/m2, have one guardian or parent willing to join the study, and have access to the Internet at home. However, students who have existing medical conditions or a weight loss of more than 2 kg in the last two months were excluded from the study. From the final selected students, 47 students were allocated to the obeseGO! group in which they received internet-based health education and 50 students served as the control group in which they received health education by pamphlets.
Sample size
A previous study in Malaysia (9) showed that the response within each subject group was normally distributed with a standard deviation of 2.5. Hence, the difference in the intervention and control means is 1.5, which indicates that the present study requires 45 intervention subjects and 45 control subjects so as to reject the null hypothesis. Thus, a sample of 45 subjects along with a 20% dropout rate was considered. A total sample of 108 subjects was selected with 54 subjects for each group. However, due to certain limitations while recruiting the adolescents, only 47 subjects were considered for the intervention group and 50 subjects were considered for the control group. Nevertheless, the study did get 100% of the sample size. Eight participants from the intervention group had withdrawn before the study began.
Study tools
Part A (Sociodemographic Data)
It was focused on gender and race only.
Part B (Eating Behaviour Questionnaire)
The Eating Behaviour Pattern questionnaire consisted of 35 items that were designed to reveal the eating behaviour of the students. All these items were grouped into six categories, namely, low-fat eating, snacking and convenience, emotional eating, planning, meal skipping, and lifestyle behaviour. The scores were obtained by adding all the responses to the items. An example of a question is, “I carefully watch the portion size of my foods.” The participants have the choice of selecting “strongly disagree”, “disagree”, “neutral”, “agree” or “strongly agree” options, which are represented by the Likert scale values of 1, 2, 3, 4 and 5, respectively. Then, the mean score for each domain was calculated in which the cutoff value of 4 and above indicated that the respondents had the particular eating behaviour. This questionnaire was validated with Cronbach’s alpha of 0.87 (10).
Part C (Physical Activity Questionnaire)
The physical activities of the participants were measured using the International Physical Activity Questionnaire (IPAQ). The scores were categorised into three groups, namely, low, moderate and high. This questionnaire was tested within the respective population with a reported kappa value of 0.73. Those participants who not meet the criteria for moderate and high categories were considered to be low/inactive. Moderate physical activity was considered if the respondents satisfied the followings: 1) three or more days of vigorous activity of at least 20 minutes per day; 2) 5 or more days of moderate-intensity activity or walking for at least 30 minutes per day; or 3) 5 or more days of any combination of walking, moderate-intensity or vigorous-intensity activities achieving a minimum of at least 600 metabolic equivalent of task (MET)-minutes/week. High physical activity was considered when the respondents had vigorous-intensity activity on at least 3 days and accumulated at least 1500 MET-minutes/week or spent 7 or more days on any combination of walking, moderate-intensity or vigorous-intensity activities achieving a minimum of at least 3000 MET-minutes/week (11).
Part D (Height and Weight Measurement)
The heights of the participants, i.e., from the heel to the highest point of the head, were measured using a portable stadiometer (SECA, United Kingdom) with an accuracy of 1 mm. The participants were asked to take off their shoes during the measurement. The weight was measured using a calibrated weighing scale to the nearest 0.1 kg. They were advised to wear light clothing during the measurement so as to reduce errors. The weights and heights were measured by a trained person. Then the BMI for each participant was calculated. All the measurements were taken twice, one during the first visit as a baseline data and one after 12 weeks of interventions.
Part E (Waist Circumference Measurement)
The waist circumference of each participant was measured using a flexible tape to the nearest 0.1 mm. The point of measurement, i.e., above the hip bone, was fixed for all respondents. The tape was then placed around the waist of the respondents. During the measurement, the respondents were advised to relax the stomach by breathing out gently and not to suck in the tummy. The tape was placed properly without compressing the skin and kept parallel to the floor. The measurement was taken around the waistline at the end of normal expiration. As with the measurements of weight, height and body fat, the waist circumference measurement was also repeated at the end of the interventions.
Part F (Body Fat Measurement)
The body fat of the participants was measured using the body fat analyser during their first visit for baseline data. The Krada body fat analyser (Omron, United Kingdom) is a novel device for estimating body fat based on the principles of bioelectrical impedance. It was repeated at the end of the intervention to see the difference in measurements. The measurement was expressed in percentages.
Intervention protocol
The intervention groups received the obeseGO! intervention. The participants and the parents who are randomly chosen to enroll in this intervention group were provided with the ObeseGO! website address (www.obesego.com). The website consists of information on healthy lifestyle, diet, and ways to overcome obesity. The contents of the website were developed by a panel expert consisting of a psychologist, public health specialist, two dietitians, and a nurse. Then a simple survey was conducted among 15 adolescents to know the level of interactive message given to them.
All respondents in the obeseGO! group were signed up as a member in the website. They were notified with any updates and information. Interactive sessions were conducted in the chat toolbar in the website. Any negative comment was not approved by the admin. Table 1 summarises the topics and discussion held in the website. The respondents were advised to weigh themselves at home and calculate their BMI every two weeks or as required by using the BMI calculator provided in the website. By self-monitoring their BMI, the respondents can be aware and observe their weight reduction. This interactive and informative website boosted the awareness among the respondents for being healthy and cutting down their weights.
Table 1:
Topics on the obeseGO! website
| Week | obeseGO! | Topics |
|---|---|---|
| 1 | Introduction | • What is obesity? |
| • Know your BMI. | ||
| • What causes obesity? | ||
| 2 | Teen obesity | • Dare to take the challenge? |
| 3 | Easy tips on diet | • Eating healthy, three meals each day, breakfast is important, lunch and dinner |
| 4 | Preventing obesity by MIND | • Positive mind |
| • Sharing on experience | ||
| 5 | What is important for our body? | • The importance of hydration |
| • Why should take fiber? | ||
| 6 | Eating healthy | • Suggestion of healthy menu |
| 7 | Active habits | • Making physical activity a habit, lead the way by example, not just any activity will do. |
| • Tai chi | ||
| • Video on Senamrobik 1 murid 1 sukan | ||
| 8 | Screen time | • TV, video games and computers (pro and cons) |
| • How to benefit screen time | ||
| 9 | Tips on prevention obesity | • Proper ways on planning a good diet |
| • How does it work | ||
| 10 | Fast food | • Why we should limit intake of fast food |
| • What is the effect of taking too much fast food | ||
| 11 | Feeling good about yourself | • Body image |
| • Media message | ||
| 12 | Taking care of your body depends on your mind | • Positive attitudes, success, tips and tricks |
Control group
The control group was provided with printed reading materials on the same information as in the obeseGO! website. The pamphlets were given after the measurement of the baseline data.
Data analysis
Data were entered, cleaned and analysed using SPSS (version 20). The frequency, percentage, mean and standard deviation were reported. Then, the paired t-test was run to see the effect of the intervention within both the groups. The independent t-test and one-way analysis of variance (ANOVA) were run to compare between the groups. Since no difference was observed between the groups as shown in Table 2, only multivariate ANOVA (MANOVA) was used to see the effectiveness of the intervention with three outcomes of the body composition profile. Interaction and multicollinearity were checked. All the involved hypotheses were two-sided tests and significant at a p-value of 0.05.
Table 2:
Characteristic of respondents in obeseGO! group and control group at baseline
| obeseGO! | Control | χ2-value | p-value | |
|---|---|---|---|---|
| N=47 | N=50 | |||
| n (%) | n (%) | |||
| Gender | 0.46 | 0.499 | ||
| Male | 25 (46.8) | 30 (60.0) | ||
| Female | 22 (53.2) | 20 (40.0) | ||
| Race | 0.17 | 0.684 | ||
| Malay | 36 (76.6) | 40 (80.0) | ||
| Non-Malay | 11(23.4) | 10 (120.0) | ||
| Low-fat eating | 0.01 | 1.000 | ||
| Yes | 10 (21.3) | 11 (22.0) | ||
| No | 37 (78.7) | 39 (78.0) | ||
| Snacking and convenience | 4.44a | 0.051 | ||
| Yes | 4 (8.5) | 0 (0) | ||
| No | 43 (91.5) | 50 (100.0) | ||
| Emotional eating | 5.32 | 0.028 | ||
| Yes | 7 (14.9) | 1 (2.0) | ||
| No | 40 (85.1) | 49 (98.0) | ||
| Planning ahead | 0.06a | 1.000 | ||
| Yes | 4 (8.5) | 5 (10.0) | ||
| No | 43 (91.5) | 45 (90.0) | ||
| Meal skipping | 0.18 | 0.755 | ||
| Yes | 6 (12.8) | 5 (10.0) | ||
| No | 41 (87.2) | 45 (90.0) | ||
| Lifestyle behaviour | 3.12a | 0.105 | ||
| Yes | 5 (10.6) | 1 (2.0) | ||
| No | 42 (89.4) | 49 (98.0) | ||
| Mean (SD) | Mean (SD) | t-valueb | p-valueb | |
| Number of siblings | 3.74 (1.49) | 3.58 (1.40) | 0.56 | 0.577 |
| Parents’ monthly income (RM) | 3094.26 (1016.21) | 2716.00 (1552.39) | 1.41 | 0.162 |
| Mothers’ BMI (kg/m2) | 28.10 (4.39) | 28.06 (3.28) | 0.05 | 0.961 |
| Fathers’ BMI (kg/m2) | 27.28 (6.18) | 27.24 (2.44) | 0.05 | 0.963 |
| BMI (kg/m2) | 31.47 (4.16) | 31.58 (5.3) | –0.11 | 0.912 |
| Waist circumference (cm) | 97.46 (11.05) | 97.84 (12.28) | –0.16 | 0.874 |
| Body fat (%) | 29.65 (5.57) | 28.97 (5.53) | 0.59 | 0.554 |
| Physical activity (MET-minutes/week) | 1426.50 (5326.50)* | 1294.75 (9429.00)* | –0.69 | 0.486 |
*Median (range)
aFisher’s exact test
bIndependent sample t-test
Ethical consideration
Written informed consent was obtained from all parents/guardians. University Kebangsaan Malaysia’s (UKM) Research and Ethical Committee approval was obtained (FF 224-2013). As this study was conducted in a school, the approvals from the Ministry of Education and also from the school were obtained via web portal after getting the approval from UKM prior to the study. Data confidentiality was preserved.
Results
Overall, the majorities of the respondents were Malays (78.4%) and most (56.7%) of them were male. There was no significant difference between the socio-demographics data and anthropometric measurements between the intervention and control groups. Table 2 summarises the characteristics of the respondents in both groups.
Effects of interventions within both groups
The mean BMI, waist circumference and body fat in the obeseGO! group were significantly lower after the interventions. The respondents’ emotional functioning were also significantly increased after the intervention. Table 3 summarises the changes between both the groups.
Table 3:
Comparison of baseline and post intervention measurement within obeseGO! group and control group
| obeseGO! (n=47) | Control (n=50) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Post | Baseline | Post | |||||
| Mean (SD) | Mean (SD) | t-valuea | p-value | Mean (SD) | Mean (SD) | t-valuea | p-valuea | |
| BMI (kg/m2) | 31.47 (4.16) | 31.09 (4.05) | 3.89 | <0.001* | 31.58 (5.30) | 31.59 (5.31) | –0.43 | 0.669 |
| Waist circumference (cm) | 97.46 (11.05) | 96.28 (10.38) | 3.50 | 0.001* | 97.84 (12.28) | 97.85 (12.32) | –0.07 | 0.944 |
| Body fat (%) | 29.65 (5.57) | 29.18 (5.44) | 3.51 | 0.001* | 28.98 (5.53) | 29.0 (5.63) | –1.06 | 0.295 |
| Quality of life –Adolescents’ report (score) | ||||||||
| Physical functioning | 75.13 (15.40) | 76.99 (15.44) | –0.53 | 0.597 | 74.74 (16.80) | 78.64 (15.35) | –1.12 | 0.268 |
| Emotional functioning | 64.36 (17.93) | 72.45 (18.62) | –2.15 | 0.037* | 68.16 (18.59) | 68.88 (20.19) | –0.20 | 0.840 |
| Social functioning | 79.15 (13.96) | 78.51 (14.59) | 0.25 | 0.807 | 75.41 (17.19) | 80.20 (15.88) | –1.45 | 0.155 |
| School functioning | 62.87 (14.59) | 63.62 (14.01) | –0.31 | 0.759 | 63.16 (15.40) | 64.69 (14.98) | –0.57 | 0.572 |
| Psychosocial health | 68.79 (10.34) | 71.52 (12.01) | –1.38 | 0.175 | 68.91 (13.54) | 71.25 (12.53) | –0.96 | 0.341 |
| Quality of life – Parents’ report (score) | ||||||||
| Physical functioning | 71.41 (15.59) | 71.08 (17.51) | 0.10 | 0.920 | 65.13 (20.09) | 71.56 (16.73) | –1.88 | 0.066 |
| Emotional functioning | 62.45 (15.59) | 66.59 (14.89) | –2.14 | 0.038* | 61.40 (14.11) | 67.00 (16.57) | –2.37 | 0.022* |
| Social functioning | 75.64 (15.69) | 77.98 (12.58) | –1.25 | 0.218 | 72.90 (17.29) | 76.30 (13.16) | –1.19 | 0.242 |
| School functioning | 65.43 (11.55) | 65.21 (12.64) | 0.13 | 0.898 | 61.90 (12.16) | 65.20 (11.02) | –1.72 | 0.091 |
| Psychosocial health | 67.84 (10.62) | 69.92 (10.43) | –2.19 | 0.034 | 65.40 (11.05) | 69.50 (10.24) | –2.63 | 0.011* |
*Significant at 0.05 level
aPaired t-test
Effect of intervention towards reducing BMI, waist circumference and body fat percentage
There was no significant reduction in BMI, waist circumference, and the body fat percentage between the intervention and control groups (Table 4). The effect sizes of the reduction were too small (0.09, 0.11, and 0.09 for BMI, waist circumference and body fat percentage).
Table 4:
Comparison of BMI, waist circumference and body fat percentage between obeseGO! group and control group after 12 weeks intervention
| Group | n | Mean (SD) | Mean diff. (95% CI) | F stat.a (df) | p-value a | |
|---|---|---|---|---|---|---|
| BMI (kg/m2) | obeseGO! | 47 | 31.09 (4.05) | –0.49 (–2.41, 1.42) | 0.26 (1, 95) | 0.609 |
| Control | 50 | 31.59 (5.31) | ||||
| Waist circumference (cm) | obeseGO! | 47 | 92.28 (10.38) | –1.57 (–6.18, 3.03) | 0.46 (1, 95) | 0.500 |
| Control | 50 | 97.85 (12.32) | ||||
| Body fat (%) | obeseGO! | 47 | 29.18 (5.48) | 0.09 (–2.14, 2.33) | 0.01 (1, 95) | 0.933 |
| Control | 50 | 29.09 (5.51) |
aMANOVA analysis
Discussion
The obeseGO! intervention showed a small effect in controlling and reducing overweight and obesity compared to the health education via a pamphlet. As hypothesised, the respondents in the obeseGO! group had significantly reduced BMI, waist circumference and body fat percentage as compared to that in the control group. This suggests that the obeseGO! module provides effective health education to the adolescents. The module, which consisted of obesity information, diet information, interactive games, attractive video for exercise and other related information, created awareness among the respondents regarding practicing and living a healthier lifestyle. This interactive web-based module had a good impact on respondents who showed their commitment toward reducing their weight. Even though the intervention effect was small, it showed that technology played an important role in delivering the message compared to the routine pamphlets.
A study by Gow et al. (12) showed that the internet interventions with first-year college students resulted in lower BMI (F (3, 154) = 5.98, p < 0.05, partial eta squared = 0.10) compared to the group that received only indirect health education. Another randomised controlled trial (RCT) among adolescents in Chicago found that there was a significant reduction of BMI (p = 0.027, partial eta squared = 0.08) in the intervention group from baseline to post intervention (13). The findings suggested that an internet-delivered intervention yielded a modest reduction in weight status (13). Their effect size was similar to the present study, but their sample size was larger that may have contributed to significant results. Gow et al. (12) showed more mean difference compared with this study. This might be because their study period was 6 months. The present study was conducted for only 12 weeks; hence, an extended period of the study may have resulted in a bigger mean difference and perhaps a larger effect.
The RCT by Doyle et al. (13) proved that BMI z-scores were reduced in the intervention group as compared to control group (p = 0.027). However, there was no significant difference observed after the 4-months follow-up period. The interventions provided included internet-delivered program using a cognitive-behavioural approach, basic dietary education and guided behaviour modification for weight control. However, they suggested that the internetdelivered intervention produced a modest reduction in weight status. This is because the intervention group showed a greater increase in dietary restraint after the intervention and less improvement in body shape concern in the followup (p > 0.05). This is in agreement with our study, in which the body weight reduction was observed within three months. This might be because the respondents changed their diet toward a healthier option as suggested and recommended in the obeseGO! website. Therefore, prolongation and maintenance of the healthier diet can help in reducing the body weight.
This study was in parallel with the study done by Gow et al. (12), who reported an effect size of only 0.10. They measured the respondents’ BMI after having internet intervention on obesity. Doyle et al. (13) also reported an effect size of only 0.08. They also observed a reduction in the BMI, but it was comparatively less than the other studies. Another study by Chen et al. (14) used websites as a medium for delivering education on obesity and reported only 0.01 effect size. However, their BMI reduction was significantly lower. Thus, it should be noted that no study showed larger effect size. This might be associated with the small sample size considered in the studies. Larger sample size and effective intervention can result in a large reduction of body weight, yielding a larger effect size.
A study on the efficacy of web-based childhood obesity prevention program for Chinese-American adolescents did not find any reduction in BMI; this may be because of its short follow-up time of 2 months (14). They might have observed significant changes had the study been prolonged by maybe 3 to 6 months. However, this program seems to be feasible and effective in short term in terms of dietary habit.
An internet obesity prevention program for adolescents by Whittemore (15) compared the effectiveness of two school-based internet obesity prevention programs for adolescents on BMI, health behaviours and self-efficacy. This RCT involved students with a mean age of 15.31 years (0.69) with a baseline mean BMI of 24.69 (5.58). The 384 students studied showed no significant differences between groups on any outcomes and no change in BMI over 3 to 6 months of intervention. Comparatively, our study had lesser number of respondents. Thus, this might be one of the reasons why they observed no significant changes even after six months. When there are many respondents, it is difficult to cater to the maintenance of the measurements. The dropout rate was also higher that those contributed to non-significant results. However, there were significant improvements including healthier lifestyle. Therefore, accurate sample size should be considered in a study to prove the effectiveness of the intervention. This study provides support for the use of a school-based internet obesity prevention program to promote health behaviour in adolescents; hence, this can be a platform for the obesity control program.
Strengths and Limitations
This study has several strengths including no dropouts during the intervention period and until the end of the study. Since all the respondents were of the same age, this study also eliminated age as the confounder, indicating better results. Despite the small effect of this study, the obeseGO! can be a new platform for approaching the community, especially the adolescents, in fighting obesity provided that the website is well maintained and the sample size used is accurate. The consistency of health education and interactive sessions would be more beneficial and attractive to adolescents. The sample was recruited among the students in Kuala Lumpur, thus, it does not represent a whole population in Malaysia, especially those in the rural areas. On the other hand, the study period of 12 weeks is considered short. A better impact can be discovered if a longer study period is used.
Conclusion and Recommendation
The internet-based intervention program can be an effective medium in preventing and controlling obesity among adolescents. Such programs can help the adolescents who spend most of their time on screen by setting up reminders, resulting in a healthier lifestyle or at least a healthy eating behaviour. Future studies can measure the physical activity of the respondents by using a pedometer for having accurate results with larger sample size.
This study demonstrated that internet-based interventions have a small effect in preventing obesity among adolescents compare to the traditional methods. Further research is required to completely measure the effectiveness of promoting and maintaining a healthy lifestyle and preventing obesity. Meanwhile, this may suggest that the public health practitioner should collaborate with the Ministry of Education and the Malaysian Communication and Multimedia Commission for providing a strong internet-based intervention so that the negative impact of misuse of internet can be prevented. The finding of this study can aid the public health practitioner in planning and directing the primary intervention so as to combat obesity and reduce the prevalence of obesity in Malaysia. An effective health education is a major concern in preventing obesity and subsequent chronic diseases, particularly those who are at risk. On the other hand, this finding can also be a good platform for the public health practitioner to inculcate the elements for providing the best medium to deliver the health awareness.
It is suggested that the size of the sample can be increased to observe a larger effect size in BMI, waist circumference and body fat percentage. On the other hand, this study can also be conducted on other population including adults and rural population. It provides a solid base for more in-depth research, investigating the effectiveness of the internet-based intervention in preventing obesity. Longer-term outcome measures would have been useful to assess the sustainability of intervention effects on weight status, and longerterm follow-up should be included in future trials.
Acknowledgments
This work was supported by UKM’s Research and Ethical Committee (FF 224-2013).
Footnotes
Conflict of interest
None.
Funds
None.
Authors’ Contributions
Conception and design, and/or acquisition of data, and/or analysis and interpretation of data, drafting and revising the article: AMN, FICJ
References
- 1.WHO . Geneva (GE): WHO; 2012. Global strategy on diet, physical activity and health. [Google Scholar]
- 2.WHO . Geneva (GE): WHO; 2014. [cited 2014 Dec 1]. Global status report on noncommunicable disease. [Internet] Available from: http://www.who.int/global-coordination-mechanism/publications/global-status-report-ncds-2014-eng.pdf . [Google Scholar]
- 3.MOH . Putrajaya (MY): MOH; 2011. [cited 2014 Jan 3]. Third Malaysian health morbidity survey: Health facts. [Internet] Available from: http://www.crc.gov.my/nhsi/wp . [Google Scholar]
- 4.Grayson A. Burlington (VT): The University of Vermont; 2007. Reaching college students where they live: A descriptive study of undergraduate media usage in 2007. [Google Scholar]
- 5.Borzekowski DL, Rickert VI. Adolescents, the Internet, and health: Issues of access and content. J Appl Dev Psychol. 2001;22(1):49–59. [Google Scholar]
- 6.Siddique A. Vienna: Universitat Wien; 2010. Comparative analysis of computer-based nutrition education in primary schools of Lahore and Vienna. [PhD’s thesis] [Google Scholar]
- 7.Williamson DA, Walden HM, White MA, York-Crowe E, Newton RL, Alfonso A, et al. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obes. 2006;14:1231–1243. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- 8.Epstein DE, Sherwood A, Smith PJ, Craighead L, Caccia C, Lin P-H, et al. Determinants and consequences of adherence to the dietary approaches to stop hypertension diet in African-American and white adults with high blood pressure: Results from the ENCORE trial. J Acad Nutr Diet. 2012;112(11):1763–1773. doi: 10.1016/j.jand.2012.07.007. doi: 10.1016/j.jand.2012.07.007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wafa SW, Talib RA, Hamzaid NH, McColl JH, Rajikan R, Ng LO, et al. Randomized controlled trial of a good practice approach to treatment of childhood obesity in Malaysia: Malaysian Childhood Obesity Treatment Trial (MASCOT) Int J Pediatr Obes. 2011;6(2–2):e62–e69. doi: 10.3109/17477166.2011.566340. [DOI] [PubMed] [Google Scholar]
- 10.Schlundt DG, Hargreaves MK, Buchowski MS. The eating behavior patterns questionnaire predicts dietary fat intake in African American women. J Am Diet Assoc. 2003;103(3):338–345. doi: 10.1053/jada.2003.50049. [DOI] [PubMed] [Google Scholar]
- 11.Chu AH, Moy FM. Reliability and validity of the Malay International Physical Activity Questionnaire (IPAQ-M) among a Malay population in Malaysia. Asia-Pac J Public Health. 2015;27(2):2381–2389. doi: 10.1177/1010539512444120. doi: 10.1177/1010539512444120 . [DOI] [PubMed] [Google Scholar]
- 12.Gow RW, Trace SE, Mazzeo SE. Preventing weight gain in first year college students: An online intervention to prevent the “freshman fifteen”. EatBehav. 2010;11(1):33–39. doi: 10.1016/j.eatbeh.2009.08.005. doi: 10.1016/j.eatbeh.2009.08.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doyle AC, Goldschmidt A, Huang C, Winzelberg AJ, Taylor CB, Wilfley DE. Reduction of overweight and eating disorder symptoms via the internet in adolescents: A randomized controlled trial. J Adolesc Health. 2008;43(2):172–179. doi: 10.1016/j.jadohealth.2008.01.011. doi: 10.1016/j.jadohealth.2008.01.011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen J-L, Weiss S, Heyman MB, Lustig R. Risk factors for obesity and high blood pressure in Chinese American children: Maternal acculturation and children’s food choices. J Immigr Minor Health. 2011;13(2):268–275. doi: 10.1007/s10903-009-9288-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whittemore R, Jeon S, Grey M. An internet obesity prevention program for adolescents. J Adolesc Health. 2013;52(4):439–447. doi: 10.1016/j.jadohealth.2012.07.014. doi: 10.1016/j.jadohealth.2012.07.014 . [DOI] [PMC free article] [PubMed] [Google Scholar]