Abstract
Background:
Acute management of ischemic stroke involves thrombolysis within 4.5 h. For a successful outcome, early recognition of stroke, transportation to the hospital emergency department immediately after stroke, timely imaging, proper diagnosis, and thrombolysis within 4.5 h is of paramount importance.
Aim:
To analyze the obstacles for thrombolysis in acute stroke patients.
Materials and Methods:
The study was conducted in a tertiary care center in South India. A total of hundred consecutive patients of acute ischemic stroke who were not thrombolysed, but otherwise fulfilled the criteria for thrombolysis were evaluated prospectively for various factors that prevented thrombolysis. The constraints to thrombolysis were categorized into: i) Failure of patient to recognize stroke symptoms, ii) patient's awareness of thrombolysis as a treatment modality for stroke, iii) failure of patient's relative to recognize stroke, iv) failure of primary care physician to recognize stroke, v) transport delays, vi) lack of neuroimaging and thrombolysis facility, and vii) nonaffordability.
Results:
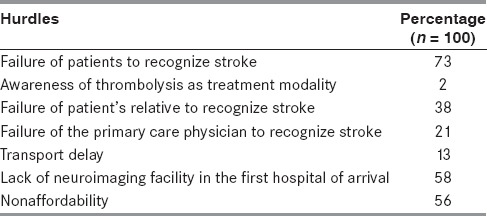
The biggest hurdle for early hospital presentation is failure of patients to recognize stroke (73%), followed by lack of neuroimaging facility (58%), nonaffordability (56%), failure of patient's relative to recognize stroke (38%), failure of the primary care physician to recognize stroke (21%), and transport problems (13%). Awareness of thrombolysis as a treatment modality for stroke was seen only in 2%.
Conclusion:
Considering the urgency of therapeutic measures in acute stroke, there is necessity and room for improvement to overcome various hurdles that prevent thrombolysis.
Keywords: Hurdles, hurdles in acute stroke management, ischemic stroke, stroke thrombolysis
Introduction
Acute management of stroke involves thrombolysis within 4.5 h. For a successful outcome, early recognition of stroke, transportation to the hospital emergency department immediately after stroke, timely imaging, proper diagnosis, and thrombolysis within 4.5 h is of paramount importance. The rate of thrombolysis all over the world is barely 1-3% due to many lapses in any of the above factors.
Stroke is one of the most common causes of death and long-term disability.[1] The developing world carries the highest burden of stroke mortality and stroke-related disability. The stroke in developing countries has grown to epidemic proportions. Two-thirds of global stroke occurs in low- and middle-income countries.[2] There has been limited progress in management of patients with stroke in developing countries and data on stroke care in these countries are sparse.[3] Guidelines are continuously developed and updated in the developed world, but their practicality for use in developing regions is unrealistic.[4] The use of intravenous thrombolytic therapy with recombinant tissue plasminogen activator (r-tPA) has been demonstrated to improve clinical outcome in selected patients with ischemic stroke.[5] Even with the extension of the time window from 3 h to the first 4.5 h after symptom onset; there is strong evidence of better outcome the earlier the treatment is started, as its efficacy is related to the time from symptom onset to treatment.[6] In 2009, 3.4-5.2% of acute ischemic stroke patients in the United States received thrombolytics.[7] In Scotland, 6% of stroke patients received thrombolysis in 2010.[8] Stroke thrombolysis is currently used in few developing countries like Brazil, Argentina, Senegal, Iran, Pakistan, China, Thailand, and India.[9] The number of stroke patients receiving r-tPA in the third world is extremely low. In a study from Pakistan, the rate of thrombolysis was 0.52-1.5%.[10]
Aim
To analyze the obstacles for thrombolysis in acute stroke patients in a tertiary care setting.
Materials and Methods
The study was conducted in a tertiary care center in South India with well-established emergency and neurological care. A total of 100 consecutive patients of acute ischemic stroke who were not thrombolysed but otherwise fulfilled the inclusion and exclusion criteria for thrombolysis[5] were evaluated prospectively for various factors that prevented thrombolysis. Period of study was from January 2014 to June 2014. Demographic data was collected followed by detailed neurological examination and neuroimaging. A questionnaire was provided to investigate the factors that deprived the patients of thrombolysis. The constraints to thrombolysis were categorized into:
Failure of patients to recognize stroke symptoms,
Awareness of thrombolysis as a treatment modality,
Failure of patient's relative to recognize stroke,
Failure of the primary care physician to recognize stroke,
Transport delay,
Lack of neuroimaging and thrombolysis facility in the first hospital of arrival, and
Nonaffordability. Descriptive statistics were used where ever necessary.
Results
A total of 100 consecutive acute ischemic stroke patients were evaluated for various factors that prevented thrombolysis; 69 patients were males and 31 females. Average age of patient in this study was 59.23 ± 10.92 years (mean ± standard deviation (SD)). Hypertension was the commonest risk factor for stroke (73%), followed by dyslipidemia (67%), diabetes mellitus (65%), smoking (31%), and atrial fibrillation (2%). According to Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification, 62 patients had large artery stroke, 35 patients had lacunar stroke, two patients had cardioembolic stroke, and one patient had stroke due to patent foramen ovale. Seventy-two patients had anterior circulation strokes and 28 had posterior circulation strokes. During the period of study, only four patients were thrombolysed with intravenous (IV) tPA (4%).
Time to reach the nearby hospital
Thirty patients arrived at the nearest primary healthcare hospital within 3 h, three patients arrived between 3 and 4.5 h, 15 patients reached between 4.5 and 6 h, 34 patients reached nearest primary healthcare hospital between 6 and 24 h, 16 patients reached between 24 and 72 h, and two patients reached beyond 72 h. Mean time to reach nearest primary healthcare hospital was 18.02 ± 26.98 h (mean ± SD).
Time to reach the tertiary care hospital
Seven patients arrived within 6 h after stroke onset at a tertiary care hospital where thrombolysis facility was available, 52 patients reached between 6 and 24 h, 15 patients reached between 24 and 48 h, 13 patients reached between 48 and 72 h, and 13 patients reached beyond 72 h. Median time to reach tertiary care hospital was 40.87 ± 45.17 h (mean ± SD).
Distance to hospital with stroke care facility
Sixty-one patients had to travel 50 km or less to reach tertiary care center, 20 patients had to travel 50-100 km. Eleven, six, and two patients had to navigate 100-150, 150-200, and more than 200 km, respectively to reach tertiary care hospital. Average distance to reach tertiary care center was 60.83 ± 66.96 km (mean ± SD).
Patient's recognition of stroke symptoms
Seventy-three patients had neglected initial stroke symptoms which included 51 males and 22 females. 73.9% of males (51/69) and 70.9% (22/31) females in this study had neglected initial stroke symptoms. Initial stroke symptoms were right or left hemiparesis in 51 patients, slurring of speech in 20 patients, and giddiness in 29 patients. Symptoms were neglected by 74.51% patients with right or left hemiparesis, 68.9% patients with giddiness, and 75% patients with slurring of speech.
Other hurdles
In 38 patients, initial stroke symptoms went unrecognized by accompanying relative. Awareness of thrombolysis as a treatment modality was present in only two patients. Primary care physician failed to recognize stroke in 21 patients, 13 patients had difficulty arranging for transportation, and 58 primary healthcare hospitals did not have facility for neuroimaging. Annual income was less than Rs. 50,000 in 13 patients, Rs. 50,000-1,00,000 in 30 patients, Rs. 100,000-150,000 in 16 patients, Rs. 150,000-2,00,000 in four patients, and more than Rs. 2,00,000 in 37 patients. Average income per annum was Rs 190,900 ± 200,822 (mean ± SD, range Rs. 10,000-60, 0000). When questioned, 56 patients would have refused thrombolysis citing financial constraint even if they had arrived within 3 h. Various hurdles for thrombolysis are shown in Table 1.
Table 1.
Hurdles in thrombolysis
Discussion
The results of our study suggest that prehospital delay in patients with acute stroke was considerable and that there are long intervals between the onset of symptoms and the initiation of seeking medical help. One of the most important prehospital barriers of thrombolysis therapy in the developing world is nonrecognition of stroke warning signs by patients at risk, families, the general public, and even health workers in some places.[11]
Failure of patients to recognize stroke
Seventy-three percent patients had neglected initial stroke symptoms in this study, by and large standing out as single most important factor for prehospital delay. There is poor recognition of stroke symptoms in developing countries.[12] The people at the highest risk have the lowest knowledge regarding vascular disease including limitations to ascertain mild and transient symptoms as stroke.[13] Several factors are related to decision delay, including failure to recognize stroke symptoms, not regarding symptoms as serious because of a lack of knowledge, a wait-and-see attitude, a hope that symptoms will resolve, and hesitation to contact emergency services.[14] The lack of awareness regarding stroke symptoms is believed to influence prehospital delay in stroke. Less is known about the proportion of the delay accounted for by the hesitation to seek medical assistance as a response to the symptoms.[15] Most stroke patients attending a university hospital in India were not aware of the importance of the time window in stroke management. Only one in 25 patients attending a stroke clinic and 27% of patients presenting to the stroke services in a tertiary care hospital in India were aware that they had suffered a stroke.[16] In the study conducted by Faiz et al., decision delay accounted for 62.3% of prehospital delay.[17] In study by Chang et al., decision delay accounted for 45% of the prehospital delay.[18]
Failure of patient's relative to recognize stroke
In 38 patients, initial stroke symptoms went unrecognized by accompanying attender. This is a significant factor contributing to prehospital delay. General public needs to be enlightened about stroke symptoms so that they act in a timely manner. This is especially true for attenders of elderly stroke patients where the patients may not have acuity as well as energy to respond appropriately after stroke.
Failure of the primary care physician to recognize stroke
Primary care physician failed to recognize stroke in 21 patients. Primary care physician may not be able to recognize subtle symptoms and signs of stroke. Most common mistake done is attributing symptoms to raised blood pressure which is a normal compensatory response of body to stroke. Primary care physician without knowledge of this compensatory response may accentuate the ongoing damage by further reducing blood pressure. Training programs is needed for primary care physicians so that they will be capable enough to recognize stroke early.
Transport problem
Thirteen patients had difficulty arranging for transportation. A dedicated ambulance service for stroke patients may circumvent this hurdle as evident from study by Mosley et al.[19] There is hardly any ambulance service, especially rural areas, in most of the developing countries.[9] Government and panchayats should act in concert to provide emergency ambulance services round the clock to mitigate prehospital delay due to transport problem. Ambulance drivers should be primed about the location of nearest thrombolysis center, thereby helping patients to get maximum benefit of thrombolysis. Because of the above mentioned factors, median time to reach tertiary care hospital in our study was 40.87 ± 45.17 h (mean ± SD). In a study from the United Kingdom and Ireland, median time between symptom onset and arrival to the hospital was 123 min for those calling the emergency medical services, compared with 432 min for patients who first saw their general practitioner.[20] In a study from Iran, 980/1,144 (85.6%) patients were initially excluded from the study because of late arrival.[21] In a study from Lebanon, only nine out of 87 patients received IV r-TPA and delayed presentation was the main barrier to thrombolysis.[22]
Lack of neuroimaging and thrombolysis facility in the first hospital of arrival
Fifty-eight primary healthcare hospitals did not have facility for neuroimaging in the current study. Infrastructure is a significant barrier against thrombolysis in developing world. A general overview shows that the quality and quantity of stroke care is largely patchy in low- and medium-developed countries with areas of excellence intermixed with areas of severe need depending upon location and socioeconomic status.[16] In China, 40% of 1,500 neurology departments have the infrastructure to facilitate thrombolysis therapy for a population of 1.3 billion.[23] In the African continent, the situation of stroke care is much worse; only northern African countries and South Africa have an appropriate number of CT and some MRI scanners.[24] It is unfortunate to note that many tertiary care hospitals in India are not geared up to provide thrombolysis facility.
Nonaffordability
In our study, 56 patients would have refused thrombolysis citing financial constraint. In India, thrombolysis facility is mainly available in private setups and cost of r-tPA is substantial. One of the main reasons of low utilization of thrombolytic therapy in developing countries is financial constraints because r-tPA in developing countries has high cost.[9] Government and NGOs should play an active role to make r-tPA available at a subsidized rate. A study from south India reported that 30% of stroke patients reached the hospital within 3 h post-event and 16% were eligible for thrombolysis therapy, but all of these eligible patients belonged to a lower socioeconomic group and could not afford the therapy due to its high cost.[25] Among 23 stroke patients admitted in a private hospital in northwest India who were eligible to intravenous thrombolysis, only five actually received the drug and the remaining patients were unable to afford the high cost of treatment.[25]
Knowledge regarding stroke among the public seems to be poor in the current study. There should be more focus on the “time is brain” paradigm to accentuate acute stroke as a condition of medical emergency in a similar manner as acute coronary syndrome (ACS). Prehospital delay is longer for stroke than for ACS.[26] Even though there is a pathophysiological overlap between the two conditions; one of the main reasons is that pain is a symptom in the majority of patients with ACS, whereas pain is rarely associated with stroke. Equally important is the difference in symptom distribution. Patients with stroke will potentially have significant deficits, such as aphasia, reduced consciousness, or cognitive impairment; preventing them from seeking help and thereby increasing the decision delay and the prehospital delay. Public education campaigns to increase awareness of stroke symptoms such as the face arm speech time (FAST)[27] campaign, have been initiated in several countries. Such campaigns are much needed in the developing countries. The limitation of the current study is that it is a single-center study with only 100 patients of stroke. In a country like India with almost 1 billion people belonging to diverse sociocultural, educational, and economic strata; multicenter studies involving larger number of stroke patients should be done for finding the various hurdles for stroke thrombolysis and to confirm whether our findings hold true in a larger group of stroke patients.
Conclusion
The biggest hurdles for early hospital presentation of acute stroke patients are failure of patients to recognize stroke, lack of neuroimaging facility, nonaffordability, failure of patient's relative to recognize stroke, failure of the primary care physician to recognize stroke, and transport problem.
The need of the hour is educational efforts focusing the public, the training of emergency physicians, and improving the infrastructure in district hospitals. Neuroimaging facilities should be improved and should be made affordable. Transport delays may be avoided by using dedicated ambulance services. r-TPA should be made available at subsidized rates to circumvent financial barrier of stroke thrombolysis. Finally, a national stroke prevention program with special emphasis on thrombolysis should be started.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: Heart disease and stroke statistics — 2010 update: A report from the American Heart Association. Circulation. 2010;121:948–54. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- 2.Feigi VL. Stroke epidemiology in the developing world. Lancet. 2005;365:2160–1. doi: 10.1016/S0140-6736(05)66755-4. [DOI] [PubMed] [Google Scholar]
- 3.Venketasubramanian N. “Stroke in developing countries,” in current review of cerebrovascular disease. In: Fisher M, Bogousslavsky J, editors. 2nd ed. Philadelphia: CM Publications; 2001. pp. 212–4. [Google Scholar]
- 4.Hill K, Lalor E. Clinical guidelines for stroke care: Why the fuss and is there opportunity for collaboration? Int J Stroke. 2008;3:173–4. doi: 10.1111/j.1747-4949.2008.00206.x. [DOI] [PubMed] [Google Scholar]
- 5.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 6.Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–29. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 7.Adeoye O, Hornung R, Khatri P, Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States: A doubling of treatment rates over the course of 5 years. Stroke. 2011;42:1952–5. doi: 10.1161/STROKEAHA.110.612358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.7 NHS National Services Scotland Scottish Stroke Care Audit 2011. National Report ISD Scotland. 2011:31. [Google Scholar]
- 9.Durai Pandian J, Padma V, Vijaya P, Sylaja PN, Murthy JM. Stroke and thrombolysis in developing countries. Int J Stroke. 2007;2:17–26. doi: 10.1111/j.1747-4949.2007.00089.x. [DOI] [PubMed] [Google Scholar]
- 10.Wasay M, Barohi H, Malik A, Yousuf A, Awan S, Kamal AK. Utilization and outcome of thrombolytic therapy for acute stroke in Pakistan. Neurol Sci. 2010;31:223–5. doi: 10.1007/s10072-009-0159-y. [DOI] [PubMed] [Google Scholar]
- 11.Yu RF, San Jose MC, Manzanilla BM, Oris MY, Gan R. Sources and reasons for delays in the care of acute stroke patients. J Neurol Sci. 2002;199:49–54. doi: 10.1016/s0022-510x(02)00103-x. [DOI] [PubMed] [Google Scholar]
- 12.Brainin M, Teuschl Y, Kalra L. Acute treatment and long-term management of stroke in developing countries. Lancet Neurol. 2007;6:553–61. doi: 10.1016/S1474-4422(07)70005-4. [DOI] [PubMed] [Google Scholar]
- 13.Ferris RM, Robertson RM, Fabunmi R, Mosca L. American Heart Association; American Stroke Association. American Heart Association and American Stroke Association national survey of stroke risk awareness among women. Circulation. 2005;111:1321–6. doi: 10.1161/01.CIR.0000157745.46344.A1. [DOI] [PubMed] [Google Scholar]
- 14.Jarrell B, Tadros A, Whiteman C, Crocco T, Davis SM. National healthline responses to a stroke scenario: Implications for early intervention. Stroke. 2007;38:2376–8. doi: 10.1161/STROKEAHA.107.487710. [DOI] [PubMed] [Google Scholar]
- 15.Teuschl Y, Brainin M. Stroke education: Discrepancies among factors influencing pre-hospital delay and stroke knowledge. Int J Stroke. 2010;5:187–208. doi: 10.1111/j.1747-4949.2010.00428.x. [DOI] [PubMed] [Google Scholar]
- 16.Pandian J, Kalra G, Jaison A, Deepak SS, Shamsher S, Singh Y, et al. Knowledge of stroke among stroke patients and their relatives in Northwest India. Neurol India. 2006;54:152–6. [PubMed] [Google Scholar]
- 17.Faiz KW, Sundseth A, Thommessen B, Rønning OM. Factors related to decision delay in acute stroke. J Stroke Cerebrovasc Dis. 2014;23:534–9. doi: 10.1016/j.jstrokecerebrovasdis.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Chang KC, Tseng MC, Tan TY. Pre-hospital delay after acute stroke in Kaohsiung, Taiwan. Stroke. 2004;35:700–4. doi: 10.1161/01.STR.0000117236.90827.17. [DOI] [PubMed] [Google Scholar]
- 19.Mosley I, Nicol M, Donnan G, Patrick I, Kerr F, Dewey H. The impact of ambulance practice on acute stroke care. Stroke. 2007;38:2765–70. doi: 10.1161/STROKEAHA.107.483446. [DOI] [PubMed] [Google Scholar]
- 20.Harraf F, Sharma AK, Brown MM, Lees KR, Vass RI, Kalra L. A multicentre observational study of presentation and early assessment of acute stroke. BMJ. 2002;325:17. doi: 10.1136/bmj.325.7354.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nikkhah K, Avan A, Shoeibi A, Azarpazhooh A, Ghandehari K, Foerch C, et al. Gaps and hurdles deter against following stroke guidelines for thrombolytic therapy in Iran: Exploring the problem. J Stroke Cerebrovasc Dis. 2015;24:408–15. doi: 10.1016/j.jstrokecerebrovasdis.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 22.El Sayed MJ, El Zahran T, Tamim H. Acute stroke care and thrombolytic therapy use in a tertiary care center in Lebanon. Emerg Med Int 2014. 2014 doi: 10.1155/2014/438737. 438737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wei G, Ji X, Bai H, Ding Y. Stroke research in China. Neurol Res. 2006;28:11–5. doi: 10.1179/016164106X91807. [DOI] [PubMed] [Google Scholar]
- 24.El Khamlichi A. African neurosurgery: Current situation, priorities, and needs. Neurosurgery. 2001;48:1344–7. doi: 10.1097/00006123-200106000-00034. [DOI] [PubMed] [Google Scholar]
- 25.Pandian JD, Sethi V, Dhillon R, Kaur R, Padala S, Chakravorty R, et al. Is intravenous thrombolysis feasible in a developing country? Cerebrovascular Dis. 2005;20:134–6. doi: 10.1159/000086804. [DOI] [PubMed] [Google Scholar]
- 26.Herlitz J, Wireklintsundstrom B, Bang A, Berglund A, Svensson L, Blomstrand C. Early identification and delay to treatment in myocardial infarction and stroke: Differences and similarities. Scand J Trauma Resusc Emerg Med. 2010;18:48. doi: 10.1186/1757-7241-18-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harbison J, Hossain O, Jenkinson D, Davis J, Louw SJ, Ford GA. Diagnostic accuracy of stroke referrals from primary care, emergency room physicians, and ambulance staff using the face arm speech test. Stroke. 2003;34:71–6. doi: 10.1161/01.str.0000044170.46643.5e. [DOI] [PubMed] [Google Scholar]


