Sir,
Some patients after ischemic stroke show significant functional recovery after a very short period of time, while others show minimal progress.[1,2] Although a lot of research has been undertaken on this subject, authors still disagree on the effect of different factors on rehabilitation outcome.[3,4,5] Therefore, the purpose of this study was to evaluate the impact of age, gender, cognitive status, depression, subtype of ischemic stroke based on the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification,[6] and co-morbidity on rehabilitation outcome of stroke patients.
This prospective study included 150 patients with ischemic stroke treated at the Rehabilitation Clinic in Novi Sad between June 2012 and May 2014. The following clinical data were collected: Type of stroke and impairment, the presence of cardiac co-morbidities (hypertension, atrial fibrillation, myocardial infarction and dilated cardiomyopathy), presence of diabetes mellitus, length of waiting (LOW; time from stroke onset to admission to our hospital) and length of stay (LOS).
A patient's performance in ADLs was evaluated by the Barthel Index (BI), ambulation ability by the Rivermead Mobility Index (RMI) and degree of disability by modified Rankin Scale (mRS). We defined successful rehabilitation as the value of BI at discharge ≥80 or the difference between BI value at discharge and admission ≥40. Cognitive condition was evaluated using Mini Mental State Evaluation (MMSE), and the presence of depression was registered by Hospital Anxiety and Depression Scale (HADS) after seven days of an admission to our institution.
In the study population (N = 150; mean age 63.6 ± 10.5; range 29-90), there were less women (N = 54 [36%]) than men (N = 96 [64%]). Breakdown of patients by the type of impairment and stroke etiology are shown in Table 1. The most prevalent co-morbidities in the study group were hypertension (N = 126 [84.0%]) and diabetes mellitus (N = 50 [33.3%]) [Figure 1].
Table 1.
Relation between rehabilitation outcome andgender, type of impairment and stroke subtype
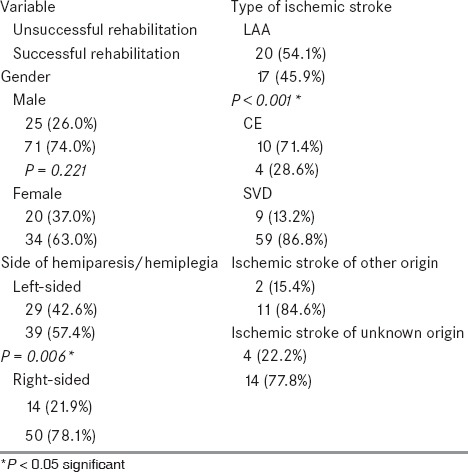
Figure 1.
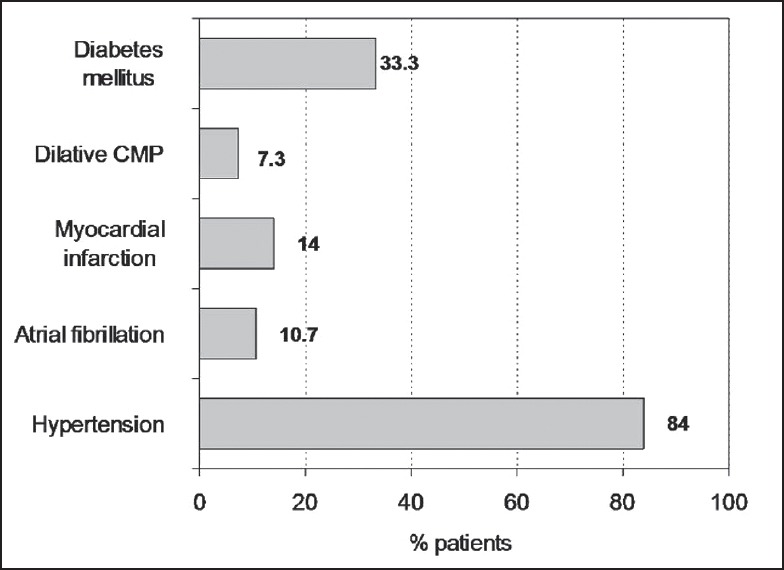
Comorbid disorders
According to the criteria we have established, 70% of the patients had successful rehabilitation (N = 105), and 30% had unsuccessful rehabilitation (N = 45). A statistically significant difference was found between the average values of BI, RMI and mRS at admission and discharge (P < 0.001) [Figure 2].
Figure 2.
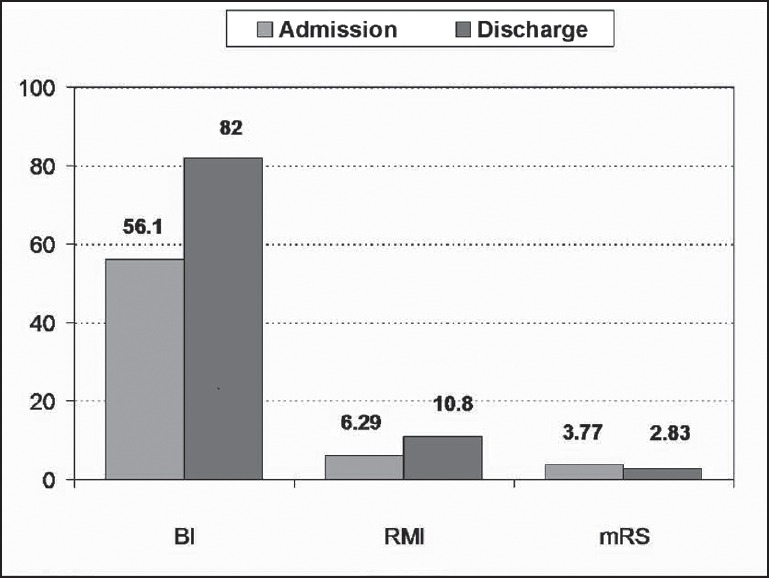
Average values of BI, RMI and mRS on admission and discharge
Statistically significant difference was found regarding the rehabilitation success in relation to the type of stroke based on the TOAST classification [Table 1]. Also, the presence of hypertension, atrial fibrillation, myocardial infarction and dilated cardiomyopathy had a statistically significant impact on the success of rehabilitation, but not diabetes mellitus (P = 0.571; 74.0% vs. 68.0%) [Table 2]. Relation between rehabilitation outcome and MMSE, HAD scale, RMI, BI and mRS on admission and discharge are shown in Table 3.
Table 2.
Relation between rehabilitation outcome and co-morbidity
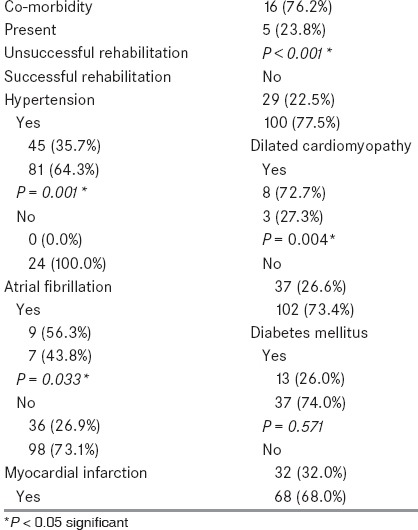
Table 3.
Relation between rehabilitation outcome and MMSE, HAD scale, RMI, BI and mRS on admission and discharge
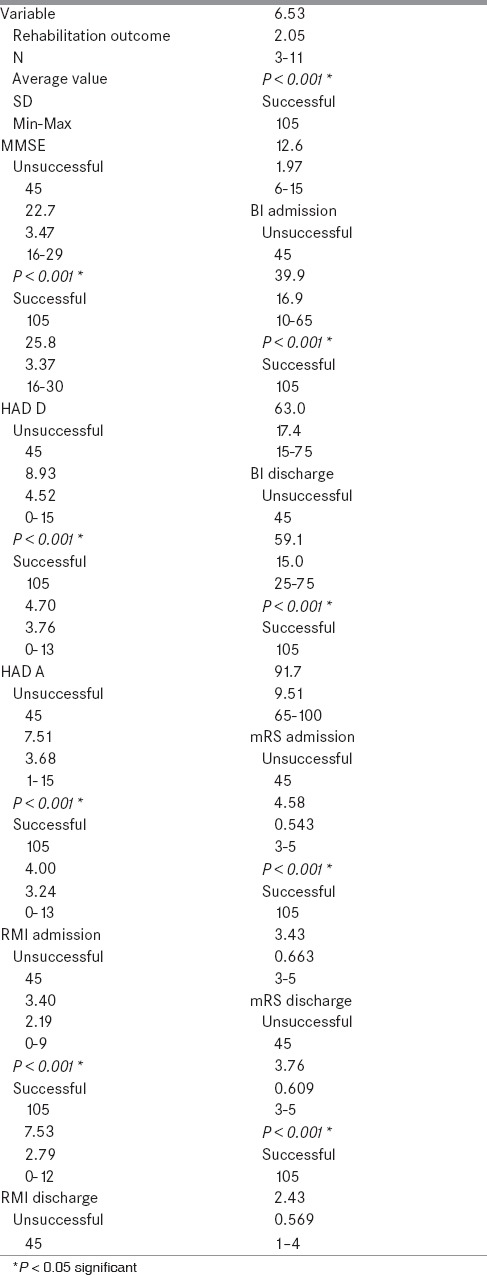
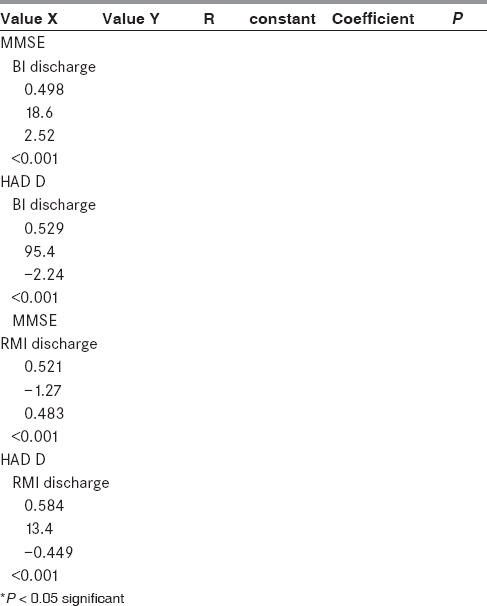
In order to analyze the impact of cognitive status and depression on rehabilitation outcome, we performed correlation and regression analysis. Correlation between MMSE and BI, as well as MMSE and RMI at discharge was moderate and the coefficient of linear regression was positive and statistically significant (P < 0.001). The correlation between the values of HAD D and BI, and HAD D and RMI at discharge were moderate, and the coefficient of linear regression was negative and statistically significant (P < 0.001) [Table 4].
Table 4.
Correlation between MMSE, HAD D subscale and BI and RMI on discharge
Our results suggest that the presence of cognitive decline and depression in patients with ischemic stroke are negative determinants of rehabilitation outcome, which is consistent with several recent studies.[7,8,9] Furthermore, cardiac co-morbidities (arterial hypertension, myocardial infarction, atrial fibrillation, and dilated cardiomyopathy) show significant clinical relevance and have strong influence on rehabilitation outcome. On the other hand, our findings imply that gender and the presence of diabetes mellitus are not related to functional outcome of stroke rehabilitation. A negative association was observed between patients’ age and functional gain after rehabilitation treatment. The etiological stroke subtype should be taken into account when setting rehabilitation goal since patients with large-artery atherosclerosis (LAA) and cardioembolic (CE) ischemic stroke have worse functional outcomes compared to patients with small-vessel disease (SVD) ischemic stroke. The main highlight and purpose of this study is to shed some new light on factors that determine rehabilitation success so that rehabilitation goals are set according to patients’ potentials. However, to strengthen this observation, further large multi-centric studies have to be done in future. To have a simple, easy to administer system for predicting stroke rehabilitation outcome would be an ideal step forward in planning feasible rehabilitation treatment in future.
References
- 1.Roth EJ. Trends in stroke rehabilitation. Eur J Phys Rehabil Med. 2009;45:247–54. [PubMed] [Google Scholar]
- 2.Ones K, Yalcinkaya EY, Toklu BC, Caglar N. Effects of age, gender, and cognitive, functional and motor status on functional outcomes of stroke rehabilitation. NeuroRehabilitation. 2009;25:241–9. doi: 10.3233/NRE-2009-0521. [DOI] [PubMed] [Google Scholar]
- 3.Mirzahi EH, Waitzman A, Arad M, Adunsky A. Gender and functional outcome of elderly ischemic stroke patients. Arch Gerontol Geriatr. 2012;55:438–41. doi: 10.1016/j.archger.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Mustanoja S, Meretoja A, Putaala J, Viitanen V, Curtze S, Atula S, et al. Outcome by stroke etiology in patients receiving thrombolytic treatment: Descriptive subtype analysis. Stroke. 2011;42:102–6. doi: 10.1161/STROKEAHA.110.597534. [DOI] [PubMed] [Google Scholar]
- 5.Jovićević M, Divjak I, Slankamenac P, Božić K, Rabi Žikić TR, Kaloci SR. The most frequent causes of ischemic stroke in young adults. Med Pregl. 2011;64:331–5. doi: 10.2298/mpns1106331j. [DOI] [PubMed] [Google Scholar]
- 6.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtypes of acute ischemic stroke. Definitions for use in a multicenter clinical trial. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 7.Hadidi N, Treat-Jacobson DJ, Lindquist R. Poststroke depression and functional outcome: A critical review of literature. Heart Lung. 2009;38:151–62. doi: 10.1016/j.hrtlng.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Paolucci S, Antonucci G, Pratesi L, Traballesi M, Grasso M, Lubich S. Poststroke depression and its role in rehabilitation of inpatients. Arch Phys Med Rehabil. 1999;80:985–90. doi: 10.1016/s0003-9993(99)90048-5. [DOI] [PubMed] [Google Scholar]
- 9.Lai S, Duncan P, Keighley J, Jonson D. Depressive symptoms and independence in BADL and IADL. J Rehabil Res Dev. 2002;39:589–96. [PubMed] [Google Scholar]


