Abstract
Background
Secondhand Smoking (SHS) has been suggested as a major health problem in the world and is known to cause various negative health effects that have in turn caused the deaths of almost 600,000 people per year. Evidence has suggested that SHS may have an effect on health problems and such findings have influenced the implementation of smoking-free areas. However, few studies have investigated the effects of SHS on stress which is considered major risk factor for mental health. Thus, the purpose of our study was to investigate the association between exposure to SHS and stress.
Methods
We performed a cross-sectional study using data from the Korea National Health and Nutrition Examination Survey (2007–2012). In our study, a total of 33,728 participants were included to evaluate the association between SHS exposure and stress based on smoking status. Association between SHS exposure and stress was examined using logistic regression models.
Results
A total of 12,441 participants (42.9 %) were exposed to SHS in the workplace or at home. In our study, exposure to SHS was significantly associated with higher stress compared to non-exposure, regardless of smoking status (smoker odds ratio [OR]: 1.22; ex-smoker OR: 1.25; never-smoker OR: 1.42). Our results showed that the effect of SHS on stress was greater when exposure took place both at home and in the workplace in smokers and never-smokers.
Conclusions
Exposure to SHS in the workplace and at home is considered to be a risk factor for high stress in both smokers and never-smoker. Therefore, strict regulations banning smoke which can smoking ban reduce SHS exposure are recommended in order to improve the populations’ health.
Keywords: Secondhand smoke, Public health, Stress, Mental health
Background
Smoking is a major problem worldwide that affects the health of individuals and may lead to disease or death. Worldwide, more than 5 million of deaths per year are caused by direct smoking, and 600,000 people have also died from the effects of second-hand smoke (SHS) [1]. Furthermore, smoke-related mortality has increased throughout the 21st century. If no regulations are implemented to ban smoking, smoke-related deaths will increase to more than 8 million per year by 2030 [2]. Therefore, many countries have implemented policies that ban smoking in public places to protect people from SHS exposure [3].
In Korea, the Health Promotion Act was enacted in 1995; this included smoking bans in public buildings and places [4, 5]. However, smoking restrictions in buildings were limited to those of certain sizes (1998: over 3000 m2 ➔ 2006: over 1000 m2), and there has been only slight progress in designating non-smoking areas [5]. In 2010, it was possible to designate non-smoking areas, and fines could be imposed by local government ordinances. Smoke-free areas expanded to public places, and warning labels have had to be added to tobacco packaging since 2012. However, these efforts to reduce smoking have not had a large effect on smoking rates and the SHS exposure rate in Korea. According to Statistics Korea, there has been only a slight difference in the smoking rate between 2007 (25.3 %) and 2013 (24.1 %; smokers: daily or intermittent smokers over 19 years old) [6]. In addition, nearly half of all nonsmokers (including ex-smokers and never-smokers) have been exposed to SHS in the workplace according to data from 2007 (45.9 %) and 2013 (47.3 %) [6].
Recently, new smoke-free policies have resulted in major reductions in both the smoking rate and SHS exposure. First, the price of tobacco was increased from 2500 KRW to 4500 KRW in 2015. Over the past decade, there had been no changes in the tobacco price in Korea. Second, non-smoking areas were expanded so as to include all restaurants. Reductions in the smoking rate and exposure to SHS are expected; however, there have been disputes regarding the designation of smoke-free areas among policymakers and smokers, specifically whether these restrictions are excessive and infringe on the right to smoke [7].
Previous studies have shown that exposure to SHS can cause severe cardiovascular and pulmonary diseases, such as lung cancer, coronary heart disease, and heart failure [8–11]. Low infant birth weight and asthma in children may also occur if pregnant woman are exposed to SHS [12, 13]. In addition, SHS was associated with poor mental health, including depression and insufficient sleep [14–17]. Less is known, however, about the effect of exposure to SHS on stress. Particularly, evidence relating to the effects of SHS on mental health is lacking in Korea.
Stress is caused by various factors, including external stressors, responses to the external environment, and physical reactions to certain circumstances [18, 19]. In general, stress is the result of physical reactions in each individual, and it is caused by changes in health [19–21]. Stress can raise negative effective states, such as anxiety and depression, which can influence physical disease or disease risk. Chronic exposure to stress is considered the most harmful, as it can result in long-term or permanent changes in the emotional, physiological, and behavioral responses that influence susceptibility to and the course of disease [22]. In addition, stress is suggested as a major risk factor for suicide; thus, it is particularly important in Korea, which has the highest suicide rate among Organization for Economic Cooperation and Development (OECD) countries [23–25].
Thus, the aim of our study was to provide evidence to policymakers that can be used to support the implementation of smoke-free areas by investigating the association between exposure to SHS and stress. Considering that reported stress differs according to smoking status, we analyzed smokers, ex-smokers, and never-smoker separately [26]. Furthermore, we investigated the effects of SHS on stress according to different exposure locations, such as in the workplace and at home.
Methods
Data and population
This cross-sectional study was performed using data from the 2007–2012 4th and 5th Korea National Health and Nutrition Examination Survey (KNHANES), which was performed by the Korea Center for Disease Control and Prevention. This nationwide cross-sectional survey has been conducted every year and has received approval from the Institutional Review Board at the Korea Center for Disease Control and Prevention since 2007 (2009-01CON-03-2C/2012-01-EXP-01-2C). The purpose of the KNHANES was to assess the health and nutritional status of Koreans and to provide data for evaluating health risk factors and other factors [27]. It was composed of a health interview, a health examination, and a nutrition survey, all of which were performed by trained medical staff and dieticians. Health interview questionnaires on individual factors such as smoking status, alcohol use, and mental health were collected via self-report. Other individual factors such as socioeconomic status, housing characteristics, and medical condition were collected via face-to-face interview. These data were collected from a total of 50,405 participants during the period of 2007–2012. From these data, we excluded subjects under 19 years old (n = 12,400) (i.e., those deemed too young to work), as we intended to assess exposure according to whether subjects were exposed in the workplace or at home. Next, we excluded missing values and non-responders from the data (n = 4277; see details in Fig. 1). A total of 33,728 participants were included in our study.
Fig. 1.
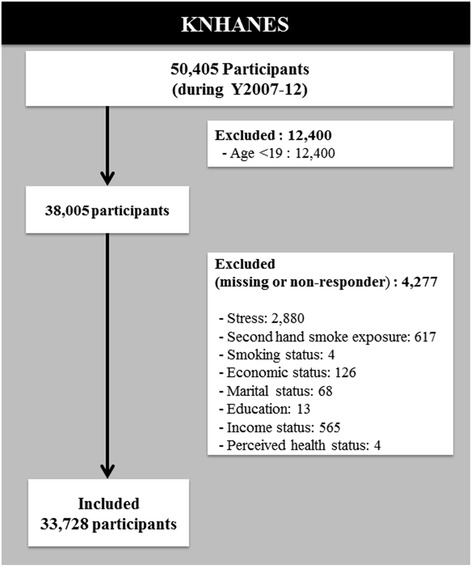
Flow diagram of the study participants
Stress, smoking status and SHS
Stress was measured using self-reports that depended on typical stress recognition following the question: “Do you feel stress in your usual life activities?” Based on the self-report, stress was measured on a scale of 1 to 4 (1 = almost no stress in daily life, 2 = a little stress, 3 = much stress, 4 = very much stress). We classified subjects into two groups: a high stress group (score of 3 or 4) and a low stress group (score of 1 or 2).
We classified smoking status as never-smoker, ex-smoker, or smoker. We defined “never-smoker” as a person who had never smoked. Ex-smokers were defined as those who had smoked in the past yet currently did not. Smokers were defined as those who smoked every day or intermittently.
Exposure to SHS was measured only in the workplace or at home. In the workplace, exposure was self-reported and measured based on answers to the question “How long are you exposed to SHS in your workplace during a day?” Exposure to SHS at home was measured using answers to the question “How long are you exposed to SHS at home during a day?” A status of non-exposure was assigned to participants who answered that they were exposed to 0 h of SHS for each question. In addition, participants who were not employed were also classified as having a status of non-exposure in the workplace. Similarly, subjects were classified as having a non-exposure status at home if they answered “No” to the question “Do you live with a smoker, excluding yourself?” We then divided exposure to SHS into four groups: workplace & home, workplace, home, and non-exposure. Participants were classified as having exposure to SHS regardless of the duration, frequency, or location of any exposure they encountered.
Covariates
We included sex, marital status, age, income, economic status, education level, perceived health status (good or bad), and year (2007–2012) as covariates. Age was stratified into six groups, beginning with 19 years of age. Income was classified as low, middle-low, middle-high, or high. Economic status was classified as employed or unemployed. Education level was classified as elementary school, middle school, high school, or university. Perceived health status was classified as good or bad, based on the question: “What do you think about your health status?”.
Statistical analysis
All analyses were conducted using SAS version 9.2. We weighted the sampling results to convey an accurate representation of the whole nation. The weights were calculated by accounting for the complex survey design, survey non-response, and post-stratification [27]. The participants were thus assumed to represent the Korean population after weighting the data. In the fully adjusted model, all variables were entered simultaneously. Baseline demographic and clinical characteristics were compared using chi-squared tests, and p < 0.05 was considered statistically significant. We used logistic regression analysis (SAS procedure: PROC SURVEYLOGISTIC) [28] to calculate odds ratios (ORs) with 95 % confidence intervals in order to determine the association between exposure to SHS and stress. The main outcome measured the association between stress and exposure to SHS regardless of location, according to smoking status. The second outcome evaluated the association between different exposure locations and stress according smoking status.
Results
In our study, a total of 33,728 participants were included to assess the association between exposure to SHS and stress. Among of them, 7237 (26.9 %) reported that they were current cigarette smokers, 6738 (19.9 %) reported themselves as ex-smokers, and 19,753 (53.2 %) reported themselves as never-smokers. Particularly, the workplace was found to be a major SHS exposure location (Table 1).
Table 1.
General Characteristics of participants by smoking status
| (unit = n, %) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Smoking status | p-value | |||||||
| Smoker | Ex-smoker | Never-smoker | ||||||
| Secondhand smoke exposure state | ||||||||
| Exposure | Workplace & home | 422 | (7.1) | 132 | (2.4) | 978 | (6.0) | <.0001 |
| Workplace | 2,875 | (42.5) | 2,160 | (38.4) | 3,382 | (19.9) | ||
| Home | 424 | (5.8) | 232 | (3.7) | 1,836 | (10.2) | ||
| Non-exposure | 3,516 | (44.5) | 4,214 | (55.5) | 13,557 | (63.9) | ||
| Sex | ||||||||
| Male | 6,120 | (86.8) | 5,634 | (83.4) | 2,668 | (18.5) | <.0001 | |
| Female | 1,117 | (13.2) | 1,104 | (16.6) | 17,085 | (81.5) | ||
| Marital status | ||||||||
| Married | 5,789 | (72.2) | 6,154 | (85.7) | 17,183 | (79.6) | <.0001 | |
| Single | 1,448 | (27.8) | 584 | (14.3) | 2,570 | (20.4) | ||
| Age | ||||||||
| 19–29 | 1,113 | (22.6) | 524 | (13.2) | 2,557 | (20.8) | <.0001 | |
| 30–39 | 1,852 | (27.8) | 1,026 | (18.6) | 3,689 | (19.6) | ||
| 40–49 | 1,542 | (23.2) | 1,135 | (22.4) | 3,694 | (21.7) | ||
| 50–59 | 1,216 | (15.5) | 1,214 | (19.9) | 3,676 | (17.5) | ||
| 60–69 | 858 | (6.5) | 1,399 | (13.8) | 3,290 | (11.0) | ||
| ≥ 70 | 656 | (4.4) | 1,440 | (12.0) | 2,847 | (9.5) | ||
| Income | ||||||||
| Low | 2,134 | (30.2) | 1,513 | (22.3) | 4,649 | (24.8) | <.0001 | |
| Middle-low | 1,904 | (25.7) | 1,700 | (25.8) | 4,860 | (24.8) | ||
| Middle-high | 1,674 | (23.5) | 1,784 | (26.3) | 5,055 | (25.3) | ||
| High | 1,525 | (20.6) | 1,741 | (25.5) | 5,189 | (25.1) | ||
| Economic status | ||||||||
| Employed | 5,510 | (78.5) | 4,388 | (70.8) | 10,207 | (54.3) | <.0001 | |
| Unemployed | 1,727 | (21.5) | 2,350 | (29.2) | 9,546 | (45.7) | ||
| Educational level | ||||||||
| Elementary school | 1,295 | (12.2) | 1,661 | (17.8) | 6,138 | (23.1) | <.0001 | |
| Middle school | 841 | (10.6) | 844 | (11.1) | 2,048 | (9.7) | ||
| High school | 2,933 | (45.7) | 2,230 | (37.8) | 6,283 | (37.0) | ||
| University & college | 2,168 | (31.5) | 2,003 | (33.4) | 5,284 | (30.2) | ||
| Perceived health status | ||||||||
| Good | 5,824 | (82.8) | 5,343 | (82.5) | 15,152 | (79.8) | <.0001 | |
| Bad | 1,413 | (17.2) | 1,395 | (17.5) | 4,601 | (20.2) | ||
| Year | ||||||||
| 2007 | 543 | (8.0) | 561 | (9.1) | 1,511 | (8.0) | <.0001 | |
| 2008 | 1,457 | (18.4) | 1,240 | (18.0) | 3,732 | (17.4) | ||
| 2009 | 1,650 | (18.7) | 1,406 | (18.1) | 4,318 | (19.0) | ||
| 2010 | 1,329 | (19.0) | 1,252 | (18.9) | 3,570 | (18.6) | ||
| 2011 | 1,208 | (18.4) | 1,177 | (17.8) | 3,262 | (17.8) | ||
| 2012 | 1,050 | (17.5) | 1,102 | (18.1) | 3,360 | (19.1) | ||
| Total | 7,237 | (26.9) | 6,738 | (19.9) | 19,753 | (53.2) | ||
% weighted percentage
Among all participants, 1532 (5.6 %) were exposed to SHS both in the workplace and at home, and 564 (37.2 %) of these participants reported that they felt high stress. A total of 8417 (29.7 %) participants were exposed to SHS in the workplace only, and among them, 2678 (31.2 %) reported that they felt high stress. A total of 2492 participants were exposed to SHS at home only, and among them, 867 reported high stress. In addition, the proportion of participants who felt high stress was higher among smokers (n = 2306; 32.8 %) than among ex-smokers (n = 1552; 24.5 %; Table 2).
Table 2.
General characteristics of participants according to stress
| (unit = n, %) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Stress | Total | p-value | ||||||
| High | Low | |||||||
| Secondhand smoke exposure state | ||||||||
| Exposure | Workplace & home | 564 | (37.2) | 968 | (62.8) | 1,532 | (5.6) | <.0001 |
| Workplace | 2,678 | (31.2) | 5,739 | (68.8) | 8,417 | (29.7) | ||
| Home | 867 | (34.8) | 1,625 | (65.2) | 2,492 | (7.7) | ||
| Non-exposure | 5,145 | (25.3) | 16,142 | (74.7) | 21,287 | (57.1) | ||
| Smoking status | ||||||||
| Smoker | 2,306 | (32.8) | 4,931 | (67.2) | 7,237 | (26.9) | <.0001 | |
| Ex-smoker | 1,552 | (24.5) | 5,186 | (75.5) | 6,738 | (19.9) | ||
| Non-smoker | 5,396 | (27.8) | 14,357 | (72.2) | 19,753 | (53.2) | ||
| Sex | ||||||||
| Male | 3,501 | (25.7) | 10,921 | (74.3) | 14,422 | (49.8) | <.0001 | |
| Female | 5,753 | (31.2) | 13,553 | (68.8) | 19,306 | (50.2) | ||
| Marital status | ||||||||
| Married | 7,720 | (27.5) | 21,406 | (72.5) | 29,126 | (78.8) | <.0001 | |
| Single | 1,534 | (32.2) | 3,068 | (67.8) | 4,602 | (21.2) | ||
| Age | ||||||||
| 19–29 | 1,454 | (33.5) | 2,740 | (66.5) | 4,194 | (19.8) | <.0001 | |
| 30–39 | 2,136 | (32.9) | 4,431 | (67.1) | 6,567 | (21.6) | ||
| 40–49 | 1,804 | (28.1) | 4,567 | (71.9) | 6,371 | (22.2) | ||
| 50–59 | 1,533 | (24.4) | 4,573 | (75.6) | 6,106 | (17.5) | ||
| 60–69 | 1,210 | (21.7) | 4,337 | (78.3) | 5,547 | (10.4) | ||
| ≥ 70 | 1,117 | (23.4) | 3,826 | (76.6) | 4,943 | (8.6) | ||
| Income | ||||||||
| Low | 2,516 | (31.0) | 5,780 | (69.0) | 8,296 | (25.8) | <.0001 | |
| Middle-low | 2,375 | (28.8) | 6,089 | (71.2) | 8,464 | (25.2) | ||
| Middle-high | 2,229 | (26.7) | 6,284 | (73.3) | 8,513 | (25.0) | ||
| High | 2,134 | (27.3) | 6,321 | (72.7) | 8,455 | (24.0) | ||
| Economic status | ||||||||
| Employed | 5,818 | (29.6) | 14,287 | (70.4) | 20,105 | (64.1) | <.0001 | |
| Unemployed | 3,436 | (26.4) | 10,187 | (73.6) | 13,623 | (35.9) | ||
| Educational level | ||||||||
| Elementary school | 2,439 | (27.2) | 6,655 | (72.8) | 9,094 | (19.1) | <.0001 | |
| Middle school | 847 | (23.9) | 2,886 | (76.1) | 3,733 | (10.2) | ||
| High school | 3,054 | (27.7) | 8,392 | (72.3) | 11,446 | (39.5) | ||
| University & college | 2,914 | (31.7) | 6,541 | (68.3) | 9,455 | (31.2) | ||
| Perceived health status | ||||||||
| Good | 6,189 | (24.9) | 20,130 | (75.1) | 26,319 | (81.1) | <.0001 | |
| Bad | 3,065 | (43.9) | 4,344 | (56.1) | 7,409 | (18.9) | ||
| Year | ||||||||
| 2007 | 684 | (27.2) | 1,931 | (72.8) | 2,615 | (8.2) | <.0001 | |
| 2008 | 1,803 | (28.8) | 4,626 | (71.2) | 6,429 | (17.8) | ||
| 2009 | 2,195 | (31.0) | 5,179 | (69.0) | 7,374 | (18.8) | ||
| 2010 | 1,674 | (28.1) | 4,477 | (71.9) | 6,151 | (18.7) | ||
| 2011 | 1,502 | (28.1) | 4,145 | (71.9) | 5,647 | (18.0) | ||
| 2012 | 1,396 | (26.9) | 4,116 | (73.1) | 5,512 | (18.4) | ||
| Total | 9,254 | (28.5) | 24,474 | (71.5) | 33,728 | (100.0) | ||
% weighted percentage
The main results of the association between SHS exposure and stress were calculated according to smoking status. Regardless of smoking status, SHS exposure was more associated with higher stress than non-exposure after fully adjusted model. However, the effect of SHS exposure on stress was greater in never-smokers (OR: 1.42; 95 % CI: 1.30–1.56) than in smokers (OR: 1.22; 95 % CI: 1.08–1.39) and, similarly, ex-smokers (OR: 1.25; 95 % CI: 1.07–1.46). Regarding economic status, employed never-smokers felt higher stress than those who were unemployed (OR: 1.23; 95 % CI: 1.12–1.34; Table 3).
Table 3.
The association between SHS exposure and stress by smoking status
| Unadjusted | Adjusted | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Smoker | Ex-smoker | Never smoker | Smoker | Ex-smoker | Never smoker | |||||||||||||
| Variable | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | ||||||
| Secondhand smoke exposure state | ||||||||||||||||||
| Exposurea | 1.31 | 1.16 | 1.47 | 1.42 | 1.23 | 1.63 | 1.44 | 1.33 | 1.57 | 1.22 | 1.08 | 1.39 | 1.25 | 1.07 | 1.46 | 1.42 | 1.30 | 1.56 |
| Non-exposure | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Sex | ||||||||||||||||||
| Male | 0.49 | 0.42 | 0.00 | 0.44 | 0.37 | 0.52 | 0.64 | 0.57 | 0.73 | 0.51 | 0.43 | 0.61 | 0.50 | 0.41 | 0.61 | 0.59 | 0.52 | 0.67 |
| Female | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Marital status | ||||||||||||||||||
| Married | 0.90 | 0.78 | 1.03 | 0.70 | 0.57 | 0.86 | 0.82 | 0.74 | 0.91 | 1.22 | 1.01 | 1.46 | 0.99 | 0.74 | 1.32 | 1.08 | 0.91 | 1.29 |
| Single | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Age | ||||||||||||||||||
| 19–29 | 1.88 | 1.44 | 2.45 | 2.50 | 1.92 | 3.26 | 1.29 | 1.12 | 1.49 | 2.69 | 1.86 | 3.89 | 2.54 | 1.67 | 3.84 | 1.98 | 1.57 | 2.52 |
| 30–39 | 2.01 | 1.57 | 2.57 | 2.56 | 2.06 | 3.18 | 1.13 | 0.98 | 1.29 | 2.61 | 1.87 | 3.63 | 2.68 | 1.98 | 3.62 | 1.51 | 1.25 | 1.83 |
| 40–49 | 1.60 | 1.26 | 2.05 | 1.93 | 1.56 | 2.39 | 0.96 | 0.84 | 1.09 | 2.03 | 1.48 | 2.78 | 2.30 | 1.72 | 3.08 | 1.25 | 1.04 | 1.50 |
| 50–59 | 1.19 | 0.91 | 1.54 | 1.39 | 1.11 | 1.75 | 0.90 | 0.79 | 1.03 | 1.45 | 1.08 | 1.95 | 1.66 | 1.27 | 2.17 | 1.08 | 0.92 | 1.25 |
| 60–69 | 0.81 | 0.61 | 1.08 | 0.92 | 0.72 | 1.16 | 0.93 | 0.81 | 1.07 | 0.96 | 0.70 | 1.30 | 1.06 | 0.82 | 1.36 | 1.02 | 0.88 | 1.18 |
| 70≥ | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Income | ||||||||||||||||||
| Bottom | 0.90 | 0.76 | 1.07 | 1.41 | 1.14 | 1.74 | 1.26 | 1.13 | 1.41 | 0.87 | 0.72 | 1.04 | 1.30 | 1.03 | 1.63 | 1.22 | 1.08 | 1.38 |
| Middle-bottom | 0.86 | 0.72 | 1.02 | 1.22 | 1.00 | 1.49 | 1.13 | 1.01 | 1.26 | 0.84 | 0.70 | 1.01 | 1.18 | 0.96 | 1.46 | 1.10 | 0.98 | 1.24 |
| Middle-top | 0.85 | 0.72 | 1.00 | 0.91 | 0.74 | 1.11 | 1.05 | 0.94 | 1.18 | 0.84 | 0.70 | 1.00 | 0.87 | 0.70 | 1.08 | 1.05 | 0.93 | 1.18 |
| Top | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Economic status | ||||||||||||||||||
| Working | 1.01 | 0.88 | 1.17 | 1.10 | 0.95 | 1.28 | 1.21 | 1.12 | 1.30 | 1.01 | 0.85 | 1.21 | 1.20 | 0.99 | 1.45 | 1.23 | 1.12 | 1.34 |
| Not working | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Educational level | ||||||||||||||||||
| Elementary school | 0.61 | 0.51 | 0.73 | 0.72 | 0.60 | 0.86 | 0.93 | 0.85 | 1.02 | 0.77 | 0.60 | 0.98 | 1.03 | 0.80 | 1.34 | 0.89 | 0.76 | 1.03 |
| Middle school | 0.72 | 0.58 | 0.89 | 0.63 | 0.49 | 0.81 | 0.66 | 0.58 | 0.76 | 0.82 | 0.64 | 1.04 | 0.83 | 0.63 | 1.11 | 0.67 | 0.57 | 0.79 |
| High school | 0.81 | 0.71 | 0.92 | 0.88 | 0.75 | 1.03 | 0.80 | 0.73 | 0.88 | 0.78 | 0.68 | 0.90 | 0.84 | 0.71 | 1.01 | 0.76 | 0.68 | 0.84 |
| University & college | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Perceived health status | ||||||||||||||||||
| Good | 0.45 | 0.39 | 0.52 | 0.54 | 0.46 | 0.64 | 0.37 | 0.34 | 0.41 | 0.39 | 0.34 | 0.46 | 0.45 | 0.38 | 0.55 | 0.33 | 0.30 | 0.36 |
| Bad | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Year | ||||||||||||||||||
| 2007 | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| 2008 | 1.18 | 0.92 | 1.51 | 1.41 | 1.06 | 1.87 | 0.93 | 0.79 | 1.09 | 1.14 | 0.89 | 1.46 | 1.39 | 1.02 | 1.88 | 0.87 | 0.73 | 1.02 |
| 2009 | 1.18 | 0.92 | 1.50 | 1.39 | 1.06 | 1.83 | 1.15 | 0.99 | 1.33 | 1.20 | 0.94 | 1.53 | 1.38 | 1.04 | 1.83 | 1.12 | 0.96 | 1.31 |
| 2010 | 1.07 | 0.82 | 1.40 | 1.27 | 0.95 | 1.70 | 0.95 | 0.81 | 1.12 | 1.10 | 0.84 | 1.45 | 1.25 | 0.92 | 1.71 | 0.92 | 0.77 | 1.09 |
| 2011 | 1.16 | 0.89 | 1.51 | 1.01 | 0.75 | 1.36 | 0.98 | 0.84 | 1.15 | 1.22 | 0.93 | 1.60 | 1.06 | 0.77 | 1.46 | 1.00 | 0.84 | 1.18 |
| 2012 | 1.02 | 0.79 | 1.34 | 1.19 | 0.88 | 1.59 | 0.90 | 0.77 | 1.05 | 1.02 | 0.78 | 1.34 | 1.26 | 0.92 | 1.73 | 0.92 | 0.78 | 1.09 |
aExposure included participants who were exposed to SHS in the workplace or at home
The second outcome, the association between different exposure locations and stress according to smoking status, is shown in Fig. 2. In smokers, SHS exposure both in the workplace and at home (OR: 1.35; 95 % CI: 1.04–1.74) and in the workplace only (OR: 1.26; 95 % CI: 1.10–1.45) was more associated with higher stress than non-exposure. Among ex-smokers, the effect of SHS on stress was highest when exposure occurred at home (OR: 1.58; 95 % CI: 1.06–2.34). Never-smokers felt the least stressed when exposed to SHS, regardless of the location. However, the effect was highest when exposed to SHS both in the workplace and at home (OR: 1.56; 95 % CI: 1.06–2.34; Fig. 2).
Fig. 2.

Results of logistic regression, indicating the association between exposure to SHS in different locations and stress according to smoking status. *All variables are adjusted for marital status, age, income, economic status education level, perceived health status, and year
Discussion
The aim of our study was to assess the association between SHS exposure and stress. We found that almost half of the participants were exposed to SHS, with exposure in the workplace occurring more prevalently than at home. Although the intensity of the effect of SHS on stress varied according to smoking status, SHS was associated with an increase in stress. Particularly, the effect of SHS on stress was greatest in never-smokers. These results indicate that many people in Korea are exposed to unwanted SHS in their own homes and the workplace, suggesting that these locations are key sources of harm. Previous studies also suggested that the location of SHS is important (e.g., bars, restaurants, public places, homes) [29–32]. Such locations are closely connected with personal everyday life, meaning that the potential for exposure to SHS also increases when visiting such locations. It also implies that designating smoke-free areas in such locations is important for reducing SHS.
Thus, we performed a further evaluation that compared SHS exposure in the workplace and at home. Our results indicated that the effect of SHS on stress differed according to both location and smoking status. Among smokers, exposure to SHS in the workplace and at home was associated with an increase in stress. However, the effect of SHS on stress decreased when smokers were exposed only in the workplace. This increase in stress among smokers may have been associated with the effects of nicotine. Smokers undergo physical changes associated with smoking that are similar to those that occur when people experience stress [33–35], as nicotine leads to increased heart rate, blood pressure, and breathing rate [26]. Thus, the chronically high nicotine levels in the bodies of smokers compared to non-smokers may mean that smokers have a greater physical reaction to SHS exposure that makes them feel more stressed. However, ex-smokers were found to experience a greater effect of SHS on stress when they were exposed to SHS at home only; conversely, a lesser effect was found for SHS exposure in the workplace. Ex-smokers may find it difficult to quit smoking due to the nicotine addiction associated with smoking [36]. Therefore, an ex-smoker (who does not currently smoke) may feel stressed when exposed to SHS, as it may tempt him or her to smoke. A previous study suggests that exposure to SHS is an important factor in determining the success of people who attempt to quit the smoking [37, 38]. Similar research has suggested that, in Korea, it is difficult to quit smoking when living with a smoker [39]. Thus, ex-smokers who are exposed to SHS at home might be hindered in their intention to quit smoking, which could account for the increase in stress. Among never-smokers, exposure to SHS was associated with a high increase in stress, both in the workplace and at home. These results suggest that the restriction of smoking both in the workplace and at home may be important to reducing stress. This finding is similar to a previous study that reported that SHS was found to have a negative effect on mental health [14, 40]. However, certain studies contrasted with our study in that they were unable to find an association between mental health and exposure to SHS [41, 42].
In Korea, there has been a ban on smoking in buildings of a certain size, which has contributed to an increase in the number of smoke-free areas. However, this ban does not currently apply to all indoor locations and is weaker than those of other countries. As a result, there has been no decrease in SHS, even after the implementation of a smoke-free law [43, 44]. Although many public places and other indoor locations have been designated as smoke-free areas, many people in Korea continue to face problems related to SHS. These results suggest that stronger regulations related to smoking bans are needed in Korea. Restrictions calling for smoke-free areas should also include exact evaluations as to how to create separate smoking areas. In Korea, public places that have designated smoke-free areas must also create areas for smokers. However, such smoking areas were often found to not be completely separate from smoke-free areas, resulting in the occurrence of SHS in smoke-free areas [45]. Thus, policies allowing for smoking areas must ensure that such areas are completely separated from smoke-free areas in the future. To do so, an employer must establish strict smoking regulations in the workplace and provide a separate space for smokers. In addition, better regulations for ensuring smoke-free areas in homes are needed in order to reduce domestic SHS. In Korea, smoke-free areas have primarily been implemented in public places and locations used by many people, and regulations calling for smoke-free areas in private places are lacking in comparison. Such differences might be due to the social aspect of smoking, as, generally, few home smoking restrictions have been implemented in Korea [46]. Thus, a public campaign for improving awareness of the risk of SHS on health is needed in order to reduce unwanted SHS at home. In addition, children should be educated about the risks of both smoking and exposure to SHS.
There were a number of limitations in this study. First, our study was cross-sectional, and information was obtained via self-report, meaning that we were unable to imply causation between stress and exposure to SHS. Self-report can lead to an underestimation of the actual exposure to SHS and might be associated with recall bias [47]. However, a previous study suggested that self-report had high validity and that results were similar to those obtained from biological markers [48]. Second, our study did not investigate SHS exposure other than that in the home and workplace, and the exposure duration in each of these locations was not assessed. Therefore, future studies should investigate other public places of SHS exposure, such as at bus stops and on streets. Third, we did not consider the potential effect of the workplace environment on stress. Finally, unmeasured variables and other potential stressors, such as relationships with co-workers and spouses, could have confounded the present results. Thus, a further study considering such factors is needed.
However, this study had several strengths. We used KNHANES data, which ensured that a reliable sampling design was implemented countrywide. Additionally, the large scale of the survey meant that it was representative of the nation as a whole. Second, although many studies have focused on the physical health effects of SHS exposure, our study was the first to focus on stress, a negative mental effect, in relation to SHS exposure. Finally, we suggest that exposure to SHS may be an important risk factor for stress, particularly if no interventions to prevent SHS are undertaken.
In our study, we found that SHS exposure in a specific location may increase individual stress. Both the workplace and the home are important places, as they are closely connected to life and can have a major influence on each individual. Therefore, the enforcement of smoke-free policies and laws banning smoking is essential for reducing unnecessary stress, and policymakers should strengthen smoke-free regulations to reduce unwanted stress related to SHS exposure.
Conclusions
In conclusion, SHS may be a preventable risk factor for stress that should be managed appropriately. Consistent management of smoke-free areas would result in a healthier environment. Thus, policymakers should consider anti-SHS policies in order to reduce preventable stress.
Data source
The data used in our study are open data. Anyone who submits a suitable form can use the data via website (https://knhanes.cdc.go.kr/knhanes/index.do).
Acknowledgements
This study did not receive any external funding. The authors have declared that they have no competing or potential conflicts of interest.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SJK conceived the idea for the study, carried out the statistical analysis, interpreted the data, and drafted the manuscript. ECP acted as an advisor of the study design and substantially contributed to the conception and drafting of the paper. KTH and SYC substantially contributed to the interpretation of the data. SYL substantially contributed to the drafting of the paper. All authors read and approved the final manuscript.
Contributor Information
Seung Ju Kim, Email: yuwooki@yuhs.ac.
Kyu-Tae Han, Email: kthan@yuhs.ac.
Seo Yoon Lee, Email: sunjung5958@yuhs.ac.
Sung-Youn Chun, Email: csy6909@yuhs.ac.
Eun-Cheol Park, Phone: 82-2-2228-1862, Email: ecpark@yuhs.ac.
References
- 1.Oberg M, Jaakkola MS, Woodward A, Peruga A, Pruss-Ustun A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet. 2011;377(9760):139–46. doi: 10.1016/S0140-6736(10)61388-8. [DOI] [PubMed] [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11) doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization(WHO) WHO report on the global tobacco epidemic, 2008: the MPOWER package. 2008. [Google Scholar]
- 4.Chung W, Kim H, Lim S, Lee S, Cho K. Factors influencing cigarette smoking and quantified implications for anti-smoking policy: evidence from South Korea. Int J Public Health. 2009;54(6):409–19. doi: 10.1007/s00038-009-0087-x. [DOI] [PubMed] [Google Scholar]
- 5.Khang Y-H, Yun S-C, Cho H-J, Jung-Choi K. The impact of governmental antismoking policy on socioeconomic disparities in cigarette smoking in South Korea. Nicotine Tob Res. 2009;11(3):262–9. doi: 10.1093/ntr/ntn036. [DOI] [PubMed] [Google Scholar]
- 6.Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2012. Available from: http://kostat.go.kr.
- 7.Lee Minjin LS, Lee S, Cho H. Analyzing issues and a status investigation of studies on tobacco control policies in South Korea. Korea Inst Health Soc Aff. 2014;34(3):165–91. [Google Scholar]
- 8.Liu R, Jiang Y, Li Q, Hammond SK. An assessment of health risks and mortality from exposure to secondhand smoke in Chinese restaurants and bars. PLoS One. 2014;9(1) doi: 10.1371/journal.pone.0084811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim CH, Lee YC, Hung RJ, McNallan SR, Cote ML, Lim WY, et al. Exposure to secondhand tobacco smoke and lung cancer by histological type: a pooled analysis of the International Lung Cancer Consortium (ILCCO). Int J Cancer. 2014. [DOI] [PMC free article] [PubMed]
- 10.Vardavas CI, Mpouloukaki I, Linardakis M, Ntzilepi P, Tzanakis N, Kafatos A. Second hand smoke exposure and excess heart disease and lung cancer mortality among hospital staff in Crete, Greece: a case study. Int J Environ Res Public Health. 2008;5(3):125–9. doi: 10.3390/ijerph5030125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laden F, Chiu YH, Garshick E, Hammond SK, Hart JE. A cross-sectional study of secondhand smoke exposure and respiratory symptoms in non-current smokers in the U.S. trucking industry: SHS exposure and respiratory symptoms. BMC Public Health. 2013;13:93. doi: 10.1186/1471-2458-13-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Norsa’adah B, Salinah O. The effect of second-hand smoke exposure during pregnancy on the newborn weight in Malaysia. Malays J Med Sci. 2014;21(2):44–53. [PMC free article] [PubMed] [Google Scholar]
- 13.Simons E, To T, Moineddin R, Stieb D, Dell SD. Maternal second-hand smoke exposure in pregnancy is associated with childhood asthma development. J Allergy Clin Immunol In Pract. 2014;2(2):201–7. doi: 10.1016/j.jaip.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 14.Hamer M, Stamatakis E, Batty GD. Objectively assessed secondhand smoke exposure and mental health in adults: cross-sectional and prospective evidence from the Scottish Health Survey. Arch Gen Psychiatry. 2010;67(8):850–5. doi: 10.1001/archgenpsychiatry.2010.76. [DOI] [PubMed] [Google Scholar]
- 15.Sabanayagam C, Shankar A. The association between active smoking, smokeless tobacco, second-hand smoke exposure and insufficient sleep. Sleep Med. 2011;12(1):7–11. doi: 10.1016/j.sleep.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bandiera FC, Caban-Martinez AJ, Arheart KL, Davila EP, Fleming LE, Dietz NA, et al. Secondhand smoke policy and the risk of depression. Ann Behav Med. 2010;39(2):198–203. doi: 10.1007/s12160-010-9174-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sobotova L, Liu Y-H, Burakoff A, Sevcikova L, Weitzman M. Household exposure to secondhand smoke is associated with decreased physical and mental health of mothers in the USA. Matern Child Health J. 2011;15(1):128–37. doi: 10.1007/s10995-009-0549-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kasl SV. Stress and health. Annu Rev Public Health. 1984;5(1):319–41. doi: 10.1146/annurev.pu.05.050184.001535. [DOI] [PubMed] [Google Scholar]
- 19.Bovier PA, Chamot E, Perneger TV. Perceived stress, internal resources, and social support as determinants of mental health among young adults. Qual Life Res. 2004;13(1):161–70. doi: 10.1023/B:QURE.0000015288.43768.e4. [DOI] [PubMed] [Google Scholar]
- 20.Selye H. Stress in health and disease: Butterworth-Heinemann; 2013.
- 21.Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci. 2012;109(16):5995–9. doi: 10.1073/pnas.1118355109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298(14):1685–7. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 23.Song TM, Song J, An J-Y, Hayman LL, Woo J-M. Psychological and social factors affecting Internet searches on suicide in Korea: a big data analysis of Google search trends. Yonsei Med J. 2014;55(1):254–63. doi: 10.3349/ymj.2014.55.1.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lim M, Kim S-W, Nam Y-Y, Moon E, Yu J, Lee S, et al. Reasons for desiring death: examining causative factors of suicide attempters treated in emergency rooms in Korea. J Affect Disord. 2014;168:349–56. doi: 10.1016/j.jad.2014.07.026. [DOI] [PubMed] [Google Scholar]
- 25.Song TM, An J-Y, Hayman LL, Woo J-M, Yom Y-H. Stress, depression, and lifestyle behaviors in Korean adults: A latent means and multi-group analysis on the Korea health panel data. Behav Med. 2014; (ahead-of-print):1-10. [DOI] [PubMed]
- 26.Richards JM, Stipelman BA, Bornovalova MA, Daughters SB, Sinha R, Lejuez C. Biological mechanisms underlying the relationship between stress and smoking: state of the science and directions for future work. Biol Psychol. 2011;88(1):1–12. doi: 10.1016/j.biopsycho.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kweon S, Kim Y, Jang M-j, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43(1):69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nadimpalli V, Hubbell K, Rockville W. Simplifying the analysis of complex survey data using the SAS® survey analysis procedures. Cary, NC: SAS Institute Inc; 2012. [Google Scholar]
- 29.Jones S, Love C, Thomson G, Green R, Howden‐Chapman P. Second‐hand smoke at work: the exposure, perceptions and attitudes of bar and restaurant workers to environmental tobacco smoke. Aust N Z J Public Health. 2001;25(1):90–3. doi: 10.1111/j.1467-842X.2001.tb00557.x. [DOI] [PubMed] [Google Scholar]
- 30.Bates M, Fawcett J, Dickson S, Berezowski R, Garrett N. Exposure of hospitality workers to environmental tobacco smoke. Tob Control. 2002;11(2):125–9. doi: 10.1136/tc.11.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stillman F, Navas-Acien A, Ma J, Ma S, Avila-Tang E, Breysse P, et al. Second-hand tobacco smoke in public places in urban and rural China. Tob Control. 2007;16(4):229–34. doi: 10.1136/tc.2006.018333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akhtar PC, Haw SJ, Currie DB, Zachary R, Currie CE. Smoking restrictions in the home and secondhand smoke exposure among primary schoolchildren before and after introduction of the Scottish smoke-free legislation. Tob Control. 2009;18(5):409–15. doi: 10.1136/tc.2009.030627. [DOI] [PubMed] [Google Scholar]
- 33.Aronson KR, Almeida DM, Stawski RS, Klein LC, Kozlowski LT. Smoking is associated with worse mood on stressful days: results from a national diary study. Ann Behav Med. 2008;36(3):259–69. doi: 10.1007/s12160-008-9068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lyvers M, Thorberg FA, Dobie A, Huang J, Reginald P. Mood and interpersonal functioning in heavy smokers. J Subst Use. 2008;13(5):308–18. doi: 10.1080/14659890802040807. [DOI] [Google Scholar]
- 35.Asbridge M, Ralph K, Stewart S. Private space second-hand smoke exposure and the mental health of non-smokers: a cross-sectional analysis of Canadian adults. Addict Behav. 2013;38(3):1679–86. doi: 10.1016/j.addbeh.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 36.Benowitz NL. Neurobiology of nicotine addiction: implications for smoking cessation treatment. Am J Med. 2008;121(4 Suppl 1):S3–10. doi: 10.1016/j.amjmed.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 37.Eng L, Su J, Qiu X, Palepu PR, Hon H, Fadhel E, et al. Second-hand smoke as a predictor of smoking cessation among lung cancer survivors. J Clin Oncol. 2014;32(6):564–70. doi: 10.1200/JCO.2013.50.9695. [DOI] [PubMed] [Google Scholar]
- 38.Wang MP, Ho SY, Lo WS, Lam TH. Smoking family, secondhand smoke exposure at home, and quitting in adolescent smokers. Nicotine Tob Res. 2013;15(1):185–91. doi: 10.1093/ntr/nts109. [DOI] [PubMed] [Google Scholar]
- 39.Ryu S-Y, Shin J-H, Kang M-G, Park J. Factors associated with intention to quit smoking among male smokers in 13 communities in honam region of Korea: 2010 community health survey. Korean J Health Educ Promot. 2011;28(2):75–85. [Google Scholar]
- 40.Lee K-J. Current smoking and secondhand smoke exposure and depression among Korean adolescents: analysis of a national cross-sectional survey. BMJ Open. 2014;4(2) doi: 10.1136/bmjopen-2013-003734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lam E, Kvaavik E, Hamer M, Batty G. Association of secondhand smoke exposure with mental health in men and women: cross-sectional and prospective analyses using the UK Health and Lifestyle Survey. Eur Psychiatry. 2013;28(5):276–81. doi: 10.1016/j.eurpsy.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 42.Bot M, Vink JM, Willemsen G, Smit JH, Neuteboom J, Kluft C, et al. Exposure to secondhand smoke and depression and anxiety: a report from two studies in the Netherlands. J Psychosom Res. 2013;75(5):431–6. doi: 10.1016/j.jpsychores.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 43.Oh BYJ, Hong SY, Lee D-H, Tamplin S. Policy effects of secondhand smoke exposure in public places in the Republic of Korea: evidence from PM2. 5 levels and air nicotine concentrations. Asian Pac J Cancer Prev. 2013;14(12):7725–30. doi: 10.7314/APJCP.2013.14.12.7725. [DOI] [PubMed] [Google Scholar]
- 44.Hughes SC, Corcos IA, Hofstetter CR, Hovell MF, Seo D-C, Irvin VL, et al. Secondhand smoke exposure among nonsmoking adults in Seoul, Korea. Asian Pac J Cancer Prev. 2008;9(2):247–52. [PubMed] [Google Scholar]
- 45.Sooyoung Guak KL, Kim S, Kim S, Yang W, Ha K. Impact of the smoke-free law on secondhand smoke in computer game rooms. Korean Soc Environ Health. 2015;41(1):11–6. doi: 10.5668/JEHS.2015.41.1.11. [DOI] [Google Scholar]
- 46.Ayers JW, Hofstetter CR, Hughes SC, Park H, Paik H-Y, Irvin VL, et al. Smoking on both sides of the Pacific: home smoking restrictions and secondhand smoke exposure among Korean adults and children in Seoul and California. Nicotine Tob Res. 2010;12(11):1142–50. doi: 10.1093/ntr/ntq164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Donaldson SI, Grant-Vallone EJ. Understanding self-report bias in organizational behavior research. J Bus Psychol. 2002;17(2):245–60. doi: 10.1023/A:1019637632584. [DOI] [Google Scholar]
- 48.Vartiainen E, Seppälä T, Lillsunde P, Puska P. Validation of self reported smoking by serum cotinine measurement in a community-based study. J Epidemiol Community Health. 2002;56(3):167–70. doi: 10.1136/jech.56.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]


