Abstract
Background
Before 2012, UK GPs were paid only to offer cessation advice to smokers and only to those with smoking-related disease, a minority of all smokers. From 2012, GPs are now paid to offer all smokers referral for behavioural support and medication to assist cessation at least once every 2 years.
Aim
To quantify the impact of this new recommendation and payment on indicators of smoking cessation activity.
Design and setting
Interrupted time series analysis of data from general practices in England contributing data to The Health Improvement Network (THIN).
Method
Data were extracted on monthly rates of recorded delivery of smoking cessation advice, referral to NHS Stop Smoking Services, and prescription of smoking cessation medications, among an average of 3.3 million patients aged >16 years registered each month in THIN. ARIMA models were used to quantify changes in rates of cessation activity after the 2012 Quality and Outcomes Framework (QOF) revision compared with beforehand.
Results
The proportion of patients each month with a record of advice to quit smoking increased by 19.6% (95% CI = 7.9 to 31.4) in the year after the introduction of payments compared with the 8 years beforehand; the recording of referral to Stop Smoking Services increased by 38.8% (95% CI = 15.2 to 62.4). There was no significant change in prescription of smoking cessation medication, −7.7% (95% CI = −21.6 to 6.2).
Conclusion
Paying GPs to intervene with all smokers and offer support rather than just advice to quit is associated with an increase in recording of advice and referring patients for behavioural support to stop smoking, but no change in prescribing pharmacotherapy for cessation.
Keywords: financial incentive, interrupted time series analysis, prescribing patterns, primary care, smoking cessation, tobacco use
INTRODUCTION
Smoking remains the largest avoidable cause of premature death worldwide.1 Primary care physicians or GPs and other members of the primary healthcare team are well placed to intervene with smokers, having at their disposal a range of cessation interventions proven effective and cost-effective in helping smokers to quit, including offering brief cessation advice during the course of a consultation,2 referring smokers to behavioural support programmes,3 and prescribing nicotine replacement therapy (NRT),4 bupropion,5 and varenicline.6
About one-third of the pay for GPs in the UK derives from the pay-for-performance scheme called the Quality and Outcomes Framework (QOF), introduced in 2004. Since the QOF’s inception, GPs have been remunerated for maintaining a register of all their patients who smoke and for offering unspecified ‘advice’ only to smokers who had certain smoking-related illnesses (asthma, chronic obstructive pulmonary disease, and most common forms of cardiovascular disease), but no payment for advising smokers without such a condition. Previous studies have found that the introduction of the QOF led to increased rates of ascertainment of smoking status and delivery of advice for all smokers, and for smokers with the ‘remunerated’ smoking-related diseases in particular.7,8 The precise requirements of the QOF targets have changed over time. The most substantial revision to the QOF smoking targets came in April 2012, requiring GPs to offer ‘support and treatment’ to smokers, every 15 months for patients with chronic conditions, and, for the first time, offer support and treatment every 27 months to everyone who smokes. This offer of support and treatment is intended to include offering referral to the NHS Stop Smoking Service, along with prescribing pharmacotherapy.9
No previous evaluations have been identified of pay-for-performance interventions rewarding GPs for systematically identifying smokers and offering evidence-based treatment. This study quantifies the impact of the April 2012 QOF revision on the monthly rate of delivery of cessation advice, referral of smokers to specialist cessation services, and prescribing of smoking cessation medications, using a large database of electronic primary care records.
METHOD
Data source
Data were taken from The Health Improvement Network (THIN), which to date contains information from over 12 million patients from nearly 600 general practices throughout the UK.10 THIN has been validated previously and was shown to be broadly representative of the UK population in terms of the age–sex distribution of patients.11 Adult smoking prevalence recorded in THIN is comparable at national11 and regional12 levels with data from population surveys, and prescription data for smoking cessation medications are comparable with data on dispensed prescriptions.13
How this fits in
In April 2012 a pay-for-performance target was introduced into UK primary care to encourage GPs to offer referral to the NHS Stop Smoking Services and prescribe pharmacotherapy to all smokers, regardless of their smoking-related medical history. Recording of the delivery of cessation advice and referral to Stop Smoking Services increased after this point in time. There was no increase, and possibly a decrease, however, in prescription of pharmacotherapy.
The QOF rewards GPs for certain specified actions with smokers. The precise terminology of the QOF before the change in 2012 and afterwards is shown in Box 1.
Box 1. Key elements of the wording change from the QOF before and after 2012.
| Before 2012 | After 2012 | |
|---|---|---|
| Patients with specified chronic conditions | The percentage of patients with any or any combination of the following conditions: coronary heart disease, stroke or transient ischaemic attack, hypertension, diabetes, chronic obstructive pulmonary disease, chronic kidney disease, asthma, schizophrenia, bipolar affective disorder or other psychoses, and who smoke whose notes contain a record that smoking cessation advice or referral to a specialist service, where available, has been offered within the preceding 15 months | The percentage of patients with any or any combination of the following conditions: coronary heart disease, peripheral arterial disease, stroke or transient ischaemic attack, hypertension, diabetes, chronic obstructive pulmonary disease, chronic kidney disease, asthma, schizophrenia, bipolar affective disorder or other psychoses, and who smoke who have a record of an offer of support and treatment within the preceding 12 months |
| General population | No equivalent | The percentage of patients aged 15 years and over who are recorded as current smokers who have a record of an offer of support and treatment within the preceding 24 months |
The QOF is implemented through detailed business rules.14 These rules specify the Read Codes15 that can be used to show that a requirement has been met. In this case, the codes that are allowed to indicate offering support and treatment to smokers include one termed ‘smoking cessation advice’. This is the same code that was used to indicate the delivery of advice in the wording of the QOF before the 2012 change.
All patients aged >16 years were identified who contributed data to THIN each month from April 2004 (when the QOF was implemented) to March 2013 (1 year after the revision to the smoking targets). For each patient, Read Codes were used to identify whether they were advised to quit or referred to the NHS Stop Smoking Service in that month. Multilex drug codes were used to identify whether patients were prescribed a smoking cessation medication (NRT, bupropion, or varenicline) each month.
Statistical analysis
As indicators of GP delivery of cessation activity, rates of recording of advice to quit, referral to the NHS Stop Smoking Service, and prescription of smoking cessation medication per 10 000 patients aged >16 years registered in THIN per month were calculated. As in a previous work,16 ARIMA (autoregressive integrated moving average) modelling was used to demonstrate the impact of the 2012 QOF revisions on each of the three data series, taking into account any underlying long-term and/or seasonal trends in GP activity.
Each series was first log-transformed to stabilise its variance. The autocorrelation and partial autocorrelation functions (ACF and PACF) were then examined to assess whether first-order or seasonal differencing were necessary and to determine the order of the autoregressive and moving-average parameters needed to model autocorrelation in the data. A dummy variable (coded 0 before April 2012 and 1 from this month onwards) was included in each model to examine the effect of the QOF revision, assuming a priori a step change in the outcome at the time of the QOF revision. Model residuals were examined for normality, and the residual ACF and PACF examined to assess whether all autocorrelation was adequately modelled. Results are presented as percentage changes in the outcome variable in the period after the QOF revision relative to the period beforehand.
Initial examination of plots of each data series over time showed a peak in the recording of referral in early 2009, and previous literature has suggested there was an increase in prescribing of smoking cessation medications in the run up to the introduction of smoke-free legislation.16 Therefore, as a sensitivity analysis ARIMA modelling was also carried out using a restricted time series of data from April 2010 onwards to estimate the effect of the QOF revision relative to the most recent 2 years before its implementation.
All data management and analysis was carried out using Stata (version 13).
RESULTS
On average there were 3 337 881 (standard deviation [SD] 81 110) patients aged >16 years registered in THIN each month. Each month an average of 41 649 (SD 9082) people had a record of advice to quit, 1001 (SD 371) had a record of referral to the NHS Stop Smoking Service, and 9921 (SD 1851) had a prescription for a smoking cessation medication.
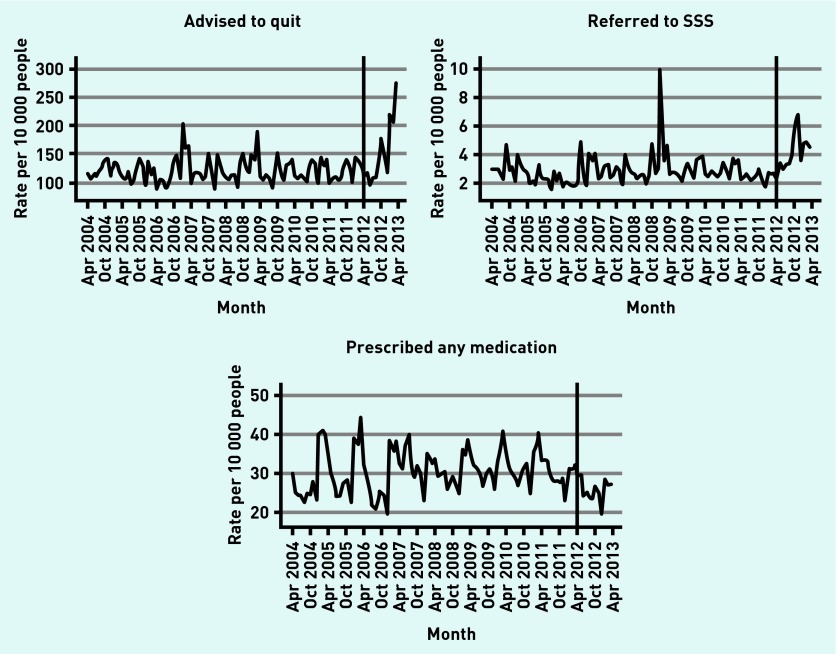
Figure 1 shows the monthly pattern of cessation activity per 10 000 registered patients over the study period. These graphs clearly show strong monthly variation in recording of advice to quit, referral to the NHS Stop Smoking Service, and prescribing of cessation medication.
Figure 1.
Monthly rates of recording of advice to quit, referral to the NHS Stop Smoking Service (SSS), and prescribing of smoking cessation medications.
Table 1 shows results from the ARIMA models indicating the percentage change in each outcome variable in the period after the QOF revision relative to the period beforehand, filtering out the underlying long-term and seasonal trends in each data series.
Table 1.
Percentage change in cessation activity after the 2012 QOF revisions relative to beforehand
| Outcome | Relative to the period April 2004 to March 2012 | Relative to the period April 2010 to March 2012 | ||
|---|---|---|---|---|
| % change (95% CI) | ARIMA model (pdq, PDQ) | % change (95% CI) | ARIMA model (pdq, PDQ) | |
| Record of cessation advice | 19.6 (7.9 to 31.4) P<0.001 |
(102, 100) | 18.9 (9.9 to 27.9) P<0.001 |
(000, 100) |
| Referral to the NHS Stop Smoking Service | 38.8 (15.2 to 62.4) P<0.001 |
(101, 100) | 38.1 (19.3 to 57.0) P<0.001 |
(100, 100) |
| Prescription for pharmacotherapy | −7.7 (−21.6 to 6.2) P= 0.280 |
(100, 100) | −13.8 (−21.0 to −6.5) P<0.001 |
(100, 100) |
ARIMA = autoregressive integrated moving average.
The present results show an increase in recording of both cessation advice and referral to the NHS Stop Smoking Service after the 2012 revision to the QOF, relative to both the longer and shorter reference periods beforehand.
Compared with the period April 2004 to March 2012, there was no significant change in the prescribing of cessation medications after the 2012 QOF revision. When the post-QOF period was compared with just the 2 years beforehand, however, there was a statistically significant 13.8% decrease in prescribing (95% CI = −21.0% to −6.5%).
DISCUSSION
Summary
The 2012 revision to the QOF required GPs for the first time to intervene with smokers without a smoking-related disease and to offer support and treatment rather than just advice to quit. This was associated with an increase in the rate of recording of cessation advice and referral to the NHS Stop Smoking Service. At best, however, there was no change in prescribing of smoking cessation medications, as, depending on the reference period used, prescribing may have declined after April 2012.
The 2012 change in the QOF had two clear targets. First, the aim was to reorient doctors away from advising patients to stop smoking and towards offering help to achieve this, in line with evidence that says offering help is more effective than advice and with the development of a national training programme to support health professionals to deliver very brief advice to quit.17,18 Second, it aimed at improving prevention by extending care to smokers who had yet to develop smoking-related conditions. The change in the QOF appears to have been partly successful in meeting both aims. The most striking finding of this research, however, is that smoking cessation advice, typically advice to stop smoking, was over 30 times more commonly recorded than referral for cessation support. At first sight, it may appear surprising that the QOF wording of offering support or treatment should lead to a rise in advice to stop smoking. This probably reflects how these QOF changes were implemented in practice, however. The Read Codes used are implemented in templates on GPs’ clinical systems. These templates offer drop-down lists of appropriate codes that will generate payment for the practice if selected. Thus, although the ‘headline’ text in the QOF changed to support and treatment and away from advice, the codes that GPs were able to use to receive payment included the code that they had used before the 2012 change. GPs could have felt little obvious imperative to change practice despite the headline change in QOF wording.
Strengths and limitations
The present findings are derived from an extremely large dataset that is representative of the UK population, and an analytical approach able to filter out underlying secular and seasonal trends. Although an ARIMA model is not able to distinguish between the effects of multiple policy changes occurring at the same time, and thus it is not possible to causally ascribe the changes in recording of advice and referral seen here to the revision of the QOF, to the best of the authors’ knowledge there were no other significant changes in tobacco control policy or primary care occurring close to April 2012 that might have caused more smokers to seek cessation advice or referral from primary care. Thus, it seems likely that the changes described are associated with the QOF revision.
There are some limitations with the routinely collected data analysed in this study. A recording that advice has been delivered tells us nothing about the quality of that advice, or indeed whether the patient interpreted it as a suggestion or instruction to quit smoking. On the other hand, smoking cessation may have been discussed in a consultation but not documented, although rates of recording of advice have previously been shown to exceed rates of patient recall of having received advice.19
In basing the present analysis on the adult population registered in THIN each month, potential changes in underlying smoking prevalence were not accounted for — an increase or decrease in prevalence may itself alter the volume of cessation activity recorded in primary care, confounding assessment of the impact of the QOF revision. The ability to identify smokers from their primary care records is not complete, however, and has changed over time.11 Previous work using THIN data has shown policy effect estimates to be similar when based on a denominator of all identified smokers compared with all patients,16 and this is likely to also be the case here. If anything, a decline in smoking prevalence may mean the relative change in the rate of recording of cessation advice and referral has been underestimated. For illustration only, the percentages of smokers receiving advice, referral, and a prescription were calculated assuming the prevalence of smoking was 20% during the period immediately before and after the 2012 change.20 Before the change, 6.3% of the population of people who smoked received advice to stop each month, rising to 7.5% after the change. Referrals increased from 0.15% to 0.21%, and prescribing decreased from 1.50% to 1.38%.
Comparison with existing literature
The present finding of an increase in referrals to the Stop Smoking Service is contrary to the decline in use of this service. NHS Stop Smoking Service monitoring data showed a decline in the number of smokers who receive their support to quit: 724 247 smokers set a quit date with the Service in England in 2012–2013, compared with 816 444 the previous year.21 If referrals to the Service from GPs are increasing, this might suggest that the overall decline is as a result of fewer smokers proactively seeking NHS support themselves.
What may appear surprising is that a greater number of conversations led either to no increase or even a decrease in prescribing pharmacotherapy. There are several possible explanations for this. Alternative prescribing systems, called Patient Group Directions (PGDs), mean that an increasing proportion of (non-medical) NHS cessation advisers can prescribe pharmacotherapy themselves. This would imply that use of cessation pharmacotherapy would have increased in line with apparent rises in other cessation activity. A repeated cross-sectional national survey in which people report using medication also shows a decline, however, in use of prescribed and non-prescribed medication over the same period.22 Data from this survey do, however, show a concurrent increase in the reported use of e-cigarettes, which began to gain in popularity in early 2012 and are now the most commonly used cessation aid in England. It is therefore possible that some of the decline in prescribing seen in the THIN data analysed here, particularly in the analysis of the restricted time series, may be the result of smokers substituting licensed pharmacotherapy for e-cigarettes in their attempts to quit. A recent study concluded, however, that increasing e-cigarette use is not associated with the reduction in the use of licensed NRTs, and might have grown the market for the use of nicotine products among current smokers.23
Implications for practice
Although the present data do not tell us whether cessation advice delivered to a patient is acted on, a referral is taken up, or a prescription is redeemed and used as intended, the apparent increase in the provision of cessation advice and referral could increase both the number of smokers making a quit attempt and their ultimate success in quitting. The overall impact of the QOF change appears to have been modest, however, and, although the change in wording was intended to alter practice towards more frequent offering of cessation support, this does not appear to have had entirely the desired effect. GPs probably would feel greater imperative to change their practice if the QOF business rules removed the Read Codes, which do not imply offering support and medication.
Acknowledgments
The authors thank Dr Yue Huang, University of Nottingham, for her help in extracting the THIN data.
Funding
Both authors are members of the UK Centre for Tobacco and Alcohol Studies, which receives core funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, and the Department of Health under the auspices of the UK Clinical Research Collaboration. No specific funding was received for this work.
Ethical approval
Ethical approval for use of the THIN data was obtained from the THIN scientific review committee (reference 13–037).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
Lisa Szatkowski has declared no competing interests. Paul Aveyard has done 1 day of consultancy for Pfizer on smoking cessation leading to payments to his institution and to him personally.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.World Health Organization . WHO report on the global tobacco epidemic: Enforcing bans on tobacco advertising, promotion and sponsorship. Geneva: WHO; 2013. [Google Scholar]
- 2.Stead LF, Buitrago D, Preciado N, et al. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2013;5:CD000165. doi: 10.1002/14651858.CD000165.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauld L, Bell K, McCullough L, et al. The effectiveness of NHS smoking cessation services: a systematic review. J Public Health (Oxf) 2010;32(1):71–82. doi: 10.1093/pubmed/fdp074. [DOI] [PubMed] [Google Scholar]
- 4.Stead LF, Perera R, Bullen C, et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2012;11:CD000146. doi: 10.1002/14651858.CD000146.pub4. [DOI] [PubMed] [Google Scholar]
- 5.Hughes JR, Stead LF, Hartmann-Boyce J, et al. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2014;1:CD000031. doi: 10.1002/14651858.CD000031.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev. 2012;4:CD006103. doi: 10.1002/14651858.CD006103.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Coleman T, Lewis S, Hubbard R, Smith C. Impact of contractual financial incentives on the ascertainment and management of smoking in primary care. Addiction. 2007;102(5):803–808. doi: 10.1111/j.1360-0443.2007.01766.x. [DOI] [PubMed] [Google Scholar]
- 8.Taggar JS, Coleman T, Lewis S, Szatkowski L. The impact of the Quality and Outcomes Framework (QOF) on the recording of smoking targets in primary care medical records: cross-sectional analyses from The Health Improvement Network (THIN) database. BMC Public Health. 2012;12:329. doi: 10.1186/1471-2458-12-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NHS Employers and British Medical Association . Quality and Outcomes Framework for 2012/13: guidance for PCOs and practices. London: NHS Employers; 2012. [Google Scholar]
- 10.CSD Medical Research THIN data — Statistics. http://csdmruk.cegedim.com/our-data/statistics.shtml (accessed 16 Nov 2015).
- 11.Szatkowski L, Lewis S, McNeill A, et al. Can data from primary care medical records be used to monitor national smoking prevalence? J Epidemiol Community Health. 2012;66(9):791–795. doi: 10.1136/jech.2010.120154. [DOI] [PubMed] [Google Scholar]
- 12.Langley TE, Szatkowski LC, Wythe S, Lewis SA. Can primary care data be used to monitor regional smoking prevalence? An analysis of The Health Improvement Network primary care data. BMC Public Health. 2011;11:773. doi: 10.1186/1471-2458-11-773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langley T, Szatkowski L, Gibson J, et al. Validation of The Health Improvement Network (THIN) primary care database for monitoring prescriptions for smoking cessation medications. Pharmacoepidemiol Drug Saf. 2010;19(6):586–590. doi: 10.1002/pds.1960. [DOI] [PubMed] [Google Scholar]
- 14.Health and Social Care Information Centre QOF business rules v300. http://www.hscic.gov.uk/qofbrv30 (accessed 16 Nov 2015). [Google Scholar]
- 15.Health and Social Care Information Centre Read codes. http://systems.hscic.gov.uk/data/uktc/readcodes (accessed 16 Nov 2015).
- 16.Szatkowski L, Coleman T, McNeill A, Lewis S. The impact of the introduction of smoke-free legislation on prescribing of stop-smoking medications in England. Addiction. 2011;106(10):1827–1834. doi: 10.1111/j.1360-0443.2011.03494.x. [DOI] [PubMed] [Google Scholar]
- 17.National Centre for Smoking Cessation and Training Very Brief Advice training module: a short training module on how to deliver Very Brief Advice on Smoking. http://www.ncsct.co.uk/publication_very-brief-advice.php (accessed 26 Nov 2015).
- 18.Aveyard P, Begh R, Parsons A, West R. Brief opportunistic smoking cessation interventions: a systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction. 2012;107(6):1066–1073. doi: 10.1111/j.1360-0443.2011.03770.x. [DOI] [PubMed] [Google Scholar]
- 19.Szatkowski L, McNeill A, Lewis S, Coleman T. A comparison of patient recall of smoking cessation advice with advice recorded in electronic medical records. BMC Public Health. 2011;11:291. doi: 10.1186/1471-2458-11-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.West R, Brown J. Latest trends on smoking in England from the Smoking Toolkit Study. http://www.smokinginengland.info/latest-statistics/ (accessed 16 Nov 2015).
- 21.Health and Social Care Information Centre . Statistics on NHS Stop Smoking Services: England, April 2012 to March 2013. London: Health and Social Care Information Centre; 2013. [Google Scholar]
- 22.West R, Brown J, Beard E. Electronic cigarettes in England — latest trends. http://www.smokinginengland.info/latest-statistics/ (accessed 16 Nov 2015). [Google Scholar]
- 23.Beard E, Brown J, McNeill A, et al. Has growth in electronic cigarette use by smokers been responsible for the decline in use of licensed nicotine products? Findings from repeated cross-sectional surveys. Thorax. 2015 doi: 10.1136/thoraxjnl-2015-206801. [DOI] [PMC free article] [PubMed] [Google Scholar]