Abstract
Objective
Living a purposeful life is associated with better mental and physical health, including longevity. Accumulating evidence shows that these associations might be explained by the association between life purpose and regulation of physiological systems involved in the stress response. The aim of this study was to investigate the prospective associations between life purpose and allostatic load over a 10-year period.
Methods
Analyses were conducted using data from the Midlife in the United States (MIDUS) survey. Assessment of life purpose, psychological covariates and demographics were obtained at baseline, while biomarkers of allostatic load were assessed at the 10-year follow-up.
Results
We found that greater life purpose predicted lower levels of allostatic load at follow-up, even when controlling for other aspects of psychological well-being potentially associated with allostatic load. Further, life purpose was also a strong predictor of individual differences in self-health locus of control—i.e., beliefs about how much influence individuals can exert on their own health—which, in turn, partially mediated the association between purpose and allostatic load. Although life purpose was also negatively linked to other-health locus of control —i.e., the extent to which individuals believe their health is controlled by others/chance —this association did not mediate the impact of life purpose on allostatic load.
Conclusion
The current study provides the first empirical evidence for the long-term physiological correlates of life purpose and supports the hypothesis that self-health locus of control acts as one proximal psychological mechanism through which life purpose may be linked to positive biological outcomes.
Keywords: Allostatic Load, Purpose in Life, Health Locus of Control
“There is nothing in the world, I venture to say, that so effectively helps one to survive even the worse conditions as the knowledge that there is a meaning in one’s life.”
Viktor Frankl, Man’s Search for Meaning
In the midst of the most dehumanizing and horrendous persecution in recent Western world history, psychiatrist Viktor Frankl, inmate at the Auschwitz concentration camp, finds what he deems the key to surviving the Holocaust: living a purposeful life. The link between life purpose (or simply purpose) and longevity is not new in the scientific literature. Plenty of evidence has shown that a greater purpose is associated with decreased mortality in both older [1] and younger adults [2] across different cultures [3]. Further, epidemiological studies have linked life purpose to lower incidence of certain diseases [4], improved cognitive aging [5] and better mental health [6]. Biological intermediaries of these relationships can be traced in the intertwined network of physiological regulatory systems responsible for the coordination of allostasis [7]. For instance, individuals reporting more life purpose have lower levels of chronic inflammation, including lower circulating levels of interleukin-6 (IL-6) [8] and soluble IL-6 receptor [9]. Similarly, purpose in life has been associated with healthier endocrine profiles [10], cardiovascular indicators (i.e. waist-to-hip ratio and high-density lipoprotein cholesterol), and restorative sleep [8].
Although within this line of work a few longitudinal studies have investigated the link between life purpose and morbidity [4], to our knowledge no prospective study has explored the potential biological pathways through which living a purposeful life impacts health over an extended period of time. Further, virtually all of the existing cross-sectional work has looked at only one aspect of physiology at a time (e.g., immune function) rather than considering different biological systems simultaneously, such as through the assessment of allostatic load [7]. This term refers to the cumulative multi-facetted physiological burden experienced by the body as a result of its attempt to repeatedly adjust to environmental challenges via allostasis. Allostasis, therefore, refers to the physiological change that the cardiovascular, autonomic, neuroendocrine, immune and metabolic systems simultaneously undergo in situations of stress. Too frequent, too sustained or inappropriate cycles of allostasis lead to a state of biological “frailty”, known as allostatic load, which is positively associated with greater risk of diseases, cognitive decline and mortality [11] [12] [13]. Framing the human stress response—and its modulation by psychological well-being—under the allostatic load model allows for a more integrated view of the link between stress and disease (morbidity and progression), away from looking at specific biomarkers in isolation. Thus, research on the long-term correlation between life purpose and allostatic load would represent an important advance for the field.
A second related gap in this emerging literature concerns the investigation of more proximal psychological mechanisms through which life purpose might be linked to long-lasting aspects on physiology. In other words, what set of health-related beliefs characterize people with a high sense of purpose compared to individuals with a low sense of purpose? Data from cross-sectional studies suggest that meaning in life is positively associated with health-promoting behaviors such as physical exercise, relaxation and preventive check-ups [14] [15]. Wells and colleagues [15], for example, found that women reporting a higher life purpose engaged in more frequent breast cancer screenings and self-examinations than women with a low life purpose.
Interestingly, these cross-sectional findings have been recently confirmed and extended by Kim and colleagues [16], who found, in a large sample of older adults, that purpose was associated with a higher likelihood to proactively use a variety of preventive health care services, suggesting that purpose heightens people’s motivation to take care of their health [16]. The compelling nature of these data raise the question about which psychological mechanisms are responsible for translating beliefs about purpose into observable behaviors. In other words, what beliefs about health might people with a high sense of purpose in life have that are different from people with a low sense of life purpose?
A viable hypothesis is that purpose directs beliefs about an individual’s sense of control over his/her own health. Thus, a key construct to consider is health locus of control, the set of convictions about how the self, others and fate have control over one’s health [17]. In this regard, a general distinction can be drawn between internal (or self, simply SHLC) and external (or others, simply OHLC) health locus of control. People with a strong SHLC feel in control of their health and therefore perceive themselves as the main agent responsible for the attainment of positive health outcomes. On the other hand, people with a more pronounced OHLC feel that others—especially “powerful others”, such as doctors— and chance are in control of their health. These dimensions are not necessarily orthogonal as multi-causation often characterizes individuals’ convictions about their health outcomes [18]. Generally, high SHLC has been found to predict healthy lifestyle practices ([19], including use of health care services [20], while high OHLC has been associated with less healthy behaviors [19], which probably explains its link with poor physical [21] and mental health [22]. The hypothesis that purpose in life might be, at least partially, associated with health via modulation of health-control beliefs awaits empirical testing.
Using data from the Midlife in the United States (MIDUS) survey, we investigated the prospective associations between life purpose and allostatic load over a 10-year period. In our initial analyses, we tested this association while controlling for age, gender, education (college education vs. high school or less) and ethnicity. Next, we repeated the same analyses while controlling for current purpose in life, as well as psychological variables indicated by previous studies as important covariates when investigating the link between purpose and health [23] [24] [2]. Lastly, we tested whether SHLC and OHLC measured concurrently with allostatic load (at Wave 2) mediated the associations between life purpose at baseline and allostatic load at follow-up.
Method
Data and Analytic Sample
Data are from a national sample of adults who participated in the Midlife in the United States (MIDUS) follow-up survey, a two-wave panel survey of English-speaking adults between the ages of 25 and 74 residing in the contiguous United States. Phone interviews and self-administered questionnaires were collected in 1995–1996 (Wave 1) and again in 2004–2006 (Wave 2). At Wave 2, a subset of individuals participated in the Biomarker Substudy (N=1054), wherein they provided samples for the assessment of various biomarkers. Additional details about the sampling procedure are described elsewhere [25]. People with missing values on any of the main variables included in this study were excluded, leaving a final sample of 985 adults (55.7% female, 94% White/Caucasian, 72.8% completed some college or more at baseline; age at baseline, M = 46.14 years, SD = 11.7 years) at MIDUS II who participated in a biomarker sub-study. Biomarker data were collected during an overnight visit at one of three regional medical centers (Washington, DC, Los Angeles, CA, and Madison, WI) between 2004 and 2009. Study participants provided a complete medical history, underwent a physical examination, and provided blood, urine, and saliva samples, along with cardiovascular and heart rate variability measurements. Fasting blood was collected at 07:00 h (before caffeine or nicotine consumption). Urine was collected during a 12-hr (19:00 h to 07:00 h) overnight stay [for details, see 26]. Data collection for the MIDUS and biomarker studies were approved by Institutional Review Boards at each participating site, and all participants provided informed consent.
Measures
Biomarker measurement
A comprehensive range of biological and anthropometric measurements representing seven physiological systems were collected during the study visit. Measures of (1) cardiovascular functioning included resting systolic and diastolic blood pressure (SBP, DBP) and resting pulse. Indicators of (2) lipid metabolism included high density lipoprotein (HDL) cholesterol, low density lipoprotein (LDL) cholesterol, triglycerides, body mass index (BMI), and waist-hip ratio (WHR). Levels of (3) glycosylated hemoglobin, fasting glucose, and the homeostasis model of insulin resistance (HOMA-IR), served as measures of glucose metabolism. Measures of (4) chronic inflammation included plasma C-reactive protein (CRP), fibrinogen, and serum measures of interleukin-6 (IL-6) and the soluble adhesion molecules e-Selectin and intracelleular adhesion molecule-1 (ICAM-1). Indicators of (5) sympathetic nervous system (SNS) activity included overnight urinary measures of epinephrine and norepinephrine. Measures of (6) parasympathetic nervous system (PNS) activity included the following heart rate variability parameters: low and high frequency spectral power, the standard deviation of R-R (heartbeat to heartbeat) intervals (SDRR), and the root mean square of successive differences (RMSSD). Indicators of (7) hypothalamic pituitary adrenal (HPA) axis activity included an overnight urinary measure of the hormone cortisol and a serum measure of the hormone dehydroepiandrosterone sulfate (DHEA-S). Additional details about laboratory assays and HRV measurement are available elsewhere [26, 27].
Allostatic load
An allostatic load (AL) score, designed to summarize dysregulation across multiple physiological systems, was computed as the sum of seven system-level (cardiovascular, lipid, glucose metabolism, inflammation, SNS, PNS, HPA) risk scores. Following previous work, system risk scores were computed as the average of individual biomarker indicators for each system for which participant values fell into high-risk quartile ranges [28]. High risk was defined as the upper or lower quartile depending on whether high or low values of the biomarker typically confer greater risk for poor health outcomes. System risk scores could range from 0 to 1 (indicating the percentage of system biomarkers in high-risk range for a given participant) and were computed for individuals with values on at least half of the system biomarkers. An AL score (possible range: 0–7) was computed for participants with information on at least six of the seven systems. Descriptive statistics are reported in Table 1, while Table 2 reports the zero-order correlations among risk scores for each physiological system and life purpose.
Table 1.
Descriptive statistics and high-risk cutpoint for biomarkers used to compute total allostatic load
| Descriptive variables | N | M | SD | High-risk cutpoint (≥) |
|---|---|---|---|---|
| Cardiovascular | ||||
| Resting SBP (mmHg) | 985 | 130.98 | 17.69 | 143.00 |
| Resting DBP (mmHg) | 985 | 74.96 | 10.20 | 82.00 |
| Resting hear rate (bpm) | 984 | 70.57 | 11.07 | 77.00 |
| Metabolic - lipids | ||||
| BMI | 985 | 29.10 | 5.91 | 32.31 |
| WHR | 984 | 0.89 | 0.10 | 0.97 |
| Triglycerides (mg/dL) | 983 | 130.12 | 79.03 | 160.00 |
| HDL Cholesterol (mg/dL) | 983 | 54.68 | 17.45 | 41.37 |
| LDL Cholesterol (mg/mL) | 983 | 106.59 | 35.13 | 128.00 |
| Metabolic - glucose metabolism | ||||
| Glycosylated hemoglobin (HbA1c) | 981 | 5.98 | 0.89 | 6.10 |
| Fasting glucose (mg/dL) | 980 | 100.04 | 21.58 | 105.00 |
| Insulin Resistance (HOMA-IR) | 979 | 3.29 | 3.49 | 4.05 |
| Inflammation | ||||
| IL-6 (pg/ml) | 985 | 2.78 | 2.79 | 3.18 |
| CRP (mg/L) | 980 | 2.68 | 3.95 | 3.18 |
| Fibrinogen (mg/dL) | 981 | 341.45 | 84.42 | 390.00 |
| sE-Selectin (ng/Mi) | 985 | 41.50 | 20.69 | 50.58 |
| sICAM-1 (ng/MI) | 985 | 286.18 | 99.79 | 329.65 |
| Sympathesic Nervous System | ||||
| Urine Epinephrine (ug/g creatine) | 969 | 2.04 | 1.29 | 2.54 |
| Urine Norepinephrine (ug/g creatine) | 975 | 27.79 | 13.11 | 33.33 |
| Hypothalamic Pituitary Adrean Axis | ||||
| Urine Cortisol (ug/g creatine) | 983 | 16.52 | 16.46 | 21.00 |
| Blood DHEA-s (ug/dL) | 981 | 106.15 | 76.23 | 51.00 |
| Parasympathetic Nervous System | ||||
| SDRR (msec) | 908 | 34.97 | 16.87 | 23.54 |
| RMSSD | 908 | 21.04 | 14.53 | 11.83 |
| Low frequency spectral power | 908 | 421.66 | 628.24 | 113.96 |
| High frequency spectral power | 908 | 245.58 | 403.73 | 54.16 |
| Allostaic load | 985 | 1.72 | 1.02 | |
Table 2.
Bivariate Correlations Between Allostatic load systems and purpose in life
| Descriptive variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Cardiovascular | 1 | 0.235** | 0.131** | 0.146** | 0.143** | 0.0 12 | 0.157** | 0.502** | −0.041 |
| 2. Metabolic - lipids | 1 | 0.358** | 0.244** | −0.098** | −0.14 1** | 0.091** | 0.437** | −0.116** | |
| 3. Metabolic - glucose metabolism | 1 | 0.265** | 0.056† | −0.0 27 | 0.203** | 0.58** | −0.058† | ||
| 4. Inflammation | 1 | 0.117** | −0.0 26 | 0.201** | 0.522** | −0.07* | |||
| 5. Sympathesic Nervous System | 1 | 0.13 ** | 0.101** | 0.471** | −0.027 | ||||
| 6. Hypothalamic Pituitary Adrean Axis | 1 | 0.045 | 0.307** | −0.018 | |||||
| 7. Parasympathetic Nervous System | 1 | 0.586** | −0.076* | ||||||
| 8. Allostatic load | 1 | −0.118** | |||||||
| 9. Purpose in life | 1 |
Note: Sample size ranged from 898 to 985,;
p < .10,
p < .05,
p < .01
Life purpose
Life purpose was assessed using three items from the Ryff Scales of Psychological Well-Being [29] and previous work on the MIDUS database used this scale [30] [2]. Each item, which is meaningfully linked to the conceptual definition of life purpose [29], was rated on a 7-point Likert scale ranging from “strongly agree” to “strongly disagree” and the overall life purpose index (α = .35) was computed by calculating the sum of the these values. Higher scores represent higher purpose (M = 17.21, SD = 3.23). Items included, “Some people wander aimlessly through life, but I am not one of them” (reversed); “I live life one day at a time and don’t really think about the future”; and “I sometimes feel as if I’ve done all there is to do in life”. The first item measures an individual’s sense of aims and direction, the second item is concerned with future orientation, and the third item relates to having compelling upcoming goals. As reported previously [30], the low alpha coefficients of this scale likely reflect the small number of items and the fact that these items were chosen to represent the conceptual breadth within the construct of life purpose rather than to maximize internal consistency. Ryff and Keyes [30] also reported that concurrent correlations between shortened versions and full versions of the well-being scales are high, ranging between .70 and .89. This further demonstrates that the low alpha coefficient is mainly a byproduct of the restricted number of items. Notably, this short version of the scale has been widely used in prior research over the last twenty years [31] [32] [33] [34] [35] [36] [37] [38] [39] [40] [41]. At Wave 2, purpose was assessed using the longer 7-item scale (M = 39.74, SD = 6.47, α = .69), which was not available for Wave 11. This variable was introduced to rule out the possibility that the effect of purpose at Wave 1 was actually due to purpose at Wave 2.
Health Locus of Control
SHLC and OHLC at Wave 2 were assed using six items adapted from Marmot et al.’s work [42] and used in previous work [43] [44]. Each item was rated on a 7-point Likert scale ranging from “strongly agree” to “strongly disagree” and the overall SHLC (four items, α = .71) and OHLC (two items, α = .30) were computed by calculating the mean of the these values. Items were recoded so that higher scores represent higher levels of SHLC (M = 6.2, SD = .77) or OHLC (M = 3.11, SD = 1.27). Example items for SHLC are “Keeping healthy depends on things that I can do” (SHLC) and “There are certain things I can do for myself to reduce the risk of a heart attack”. OHLC items included “When I am sick, getting better is in the doctor’s hand” and “It is difficult for me to get good medical care”.
Psychological Covariates
Following recent work by Hill and Turiano [2], who investigated the link between purpose and mortality using the MIDUS data, we included three psychological covariates measured at Wave 1 (positive affect, negative affect and positive relations with others) that have been shown to have shared variance with purpose in life and allostatic load.
For positive and negative affect [45], participants were asked to indicate on a Likert scale ranging from 1 (all of the time) to 5 (none of the time) to what extent they felt a specific emotional state (e.g., happy, nervous, satisfied) during the last thirty days. Each scale comprised six items and overall positive (α = .90) and negative (α = .85) affect were computed by calculating the mean of the item responses. Higher scores represent higher positive (M = 3.42, SD = .69) or negative (M = 1.49, SD = .56) affect.
Positive relation with others was assessed using three items from the Ryff Scales of Psychological Well-Being [29]. Each item was rated on a 7-point Likert scale ranging from “strongly agree” to “strongly disagree” and the overall positive relation with others index (α =.60) was computed by calculating the sum of the these values. Higher scores represent higher positive relations with others (M = 16.42, SD = 3.99). Items included, “Maintaining close relationships has been difficult and frustrating for me”; “People would describe me as a giving person, willing to share my time with others” (reversed); and “I have not experienced many warm and trusting relationships with others”.
Data Analysis
Ordinary least square regressions were run to test the association between life purpose and allostatic load, controlling for age only in Model 1, age and other demographic covariates in Model 2, and demographics and psychological covariates in Model 3. In Model 4, current (Wave 2) purpose in life was included. Next, a mediation analysis, using the bootstrapping approach [46] was run to test whether SHLC and OHLC mediated the hypothesized purpose/allostatic load link while controlling for demographic covariates. To facilitate interpretation, all predictors were standardized.
Results
As shown in Table 3 (Model 1)2, purpose at Wave 1 was inversely associated with allostatic load measured at Wave 2 (95% CI: −0.15383, −0.03217), indicating higher levels of allostatic load among those people who reported less purpose. Confirming previous findings [47] [28], allostatic load increased as a function of age (95% CI: 0.29313, 0.410837) (Model 1) and was higher for those people with low levels of educational attainment (95% CI: −.31437, −0.03963) (Model 2). Results for Model 3 suggest a minor reduction in the magnitude of the association between life purpose and allostatic load (95% CI: −0.15472, −0.02128) as well as with the addition of negative affect as a significant predictor of allostatic load (95% CI: 0.00450, 0.16150). Further, the association between purpose at Wave 1 and allostatic load remained significant (95% CI: −0.15468, −0.01732) when life purpose at Wave 2 was included as an additional covariate (95% CI: −0.07468, 0.06268) (Model 4). Notably, when purpose at Wave 2 was introduced in the model and purpose at Wave 1 was omitted, purpose at Wave 2 was not a significant predictor of allostatic load (b = −.030, SE = .034, p = .374).
Table 3.
Results of Models Predicting Allostatic Load From Life Purpose
| Predictor | Model 1
|
Model 2
|
Model 3
|
Model 4
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate (SE) | 95% CI | P | Estimate (SE) | 95% CI | P | Estimate (SE) | 95% CI | P | Estimate (SE) | 95% CI | P | |
| Life Purpose at Wave 1, β1 | −0.192 (.030) | [−0.16787, −0.05013] | <.001 | −0.093 (.031) | [−0.15383, −0.03217] | 0.003 | −0.085 (.034) | [−0.15472, −0.02128] | 0.01 | −0.086 (.035) | [−0.15468, −0.01732] | 0.015 |
| Age at baseline, β2 | 0.352 (.030) | [0.29313, 0.410837] | <.001 | 0.350 (.031) | [0.28917, 0.41083] | <.001 | 0.360 (.031) | [0.29917, 0.42083] | <.001 | 0.360 (.031) | [0.29917, 0.42083] | <.001 |
| Gender, β3 | --- | --- | --- | −0.017 (.061) | [−0.13671, 0.10271] | 0.78 | 0.058 (.063) | [−0.16667, 0.07667] | 0.472 | −0.044 (.062) | [−0.16567, 0.07767] | 0.479 |
| Ethnicity, β4 | --- | --- | --- | 0.157 (.128) | [−0.09419, 0.40819] | 0.221 | 0.162 (.128) | [−0.08919, 0.41319] | 0.206 | 0.163 (.129) | [−0.09015, 0.41615] | 0.204 |
| Education at baseline, β5 | --- | --- | --- | −0.177 (.070) | [−0.31437, −0.03963] | 0.011 | −0.175 (.070) | [−0.31237, −0.03763] | 0.012 | −0.174 (.070) | [−0.31137, −0.03663] | 0.013 |
| Positve affect, β6 | --- | --- | --- | --- | --- | --- | 0.008 (.040) | [−0.08650, 0.07050] | 0.842 | 0.007 (.041) | [−0.07246, 0.07346] | 0.859 |
| Negative affect, β7 | --- | --- | --- | --- | --- | --- | 0.083 (.040) | [0.00450, 0.16150] | 0.039 | 0.082 (.040) | [0.00350, 0.16050] | 0.041 |
| Positive relations with others, β8 | --- | --- | --- | --- | --- | --- | 0.054 (.036) | [−0.01665, 0.12465] | 0.137 | 0.055 (.037) | [−0.01761, 0.12761] | 0.135 |
| Life Purpose at Wave 2, β9 | --- | --- | --- | --- | --- | --- | --- | --- | --- | −0.006 (.035) | [−0.07468, 0.06268] | 0.857 |
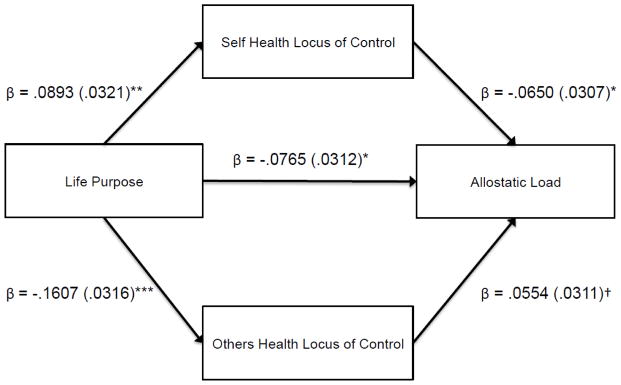
Next, we tested whether SHLC and OHLC, included simultaneously in the model, mediated the link between life purpose and allostatic load. The bootstrap analyses revealed a significant indirect effect of purpose on allostatic load via SHLC (95% CI: −0.0148, −0.0006), but not via OHLC (95% CI: −0.0223, 0.0002). Unstandardized regression coefficients and standard errors for the mediation model are reported in Figure 1. However, both SHLC and OHLC were significant mediators when separate models were run (SHLC, 95% CI: −0.0149, −0.0008; OHLC 95% CI: −0.0226, −0.0003).3
Figure 1.
Mediation paths linking life purpose and allostatic load via SHLC and OHLC. † <.10, * < .05, ** < .01, *** < .001.
Lastly, because the sample included a sibling subsample, we repeated the same analyses reported previously using generalized estimating equations (GEE) models in order to account for nested data. In all cases, results were unchanged.
Discussion
In a large sample of adults living in the U.S., we found that a greater sense of life purpose—the extent to which people report having meaning and direction in their life—predicted lower levels of allostatic load at a 10-year follow-up. This finding remained significant after controlling for demographic covariates (education, gender, age and ethnicity), other indicators of psychological well-being potentially associated with cumulative physiological costs (i.e. positive affect, negative affect, and positive relations with others), and life purpose measured at follow-up. Further, purpose was also a strong predictor of individual differences in both SHLC (i.e., the degree to which an individual believes he/she is in control of his/her own health) and OHLC (i.e., the degree to which an individual believes that others/chance are in control of his/her health), such that people reporting greater purpose scored higher on SHLC and lower on OHLC than people who appraised their life as having less purpose. Lastly, when considered together, SHLC—but not OHLC—was found to mediate the relationship between purpose and allostatic load. In other words, the inverse association between purpose and physiological strain was partially explained by the positive association between purpose and SHLC and the negative association between SHLC and allostatic load.
Previous work investigated the relationship between purpose and stress physiology cross-sectionally; this prior work only considered one biomarker at a time [9] rather than adopting the comprehensive framework of allostasis. To our knowledge, this is the first study that demonstrates that high levels of meaning in life are longitudinally associated with lower allostatic load. This finding is in line with previous work showing covariation between aspects of psychological well-being and long-term patterns of physiological activation [48] and, given the well-established link between allostatic load and mortality [11], it offers a strong biological foundation for the growing body of research showing greater longevity among those people reporting living a more purposeful life [1] [2]. Future waves of data will allow us to unequivocally test this hypothesis and articulate how purpose and physiological strain, assessed in multiple occasions, are linked to each other. This last point is particularly interesting, as our results showed that purpose at baseline was associated with future wear and tear of the body, while concurrent purpose was not a significant predictor of greater physiological costs. This finding suggests that the impact of purpose on allostatic load might occur over an extended period of time, similar to other studies showing prospective—but not concurrent—association between psychosocial factors and physiology [48]. A second, not mutually exclusive, explanation is that the benefits of purpose might dissipate over time and/or be more pronounced in some phases of adulthood compared to others [49], likely because of the decline in purpose from midlife to old age [50]. This possibility, however, should be considered with caution and only future data will allow us to empirically corroborate it.
Interestingly, the association between purpose and allostatic load remained significant after controlling for negative affect, which was also a significant (negative) predictor of physiological strain. This longitudinal finding extends previous cross-sectional work highlighting a positive association between negative emotionality and wear and tear of the body [23]. Further, our findings remained unchanged when we controlled for other aspects of psychological well-being previously shown to covary with both purpose and allostatic load (i.e., positive affect and positive relations with others) [24] [2]. This speaks to the robustness of our findings and the unique role played by purpose in regulating physiology, adding longitudinal evidence to those findings that showed, for example, how interrelated facets of well-being (i.e., eudaimonic and hedonic) affect health related to biological processes [51].
Lastly, our results shed some light on the potential psychological pathways through which purpose might be linked to allostatic load. Following the idea that having direction in life might lead people to feel more in charge of their health [14] [15] [16], we found that greater purpose was predictive of lower cumulative physiological cost partially via individual differences in SHLC, but, at least when considered together, not OHLC. In other words, individuals who reported having high levels of purpose also strongly believed in the ability to influence their health, which in turn explained low levels of allostatic load. Although the reverse pattern, which was of comparable effect size, was found for OHLC, it failed to reach statistical significance, at least when considering the two locus of control subdomains simultaneously. Previous work provides compelling evidence for the relationship between SHLC and health-promoting behaviors such as oral health, eating a healthy diet, exercise regularly, [19], and use of health care services [20], whereas individuals who score high OHLC tend to engage in less healthy behaviors [19]. This body of research complements our findings, providing a plausible explanation for the link between self-locus of control and allostatic load found in our study as well as previous work [52]. Knowing that individuals’ beliefs about perceived control over health act as a proximal psychological mechanism through which life purpose supposedly promotes healthful lifestyle practices has important practical implications. For example, intervention programs/therapies designed to improve psychological well-being [53]—and, concurrently, health outcomes—would benefit from intervening to directly enhance beliefs of purpose so as to potentially buffer individuals from the physiological costs of sustained allostasis.
Although the current work provides some of the first evidence of a longitudinal association between life purpose and allostatic load and a potential psychological pathway mediating this relationship, it is not without limitations. Unfortunately, some of the measures used in current study (e.g., OHLC) had low internal reliability. This problem likely arises from the use of a reduced number of items included on these scales, which is an acknowledged trade-off of large-scale studies such as MIDUS [30]. Second, although our study tested a prospective association between a dimension of well-being and a physiological outcome ten years later, the fact that no data for allostatic load were available at baseilne prevented us from ruling out that the reported association was not also present at Wave 1. Further, although we were not able to test whether life purpose at Wave 1 predicted changes in allostatic load from Wave 1 to Wave 2, it remains that current life purpose at Wave 2 was not associated with current allostatic load, suggesting that any consequences of life purpose on allostatic load accumulate over time. It is imporatnt to note that our use of the term “proximal mechanism” should be considered in light of the fact that SHLC and OHLC were measured at the same time of allostatic load, which does not allow a direct causal inference; thus, our results need to be complemented by future research that would experimentally/longitudinally test the meditational models here reported. Lastly, future research will benefit from investigating the meditational role of other health beliefs beyond health locus of control.
In conclusion, despite these limitations, we hope that the results of our study will stimulate further prospective research on the physiological consequences of purpose as well as other dimensions of psychological well-being and that such research will take into consideration its implications for health-related outcomes. In this regard, longitudinal studies employing large samples and multiple waves of data are ideal for testing the underlying biological mechanisms of links between psychosocial factors and physical health, including mortality.
Highlights.
Among 985 adults, greater life purpose predicted lower levels of allostatic load at the 10-year follow-up.
Life purpose was also a strong predictor of individual differences in self-health locus of control.
Life purpose was also a strong predictor of individual differences in other-health locus of control.
Self-health locus of control – but not other-health locus of control- mediated the effect of purpose on allostatic load.
Acknowledgments
Data collection was supported by the National Institute on Aging (Grant P01-AG020166).
Footnotes
Please note that results reported in the paper do not change when purpose in life at Wave 2 was calculated by summing the three items used to calculate purpose at Wave 1.
In an analogous model, each items of the purpose in life scale was introduced separately. Interestingly, all items were significant predictors: “I live life one day at a time and don’t really think about the future,” b = −.079, SE = .031, 95% CI = [−0.13983, −0.01817], p = .010; “I sometimes feel as if I’ve done all there is to do in life,” b = −.069, SE = .031, 95% CI = [−0.12983, −0.00817], p = .025; “Some people wander aimlessly through life, but I am not one of them,” (reversed) b = −.068, SE = .031, 95% CI = [−0.12983, −0.00817], p = .027.
Because the second item of the OHLC scale might not necessary tap into external health locus of control, we ran the same statistical models involving OHLC using only the first item. Both when OHLC was considered as the only predictor or simultaneously with SHLC, no evidence for a significant indirect effect emerged.
Conflict of Interest
None declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Samuele Zilioli, Department of Psychology, Wayne State University.
Richard B. Slatcher, Email: rich.slatcher@gmail.com, Department of Psychology, Wayne State University.
Anthony D. Ong, Email: ado4@cornell.edu, Department of Human Development, Cornell University.
Tara Gruenewald, Email: gruenewa@usc.edu, Davis School of Gerontology, University of Southern California.
References
- 1.Boyle PA, Barnes LL, Buchman AS, Bennett DA. Purpose in life is associated with mortality among community-dwelling older persons. Psychosom Med. 2009;71:574–9. doi: 10.1097/PSY.0b013e3181a5a7c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hill PL, Turiano NA. Purpose in Life as a Predictor of Mortality Across Adulthood. Psychol Sci. 2014 doi: 10.1177/0956797614531799. 0956797614531799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sone T, Nakaya N, Ohmori K, Shimazu T, Higashiguchi M, Kakizaki M, et al. Sense of life worth living (ikigai) and mortality in Japan: Ohsaki Study. Psychosom Med. 2008;70:709–15. doi: 10.1097/PSY.0b013e31817e7e64. [DOI] [PubMed] [Google Scholar]
- 4.Kim ES, Sun JK, Park N, Kubzansky LD, Peterson C. Purpose in life and reduced risk of myocardial infarction among older US adults with coronary heart disease: a two-year follow-up. J Behav Med. 2013;36:124–33. doi: 10.1007/s10865-012-9406-4. [DOI] [PubMed] [Google Scholar]
- 5.Boyle PA, Buchman AS, Barnes LL, Bennett DA. Effect of a purpose in life on risk of incident Alzheimer disease and mild cognitive impairment in community-dwelling older persons. Arch Gen Psychiatry. 2010;67:304–10. doi: 10.1001/archgenpsychiatry.2009.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simonelli LE, Fowler J, Maxwell GL, Andersen BL. Physical sequelae and depressive symptoms in gynecologic cancer survivors: meaning in life as a mediator. Ann Behav Med. 2008;35:275–84. doi: 10.1007/s12160-008-9029-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- 8.Ryff CD, Singer BH, Love GD. Positive health: Connecting well-being with biology. Philosophical Transactions-Royal Society of London Series B Biological Sciences. 2004:1383–94. doi: 10.1098/rstb.2004.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedman EM, Hayney M, Love GD, Singer BH, Ryff CD. Plasma interleukin-6 and soluble IL-6 receptors are associated with psychological well-being in aging women. Health Psychol. 2007;26:305. doi: 10.1037/0278-6133.26.3.305. [DOI] [PubMed] [Google Scholar]
- 10.Lindfors P, Lundberg U. Is low cortisol release an indicator of positive health? Stress Health. 2002;18:153–60. [Google Scholar]
- 11.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences. 2001;98:4770–5. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karlamangla AS, Singer BH, McEwen BS, Rowe JW, Seeman TE. Allostatic load as a predictor of functional decline: MacArthur studies of successful aging. J Clin Epidemiol. 2002;55:696–710. doi: 10.1016/s0895-4356(02)00399-2. [DOI] [PubMed] [Google Scholar]
- 13.Seeman TE, Crimmins E, Huang MH, Singer B, Bucur A, Gruenewald T, et al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc Sci Med. 2004;58:1985–97. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- 14.Holahan CK, Suzuki R. Motivational factors in health promoting behavior in later aging. Activities, Adaptation & Aging. 2006;30:47–60. [Google Scholar]
- 15.Wells JNB, Bush HA. Purpose-in-life and breast health behavior in Hispanic and Anglo women. J Holist Nurs. 2002;20:232–49. doi: 10.1177/089801010202000304. [DOI] [PubMed] [Google Scholar]
- 16.Kim ES, Strecher VJ, Ryff CD. Purpose in life and use of preventive health care services. Proceedings of the National Academy of Sciences. 2014;111:16331–6. doi: 10.1073/pnas.1414826111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wallston KA, Wallston BS, DeVellis R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ Behav. 1978;6:160–70. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
- 18.Levenson H. Activism and powerful others: Distinctions within the concept of internal-external control. J Person Assess. 1974;38:377–83. [Google Scholar]
- 19.Steptoe A, Wardle J. Locus of control and health behaviour revisited: a multivariate analysis of young adults from 18 countries. Br J Psychol. 2001;92:659–72. doi: 10.1348/000712601162400. [DOI] [PubMed] [Google Scholar]
- 20.Rennemark M, Holst G, Fagerstrom C, Halling A. Factors related to frequent usage of the primary healthcare services in old age: findings from The Swedish National Study on Aging and Care. Health & social care in the community. 2009;17:304–11. doi: 10.1111/j.1365-2524.2008.00829.x. [DOI] [PubMed] [Google Scholar]
- 21.van den Akker M, Buntinx F, Metsemakers JFM, Knottnerus JA. Marginal impact of psychosocial factors on multimorbidity: results of an explorative nested case-control study. Soc Sci Med. 2000;50:1679–93. doi: 10.1016/s0277-9536(99)00408-6. [DOI] [PubMed] [Google Scholar]
- 22.Bramston P, Tomasevic V. Health locus of control, depression and quality of life in people who are elderly. Australasian Journal on Ageing. 2001;20:192–5. [Google Scholar]
- 23.Kubzansky LD, Kawachi I, Sparrow D. Socioeconomic status, hostility, and risk factor clustering in the Normative Aging Study: any help from the concept of allostatic load? nn. Behav Med. 1999;21:330–8. doi: 10.1007/BF02895966. [DOI] [PubMed] [Google Scholar]
- 24.Seeman TE, Singer BH, Ryff CD, Love GD, Levy-Storms L. Social relationships, gender, and allostatic load across two age cohorts. Psychosom Med. 2002;64:395–406. doi: 10.1097/00006842-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Radler BT, Ryff CD. Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well-being. Journal of Aging and Health. 2010;22:307–31. doi: 10.1177/0898264309358617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Love GD, Seeman TE, Weinstein M, Ryff CD. Bioindicators in the MIDUS National Study: Protocol, measures, sample, and comparative context. Journal of Aging and Health. 2010;22:1059–80. doi: 10.1177/0898264310374355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crowley OV, McKinley PS, Burg MM, Schwartz JE, Ryff CD, Weinstein M, et al. The interactive effect of change in perceived stress and trait anxiety on vagal recovery from cognitive challenge. Int J Psychophysiol. 2011;82:225–32. doi: 10.1016/j.ijpsycho.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gruenewald TL, Karlamangla AS, Hu P, Stein-Merkin S, Crandall C, Koretz B, et al. History of socioeconomic disadvantage and allostatic load in later life. Soc Sci Med. 2012;74:75–83. doi: 10.1016/j.socscimed.2011.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069–81. [Google Scholar]
- 30.Ryff CD, Keyes CLM. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69:719–27. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- 31.Marks NF, Lambert JD. Marital status continuity and change among young and midlife adults longitudinal effects on psychological well-being. Journal of Family Issues. 1998;19:652–86. [Google Scholar]
- 32.Ryff CD, Keyes CLM, Hughes DL. Status inequalities, perceived discrimination, and eudaimonic well-being: do the challenges of minority life hone purpose and growth? J Health Soc Behav. 2003:275–91. [PubMed] [Google Scholar]
- 33.Greenfield EA, Marks NF. Formal volunteering as a protective factor for older adults’ psychological well-being. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2004;59:S258–S64. doi: 10.1093/geronb/59.5.s258. [DOI] [PubMed] [Google Scholar]
- 34.An JS, Cooney TM. Psychological well-being in mid to late life: The role of generativity development and parent–child relationships across the lifespan. International Journal of Behavioral Development. 2006;30:410–21. [Google Scholar]
- 35.Bierman A, Fazio EM, Milkie MA. A multifaceted approach to the mental health advantage of the married assessing how explanations vary by outcome measure and unmarried group. Journal of Family Issues. 2006;27:554–82. [Google Scholar]
- 36.Riggle EDB, Rostosky SS, Danner F. LGB identity and eudaimonic well being in midlife. J Homosex. 2009;56:786–98. doi: 10.1080/00918360903054277. [DOI] [PubMed] [Google Scholar]
- 37.Springer KW, Pudrovska T, Hauser RM. Does psychological well-being change with age? Longitudinal tests of age variations and further exploration of the multidimensionality of Ryff’s model of psychological well-being. Soc Sci Res. 2011;40:392–8. doi: 10.1016/j.ssresearch.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karasawa M, Curhan KB, Markus HR, Kitayama SS, Love GD, Radler BT, et al. Cultural perspectives on aging and well-being: A comparison of Japan and the United States. The International Journal of Aging and Human Development. 2011;73:73–98. doi: 10.2190/AG.73.1.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Keyes CLM, Simoes EJ. To flourish or not: Positive mental health and all-cause mortality. Am J Public Health. 2012;102:2164–72. doi: 10.2105/AJPH.2012.300918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Greenfield EA, Reyes L. Continuity and change in relationships with neighbors: Implications for psychological well-being in middle and later life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2014:gbu084. doi: 10.1093/geronb/gbu084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hill PL, Turiano NA. Purpose in Life as a Predictor of Mortality Across Adulthood. Psychol Sci. 2014;25:1482–6. doi: 10.1177/0956797614531799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marmot MG, Stansfeld S, Patel C, North F, Head J, White I, et al. Health inequalities among British civil servants: the Whitehall II study. The Lancet. 1991;337:1387–93. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- 43.Lachman ME, Weaver SL. Sociodemographic variations in the sense of control by domain: findings from the MacArthur studies of midlife. Psychol Aging. 1998;13:553–62. doi: 10.1037//0882-7974.13.4.553. [DOI] [PubMed] [Google Scholar]
- 44.Bobak M, Pikhart H, Rose R, Hertzman C, Marmot M. Socioeconomic factors, material inequalities, and perceived control in self-rated health: cross-sectional data from seven post-communist countries. Soc Sci Med. 2000;51:1343–50. doi: 10.1016/s0277-9536(00)00096-4. [DOI] [PubMed] [Google Scholar]
- 45.Mroczek DK, Kolarz CM. The effect of age on positive and negative affect: a developmental perspective on happiness. J Pers Soc Psychol. 1998;75:1333–49. doi: 10.1037//0022-3514.75.5.1333. [DOI] [PubMed] [Google Scholar]
- 46.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–91. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 47.Crimmins EM, Johnston M, Hayward M, Seeman T. Age differences in allostatic load: an index of physiological dysregulation. Exp Gerontol. 2003;38:731–4. doi: 10.1016/s0531-5565(03)00099-8. [DOI] [PubMed] [Google Scholar]
- 48.Slatcher RB, Selcuk E, Ong A. Partner Responsiveness Predicts Diurnal Cortisol Profiles 10. Years Later. Psychol Sci. 2015 doi: 10.1177/0956797615575022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hill PL, Burrow AL, Brandenberger JW, Lapsley DK, Quaranto JC. Collegiate purpose orientations and well-being in early and middle adulthood. Journal of Applied Developmental Psychology. 2010;31:173–9. [Google Scholar]
- 50.Ryff CD. Psychological well-being in adult life. Current directions in psychological science. 1995:99–104. [Google Scholar]
- 51.Steptoe A, Demakakos P, de Oliveira C, Wardle J. Distinctive biological correlates of positive psychological well-being in older men and women. Psychosom Med. 2012;74:501–8. doi: 10.1097/PSY.0b013e31824f82c8. [DOI] [PubMed] [Google Scholar]
- 52.Glei DA, Goldman N, Chuang YL, Weinstein M. Do chronic stressors lead to physiological dysregulation? Testing the theory of allostatic load. Psychosom Med. 2007;69:769–76. doi: 10.1097/PSY.0b013e318157cba6. [DOI] [PubMed] [Google Scholar]
- 53.Frankl VE. Man’s search for meaning. Simon and Schuster; 1985. [Google Scholar]