Abstract
Despite knowing that fruit and vegetable (FV) intake promotes health and well-being, few U.S. adults meet current guidelines. Thus, understanding people’s motivation for FV intake is important for predicting dietary behavior. Applying self-determination theory, the goal of this study was to examine the role of social support as a potential moderator of the link between autonomous and controlled motivations and FV intake. Cross-sectional data from 2,959 adults in the United States were analyzed. Autonomous motivation and perceived social support were positively associated with FV intake, while controlled motivation was negatively associated with FV intake. Additionally, there was evidence that the negative association between controlled motivation and FV intake was attenuated by higher levels of perceived social support. Findings suggest the need for a more comprehensive approach to understanding the role of motivation in health behaviors like FV intake and the potential roles played by friends and family in these motivational processes.
Keywords: fruit and vegetable intake, motivation, social support
A consistent body of research has emerged indicating that fruit and vegetable (FV) intake is associated with lower risk of several chronic conditions including cardiovascular disease, diabetes and cancer (Hung et al., 2004). The recommended intake of fruits and vegetables for adults is between 3.5 and 6.5 cups per day, depending on age, sex, and level of physical activity (US Department of Health and Human Services (USDHHS), 2010). However, despite these guidelines and the well-known evidence of health benefits of fruit and vegetables, the majority of adults in the United States do not consume the recommended amount (Grimm, Blanck, Scanlon, Moore, & Grummer-Strawn, 2010; Kimmons, Gillespie, Seymour, Serdula, & Blanck, 2009). Thus, research is needed to identify more proximal factors critical to promoting FV intake. One such variable is motivation (Shaikh, Yaroch, Nebeling, Yeh, & Resnicow, 2008).
Several theories have been developed to explain the nature and role of motivation in various health behaviors, including fruit and vegetable intake. For example, the transtheoretical model has been used to characterize readiness to change across a host of health behaviors (cf. Glanz & Bishop, 2010; Horwath, Nigg, Motl, Wong & Dishman, 2010). Other, more cognitive models, have addressed issues such as barriers to and facilitators of health behavior (cf. Belanger-Gravel, Godin, Vezina-Im, Amireault & Poirier, 2011; Spahn et al., 2010). More recently, researchers have begun to apply self-determination theory (SDT; Deci & Ryan, 2000; Ryan & Deci, 2000) to health behaviors, as well as health behavior change. SDT has shown particular promise for health behavior research. Evidence has emerged suggesting that the motivational components identified by the theory, and interventions based on this theory, yield not only behavior change initiation, but also long-term maintenance (Ng et al., 2012).
Self-Determination Theory
SDT: Conceptualizing Motivation
SDT defines motivation as psychological energy directed toward a goal. Consistent with the broader literature on motivation, SDT has distinguished between intrinsic motivation (i.e., engaging in a behavior because it is enjoyable and valuable in its own right) and extrinsic motivation (i.e., engaging in a behavior for some separable outcome). One unique aspect of SDT is the characterization of extrinsic motivation as a continuum that reflects the degree to which motivations are relatively internal to the self and concordant with other processes of one’s core self (Pelletier, Dion, Slovinec-D’Angelo, & Reid, 2004; Ryan & Connell, 1989). More autonomous forms of motivation include both intrinsic motivation as well as relatively more internalized forms of extrinsic motivation, often derived from sources like values and self-integration. In contrast, more controlled forms of motivation reflect a less internalized form of self-regulation, including engaging in a behavior to achieve social approval, to earn rewards, or to avoid self-inflicted feelings of guilt. Research has consistently demonstrated that the more autonomously-motivated individuals are toward a given behavior, the greater effort, engagement, and persistence the individual is likely to display in that behavior (Ryan & Deci, 2000).
Evidence for Autonomous and Controlled Motivation in Health Behaviors
The motivation continuum is particularly relevant to health behaviors. Although some health behaviors such as exercise may be engaged in for intrinsic reasons, most health behaviors are engaged for extrinsic reasons – i.e., they are engaged in for some separable outcome beyond the inherent enjoyment or value of the behavior in its own right. Thus, the extent to which motivation for health behaviors is more or less internal to the self has important implications for the likelihood that people will continue to engage in these behaviors over time. When a behavior is endorsed at a deep personal level, individuals find it easier to assume responsibility and feel accountable for that behavior (Teixeira, Patrick, & Mata, 2011).
A number of studies have assessed the relationship between autonomous motivation for eating regulation and healthy eating. In two survey studies by Pelletier and colleagues (2004; 2007), autonomous motivation was positively correlated with eating healthy foods, while controlled motivation for eating regulation was positively correlated with dysfunctional eating (e.g., bingeing). Furthermore, autonomous eating regulation was associated with being concerned with what one ate (i.e., dietary quality), whereas controlled eating regulation was associated with being concerned with how much one ate (Pelletier & Dion, 2007). Pelletier and Dion (2007) also found that healthy eating behaviors were associated with positive psychological adjustment (lower depressive symptoms, higher self-esteem, and life satisfaction scores), while dysfunctional eating behaviors were correlated with less positive psychological adjustment.
In line with these studies, Leong and colleagues (Leong, Madden, Gray, & Horwath, 2012) examined the associations between eating behavior regulation and Body Mass Index (BMI). They found that autonomous motivation for healthy eating was associated with lower BMI, while controlled motivation was associated with higher BMI, concluding that more autonomous motivation for eating behavior is likely to facilitate healthier food habits and, subsequently, lower BMI. Furthermore, frequency of binge eating was found to mediate the relationship between both autonomous and controlled regulation of eating behaviors and BMI. Thus, motivation for healthy eating was not only associated with an important health outcome – BMI – but also with an important behavioral precursor to BMI and other negative health outcomes – binge eating. In addition, Hagger and colleagues (Hagger, Chatzisarantis, & Harris, 2006) examined the relationship between autonomous motivation for dieting and eating behaviors. They found that autonomous motivation for dieting predicted a positive attitude toward dieting and greater perceived control over eating behaviors. Finally, in the context of fruit and vegetable (FV) intake, Trudeau and colleagues (Trudeau, Kristal, Li, & Patterson, 1998) found that autonomous motivation for eating a healthful diet was positively associated with FV consumption, while controlled motives were not. Likewise, Shaikh et al. (2008) reviewed psychosocial predictors of FV intake and found evidence that autonomous motivation was positively associated with FV intake. Autonomous motivation is also an important correlate of FV intake because it is malleable via interventions. For example, among participants who initially reported low autonomous motivation, an intervention containing motivational interviewing had significant effects on FV intake that were partially explained by increases in autonomous motivation (Shaikh, Vinkour, Yaroch, Williams, & Resnicow, 2011). Collectively, these studies demonstrate the importance of studying and promoting autonomous motivation for FV intake.
SDT: Psychological Needs and the Role of the Social Context in Motivation
An important tenet of SDT involves the role of the social context in supporting (or thwarting) autonomous motivation and the process of internalization (Patrick & Williams, 2012). SDT posits that there are three basic psychological needs necessary for optimal growth and development: autonomy (i.e., the need to feel volitional, as the originator of one’s actions); competence (i.e., the need to feel capable of achieving desired outcomes); and relatedness (i.e., the need to feel connected to and understood by important others). Support of these three needs has been associated with autonomous motivation and the internalization of extrinsic motivation (Ryan & Deci, 2000).
Psychological need support has been operationalized as consisting of a number of critical elements, including: offering and respecting choices, giving a meaningful explanation for recommended courses of action (e.g., health behavior change), avoiding controlling language and guilt, and refraining from use of performance-contingent rewards and punishments (Ryan, 1995; Ryan & Deci, 2000). In short, social contexts that support basic psychological needs are characterized as establishing a sense of unconditional positive regard (i.e., relatedness support), providing an opportunity for patients, clients, and research subjects to explore reasons both for and against behavior change so that they can come to their own conclusions (i.e., autonomy support), and addressing barriers to desired behavior change, including reframing failures in terms of steps toward success (i.e., competence support).
The strongest evidence for the role of psychological need support in facilitating autonomous motivation for health behavior has come from emerging intervention research in a variety of domains, including tobacco cessation (Williams et al., 2006), oral health (Halvari & Halvari, 2006), and physical activity (Fortier, Sweet, O’Sullivan, & Williams, 2007). Most germane to the current study is research that has focused on targeting diet and physical activity in the context of a weight loss intervention. In a longitudinal randomized controlled trial, Silva and colleagues (2011) evaluated predictors of successful long-term weight control. They analyzed the extent to which psychological need support provided by intervention staff predicted more autonomous motivation for lifestyle behaviors (i.e., diet, physical activity) and long-term weight loss in overweight and obese women. The study showed that the degree to which participants experienced psychological need support significantly predicted autonomous motivation for physical activity one year after the intervention ended, which was in turn associated with weight loss maintenance 2 years after the intervention was terminated.
Additional analyses from this same study examined whether autonomous motivation for physical activity resulted in motivational “spill-over” for another health behavior: eating regulation (Mata et al., 2009). Researchers were interested in the added synergistic effects of changing both eating and exercise behaviors, rather than either one alone. Results confirmed that increasing exercise-specific motivation (as a function of providing a need-supportive intervention context) contributed to improved eating behavior. Their findings suggest that moving from less to more autonomous motivation may not happen in isolation, but rather may apply to various health domains simultaneously. Together, these results provide strong evidence for psychological need support as a mechanism responsible for influencing autonomous motivation, which in turn affects long-term behavior change and maintenance.
From Psychological Need Support to Broader Social Support
As described above, SDT posits that more autonomous forms of motivation are likely to emerge based upon the extent to which psychological needs are met. The social context framed by psychological needs is a precursor to optimal motivation. However, there are many circumstances in which people are functioning in less autonomous ways. Perhaps the social context does not provide the necessary psychological supports for autonomous motivation, or a specific behavior or goal is difficult to find as inherently enjoyable or valuable in its own right (i.e., more controlled). Therefore, an understanding of other characteristics of individuals or social contexts that may mitigate the negative effects of being less autonomously motivated is important. Perceived social support is one candidate variable to consider.
Social support has been defined as the availability of a network of family and friends for information, encouragement, emotional support, and enhancing the environment to support a behavior (Spahn et al., 2010). Extensive literature has documented the importance of social support in a range of health outcomes, and has found that perceiving social support resources to be generally available can be particularly beneficial for health (Uchino, 2009). An emerging literature has begun to examine the role of social support in health behaviors. For example, studies have found social support to be positively associated with: smoking cessation (Sobell, Sobell, & Leo, 2000), diabetic management and compliance (McDonald, Wykle, Misra, Suwannaroop, & Burant, 2002), and is one of the strongest psychosocial correlates of adult FV intake (Shaikh et al., 2008). Brug (2008) summarized the results of recent systematic reviews on the association between environmental factors and healthy nutrition behaviors and concluded that the social environment (specifically social support and modeling) appeared to have a more consistent influence on nutrition behaviors than the physical environment. In another study, researchers found social support and norms related to healthy eating to be positively correlated with total fruit and vegetable intake as well as 100% fruit juice intake (Van Duyn et al., 2001). Taken together, these studies show that perceived social support is an important variable to consider in health behaviors, particularly FV intake.
Traditionally, research has examined the role of social support in people coping with difficult, even traumatic, situations (e.g., a health diagnosis, or work or academic challenge). Consistent with the stress and coping literature, social support is often conceptualized as most beneficial as a buffer in contexts that are unfavorable, stressful, or not ideal (Lazarus & Folkman, 1984). However, research on social support among general (healthy) adult populations is understudied but important (Uchino, 2009). Being motivated in less autonomous ways – whether one is less autonomously motivated because the social context has not met one’s basic psychological needs or because one is engaging in the behavior for some separable outcome – is a less than optimal form of motivation and one such circumstance in which social support may be especially beneficial.
The Current Study
This study examines the role of perceived social support as a potential moderator of the link between motivation (i.e., autonomous and controlled) and fruit and vegetable (FV) intake. Consistent with prior research, we hypothesized that autonomous motivation (H1a) and perceived social support (H1b) would be positively correlated with FV intake, while controlled motivation (H1c) would be negatively associated with FV intake, if at all. Further, we hypothesized that social support would moderate the association between motivation and FV intake. Specifically, we expected that social support would enhance the positive association of autonomous motivation (H2a) and buffer the negative association of controlled motivation (H2b), for FV intake.
Method
Participants and Procedures
The current study used data from the US National Cancer Institute’s Food Attitudes and Behavior (FAB) Survey (National Cancer Institute (NCI), 2009). The FAB Survey assessed correlates of fruit and vegetable intake among US adults ages 18 years and older. Participants were selected from the Synovate Consumer Opinion Panels using stratified random sampling. The FAB survey was mailed to 5,803 potential participants, with an oversampling of African Americans; 3418 surveys were returned, yielding a response rate of 59%. These participants were mailed a $5 incentive and thank you letter for completing the survey. The FAB survey was administered between September and December, 2007. The institutional review boards of the NCI and Westat approved the study. The final FAB survey sample consisted of 3,397 adults of whom 2,187 were Non-Hispanic white, 834 were African-American, and 291 categorized themselves as “other” race/ethnicities (i.e., Hispanic, Asian, American Indian/Alaskan Native, etc.). Eighty-five adults did not report their race.
Measures
The current analyses utilize FAB survey data on demographics, FV intake, and three psychosocial measures (autonomous motivation, controlled motivation, and perceived social support). Psychosocial constructs in FAB were informed by a literature review identifying correlates of FV intake (Shaikh et al., 2008) and ultimately represented constructs from multiple theoretical frameworks (Erinosho et al., 2015). Psychosocial items were tested and refined through cognitive interviewing and pilot testing procedures, and greater detail on the development of FAB survey items is discussed elsewhere (Erinosho et al., 2015).
Demographics
Demographic characteristics of participants included sex, age, race/ethnicity, and highest level of education completed.
Autonomous and controlled motivation
Autonomous and controlled motivation were measured using a modified version of the Treatment Self-Regulation Questionnaire for fruit and vegetable intake (Resnicow et al., 2008). The items begin with the stem, “A reason I eat fruits and vegetables is….”. Participants reported the extent to which each of 19 statements is true for them, using a 5-point Likert scale ranging from “not true at all” (1) to “very true” (5). Sample autonomous items include, “Because I personally believe it is a good thing for my health”, and “Because I want to take responsibility for my own health”. Sample controlled items include “Because I want others to approve of me”, and “Because I don’t want to let others down”. Motivation subscale scores were calculated by averaging autonomous (11 items) and controlled (7) items, respectively. One of the controlled motivation items had a low factor loading and was not included in the scale (Erinosho et al., 2015). Internal reliabilities (i.e., Cronbach’s α) were satisfactory and consistent with previous research: .93 for autonomous and .70 for controlled in this study. One item assessed amotivation for FV intake and was not included in these analyses.
FV intake
FV intake was assessed using a 16-item fruit and vegetable screener that was modified from the NCI’s Fruit and Vegetable screener (NCI, 2009; Thompson et al., 2002) and validated using multiple 24-hour dietary recalls. The items specifically assessed fruit and vegetable intake during the past month and consisted of eight items: one item assessed fruit consumption, one item assessed 100% fruit juice consumption, and six items assessed vegetable consumption. For each of these FV items, respondents indicated both 1) the frequency of consumption (in ten categories ranging from “never” to “5 times per day”) and 2) the portion size consumed at a time (in four categories for each item). Frequency and portion size responses were converted into Pyramid servings as defined by the 1992 dietary guidance (National Cancer Institute (NCI), 2009). One pyramid serving was defined as, for example, ¾ cup of juice, 1 cup leafy greens, and ½ cup of fruit, other potatoes, other vegetables, and tomato sauce. Total fruit and vegetable intake of participants was calculated as the sum of all items on the screener, excluding fried potatoes.
Perceived social support
Perceived social support was operationalized as the availability of a network of family and friends who provide information, encourage, and enhance the environment to support a specific behavior (Spahn et al., 2010) and was assessed using 3 items: “My family or friends encourage me to eat fruits and vegetables”, “My family or friends remind me not to eat junk food”, and “My family or friends would say something to me if they saw I was not eating fruits and vegetables”. Responses were on a 5-point Likert-type scale, ranging from “strongly disagree” (1) to “strongly agree” (5). Two additional items had low factor loadings and were dropped from the scale (Erinosho et al., 2015). The three items were averaged to form the perceived social support score, and internal reliability (Cronbach’s α) was .68.
Statistical Methods
All statistical analyses were conducted using SPSS v. 18 (SPSS, Chicago, IL). The data were weighted by sex, race, age, education and annual household income based on the 2000 US Census data. Descriptive statistics were calculated to characterize sample demographics. Partial correlations determined the unique association between motivation variables (i.e., autonomous and controlled motivation), perceived social support and FV intake, controlling for demographic variables and the other motivation subscale scores (e.g., partial correlations for autonomous motivation statistically controlling for demographics and controlled motivation). To test the moderating role of perceived social support in the association between motivation and FV intake, a hierarchical linear regression was conducted. In the first step, demographic variables (race/ethnicity, age, gender and highest level of education) were entered, as well as autonomous motivation, controlled motivation, and perceived social support. In the second step, the product terms for the interactions between autonomous motivation and perceived social support and between controlled motivation and perceived social support were entered. Statistical significance was evaluated at the p < 0.05 (two-tailed) level.
Results
In the FAB sample, the mean daily cups of fruits and vegetables was 3.41 (SD = 3.82). Participants who did not respond to the variables of interest (i.e., perceived social support, autonomous and controlled motivation, fruit and vegetable intake) were excluded from further analyses, resulting in a final sample of 2,959. Between 1% and 3% of participants were missing responses for each item contributing to these scales. Demographic information about the sample is provided in Table 1. As shown, 59% of the participants were female, 41% were between 35 and 54 years old, 67% were Non-Hispanic white, and 31% had some college education but did not have a college degree.
Table 1.
Sample Demographics
| Demographic Characteristic | N (%) |
|---|---|
| Total Sample | 2,959 (100.0) |
| Race/Ethnicity | |
| White, European-American | 1977 (66.8) |
| Black, African-American | 723 (24.4) |
| Hispanic/Latino | 115 (3.9) |
| Asian, Asian-American | 46 (1.6) |
| American Indian/Native American | 18 (0.6) |
| Hawaiian/Pacific Islander | 4 (0.1) |
| Other, Mixed race/ethnicity | 76 (2.6) |
| Highest Level of Education | |
| Less than a High School (HS) degree | 338 (11.4) |
| HS degree | 884 (29.9) |
| Some college, but not a college degree | 905 (30.6) |
| 4-year college degree or higher | 832 (28.1) |
| Age | |
| 18–34 years | 870 (29.4) |
| 35–54 years | 1205 (40.7) |
| 55 or older | 884 (29.9) |
| Gender | |
| Female | 1759 (59.4) |
| Male | 1200 (59.4) |
Tests of Hypotheses
We hypothesized that autonomous motivation (H1a) and perceived social support (H1b) would be positively correlated with FV intake, while controlled motivation would be negatively associated with FV intake, if at all (H1c). In order to test these hypotheses, partial correlations (pr) were calculated between motivation quality variables (i.e., autonomous and controlled), perceived social support, and FV intake, controlling for demographic variables (as well as the other motivation quality variable). The results support the directions of our proposed hypotheses, such that autonomous motivation was positively associated with FV intake (pr = .32, p < .01), as was perceived social support (pr = .04, p < .05), and controlled motivation was negatively associated with FV intake (pr = −.14, p < .01).
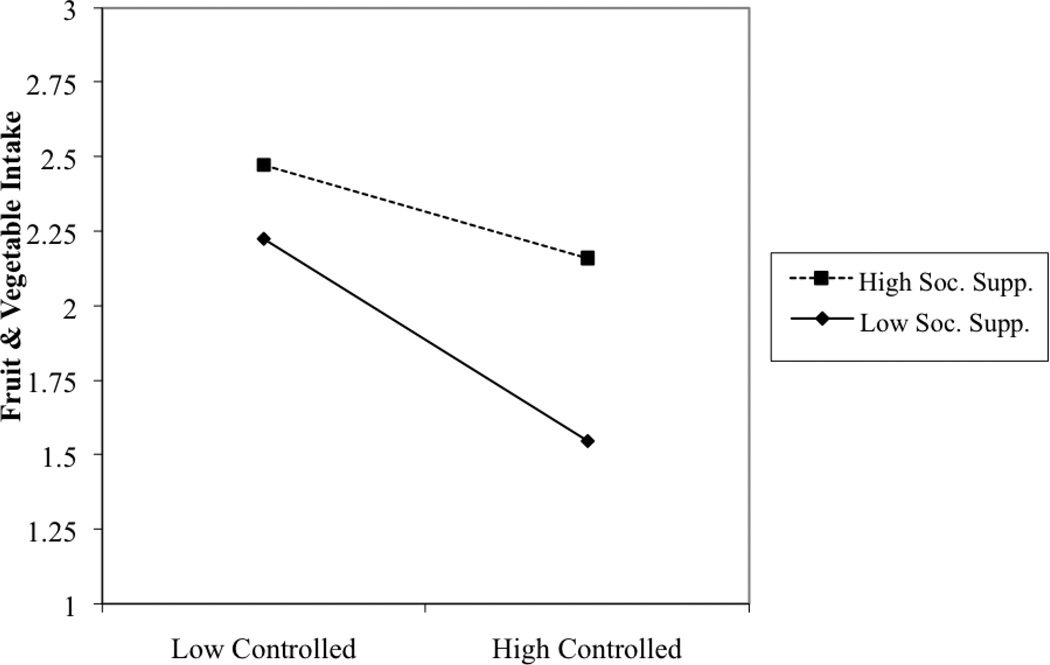
We also hypothesized that perceived social support would moderate the relationship between autonomous motivation (H2a), controlled motivation (H2b) and FV intake. Table 2 presents results for the hierarchical regression analyses testing these hypotheses. As shown, and in support of H2b, perceived social support moderated the association between controlled motivation and FV intake. We selected data points for estimating regression lines at ±1 SD for predictors of the equation (Aiken & West, 1991). Figure 1 provides simple regression lines of FV intake as a function of controlled motivation at high and low perceived social support. As shown, tests of simple slopes revealed that the association between controlled motivation and FV intake was statistically significant among those who perceived low social support (t = −2.16, p < .05), but not among those who perceived high social support (p =.61). Thus, perceived social support buffered the effect of controlled motivation on FV intake. The interaction term for autonomous motivation and social support predicting FV intake was not statistically significant, contrary to H2a.
Table 2.
Hierarchical regression analyses testing the moderating effect of social support on FV intake
| B | SE B | β | |
|---|---|---|---|
| Main effects model | |||
| Gender | .02 | .04 | .01 |
| Age | .06 | .03 | .04* |
| Race/ethnicity | .03 | .02 | .03 |
| Highest level of education | .03 | .02 | .03 |
| Perceived social support | .04 | .02 | .04* |
| Autonomous motivation | .55 | .03 | .42*** |
| Controlled motivation | −.20 | .02 | −.19*** |
| Tests of interactions | |||
| Gender | .02 | .04 | .01 |
| Age | .05 | .03 | .04* |
| Race/ethnicity | .03 | .02 | .03 |
| Highest level of education | .03 | .02 | .03 |
| Perceived social support | −.06 | .07 | −.79 |
| Autonomous motivation | .70 | .07 | .53*** |
| Controlled motivation | −.46 | .07 | −.45*** |
| Autonomous motivation X Perceived social support | −.05 | .03 | −.21 |
| Controlled motivation X Perceived social support | .08 | .02 | .41*** |
p < .05
p < .001
Figure 1.
Controlled motivation X Social support interaction predicting FV intake.
Discussion
The purpose of this study was to examine the associations of autonomous motivation, controlled motivation, and perceived social support with FV intake, as well as the role of perceived social support as a potential moderator of the associations between motivation and FV intake. An emerging literature has demonstrated a positive association between autonomous motivation and healthier eating behaviors (including fruit and vegetable intake) and the importance of psychological need support in facilitating autonomous motivation for a variety of behaviors. However, less research has focused on the potential role of more general forms of perceived social support for health behaviors in these associations. Although social support from close others can support the SDT-defined psychological needs of autonomy, competence and relatedness, social support more generally exists in multiple forms and can affect behavior and well-being through several pathways (Feeney & Collins, 2015).
Results regarding the association between autonomous motivation and FV intake (H1a), social support and FV intake (H1b), and controlled motivation and FV intake (H1c) were consistent with hypotheses and the broader SDT and social support literatures. Additionally, there was evidence for the moderating role of perceived social support on the association between controlled motivation and FV intake, such that the negative association between controlled motivation and FV intake was attenuated by perceiving greater social support. There was not a statistically significant interaction between autonomous motivation and perceived social support in predicting FV intake. Thus, perceived social support appears to play a particularly significant role in the context of controlled motivation for fruit and vegetable intake. Perceived social support may be a less relevant moderator of autonomous motivation because of the sense of personal ownership and endorsement that is engendered by autonomous motivation for a health behavior, in this case FV intake. People who are autonomously motivated to eat fruits and vegetables may gain fewer benefits from broad social support from family and friends if their specific psychological needs are already met. In contrast, individuals whose motivation is more controlled might require additional behavior-specific social support as encouragement to enact a behavior and may be particularly likely to benefit from the broader experience of perceived social support from family and friends.
Implications
Findings from this study contribute to the literature in several important ways. First, although there is a large literature assessing the role of autonomous and controlled motivation in health behaviors broadly, particularly physical activity (Ryan, Frederick-Recascino, Lepes, Rubio, & Sheldon, 1997; Ryan, Williams, Patrick, & Deci, 2009); few studies have addressed motivation with regard to specific eating behaviors like FV intake (Shaikh et al., 2008; Trudeau et al., 1998). FV intake impacts a variety of chronic conditions and health outcomes (USDHHS), 2010); and engaging in healthy eating behaviors, such as consuming greater amounts of fruit and vegetables, can yield long-term positive health benefits. Thus, understanding the role of motivation on this behavior has important public health implications. Further, this is one of the only studies to date to examine the role of broad social support constructs (that is, behavioral support that is not specific to a psychological need) in the context of self-determined motivation and a specific health behavior.
Although the SDT literature has an impressive body of evidence for the role of psychological need support in internalization and autonomous motivation, very little research has focused on potential moderators of the associations between motivation and health behaviors. Perceived social support from family and friends may be an important potential moderator for several reasons. Aside from studies of close relationships which have largely focused on relationship quality – rather than health – outcomes, most of the SDT literature on need support in health has examined the role of psychological need support coming from health “authority figures” such as physicians, health coaches, dentists, and physical activity counselors (Patrick & Williams, 2012; Ryan, Patrick, Deci, & Williams, 2008). Although these individuals play important roles in the adoption and maintenance of a range of health behaviors, people have more frequent interactions with their social networks, including friends and family. Prior research suggests that family and friends can be important sources of psychological need support. For example, perceiving more family and friends to be autonomy supportive may result in increasingly beneficial outcomes (Ratelle, Simard, & Guay, 2012). Further, another study demonstrated that autonomy support from one’s close social network may facilitate weight loss (Power, Koestner, & Gorin, 2008). Perceiving general social support from important others may attenuate the negative effects of approaching health behaviors in more controlled ways as a function of having one’s psychological needs thwarted. Thus, these findings provide initial evidence that could inform the SDT, social support and health behavior literatures. The findings can also potentially inform a more comprehensive approach to understanding the role of motivation in health behaviors and the potential multiple roles played by friends and family members in these motivational processes. Theoretical directions for future study include examining how general perceived social support for FV intake corresponds to more specific psychological need support and which features of social support attenuate negative effects of controlled motivation. Recent physical activity research suggests that perceived social support is related to satisfaction in the areas of autonomy, competence, and relatedness (George et al., 2013). However, research incorporating both SDT and broader social support perspectives should investigate whether there are any limits on social support as an effective moderator. For example, receiving social support that is closely aligned with one’s needs will likely be most influential (Uchino, 2009). In contrast, it is possible that specific types of social support could be perceived as controlling or directive and thus could reduce some of the positive effect seen in the current analysis (Gorin et al., 2014; Ng, Ntoumanis, & Thorgersen-Ntoumani, 2014).
This study also has implications for preventive interventions incorporating social support. One suggestion is that people who report controlled motivation for FV intake would particularly benefit from interventions designed to bolster effective social support for fruit and vegetable consumption. Suggested strategies for promoting social support are numerous. One possibility is to engage existing social networks (including family and friends) to more effectively provide social support, while other strategies include: connecting individuals to new socially-supportive groups, and supporting individuals’ own perceptions and abilities to seek and receive social support (Uchino, 2009; Heaney & Israel, 2008). In a recent systematic review, socially supportive intervention components were found to contribute to effective interventions for weight loss (Greaves et al., 2011), and the presence of supportive others may be particularly helpful when they are also efficacious in the context of weight loss (Gorin et al., 2005). However, further work is needed to clarify the effectiveness of social supportive interventions specifically for FV intake and how social support interventions may be particularly targeted at contexts in which psychological need support is insufficient.
Limitations and Strengths
This study is not without limitations. The FAB sample was drawn from a consumer opinion panel rather than from the U.S. population. However, this method of participant recruitment has been used in other nutrition and health studies such as the Styles Survey (Blanck et al., 2009). Furthermore, the FAB sample was selected so that households recruited from the consumer opinion panel were similar to the U.S. population in terms of age, household income, geographic region, population density, and household size (Erinosho, Moser, Oh, Nebeling, & Yaroch, 2012; Erinosho et al., 2015). This study was correlational and cross-sectional, such that causality and directionality of the associations remains unclear. Longitudinal and experimental studies are needed to better understand the role of social support in both the initiation and maintenance of behavior change and how social support and motivation act in conjunction with important correlates of FV intake from broader levels of influence, such as public health messaging and FV access and availability. Although the findings regarding social support were clear and consistent, a more refined measure may have helped to further clarify the role of perceived social support in the association between motivation variables and FV intake. Specifically, the measure used in this study combined family and friends rather than asking questions separately for separate relational contexts. As these individuals may provide different forms of support, having separate items for friends and family would be useful. Furthermore, this survey did not include additional measures of support for psychological needs that are central to SDT (i.e., autonomy, competence, relatedness). Data on these measures would be helpful in clarifying the role of general perceived social support. Finally, although the brief 16-item fruit and vegetable screener is practical for large studies, it may not provide the most precise indicator of total fruit and vegetable intake (e.g., 24 hour recalls).
Despite these limitations, this study has many strengths, including the use of a large national sample of US adults, reflecting demographic characteristics of the US population and an oversampling of African-Americans. Data on psychosocial variables like motivation and social support on health behaviors in such a large sample of adults are uncommon (Shaikh et al., 2008). Yet, this type of data are important for providing information about naturally occurring motivation and social support experiences at population levels. Individuals who enroll in clinical trials and interventions tend to be highly motivated and thus it is important to understand how motivation functions with more diverse and larger samples. The findings also contribute to the literature by providing additional evidence for the role of autonomous and controlled motivation in a specific eating behavior – FV intake – and by introducing the role of perceived social support as a potential moderator of the associations between motivation and FV intake.
Conclusions
This study expanded on prior studies of motivational and social support influences on eating behaviors by examining their interactive associations with FV intake. Controlled motivation was associated with lower consumption of fruits and vegetables among individuals who perceived low levels of social support; this association was attenuated among people reporting high perceived social support. These findings suggest that interventions might benefit from encouraging individuals reporting controlled motivation to utilize their social networks to obtain social support for their FV intake. The current study also provides useful theoretical insights that general social support from family and friends and motivation should be jointly considered in efforts to understand and promote FV intake among US adults.
Highlights.
Self-determination theory emphasizes the role of motivation for health behaviors.
Motivation and social support were associated with fruit and vegetable intake (FV).
Social support attenuated the association between controlled motivation and FV.
Findings suggest a role of social support for health motivations and behaviors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications; 1991. [Google Scholar]
- Belanger-Gravel A, Godin G, Vezina-Im LA, Amireault S, Poirier P. The effect of theory-based interventions on physical activity participation among overweight/obese individuals: A systematic review. Obesity Reviews. 2011;12:430–439. doi: 10.1111/j.1467-789X.2010.00729.x. [DOI] [PubMed] [Google Scholar]
- Blanck HM, Yaroch AL, Atienza AA, Yi SL, Zhang J, Masse LC. Factors influencing lunchtime food choices among working Americans. Health Education and Behavior. 2009;36:289–301. doi: 10.1177/1090198107303308. [DOI] [PubMed] [Google Scholar]
- Brug J. Determinants of healthy eating: Motivation, abilities and environmental opportunities. Family Practice. 2008;25 doi: 10.1093/fampra/cmn063. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. The “what” and the “why” of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry. 2000;11:227–268. [Google Scholar]
- Erinosho TO, Moser RP, Oh AY, Nebeling LC, Yaroch AL. Awareness of the Fruits and Veggies-More Matters campaign, knowledge of the fruit and vegetable recommendation, and fruit and vegetable intake of adults in the 2007 Food Attitudes and Behaviors (FAB) Survey. Appetite. 2012;59:155–160. doi: 10.1016/j.appet.2012.04.010. [DOI] [PubMed] [Google Scholar]
- Erinosho TO, Pinard CA, Nebeling LC, Moser RP, Shaikh AR, Resnicow K, Oh AY, Yaroch AL. Development and implementation of the National Cancer Institute’s Food Attitudes and Behaviors Survey to assess correlates of fruit and vegetable intake in adults. PLoS One. 2015;10:0115017. doi: 10.1371/journal.pone.0115017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeney BC, Collins NL. A new look at social support: A theoretical perspective on thriving through relationships. Personality and Social Psychology Review. 2015;19:113–147. doi: 10.1177/1088868314544222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortier MS, Sweet SN, O’Sullivan TL, Williams GC. A self-determination process model of physical activity adoption in the context of a randomized controlled trial. Psychology of Sport and Exercise. 2007;8:741–757. [Google Scholar]
- George M, Eys MA, Oddson B, Roy-Charland A, Schinke RJ, Bruner MW. The role of self-determination in the relationship between social support and physical activity intentions. Journal of Applied Social Psychology. 2013;43:1333–1341. [Google Scholar]
- Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- Gorin A, Phelan S, Tate D, Sherwood N, Jeffery R, Wing R. Involving support partners in obesity treatment. Journal of Consulting and Clinical Psychology. 2005;73:341–343. doi: 10.1037/0022-006X.73.2.341. [DOI] [PubMed] [Google Scholar]
- Gorin AA, Powers TA, Koestner R, Wing RR, Raynor HA. Autonomy support, self-regulation, and weight loss. Health Psychology. 2014;22:332–339. doi: 10.1037/a0032586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greaves CJ, Sheppard KE, Abraham C, Hardeman W, Roden M, Evans PH, Schwarz P, The IMAGE Study Group Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119. doi: 10.1186/1471-2458-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm KA, Scanlon KS, Moore LV, Grummer-Strawn LM. State-specific trends in fruit and vegetable consumption among adults. United States, 2000-2009. Morbidity and Mortality Weekly Report. 2010;59:1125–1130. [PubMed] [Google Scholar]
- Hagger MS, Chatzisarantis NLD, Harris J. From psychological need satisfaction to intentional behavior: Testing a motivational sequence in two behavioral contexts. Personality and Social Psychology Bulletin. 2006;32:131–148. doi: 10.1177/0146167205279905. [DOI] [PubMed] [Google Scholar]
- Halvari AEM, Halvari H. Motivational predictors of change in oral health: An experimental test of self-determination theory. Motivation and Emotion. 2006;30:294–305. [Google Scholar]
- Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. San Francisco, CA: Jossey Bass; 2008. pp. 189–210. [Google Scholar]
- Horwath CC, Nigg CR, Motl RW, Wong KT, Dishman RK. Investigating fruit and vegetable consumption using the transtheoretical model. American Journal of Health Promotion. 2010;24:324–333. doi: 10.4278/ajhp.071218138. [DOI] [PubMed] [Google Scholar]
- Hung H-C, Joshipura KJ, Jiang R, Hu FB, Hunter D, Smith-Warner SA, Willett WC. Fruit and vegetable intake and risk of major chronic disease. Journal of the National Cancer Institute. 2004;96:1577–1584. doi: 10.1093/jnci/djh296. [DOI] [PubMed] [Google Scholar]
- Kimmons J, Gillespie C, Seymour J, Serdula M, Blanck HM. Fruit and vegetable intake among adolescents and adults in the United States: Percentage meeting individualized recommendations. Medscape Journal of Medicine. 2009;11:26–36. [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Leong SL, Madden C, Gray A, Horwath C. Self-determined, autonomous regulation of eating behavior is related to lower body mass index in a nationwide survey of middle-aged women. Journal of the Academy of Nutrition and Dietetics. 2012;112:1337–1346. doi: 10.1016/j.jand.2012.04.018. [DOI] [PubMed] [Google Scholar]
- Mata J, Silva MN, Vieira PN, Carraca EV, Andrade AM, Coutinho SR, Teixeira PJ. Motivational “spill-over” during weight control: Increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychology. 2009;28:709–716. doi: 10.1037/a0016764. [DOI] [PubMed] [Google Scholar]
- McDonald PE, Wykle ML, Misra R, Suwonnaroop N, Burant CJ. Predictors of social support, acceptance, health promoting behaviors, and glycemic control in African-Americans with type 2 diabetes. Journal of the National Black Nurses’ Association. 2002;13:23–30. [PubMed] [Google Scholar]
- National Cancer Institute (NCI) [Accessibility verified February 11, 2015];Food Attitudes and Behaviors (FAB) Survey: Health Behaviors Research Branch. 2009 http://cancercontrol.cancer.gov/brp/fab/index.html.
- Ng JYY, Ntoumanis N, Thørgersen-Ntoumani C. Autonomy support and control in weight management: What important others do and say matters. British Journal of Health Psychology. 2014;19:540–552. doi: 10.1111/bjhp.12054. [DOI] [PubMed] [Google Scholar]
- Ng JYY, Ntoumanis N, Thørgersen-Ntoumani C, Deci EL, Ryan RM, Duda JL, Williams GC. Self-determination theory applied to health contexts: A meta-analysis. Perspectives on Psychological Science. 2012;7:325–340. doi: 10.1177/1745691612447309. [DOI] [PubMed] [Google Scholar]
- Patrick H, Williams GC. Self-determination theory: Its application to health behavior and complementarity with motivational interviewing. International Journal of Behavioral Nutrition and Physical Activity. 2012;9:18. doi: 10.1186/1479-5868-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelletier LG, Dion SC, Slovinec-D’Angelo M, Reid R. Why do you regulate what you eat? Relationships between forms of regulation, eating behaviors, sustained dietary behavior change, and psychological adjustment. Motivation and Emotion. 2004;28:245–277. [Google Scholar]
- Pelletier LG, Dion SC. An examination of general and specific motivational mechanisms for the relations between body dissatisfaction and eating behaviors. Journal of Social and Clinical Psychology. 2007;26:303–333. [Google Scholar]
- Powers TA, Koestner R, Gorin AA. Autonomy support from family and friends and weight loss in college women. Families, Systems, & Health. 2008;26:404–416. [Google Scholar]
- Ratelle CF, Simard K, Guay F. University students’ subjective well-being: The role of autonomy support from parents, friends, and the romantic partner. Journal of Happiness Studies. 2013;14:893–910. [Google Scholar]
- Resnicow K, Davis RE, Zhang G, Konkel J, Strecher VJ, Shaikh AR, Wiese C. Tailoring a fruit and vegetable intervention on novel motivational constructs: Results of a randomized study. Annals of Behavioral Med. 2008;35:159–169. doi: 10.1007/s12160-008-9028-9. [DOI] [PubMed] [Google Scholar]
- Ryan RM. Psychological needs and the facilitation of integrative processes. Journal of Personality. 1995;63:397–427. doi: 10.1111/j.1467-6494.1995.tb00501.x. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Connell JP. Perceived locus of causality and internalization: Examining reasons for acting in two domains. Journal of Personality and Social Psychology. 1989;57:749–761. doi: 10.1037//0022-3514.57.5.749. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Frederick CM, Lepes D, Rubio N, Sheldon KM. Intrinsic motivation and exercise adherence. International Journal of Sport Psychology. 1997;28:335–354. [Google Scholar]
- Ryan RM, Patrick H, Deci EL, Williams GC. Facilitating health behaviour change and its maintenance: Interventions based on self-determination theory. The European Health Psychologist. 2008;10:2–5. [Google Scholar]
- Ryan RM, Williams GC, Patrick H, Deci EL. Self-determination theory and physical activity: The dynamics of motivation in development and wellness. Hellenic Journal of Psychology. 2009;6:107–124. [Google Scholar]
- Shaikh AR, Yaroch AL, Nebeling L, Yeh M, Resnicow K. Psychosocial predictors of fruit and vegetable consumption in adults: A review of the literature. American Journal of Preventive Medicine. 2008;34:535–543. doi: 10.1016/j.amepre.2007.12.028. [DOI] [PubMed] [Google Scholar]
- Shaikh AR, Vinokur AD, Yaroch AL, Williams GC, Resnicow K. Direct and mediated effects of two theoretically based interventions to increase consumption of fruits and vegetables in the Healthy Body Healthy Spirit trial. Health Education & Behavior. 2011;38:492–501. doi: 10.1177/1090198110384468. [DOI] [PubMed] [Google Scholar]
- Silva MN, Markland D, Carraca EV, Vieira PN, Coutinho SR, Minderico CS, Teixeira PJ. Exercise autonomous motivation predicts 3-yr weight loss in women. Medicine and Science in Sports and Exercise. 2011;43:728–737. doi: 10.1249/MSS.0b013e3181f3818f. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Leo GI. Does enhanced social support improve outcomes for problem drinkers in guided self-change treatment? Journal of Behavior Therapy and Experimental Psychiatry. 2000;31:41–54. doi: 10.1016/s0005-7916(00)00007-0. [DOI] [PubMed] [Google Scholar]
- Spahn JM, Reeves RS, Keim KS, Laquatra I, Kellogg M, Jortberg B, Clark NA. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. Journal of the American Dietetic Association. 2010;110:879–891. doi: 10.1016/j.jada.2010.03.021. [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Patrick H, Mata J. Why we eat what we eat: The role of autonomous motivation in eating behavior regulation. Nutrition Bulletin. 2011;36:102–107. [Google Scholar]
- Thompson FE, Subar AF, Smith AF, Midthune D, Radimer KL, Kahle LL, Kipnis V. Fruit and vegetable assessment: Performance of 2 new short instruments and a food frequency questionnaire. Journal of the American Dietetic Association. 2002;102:1764–1772. doi: 10.1016/s0002-8223(02)90379-2. [DOI] [PubMed] [Google Scholar]
- Trudeau E, Kristal AR, Li S, Patterson RE. Demographic and psychosocial predictors of fruit and vegetable intakes differ: Implications for dietary interventions. Journal of the American Dietetic Association. 1998;98:1412–1417. doi: 10.1016/S0002-8223(98)00319-8. [DOI] [PubMed] [Google Scholar]
- Uchino BN. Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspectives on Psychological Science. 2009;4:236–255. doi: 10.1111/j.1745-6924.2009.01122.x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS), US Department of Agriculture. [Accessibility verified February 11, 2015];Dietary Guidelines for Americans, 2010. 2010 Retrieved from http://www.health.gov/dietaryguidelines/dga2010/DietaryGuidelines2010.pdf.
- Van Duyn MA, Kristal AR, Dodd K, Campbell MK, Subar AF, Stables G, Glanz K. Association of awareness, intrapersonal and interpersonal factors, and stage of dietary change with fruit and vegetable consumption: A national survey. American Journal of Health Promotion. 2001;16:69–78. doi: 10.4278/0890-1171-16.2.69. [DOI] [PubMed] [Google Scholar]
- Williams GC, McGregor HA, Sharp D, Levesque C, Kouides RW, Ryan RM, Deci EL. Testing a self-determination theory intervention for motivating tobacco cessation: Supporting autonomy and competence in a clinical trial. Health Psychology. 2006;25:91–101. doi: 10.1037/0278-6133.25.1.91. [DOI] [PubMed] [Google Scholar]