Abstract
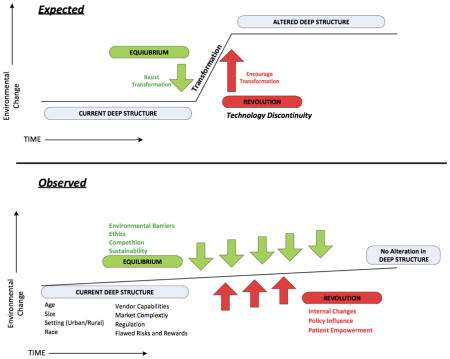
Healthcare is in a period significant transformational activity through the accelerated adoption of healthcare technologies, new reimbursement systems that emphasize shared savings and care coordination, and the common place use of mobile technologies by patients, providers, and others. The complexity of healthcare creates barriers to transformational activity and has the potential to inhibit the desired paths towards change envisioned by policymakers. Methods for understanding how change is occurring within this complex environment are important to the evaluation of delivery system reform and the role of technology in healthcare transformation. This study examines the use on an integrative review methodology to evaluate the healthcare literature for evidence of technology transformation in healthcare. The methodology integrates the evaluation of a broad set of literature with an established evaluative framework to develop a more complete understanding of a particular topic. We applied this methodology and the framework of punctuated equilibrium (PEq) to the analysis of the healthcare literature from 2004 – 2012 for evidence of technology transformation, a time during which technology was at the forefront of healthcare policy. The analysis demonstrated that the established PEq framework applied to the literature showed considerable potential for evaluating the progress of policies that encourage healthcare transformation. Significant inhibitors to change were identified through the integrative review and categorized into ten themes that describe the resistant structure of healthcare delivery: variations in the environment; market complexity; regulations; flawed risks and rewards; change theories; barriers; ethical considerations; competition and sustainability; environmental elements, and internal elements. We hypothesize that the resistant nature of the healthcare system described by this study creates barriers to the direct consumer involvement and engagement necessary for transformational change. Future policies should be directed at removing these barriers by demanding and emphasizing open technologies and unrestricted access to data versus as currently prescribed by technology vendors, practitioners, and policies that perpetuate market equilibrium.
Keywords: Integrative Review, Information Technology, Health Reform, Complex Adaptive Systems, Technology Transformation
Graphical abstract
1. Introduction
The United States receives a poor return on its healthcare dollars. Costs remain higher than any other industrialized country while low measures of patient care quality and care efficiencies persist [1–3]. There is a clear need both to improve quality and to reduce healthcare costs. Recent legislative efforts to address these issues all contain a significant emphasis on improving the use of health information technology (HIT) and enhancing value in healthcare. Since 2009, over $30 billion dollars has been spent to address these identified deficiencies through the incentivized adoption and use of HIT and new payment models [4–6]. Health reform legislation, has mandated and propelled new health care delivery models that are highly dependent on HIT, including accountable care organizations, medical homes, bundled payments, and other value based payment structures [7]. Market transformation from these policies is expected to occur through incremental acceptance of new technologies and growing adoption of new care delivery models [8, 9].
Healthcare’s multiple payer-provider relationships, multiple delivery models, the significant knowledge gap between patients and providers, and the intricacies of health behaviors and medicine itself converge to create a highly complex system. Complexity science describes complex systems as adaptive, with change emerging from the many goals and priorities of the individual agents within the system and environment itself [10–13]. These many interactions make outcomes and behavior hard to predict and traditional linear models cannot take into account the multiple relationships contributing to change within the system [14]. As a result the more complex the system becomes, the more resistant it is to change and transformation [15]. Since no individual agent has the ability to change the system, the system experiences slow incremental change until a clear superior alternative emerges [14]. To overcome this resistance, transformation may demand radical changes in the underlying structure or environment of the system and does not generally occur incrementally over time [15–17]. These periods of short radical change are the foundation of Gersick’s theory of punctuated equilibrium (PEq) [18, 19]. Punctuated equilibrium represents a pattern of transformational change that has been demonstrated in biological, organizational, and complex market settings. In each case long periods of incremental change are separated by short radical transformational periods.
Given the complexity of the healthcare system and a desire to encourage transformation, there is a need to understand how change is occurring within this complex environment. Understanding the role of government, health information technologies, health systems and patients is important to the evaluation of delivery system reform and the goal of healthcare transformation. This study describes the use on an integrative review methodology combined with the validated transformational framework of PEq to develop a more complete understanding of the potential barriers and challenges necessary to transform healthcare given its complex non-linear behavior. Complexity science describes the need to identify patterns of change when evaluating complex systems [20]. PEq was selected as it describes an identifiable pattern of change observable within complex environments. Our proposed method described here attempts to look for this observable pattern using the literature as evidence. We hope to demonstrate that the conclusions reached through such a method are uniquely beneficial to future policy discussions and as a measure of transformational change within the healthcare market.
2. Methods
2.1 Integrative Review
The integrative review methodology outlined by Whittemore and Knafl adopted for this study encompasses the following activities: literature search, data evaluation/reduction, data comparison/synthesis, and presentation [21]. The integrative review draws strength from evaluating an extensive set of primary sources emphasizing inclusion and diversity over consistency of study design. By increasing the breadth and number of data sources a more comprehensive understanding of the topic is achieved. The method is further enhanced the by use of an evaluative or theoretical framework to interpret the broad set of data identified within the review. In this case, the application of PEq theory provides the structure to evaluate the progress of healthcare transformation.
2.2 Theoretical Framework
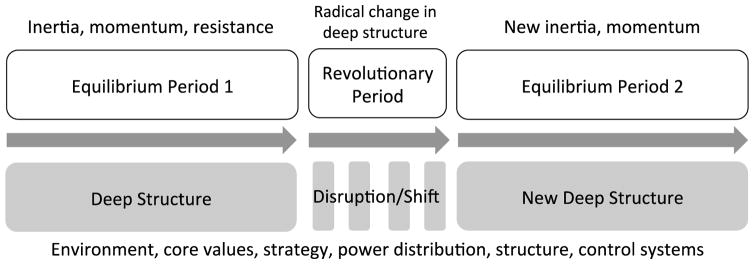
The theory of PEq defines three distinct components of market transformation guided by PEq, periods of deep structure, equilibrium, and revolution (Figure 1). Deep structure describes the existing market environment that includes the markets core values and beliefs; strategies; allocation of resources; structure; and controls. These periods are stable in that the choices and patterns exhibited often reinforce themselves as part of “mutual feedback loops.” [19].
Figure 1.
Representation of three components of Gersick’s theory of punctuated equilibrium - deep structure, equilibrium period and revolutionary period.
Equilibrium describes the influences of investments, processes, and structure that reinforce the underlying deep structure, allowing for only gradual and incremental change over time. During periods of equilibrium, complex systems make incremental adjustments based on the existing environment maintaining a level of inertia that is resistant to major change. This inertia often occurs due to blindness to new ideas that do not fit within on organization’s or system’s existing paradigm or a basic fear of change that could result in a loss of market dominance [19].
Revolutionary periods represent radical changes in the deep structure of the environment or system that results from disruptions in the relationships, values, and controls defining deep structure. Revolutionary changes in deep structure result from two basic causes; (1) internal changes that challenge the alignment of relationships, values and/or controls that define the existing environment; and/or (2) environmental changes that limit the ability of the system to maintain its current structure. Changes in political climate, new consumer demands, and/or new technological innovations are often characteristic of these periods of revolution [22].
Tushman and Romenelli describe periods of deep structure in the context of the political and economic environment, proposing five elements that impact deep structure; core values and beliefs, strategy, power distribution, structure, and control systems [23]. Gersick refers to these elements collectively as the “design of the playing field and the rules of the game” [19]. These descriptive elements were used in this review as part of the evaluative framework for deep structure within the healthcare system.
2.3 Literature Search
Multiple search strategies were applied to obtain sources for review. Five electronic databases were searched: MEDLINE/PubMed, Business Source Complete, Social Science Research Network, Web of Knowledge, and Factiva. The Web of Knowledge data base was used for an ancestry search on three foundational articles: Gersick’s 1991 synthesis of change models into the PEq model; Anderson and Tushman’s 1990 review and development of the Technology Cycle of transformation; and Tushman and Romenelli’s paper on organizational evolution and inertia in organizational systems [19, 23, 24]. Factiva was a source relevant news articles in the popular press including newspapers, magazines, and media transcripts.
Search terms encompassed multiple meanings for “technology” and “transformation” using key words, and free text related to the PEq framework. Inclusion criteria were articles written in the English language with a publication date between January 2004 and April 2012. The 2004 date was selected as it coincides with creation of the Office of the National Coordinator for Health Information Technology [25]. The specific search strategies are included in Appendix A.
2.4 Data Evaluation and Reduction
The title and abstract of each information source (i.e. publication) retrieved were assessed for inclusion using four criteria: 1) addressed implementation, delivery, or adoption of health information technology (diagnostic and therapeutic technologies such as CT scanning techniques, DNA sequencing, and others were excluded); 2) focused on change, adoption, acquisition, transformation, implementation, resistance, or the outcomes of new technology; 3) described at least one of the three components of Gersick’s PEq model (deep structure, equilibrium, and/or revolution); and 4) were set in the United States. Two content experts examined a random sample of 50 abstracts to evaluate consistent application of the inclusion criteria and a Cohen’s Kappa value was calculated. Each abstract that met the inclusion criteria was subjected to a second full-text review using the same inclusion criteria. Sources still satisfying the inclusion criteria after the second review were retained for coding and analysis.
Each source was coded for methodological rigor and relevance to the topic of technology transformation (see Table 1). Descriptive, evaluative, and interpretive data were extracted from each information source and coded based on a uniform classification schema (See Table 2). Descriptive data included publication date, study design, technology addressed, stakeholder, population, industry, and setting. Evaluative data included the specific component of punctuated equilibrium (deep structure, equilibrium, revolution) and interpretive data further describing this component. Interpretive data included linkages between PEq components, influencers, costs, culture, time, precipitators, followers, strengths and weaknesses. These interpretive elements reflect principles of PEq described in the theoretical literature [19, 23, 24]. Similar to the inclusion criteria, a random sample of 50 full-text sources was coded by two external reviewers and compared for consistency of coding and interpretation. Weighted Cohen’s Kappa’s were used for the ordinal rigor and relevance scales by placing a greater error value for scores that were farther apart [26]. All data was maintained in a Microsoft Access© database. A summary of the coding for each included source is contained in Appendix B.
Table 1.
Definitions of rigor and relevance used for data source coding
| Rigor | Relevance | ||
|---|---|---|---|
| Value | Quantitative | Qualitative | |
| 0 | Newspaper, magazine or other similar publication, opinion piece without citations for facts. | Newspaper, magazine or other similar publication, opinion piece without citations for facts. | Source does not address any component of Punctuated equilibrium. (Note: This category is rare/unlikely in that most articles that have made it through the inclusion criteria speak to at least a minimal component of equilibrium) |
| 1 | Opinion in peer reviewed journal Quantitative study with literature or expert analysis as data inputs |
Opinion in peer reviewed journal | Source speaks to a component of punctuated equilibrium, but the finding is not a direct outcome of the study, and only stated as part of the discussion or introduction to the study. Poorly developed news or opinion piece where punctuated equilibrium is a secondary element of the article and not sufficiently supported – often not in a peer reviewed journal. |
| 2 | Case studies/Focus Groups | Case studies/Focus Groups | Source identifies as part of the study findings a component of punctuated equilibrium, but the finding(s) are not the principle finding or aim of the study. News or opinion piece where punctuated equilibrium is not the primary aim of the article. |
| 3 | Observational studies with historical controls. Cross sectional surveys | Comparative case study | A principle aim and finding of the source relates to a component of equilibrium. News or opinion article that directly address a component of punctuated equilibrium. Example, a study or article evaluating the characteristics of medical practices that influence the adoption of health information technology. |
| 4 | Observational studies with concurrent control groups. | Systematic or integrative reviews. Less formal qualitative studies, but well documented repeatable methods. | A study or well-cited opinion piece that directly addresses a component of punctuated equilibrium. Article is well document and cited, makes a compelling and clear argument and is in a peer-reviewed journal. A model of technology adoption or transformation is often discussed or a unique perspective is offered. |
| 5 | Experimental study design | Formal qualitative method applied such as grounded theory, ethnography or other. Requires detailed repeatable description of methods. | The source meets more than one of the criteria for a score of ‘4’. For example, the article not only directly addresses a component of punctuated equilibrium, but additionally links these components together or defines relationships and influences among components of punctuated equilibrium. |
Table 2.
Definitions and descriptions of components used in coding data sources
| Descriptive Elements | Description |
|---|---|
| 1. Publication Date | Year of publication or dissemination |
| 2. Data Source | Source of the data. One of the five databases used or bibliography search |
| 3. Title | Title of the article or news story |
| 4. Author | Author(s) of the article or news story |
| 5. Journal | Journal, magazine, paper or other publication source |
| 6. Article Included | Article meets inclusion criteria (Y/N) |
| 7. Excluded | Article does NOT meet inclusion criteria (Y/N) |
| 8. Excluded Reason | Details on why article did not meet the criteria |
| 9. Use as background | Articles that did not meet inclusion criteria but were worthy of potential discussion within the study. These articles were often used on providing background or perspective throughout the study. |
| 10. Article not found | Full text could not be obtained |
| 11. Notes | General comments about article |
| 12. Population size | Size of population addressed by study. Blank if not a study |
| 13. Population Unit | Population unit, i.e. physician, patient, hospital. Blank if not a study. |
| 14. Industry setting | Setting of study, physicians in a hospital, hospitals within a national system. |
| 15. Study Design Type | Study design, i.e. survey, focus group, RCT, etc. “Opinion” or “News” if not a study |
| 16. Location | Location within the US if provided, “National” if concerning a national topic or national survey. |
| 17. Technology | Description of technology covered by study |
| 18. Model/Component | Article describes a “Component” of Punctuated Equilibrium or a “Model” of punctuated equilibrium |
| Evaluative Data | Definition and Example |
| 19. Deep Structure | Rules and Characteristics of the current environment either nationally or within a hospital or practice. Implementation studies that discuss structure or culture of organization including organizational priories and competitive environment. Barriers to change from the external environment of healthcare. |
| 20. Equilibrium | Internal obstacles to change. Elements that create inertia for the organization or system, i.e. large investment needed for IT. Implementation studies that describe process of implementation |
| 21. Revolution | Studies that describe deep structure altering changes within an organization. Policies that encourage such change. Definitions of revolutionary change or transformation |
| Interpretive Data | Description |
| 22. Quality Rigor | 0–5 score on the rigor of the study or article |
| 23. Quality Relevance | 0–5 score on the relevance of the study or article |
| 24. Quote or Thought | Key quote(s) or thoughts on the article as they relate to punctuated equilibrium |
| 25. Linkages | What does article say about linkages between Punctuated equilibrium components |
| 26. Influencers | What does article say about influencers of punctuated equilibrium component |
| 27. Cost | What does article say about costs and punctuated equilibrium component |
| 28. Culture | What does article say about culture and punctuated equilibrium component |
| 29. Time | What does article say about time and punctuated equilibrium component |
| 30. Precipitators | What does article say about precipitators of punctuated equilibrium component |
| 31. Followers | What does article say about followers of punctuated equilibrium component |
| 32. Punctuated Equilibrium component | Specific component addressed in study or article |
| 33. Deep Structure detail | Detail with regard to deep structure element (core value, strategy, power distribution, structure, control system). |
| 34. Patient | Does study or article address patients |
| 35. Practitioner | Does study or article address practitioners |
| 36. Hospital or Group | Does study or article address a hospital(s) or hospital group |
| 37. National System | Does study or article address the national system of healthcare |
| 38. Vendor | Does study or article address HIT vendors |
| 39. Strength Weakness | Describes the strengths and weaknesses of the study or article |
| 40. Notes | General comments |
2.5 Data Comparison/Synthesis
Directed content analysis was used to synthesize the findings. This method applies an existing framework (PEq model) to guide or “direct” analysis through constant comparison, sorting, data immersion, repeated questioning, and probing and sorting [27]. In this case the PEq model provided a starting point for coding each information source using a structured database. Once captured the data could be sorted and evaluated across multiple coded elements including, PEq component, relevance, key words, study design, setting, and others. Key themes emerged through a continued examination, sorting, probing, and evaluation of the structured data.
3. Results
3.1 Literature Retrieval
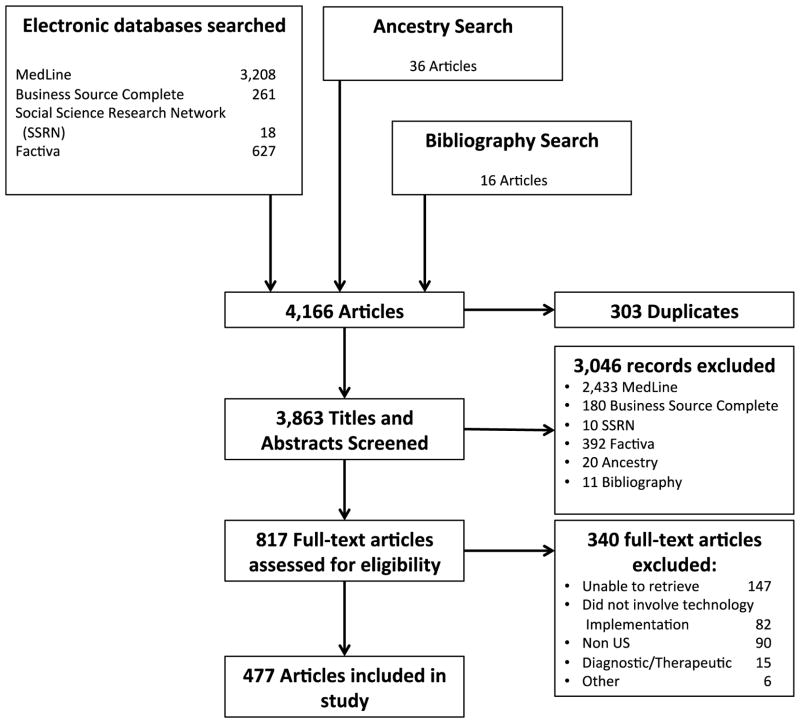
The search strategies yielded 3,863 candidate articles for which title and abstract were assessed for inclusion. This resulted in 817 articles for full text review. After full text review 477 articles met the criteria for inclusion (Figure 2). Reasons for exclusion were non-US setting, not addressing HIT, no relevance to the punctuated equilibrium framework, and a topic that addresses a therapeutic or diagnostic technique rather than a health information technology. Kappa scores calculated for each coding element represented “substantial agreement” with the exception of PEq Component (Table 3). Substantial agreement (0.61 – 0.80) indicates a significant level of consensus between the two raters. The lower “moderate agreement” (0.41 – 0.60) for the PEq component reflects the variation in knowledge between raters regarding the PEq framework [26].
Figure 2.
Search flow for relevant literature
Table 3.
Kappa scores for literature coding elements
| Coding Element | Kappa |
|---|---|
| Inclusion-Exclusion | 0.7326 |
| Rigor | 0.8047* |
| Relevance | 0.6563* |
| PEq Component | 0.5541 |
Weighted Kappa
3.2 Literature Characteristics
The majority of sources were news or opinion pieces from the popular press (n = 284, 55%). The remainder were case studies (n = 108, 21%), and cross sectional surveys (n = 80, 15%). The majority of sources did not identify a specific technology but discussed health information technology in general terms (n = 266, 51%). Technologies addressed were electronic health records (n = 113, 21%), computerized provider order entry (n = 27, 5%), and other technologies (n = 55, 10%). Other technologies included clinical decision support, health information exchange (HIE), ePrescribing, telehealth, and personal health records each of which represented no more than 3% of sources. Hospitals were the largest stakeholder group identified, followed by practitioners, national interests, patients, and vendors. Half (50%) of the sources addressed HIT from a national perspective. Massachusetts and Florida were the most frequent locations identified, followed by New York and Pennsylvania.
PEq components were represented in the 477 sources as follows: equilibrium (n = 224, 39%); deep structure (n = 202, 35%); and revolution (n = 147, 26%). A source could represent more than one PEq component. Over the study period, sources addressing equilibrium trended downward in frequency relative to other PEq components. Sources addressing revolution trended upward in frequency relative to deep structure and equilibrium. Sources addressing deep structure were distributed evenly in relation to equilibrium and revolution.
3.3 Thematic Elements of Punctuated Equilibrium
Directed content analysis identified ten themes across PEq components (Table 4): variations in the environment; market complexity; regulatory; flawed risk and reward; theories; barriers; ethical considerations; competition and sustainability; environmental elements, and internal elements. Themes are summarized in Table 4 and associated data sources are included and cross-referenced in Appendix B.
Table 4.
Summary of the Ten Themes Identified in the Literature by Punctuated Equilibrium Component.
| Identified Theme | Description | N* |
|---|---|---|
| Deep Structure | 202 | |
| 1. Variations in the environment | The environment of healthcare is defined by factors that influence the adoption and use of HIT, including provider location, size, and HIT vendor capabilities. | 85 |
| 2. Market Complexity | Healthcare operates within a complex environment characterized by patient confusion, multiple social interactions, data complexity and complex reimbursement systems. | 27 |
| 3. Regulatory | Regulations guide privacy and security, reporting, reimbursement, liability and standards. | 43 |
| 4. Flawed Risk and Reward | Incentives to adopt HIT are flawed; inure more to payers and patients than to providers adopting the systems. Fee-for-service reimbursement norms create further disincentives. | 24 |
| 5. Theories of Acceptance and Diffusion | Several models help describe the patterns of adoption and diffusion of technology within healthcare, including the Technology Acceptance Model and the Diffusion of Innovation theory among others. | 27 |
| Equilibrium | 224 | |
| 6. Barriers | Data sources highlighted the cost of HIT, lack of human and capital resources, and resistance to change from practitioners as barriers to transformation. | 134 |
| 7. Ethical Considerations | Ethical considerations contributing to equilibrium include an obligation for technology to do no harm, benefit everyone and not limit ability to practice autonomously. | 5 |
| 8. Competition and Sustainability | The market economy of the US demands a value driven business case for HIT adoption. | 34 |
| Revolution | 147 | |
| 9. Environmental Elements | Patient engagement and new models of care represent potential influencers of revolution within healthcare. | 74 |
| 10. Internal Elements | Change requires effective management, practitioner champions, a shared vision, and a favorable organizational culture. | 66 |
Data sources can reflect more than one PEq component or theme and not all data sources discussed a specific identified theme.
3.3.1 Deep Structure
Five themes were identified within the component of deep structure.
3.3.1.1
Variations in the environment were discussed in 85 sources, which described a diverse HIT environment with adoption and use correlated with practice size, urban versus rural location, and vendor capabilities. Sources generally observed a higher adoption rate by urban versus rural sites and larger versus smaller practice sizes. Differences in vendor standards, design, capabilities, and market maturity added to market variation and diversity. Authors highlighted the absence of standards and significant variation in workflows as obstacles.
3.3.1.2
Market complexity was discussed in 27 sources, characterized in the data by convoluted patient/provider/practitioner relationships, varying models of care delivery, multiple and complex reimbursement systems, data complexity, and difficulties related to the sheer size of the healthcare market. The patient-provider relationship was characterized as unbalanced compared to the influence of consumers in other market sectors. Variations in care delivery and reimbursement models were considered contributors to uncertainty in the system’s deep structure.
3.3.1.3
Regulatory issues were identified in 43 sources. Almost half of these sources (21) addressed concerns over meaningful use requirements. Meaningful use (MU) was characterized as a driver of market uncertainty that shifted focus away from service delivery and innovation. Privacy and security and anti-kickback regulations combined with evolving data standards were identified as additional regulatory components of deep structure.
3.3.1.4
Flawed risks and rewards within the healthcare market were identified in 24 sources. Fee-for-service was identified as creating flawed incentives for HIT adoption. The financial rewards of HIT investments were viewed as accruing to payers rather than providers in the form of reduced services and fees. In the case of health information exchange, benefits were described as flowing to competitors in the form of exposed consumer data. Lower productivity projections from HIT versus that achieved from IT in other markets were also highlighted.
3.3.1.5
Theories of technology acceptance and diffusion were discussed and/or tested in 27 sources. The Diffusion of Innovation and Technology Acceptance Models (TAM and TAM2) were mentioned most frequently. Other theories and models addressed were Interactive Sociotechnical Analysis, Least Effort Model, and Network Effect Model among others.
3.3.2 Equilibrium
Three themes were identified within the component of equilibrium.
3.3.2.1
Barriers to Change were identified in 134 sources, and included the high cost of HIT, resistance from practitioners, lack of technology resources, and market complexity. Resistance was characterized in terms of threats to provider autonomy, depersonalization of care, HIT inefficiency, and poor system design. The practice in healthcare of assessing innovations in care to a “gold standard” of evidence, when carried over to technology acceptance was viewed as a barrier and a sign of intrinsic risk aversion within the system.
3.3.2.2
Ethical considerations were identified by 5 sources in terms of the fair distribution of HIT resources (justice), obligation to provide a safe environment (beneficence), and the ability of patients and providers to make independent and informed decisions about care (autonomy).
3.3.3.3
Competition and sustainability were identified by 34 sources, which emphasized that HIT sustainability required innovations to deliver clear value across all stakeholder groups: insurers, patients, practices, and hospitals. Yet each stakeholder group was described as gaining value from a different aspect of innovation depending on role, size, location, goals, and funding.
3.3.4 Revolution
No sources described revolutionary change that met our definitional criteria. However, two themes were identified from the data that describe potential facilitators of transformative change.
3.3.4.1
Environmental elements necessary for transformation were discussed in 74 sources. Policy recommendations to spur transformation appeared most frequently in the data. These recommendations included a focus on patient safety, financial incentives for HIT adoption, access to capital, national standards for data interoperability, education and research on HIT and the exploration of new delivery and payment models. Patient engagement and empowerment was discussed as a requirement for health care transformation in tandem with the use of HIT and/or new delivery models. Patients were portrayed as undervalued in a system that emphasizes new processes and technologies.
3.3.3.2
Internal Elements Necessary for Transformation were discussed in 66 sources that addressed organizational conditions for transformation such as a shared vision, an employee commitment to HIT, a consistent and effective leadership, and a culture of change. Alignment of clinical and business priorities was identified as a necessity. Political and cultural clashes within an organization were identified as an impediment.
4. Discussion
This integrative review examined the healthcare literature from 2004 – 2012 for evidence of technology transformation. Analysis of 477 publications found evidence of a healthcare system resistant to change and engaged in incremental progress. No evidence of a radical departure from existing processes or technologies was found during this period.
The study has several limitations that constrain our conclusions. First is the potential for bias in use of a framework for evaluation and interpretation. It is possible that the evaluation favored findings that supported the framework. To limit this, a formal coding schema was used and the ability of external experts to consistently apply the schema was assessed with good results. Future iterations of this research could also utilize natural language processing and/or other automated methods and algorithms to limit such bias and provide a more reliable, faster, and current barometer of transformational change as it is occurring. Second there may be a lack of balance in assessing rigor and relevance of the sources leading to overemphasis on a specific theme. The integrative review methodology is meant to address this imbalance through inclusion of a broad scope of data sources. Finally, our most recent data sources are limited to April 2012. Since that time hospital adoption of HIT systems (integrated and not integrated) has increased among institutions and individual providers [28]. Shared savings and other valued based payment models have become more prevalent. The US Department of Health and Human Services has established aggressive targets for such payments through 2018 [7]. The proposed Stage 3 Meaningful Use (MU) regulations have placed greater emphasis on health information exchange and empowering patients [29] with many also perceiving an increasing focus on the consumer in the HIT community [30, 31]. Recently, the HIT vendor community has begun to recognize regulation and standardization as a value-added proposition [32]. We recognize that these developments among others are underrepresented in our pool of publications, but believe that applying this new methodology could be fruitful in evaluating the actual transformational effects of current national policies. Our intention here was to demonstrate the value of our methodological approach in assessing transformational change. We hope that either we or others will be able to apply this methodology again to evaluate transformative change observed by these recent developments. Below we discuss our conclusions in light of these and other developments.
The theory of Punctuated Equilibrium posits that a system remains in a resistant period or a state of equilibrium when the status quo dampens the disruption that precedes transformational change (Exhibit 1). Equilibrium is inertia generated by known market characteristics (deep structure) when there is uncertainty about a superior alternative. In the HIT landscape elements of deep structure include absence of uniform standards and an unregulated market with limited requirements for interoperability, workflow continuity, or product safety. Purposefully or not, these factors collude to perpetuate a fragmented market, rife with uncertainty over return on HIT investment.
Regulation has been traditionally viewed as a curb to innovation and boon for the status quo. In the current environment insufficient regulation around standards has led to innovation that fosters market uncertainty through excessive variation. The federal regulatory approach (MU) controls process and functionality, while ignoring the “few simple rules” principal of emergence in complex adaptive systems [33]. The result is equivocal improvements in quality and efficiency [34]. We argue that clear regulations are needed around data standards and interoperability to allow the free flow of data that will lay a foundation for revolution.
The nation’s HIT Strategic Plan describes a series of incremental steps culminating in the “accelerated adoption” of HIT at the market level [8]. This scenario for technological transformation is not supported by case histories in other industries like banking, manufacturing, travel, or Internet businesses [16, 17, 24, 35–39]. Consumer involvement and open access to data was a key driver of transformation in these markets [40, 41]. The strong equilibrium exhibited by the healthcare market stifles the consumer’s (patient’s) ability to assess healthcare value due to complexity and uncertainty. Our nation’s health reform policy is specifically devised to avoid disrupting the existing employer-based health insurance. New reimbursement and delivery models designed to address embedded provider roles create new uncertainties and risks [4, 5]. They also do not change how health professionals are educated which further enforces the status quo [42].
We argue that the role patients have been allowed to take is highly constrained by HIT stakeholders’ offerings and current policies. Absent disruptive forces from other parts of the healthcare system, consumers must drive transformation by demanding access to health data free of the constraints prescribed by system gatekeepers who consciously or not perpetuate market equilibrium. The strength of healthcare equilibrium does not provide any opportunity for the consumer to become involved. Understandable, consumer-driven measures of healthcare value will emerge from open data access and awaken a consumer that will demand a strong role in the process of care.
The technology and business press have begun to increase calls for market disruption as a necessary path toward technological innovation and true healthcare transformation [43–47]. The beginnings of such disruptions can be seen in the aggressive value based payment targets established by the US Department of Health and Human Services and the emphasis on open APIs within the proposed Stage 3 EHR Incentive Program regulations that will demand the free flow exchange of data and increased consumer involvement. We enter this new period with trepidation, but excitement that an empowered consumer when given open access to data will provide the disruption necessary for transformational change. Until we as a society or as consumers in a healthcare market have the ability to demand disruption in the status quo, incremental and diffusional change will continue, as Gersick’s theory tells us, with predictably disappointing results.
Supplementary Material
HIGHLIGHTS.
Describe an integrative review methodology to assess transformation in healthcare
Identify inhibitors to change within the complex healthcare market
The healthcare system inhibits direct consumer involvement and engagement
We propose policies that will encourage healthcare transformation
Acknowledgments
This work was based on research completed as part of a PhD and the authors wish to thank the remaining committee members Patricia Stone, David Kaufman, Rainu Kaushal, and Suzanne Bakken for their contributions.
Funding Source
Andrew B. Phillips received support from an institutional training grant to Columbia University from the National Institute of Nursing Research (T32NR007969).
Appendix A
Specific Search Strategies
Appendix B
Detailed Data Coding
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Davis K, Schoen C, Stremikis K. Mirror Mirror on the Wall How the Performance of the US Health Care System Compares Internationally - 2010 Update. The Commonwealth Fund; 2010. [Google Scholar]
- 2.Schuster MA, McGlynn EA, Brook RH. How good is the quality of health care in the United States? Milbank Quarterly. 2005;83:843–95. doi: 10.1111/j.1468-0009.2005.00403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kocot SL, Brennan N, Cafarella N, McKethan A, Morrison M, Nguyen N, et al. Improving Quality and Value in the US Health Care System. Bipartisan Policy Center, Brookings Institution; 2009. [Google Scholar]
- 4.Patient Protection and Affordable Care Act. 2010.
- 5.American Recovery and Reinvestment Act of 2009. 2009.
- 6.Centers for Medicare & Medicaid Services. EHR Incentive Programs, Data and Program Reports 2015. [Google Scholar]
- 7.US Department of Health and Human Services. Better, Smarter, Healthier: In historic announcement, HHS sets clear goals and timeline for shifting Medicare reimbursements from volume to value. Washington, DC: 2015. [DOI] [PubMed] [Google Scholar]
- 8.Office of the National Coordinator for Health Information Technology (ONC); US Department of Health and Human Services, editor. Federal Health Information Technology Strategic Plan: 2011 – 2015. Washington, DC: 2011. [Google Scholar]
- 9.Office of the National Coordinator for Health Information Technology (ONC) Federal Health IT Strategic Plan 2015 – 2020. Washington, DC: 2015. [Google Scholar]
- 10.Begun JW, Dooley K, Zimmerman B. Advances in Health Care Organisation Theory. San Francisco: Jossey-Bass; 2003. Health care organizations as complex adaptive systems. [Google Scholar]
- 11.Goldstein J. Emergence: A construct amid a thicket of conceptual snares. Emergence. 2000;2:5–22. [Google Scholar]
- 12.Holden LM. Complex adaptive systems: concept analysis. Journal of Advanced Nursing. 2005;52:651–7. doi: 10.1111/j.1365-2648.2005.03638.x. [DOI] [PubMed] [Google Scholar]
- 13.Tan J, Wen HJ, Awad N. Health care and services delivery systems as complex adaptive systems. Communications of the ACM. 2005;48:36–44. [Google Scholar]
- 14.Miller JH, Page SE. Complex adaptive systems: An introduction to computational models of social life. Princeton Univ Pr; 2007. [Google Scholar]
- 15.Coiera E. Why system inertia makes health reform so difficult. BMJ. 2011:342. doi: 10.1136/bmj.d3693. [DOI] [PubMed] [Google Scholar]
- 16.Tushman ML, Anderson P. Technological discontinuities and organizational environments. Admin Sci Quart. 1986:439–65. [Google Scholar]
- 17.Romanelli E, Tushman ML. Organizational transformation as punctuated equilibrium: An empirical test. Acad Manage J. 1994:1141–66. [Google Scholar]
- 18.Eldredge N, Gould SJ. Punctuated equilibria: an alternative to phyletic gradualism. Models in paleobiology. 1972;82:115. [Google Scholar]
- 19.Gersick CJG. Revolutionary change theories: A multilevel exploration of the punctuated equilibrium paradigm. Academy of Management Review. 1991:10–36. [Google Scholar]
- 20.Anderson RA, Crabtree BF, Steele DJ, McDaniel RR. Case study research: The view from complexity science. Qualitative Health Research. 2005;15:669. doi: 10.1177/1049732305275208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whittemore R, Knafl K. The integrative review: updated methodology. Journal of Advanced Nursing. 2005;52:546–53. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- 22.Martin B. Tech Boom 2.0: Lessons Learned From the Dot-Com Crash. Wired: Condé Nast. 2013. [Google Scholar]
- 23.Tushman ML, Romanelli E. Organizational evolution: A metamorphosis model of convergence and reorientation. Research in organizational behavior. 1985 [Google Scholar]
- 24.Anderson P, Tushman ML. Technological discontinuities and dominant designs: A cyclical model of technological change. Admin Sci Quart. 1990:604–33. [Google Scholar]
- 25.Bush GW. Executive Order 13335, Incentives for the Use of Health Information Technology and Establishing the Position of the National Health Information Technology Coordinator. 2004. [Google Scholar]
- 26.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–3. [PubMed] [Google Scholar]
- 27.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 28.Office of the National Coordinator for Health Information Technology (ONC) Federal Health IT Strategic Plan Progress Report. 2013. [Google Scholar]
- 29.US Department of Health and Human Services - Center for Medicare and Medicaid Services; Services DoHaH, editor. Medicare and Medicaid Programs; Electronic Health Record Incentive Program - Stage 3 - Proposed Rule. 42 CFR Part 4952015. [Google Scholar]
- 30.Huckman RS, Kelley MA. Public reporting, consumerism, and patient empowerment. New England Journal of Medicine. 2013;369:1875–7. doi: 10.1056/NEJMp1310419. [DOI] [PubMed] [Google Scholar]
- 31.Frist WH. Connected Health And The Rise Of The Patient-Consumer. Health Affairs. 2014;33:191–3. doi: 10.1377/hlthaff.2013.1464. [DOI] [PubMed] [Google Scholar]
- 32.Kellermann AL, Jones SS. What It Will Take To Achieve The As-Yet-Unfulfilled Promises Of Health Information Technology. Health Affairs. 2013;32:63–8. doi: 10.1377/hlthaff.2012.0693. [DOI] [PubMed] [Google Scholar]
- 33.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 34.Shekelle PG, Jones SS, Rudin RS, Shanman R. Health Information Technology: An Updated Systematic Review with a Focus on Meaningful Use Functionalities. Washington, DC: RAND Corporation; 2014. [DOI] [PubMed] [Google Scholar]
- 35.Dehning B, Richardson VJ, Zmud RW. The value relevance of announcements of transformational information technology investments. MIS Quarterly. 2003:637–56. [Google Scholar]
- 36.Guillemette MG, Pare G. Transformation of the Information Technology Function in Organizations: A Case Study in the Manufacturing Sector. Canadian Journal of Administrative Sciences/Revue Canadienne des Sciences de l’Administration. 2011 [Google Scholar]
- 37.Lucas HC. Inside the future: Surviving the technology revolution. Praeger Publishers; 2008. [Google Scholar]
- 38.Loch CH, Huberman BA. A punctuated-equilibrium model of technology diffusion. Management Science. 1999:160–77. [Google Scholar]
- 39.Nutt PC, Backoff RW. Organizational transformation. Journal of Management Inquiry. 1997;6:235–54. [Google Scholar]
- 40.Brown J, Cox D, Griffiths S, Sanger N, Weston D. Evolving Models of Retail Banking Distribution Capitalizing on changes in channel usage. Deloitte Center for Banking Solutions; 2008. [Google Scholar]
- 41.Daugherty P, Biltz MJ, Banerjee P. Accenture Technology Vision 2014: Every Business Is a Digital Business: From Digitally Disrupted to Digital Disrupter. Accenture Technology Labs; 2014. [Google Scholar]
- 42.Crisp N, Chen L. Global Supply of Health Professionals. New England Journal of Medicine. 2014;370:950–7. doi: 10.1056/NEJMra1111610. [DOI] [PubMed] [Google Scholar]
- 43.Feder J. The Inevitability of Disruption in Health Reform. 2014. [Google Scholar]
- 44.Christensen CM, Bohmer R, Kenagy J. Will disruptive innovations cure health care? Harvard business review. 2000;78:102–12. [PubMed] [Google Scholar]
- 45.Briggs B. Tech Trends 2014: Inspiring Disruption. Deloitte University Press; 2014. [Google Scholar]
- 46.Clayton Christensen Institute for Disruptive Innovation. 2012.
- 47.Rae-Dupree J. Disruptive Innovation, Applied to Health Care. New York Times; New York: 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.