Abstract
Between the 17th and 20th centuries, blood was transfused from various animal species into patients with a variety of pathological conditions. Skin grafts were carried out in the 19th century, with grafts from a variety of animals, with frogs being the most popular. In the 1920s, Voronoff advocated the transplantation of slices of chimpanzee testis into elderly men, believing that the hormones produced by the testis would rejuvenate his patients. In 1963–4, when human organs were not available and dialysis was not yet in use, Reemtsma transplanted chimpanzee kidneys into 13 patients, one of whom returned to work for almost 9 months before suddenly dying from what was believed to be an electrolyte disturbance. The first heart transplant in a human ever performed was by Hardy in 1964, using a chimpanzee heart, but the patient died within two hours. Starzl carried out the first chimpanzee-to-human liver transplantation in 1966; in 1992 he obtained patient survival for 70 days following a baboon liver transplant. The first clinical pig islet transplant was carried out by Groth in 1993. Today, genetically-modified pigs offer hope of a limitless supply of organs and cells for those in need of a transplant.
The concept of xenotransplantation (cross-species transplantation) is not new, and there have been numerous clinical attempts during the past 300 years or more [1–3].
Mythology
A review of Greek mythology and of religious tracts—particularly, for example, from the Hindu religion—draws attention to the fact that humans have been interested in the possibility of merging physical features from various animal species for hundreds of years. For example, the lamassu has been selected as the mythological figure to represent the International Xenotransplantation Association and its official scientific journal, Xenotransplantation.
The late Keith Reemtsma pointed out that possibly one of the earliest examples of xenotransplantation was the attempt by Daedalus and his son, Icarus, to fly across the sea from Crete to mainland Greece with the help of bird wings attached to their arms [4]. Icarus failed in the attempt, but Daedalus made the journey successfully.
Blood xenotransfusion
If we look beyond the realm of mythology and legend, we come to the 17th century, when Jean Baptiste Denis began the clinical practice of blood transfusion from animals to humans [5]. Perhaps not surprisingly, the results were mixed. As a result, xenotransfusion was banned in France for a number of years.
Skin xenotransplantation
In the 19th century, skin grafts became relatively popular between various animal species and humans [6, 7]. The grafts were either free or pedicle grafts. Pedicle grafts were complicated because they required the donor, e.g., a sheep, to be strapped immobile to the patient for several days, during which time the graft would reputedly be vascularized by the recipient. If this occurred, the graft could be disconnected from the donor. It is almost certain that none of these grafts was in any way successful, although some “successes” were reported.
The fact that many of the species used as donors—sheep, rabbits, dogs, cats, rats, chickens, and pigeons—had hair, feathers, or fur growing from the skin did not appear to disconcert the surgeons involved, but the trend was to use animal species in which these accoutrements were not present. The ideal graft would appear to have been from frogs, which were sometimes “skinned alive.” It is possible that some of these grafts were “successful” in that, when used to cover a skin ulcer, they provided protection, at least for a number of days, while the ulcer healed beneath the graft. However, probably none of the grafts actually became permanent.
Corneal xenotransplantation
Remarkably, in 1838 the first corneal xenotransplantation (from a pig) was performed in a patient, whereas the first corneal allotransplantation (human-to-human) was not carried out until more than 65 years later, in 1905. The field of corneal xenotransplantation has been reviewed by Hara and Cooper [8, 9].
The surgery of blood vessel anastomosis
More scientific efforts had to wait until the 20th century, when the French experimental surgeon, Alexis Carrel, working first in France and subsequently in North America, developed surgical techniques for anastomosing blood vessels, which enabled organ transplantation to be carried out successfully for the first time. For this work he was awarded the Nobel Prize in 1912. He developed an interest in cross-species transplantation from an experimental perspective.
“Rejuvenation” by cell xenotransplantation
A few years later, Serge Voronoff, a Russian émigré working in Paris, developed the concept of transplanting cells that produced a hormone in which the recipient was deficient. This is another example of a visionary scientist who was ahead of his time. Today we are doing exactly what he envisaged, namely transplanting human pancreatic islets that produce insulin in patients with severe type 1 diabetes. In view of the limited number of human pancreases that become available each year, there is a growing interest in using pig islets for this purpose.
Voronoff’s main interest, however, was in reversing the effects of aging in elderly men who had lost their “zest for life.” He carried out a significant number of chimpanzee or baboon testicular transplants in male human recipients [10]. His technique was to slice up the animal testicle and insert the slices into the recipient’s testicle. The procedure became popular on both sides of the Atlantic, and several hundred of these operations were performed. It is inconceivable that any of them had any beneficial effect whatsoever, except psychological, but there were reports of remarkable “rejuvenation” of men who reported much increased energy after the operation. Surprisingly, reports of complications appear to have been uncommon.
The concept of transplanting glandular tissue to produce hormones that would benefit the recipient was continued in the United States by a much less scientific doctor, John Brinkley, whose work was carried out largely in Kansas and Texas [11]. His chosen donor was the goat, as he had been convinced by a local farmer of its sexual potency.
Kidney xenotransplantation
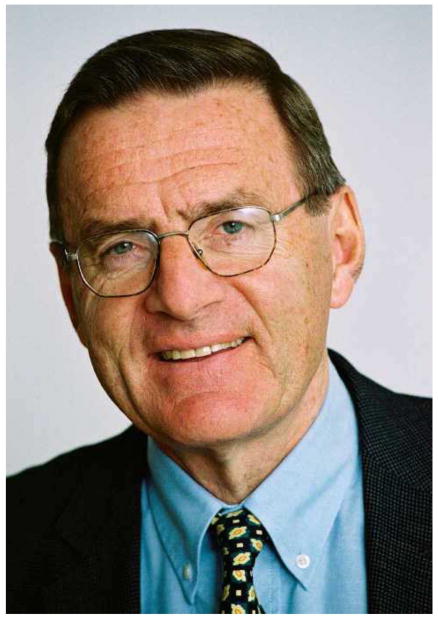
By the 1960s, Keith Reemtsma (Figure 1)—at that time at Tulane University in Louisiana—hypothesized that nonhuman primate kidneys might function in human recipients and thus be a successful treatment for renal failure. At that time, the concept of kidney transplantation had been established largely by French and American surgeons, but the availability of kidneys from deceased humans was extremely limited and chronic dialysis was not yet being undertaken. In Reemtsma’s opinion, therefore, there was little alternative to death for the patient unless organs could be made available from nonhuman species. He selected the chimpanzee as the source of organs because of its close evolutionary relationship to humans. He carried out 13 of these transplants, on each occasion transplanting both kidneys from a chimpanzee (that generally weighs significantly less than an adult human) into the recipient [12].
Figure 1.
Keith Reemtsma (1925–2000). [Courtesy the late Keith Reemtsma.]
Most of the transplants failed within 4 to 8 weeks, either from rejection (because of the limited immunosuppressive agents available at the time) or from an infectious complication (because of the overadministration of these agents). Nevertheless, one of Reemtsma’s patients lived for 9 months, returning to work as a schoolteacher and evidently remaining in good health until she suddenly collapsed and died. At autopsy, the chimpanzee kidneys appeared normal and showed no signs of acute or chronic rejection. It was suggested that she had died from an acute electrolyte disturbance. This is possible since the transplantation of nonhuman primate kidneys into patients was frequently associated with an immense diuresis in the early posttransplantation period, often exceeding 20 liters in 24 hours, and so there possibly could have also been a late electrolyte imbalance.
The concept of using nonhuman primates as kidney donors was expanded by several surgeons, particularly by Tom Starzl (Figure 2) in Colorado, who used baboons as donors [13]; his results were similar to those of Reemtsma, except that he did not achieve any relatively long-term survivors. Others in the US and in France also had small experiences [2].
Figure 2.
Tom Starzl (born 1926). [Courtesy Thomas E. Starzl.]
Heart xenotransplantation
James Hardy (Figure 3), who had carried out the first human lung allotransplant in 1963, visited Reemtsma and was impressed by the health of some of the patients with chimpanzee kidney transplants. In 1964, Hardy was determined to carry out the first clinical heart transplantation and decided to acquire some chimpanzees as potential “donors” in case he could not identify a deceased human donor. He had a less-than-ideal patient who would not be accepted for heart transplantation today, as he had widespread atheromatous vascular disease throughout his body—for which he had undergone amputations of both legs—and was in a semicomatose state at the time the transplant was undertaken. However, as the patient was rapidly dying, Hardy was stimulated to transplant a chimpanzee heart [14]. The heart proved not to be large enough to support the circulation and failed within a couple of hours.
Figure 3.
James Hardy (1918–2003). [Courtesy the late James Hardy.]
In contrast to the response to the attempted lung allotransplantation, the public and medical professional response to the heart xenotransplantation was adverse and dissuaded Hardy and his colleagues from carrying out any further attempts. The procedure of cardiac allotransplantation was later established by Barnard and his colleagues in 1967 [15], who later also carried out two heterotopic cardiac xenotransplants, using a chimpanzee and a baboon as ‘donors [16].
It is of interest to note that the consent form for Hardy’s operation—which, in view of the patient’s semicomatose condition, was signed by a close relative—stipulated that no heart transplant had ever been performed, but made no mention of the fact that an animal heart might be used for the procedure. Such was the medicolegal situation at that time that this “informed” consent was not considered in any way inadequate.
Perhaps the best known clinical cardiac xenotransplantation since Hardy’s attempt was that by Leonard Bailey (Figure 4), who transplanted a baboon heart into an infant girl, known as Baby Faye, in 1983. At that time, it was almost impossible to obtain human organs from infants, particularly those with anencephaly, for transplantation into infants with life-threatening congenital heart disease. The surgical procedure in Baby Faye was technically successful, but the graft underwent acute rejection and the patient died 20 days later [17]. As the graft was necessarily taken from a baboon that was ABO-incompatible with the recipient—as the O blood type is essentially not found in baboons—this might have added to the severity of rejection. Even though cyclosporine had become available by this time, the immunosuppressive therapy was not sufficient to prevent xenograft rejection.
Figure 4.
Leonard Bailey (born 1942). [Courtesy Leonard Bailey.]
This procedure did little to advance progress in xenotransplantation, but it did draw public and medical attention to the dearth of deceased human organs available for infants in need of a transplant. Following the procedure, particularly with the immense publicity associated with it, the situation with regard to donation of organs from infants became very much improved, and Bailey went on to develop an extremely successful cardiac allotransplantation program in infants and children at Loma Linda University.
Liver xenotransplantation
Tom Starzl (Figure 2), who is one of the greatest pioneers in the field of kidney and liver allotransplantation, performed a handful of liver transplants between nonhuman primates and young patients in Colorado in the 1960s without lasting success [18–21]. When the addition of tacrolimus had improved the immunosuppressive armamentarium, he and his team in Pittsburgh performed two liver transplants from baboons in adult patients in the 1990s, with one patient surviving for 70 days [22]. The results, however, were not successful enough to warrant continuing this experimental clinical trial.
Most of the early attempts at clinical organ xenotransplantation used nonhuman primate species as sources of the organ, although there were a few attempts using the pig [23] and other nonprimate mammals, but without significant success [2].
Islet xenotransplantation
A Swedish group headed by Carl Groth (Figure 5) was the first to attempt pig islet transplantation in patients with diabetes in 1993 [24]. Although porcine C-peptide was documented in the blood of some of the patients, indicating that some islets survived, no clinical benefit was obtained.
Figure 5.
Carl-Gustav Groth (1933–2014). [Courtesy the late Carl-Gustav Groth.]
Xenotransplantation using pigs as sources of organs and cells
The advantages of xenotransplantation, particularly if we could use a readily available animal source, such as the pig, would be numerous (Table 1) [25]. There would be an unlimited supply of “donor” organs, which would resolve the current increasing and severe shortage of human organs. The immunological and pathobiological problems associated with pig xenotransplantation, however, are significant and probably reflect the fact that it has been 80 million years since the pig and human diverged on the evolutionary scale. Therefore, in the words of Claus Hammer, what we are trying to do is to “outwit evolution.” The pathobiological barriers associated with pig-to-primate organ and cell transplantation are summarized elsewhere in this issue.
Table 1.
The advantages and disadvantages of the pig vs baboon as a epotential source of organs and cells for humans
| Pig | Baboon | |
|---|---|---|
| Availability | Unlimited | Limited |
| Breeding potential | Good | Poor |
| Period to reproductive maturity | 4–8 months | 3–5 years |
| Length of pregnancy | 114 ± 2 days | 173–193 days |
| Number of offspring | 5–12 | 1–2 |
| Growth | Rapid (adult human size within 6 months)* | Slow (9 years to reach maximum size) |
| Size of adult organs | Adequate | Inadequate† |
| Cost of maintenance | Significantly lower | High |
| Anatomical similarity to humans | Moderately close | Close |
| Physiological similarity to humans | Moderately close | Close |
| Relationship of immune system to humans | Distant | Close |
| Knowledge of tissue typing | Considerable (in selected herds) | Limited |
| Necessity for blood type compatibility with humans | Probably unimportant | Important |
| Experience with genetic engineering | Considerable | None |
| Risk of transfer of infection (xenozoonosis) | Low | High |
| Availability of specific pathogen- free animals | Yes | No |
| Public opinion | More in favor | Mixed |
Breeds of miniature swine are approximately 50% of the weight of domestic pigs at birth and sexual maturity and reach a maximum weight of approximately 30% of standard breeds. At full size, miniature swine are easier to house and to handle. Furthermore, inbred herds are available, though cloning of any pig can result in inbred herds, if needed. Although MHC-identical miniature swine may have some specific immunologic advantage, the disadvantage is that they cannot be cross-bred with other pig strains in which a genetic modification has been introduced; if cross-breeding is carried out, clearly MHC identity is lost. (Reproduced with permission from Cooper DKC. A brief history of cross-species organ transplantation. Baylor Univ Med Center Proc 2012;25:49–57)
Highlights.
Clinical xenotransplantation has involved skin, corneas, and blood
Nonhuman primate kidney and heart grafts were transplanted into patients
The first clinical attempt at pig islet transplantation was in 1993
There are advantages in the use of the pig as the source of organs and cells
Acknowledgments
Work on xenotransplantation in the Thomas E. Starzl Transplantation Institute at the University of Pittsburgh has been supported in part by National Institutes of Health grants U01 AI068642, R21 AI074844, and U19 AI090959, and by sponsored research agreements between the University of Pittsburgh and Revivicor, Inc., Blacksburg, VA.
Funding
Work on xenotransplantation in the Thomas E. Starzl Transplantation Institute at the University of Pittsburgh has been supported in part by National Institutes of Health grants U01 AI068642, R21 AI074844, and U19 AI090959, and by sponsored research agreements between the University of Pittsburgh and Revivicor, Inc., Blacksburg, VA.
Footnotes
Conflict of interest
The authors declare no conflict of interest.
Author contribution
DKCC, BE, AJT – all participated in review of the literature, writing of the manuscript, and final approval of the manuscript.
Guarantor
David K.C. Cooper, MD, PhD.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cooper DKC, Lanza RP. Xeno--the promise of transplanting animal organs into humans. New York: Oxford University Press; 2000. [Google Scholar]
- 2.Taniguchi S, Cooper DK. Clinical xenotransplantation: past, present and future. Ann R Coll Surg Engl. 1997;79:13–19. [PMC free article] [PubMed] [Google Scholar]
- 3.Deschamps JY, Roux FA, Sai P, Gouin E. History of xenotransplantation. Xenotransplantation. 2005;12:91–109. doi: 10.1111/j.1399-3089.2004.00199.x. [DOI] [PubMed] [Google Scholar]
- 4.Reemtsma K. Xenotransplantation--a brief history of clinical experience: 1900–1965. In: Cooper DKCKE, Reemtsma K, White DJG, editors. Xenotransplantation: The transplantation of organs and tissues between species. 1. Heidelberg: Springer; 1991. pp. 9–22. [Google Scholar]
- 5.Roux FA, Sai P, Deschamps JY. Xenotransfusions, past and present. Xenotransplantation. 2007;14:208–216. doi: 10.1111/j.1399-3089.2007.00404.x. [DOI] [PubMed] [Google Scholar]
- 6.Gibson T. Zoografting: a curious chapter in the history of plastic surgery. Br J Plast Surg. 1955;8:234–242. doi: 10.1016/s0007-1226(55)80040-9. [DOI] [PubMed] [Google Scholar]
- 7.Cooper DKC. Xenografting: the early, early years. Xeno. 1997;5:21–22. [Google Scholar]
- 8.Hara H, Cooper DK. The immunology of corneal xenotransplantation: a review of the literature. Xenotransplantation. 2010;17:338–349. doi: 10.1111/j.1399-3089.2010.00608.x. [DOI] [PubMed] [Google Scholar]
- 9.Hara H, Cooper DK. Xenotransplantation--the future of corneal transplantation? Cornea. 2011;30:371–378. doi: 10.1097/ICO.0b013e3181f237ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamilton D. The monkey gland affair. London: Chatto and Windus; 1986. [Google Scholar]
- 11.Lee RA. The bizarre careers of john r. Brinkley. Lexington: University Press of Kentucky; 2002. [Google Scholar]
- 12.Reemtsma K, McCracken BH, Schlegel JU, Pearl MA, Pearce CW, Dewitt CW, et al. Renal heterotransplantation in man. Ann Surg. 1964;160:384–410. doi: 10.1097/00000658-196409000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Starzl TE, Marchioro TL, Peters GN, Kirkpatrick CH, Wilson WE, Porter KA, et al. Renal heterotransplantation from baboon to man: experience with 6 cases. Transplantation. 1964;2:752–776. doi: 10.1097/00007890-196411000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hardy JD, Kurrus FD, Chavez CM, Neely WA, Eraslan S, Turner MD, et al. Heart transplantation in man. Developmental studies and report of a case. JAMA. 1964;188:1132–1140. [PubMed] [Google Scholar]
- 15.Barnard CN. The operation. A human cardiac transplant: an interim report of a successful operation performed at groote schuur hospital, cape town. S Afr Med J. 1967;41:1271–1274. [PubMed] [Google Scholar]
- 16.Barnard CN, Wolpowitz A, Losman JG. Heterotopic cardiac transplantation with a xenograft for assistance of the left heart in cardiogenic shock after cardiopulmonary bypass. S Afr Med J. 1977;52:1035–1038. [PubMed] [Google Scholar]
- 17.Bailey LL, Nehlsen-Cannarella SL, Concepcion W, Jolley WB. Baboon-to-human cardiac xenotransplantation in a neonate. JAMA. 1985;254:3321–3329. [PubMed] [Google Scholar]
- 18.Starzl TE, Marchioro TL, Faris TD, McCardle RJ, Iwaski Y. Avenues of future research in homotransplantation of the liver with particular reference to hepatic supportive procedures, antilymphocyte serum, and tissue typing. Am J Surg. 1966;112:391–400. doi: 10.1016/0002-9610(66)90209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Starzl TE. Orthotopic heterotransplantation. In: Starzl, editor. Experience in hepatic transplantation. Philadelphia: WB Saunders; 1969. p. 408. [Google Scholar]
- 20.Starzl TE, Ishikawa M, Putnam CW, et al. Progress in and deterrents to orthotopic liver transplantation, with special reference to survival, resistance to hyperacute rejection, and biliary duct reconstruction. Transplant Proc. 1974;6(4 suppl 1):129–139. [PMC free article] [PubMed] [Google Scholar]
- 21.Giles GR, Boehmig HJ, Amemiya H, Halgrimson CG, Starzl TE. Clinical heterotransplantation of the liver. Transplant Proc. 1970;2:506–512. [PMC free article] [PubMed] [Google Scholar]
- 22.Starzl TE, Fung J, Tzaki A, et al. Baboon-to-human liver transplantation. Lancet. 1993;341:65–71. doi: 10.1016/0140-6736(93)92553-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Makowka L, Wu GD, Hoffman A, et al. Immunohistopathologic lesions associated with the rejection of a pig-to-human liver xenograft. Transplant Proc. 1994;26:1074–1075. [PubMed] [Google Scholar]
- 24.Groth CG, Korsgren O, Tibell A, et al. Transplantation of porcine fetal pancreas to diabetic patients. Lancet. 1994;344:1402–1404. doi: 10.1016/s0140-6736(94)90570-3. [DOI] [PubMed] [Google Scholar]
- 25.Cooper DK, Gollackner B, Sachs DH. Will the pig solve the transplantation backlog? Annu Rev Med. 2002;53:133–147. doi: 10.1146/annurev.med.53.082901.103900. [DOI] [PubMed] [Google Scholar]