Abstract
The limited availability of deceased human organs and cells for the purposes of clinical transplantation remains critical worldwide. Despite the increasing utilization of ‘high-risk’, ‘marginal’, or ‘extended criteria’ deceased donors, in the U.S. each day 30 patients either die or are removed from the waiting list because they become too sick to undergo organ transplantation. In certain other countries, where there is cultural resistance to deceased donation, e.g., Japan, the increased utilization of living donors, e.g., of a single kidney or partial liver, only very partially addresses the organ shortage. For transplants of tissues and cells, e.g., pancreatic islet transplantation for patients with diabetes, and corneal transplantation for patients with corneal blindness (whose numbers worldwide are potentially in the millions), allotransplantation will never prove a sufficient source. There is an urgent need for an alternative source of organs and cells. The pig could prove to be a satisfactory source, and clinical xenotransplantation using pig organs or cells, particularly with the advantages provided by genetic engineering to provide resistance to the human immune response, may resolve the organ shortage. The physiologic compatibilities and incompatibilities of the pig and the human are briefly reviewed.
Keywords: cell transplantation, pig, organ shortage, organ transplantation, xenotransplantation
INTRODUCTION
Organ transplantation is an established therapy for a variety of end-stage organ diseases. Today, improved surgical techniques and our understanding of the immune system have increased survival of patients with organ allografts. In the U.S., more than 617,000 solid organ transplants, including kidney, liver, pancreas, intestine, heart, and lung, have been performed since 1988 [1]. Worldwide, the numbers are probably at least double the US figure. Although most attention has been directed towards transplantation of solid organs, corneal transplantation, bone marrow transplantation, isolation and transplantation of cells and tissues with specific differentiated functions (e.g., pancreatic islets) represent important additional clinical therapies.
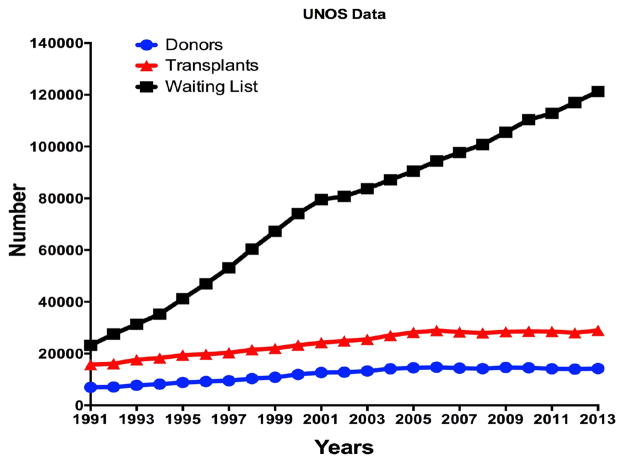
The major current problem in organ transplantation is the gap between the number of available transplantable organs that become available each year and the number of patients waiting for an organ graft (Figure 1) [2]. In the U.S., due to the lack of sufficient transplantable organs, each day 30 people either die while waiting for a transplant or are removed from the waiting list because they become too sick to undergo a transplant [2].
Figure 1. Trends in the numbers of organ donors (blue), organ transplants (red), and patients on the waiting list (black) in the U.S., 1991–2013.
In 1991, there were 6,953 donors, 15,757 organ transplants, and 23,198 patients on the waiting list. By 2013, there were 14,257 donors, 28,954 organ transplants, and 121,272 patients on the waiting list. (Data obtained from http://optn.transplant.hrsa.gov.)
Significant changes in attitude and law towards organ donation would make increased numbers of organs available, but the supply would remain inadequate. In 1991, there were 6,953 deceased human donors, enabling 15,756 organ transplants to be carried out, and 23,198 patients on the waiting list. A decade later, in 2001, although there were 12,702 donors (an 83% increase), enabling 24,239 transplants to be performed (a 54% increase), the waiting list had expanded to 79,524 patients (a 243% increase). The significant increase in donation was partially the result of the National Organ Transplant Act signed by President Ronald Regan in October 1984 [3]. This law was signed 30 years ago and was aimed to establish the legal framework for the procurement, donation, and transplantation of organs. It was hoped that the law would end the organ shortage. However, the 85% increase in donation rate was offset by a 243% increase in patients on the waiting list, which resulted from the documented better outcomes after organ transplantation compared to alternative therapies.
In the 21st century, the increase in the number of deceased donors and organ transplants has not been as significant as before. In 2004, there were 14,154 donors (11% increase from 2001), 27,040 transplants (11% increase from 2001), and 87,146 patients on the waiting list (10% increase from 2001). In the last decade (2004–2013), the increases in the numbers of donors and transplants have been minimal or small (a 0.7% increase in donors, and a 7% increase in transplants). The increased number of transplants despite virtually no increase in the number of donors is associated with (i) the liberalization of acceptance criteria of ‘high-risk’, ‘marginal’, or ‘extended criteria’ donors, and (ii) the utilization of more organs from a single donor. However, during this period, there was a 39% increase in the number of patients on the waiting list, which rose to approximately 122,000 [1,2].
The improved medical care that results in the substantial increase in patients on the waiting list is a great economic burden to the US (and to other Western countries). For example, Medicare covers the costs of care for end-stage renal disease regardless of patient age. In 2011, over 500,000 people took advantage of this benefit at a cost of over US$34 billion, which is more than 6% of Medicare’s entire budget [4]. If we add the cost of care for other end-stage organ failures, $US400 billion is spent each year, which is equivalent to almost 60% of Medicare’s budget.
According to the World Health Organization, >114,000 organ transplants are carried out annually in the world [5,6], which is <10% of global needs. The most frequently transplanted organ is the kidney, which accounts for 68% of the total organ transplants. Deceased donors account for 60–65% of all transplanted kidneys in many countries. However, this rate drops to 5–17% in regions where deceased donation is uncommon for religious or cultural reasons, such as the Middle East, Indonesia, and Japan. Although the best donation rate in deceased organs (both donation after brain and cardiac deaths) is achieved in Spain (36 per million population), organ shortage remains a major big problem in Europe [6]. Unfortunately, organ donation does not significantly increase in countries with a highly-educated population. In several developed countries, organ donation per million remains disappointingly low. For example, in Japan the organ donation rate is only 4 per million. In most Western countries, it is less than optimal, e.g., in Switzerland it is 12 per million, in Canada 15, in the UK 18, and in the US 24 [7].
The donation rate is critical where the needs are greatest, such as in India (1 donor per million population) and in China (0.5 donor per million population). In China, about 300,000 patients would benefit from organ transplants annually, but only about 10,000 transplants are currently carried out [8], which makes the ratio of supply to demand for organ transplants 1:304. However, statistics from the World Health Organization show that the mean ratio of organ supply to demand worldwide is 1:25 [9].
In addition, in the US, approximately 30 million patients suffer from diabetes (Types 1 and 2), and millions more from other disorders that might be potentially amenable to treatment by cell or tissue transplantation, e.g., neurodegenerative diseases. Worldwide, the impact is even greater since an estimated 340 million people are afflicted by diabetes alone [10].
Although corneal allotransplantation is readily available in the U.S. and in certain other countries of the developed world, the worldwide need for human donor corneas far exceeds supply, especially in China, India, Korea, and Japan, where cultural and religious concerns make it difficult to obtain corneas from human cadavers [11]. For example, in China, there are an estimated 4 million people in need of corneal transplantation.
The increased utilization of living organ donors has helped, particularly in countries where there is cultural resistance to deceased organ donation, e.g., Japan, but this has had relatively little impact on the overall need for organs; some organs, of course, e.g., the heart, clearly can only be obtained from deceased donors. Moreover, the shortage of deceased donors and the relative success of organ transplants from living donors resulted in the problem of organ trafficking, which remains a problem in some parts of the world. It is estimated that 5–10% of kidney transplants worldwide result from commercial transactions between a potential recipient and a paid living donor [12]. The organ shortage has also lead to the use of organs from executed prisoners in some countries [13]; whether truly informed consent has been obtained remains controversial.
It is clear that the current law, rate of organ donation (both deceased and living), and liberalized acceptance criteria (i.e., use of high-risk donors, marginal, or extended criteria donors) are not enough, and will never be enough to overcome the problem of organ shortage.
POTENTIAL OF XENOTRANSPLANTATION
Xenotransplantation, i.e., cross-species transplantation, using pig organs, could resolve the shortage of suitable donor organs [14,15]. If pig organs or cells could be transplanted successfully into human patients, the advantages would be numerous (Table 1).
Table 1.
Major advantages of pig organ, tissue, or cell xenotransplantation*
| Pigs would be ethically acceptable sources of organs and cells to many of the world’s population |
| Pigs are easy to breed and have large litters |
| Pig organs have similarities to human organs in respect of anatomy and physiology |
| Pigs could provide an unlimited supply of organs, tissues, and cells |
| The unlimited supply will allow transplantation procedures in ‘borderline’ candidates who might otherwise be declined |
| Organs will be available immediately and electively |
| The detrimental effects of brain death on donor organs will be avoided |
| When bred and housed under ‘clean’ conditions, pigs could provide exogenous infection-free organs, tissues, and cells |
| The ‘cultural’ barriers to deceased human donation present in some countries, e.g. Japan, will be obviated |
| Illegal organ trafficking and the use of organs from executed prisoners will be obviated |
| Organ donation by living donors, with its potential life-threatening complications, will be avoided |
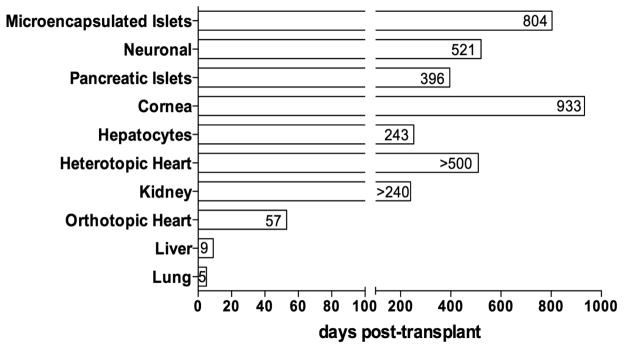
Ethically, pigs represent an acceptable choice as an alternative source of organs for humans [14,16]. An estimated 100 million pigs are slaughtered in the US each year as sources of meat, and 600 million are killed in China to provide heparin. Immunologically, however, the pig is less desirable than the nonhuman primate as a source of organs and cells because of the genetic distance between pigs and humans. The clinical application of xenotransplantation has been held back because it has proved difficult to prevent immune injury of pig grafts, a subject that is discussed by several authors elsewhere in this issue. Most major advances that have been made in this field have resulted from the introduction of genetically-engineered pigs or novel immunosuppressive agents. The current reported survival periods of various pig organ and cell transplants in nonhuman primates are indicated in Figure 2.
Figure 2. Longest reported survival times of pig organ and cell xenotransplantation in preclinical trials (pig-to-nonhuman primate models).
Microencapsulated pancreatic islets = 804 days (with re-Tx), 250 days (without re-Tx) (Sun et al [35]) (wild-type [WT] pigs); Neuronal cells = >521 days (Badin et al [31]) (CTLA4-Ig transgenic pigs); pancreatic islets = 396 days (van der Windt et al [36]) (hCD46 pigs); cornea (full thickness) = >933 days (Choi et al [37]) (WT pigs); hepatocytes = 243 days (with re-Tx), 80 days (without re-Tx) (Nagata et al [38]) (WT pigs); heterotopic heart = >500 days (Mohiuddin et al [18]) (GTKO/hCD46/hTBM pigs); kidney = >240 days (Tector AJ, personal communication) (GTKO/hCD55 pigs); orthotopic heart = 57 days (McGregor et al [19]) (GTKO/hCD55 pigs); liver = 9 days (Kim K et al [28]) (hCD55 pigs); lung = 5 days (Cantu et al [29]) (vWF-deficient pigs). Figure modified from Ekser B et al. [15].
Even if the remaining immunological and biological barriers can be resolved, which seems increasingly likely, the question needs to be asked as to whether pig organs will function adequately when transplanted to a human host. Ibrahim et al [17] have discussed selected physiological compatibilities and incompatibilities between humans and pigs, and these will be briefly reviewed here.
Heart
Anatomically, the pig heart is similar, although not identical, to the human heart. Physiologically, cardiac output and stroke volume, which are major indicators of cardiac function, have been reported to be comparable in pig and human [17]. Mean arterial pressure, heart rate, and myocardial blood flow are also nearly identical in the two species. The upright posture in humans, in contrast to pigs, does have an evolutionary impact on the structure of heart valves but this issue has been proved to be an insignificant problem in pig-to-nonhuman primate studies [18,19]. The different action potential of cardiomyocytes related to morphological differences in the atrioventricuar node between species might potentially result in increased arrhythmogenicity of a pig heart transplanted into a human, but observations of pig hearts functioning in nonhuman primates for prolonged periods have not indicated that this will be a problem [17,18].
Kidney
The kidney has a major role in maintaining homeostasis, excretion of metabolites, electrolyte balance, regulating body fluid and osmolarity. Pig kidney anatomy is remarkably similar to the human kidney. The maximum concentrating ability (1080 mOsm/L) and glomerular filtration rate (126–175 ml/h) of porcine kidneys are similar to those of human kidneys [17]. Kidney function in healthy humans and α1,3-galactosyltransferase gene-knockout (GTKO) pigs is compared in Table 2. Although serum potassium is slightly higher in pigs, the other serum electrolytes, creatinine, and urea nitrogen are similar between pig and human. Proteinuria has been identified as an important complication after pig kidney xenotransplantation [20–22], but recent evidence suggests it is associated with continuing immune activation of the kidney [Iwase H, et al, personal communication]. Pig kidneys have been demonstrated to adequately maintain homeostasis, electrolyte balance, and osmolarity in nonhuman primates [20,23].
Table 2.
Comparison of kidney function between healthy humans and GTKO pigs*
| Human | GTKO** Pig | |
|---|---|---|
| Sodium (mmol/L) | 136–146 | 144 |
| Potassium (mmol/L) | 3.5–5.0 | 5.3 |
| Chloride (mmol/L) | 95–110 | 103.0 |
| Calcium (mg/dL) | 8.4–10.2 | 10.8 |
| Phosphorus (mg/dL) | 2.5–4.5 | 8.8 |
| CO2 (mmol/L) | 21–32 | 28.1 |
| Urea (mg/dL) | 5.0–20.0 | 12.8 |
| Creatinine (mg/dL) | 0.6–1.1 | 1.1 |
Adapted from Ekser et al. [26].
GTKO = α1,3-galactosyltransferase gene-knockout.
Liver
Pig liver anatomy is slightly different from human liver anatomy. The pig liver has 3 lobes - the right lateral, the median, and the left lateral lobes. The median lobe is further subdivided by a deep umbilical fissure, which extends almost to the hilum [24]. The inferior vena cava is intraparenchymal and runs within the caudate lobe.
The liver has diverse functions, ranging from the synthesis of many vital proteins, coagulation factors, and biochemical molecules to detoxification of harmful substances. Table 3 compares liver function in healthy humans and pigs. Although there are several similarities in hepatic function, alkaline phosphatese (ALP), lactate dehydrogenase (LDH), and gamma glutamyltransferase (GGT) are higher in pigs [25,26]. It is more important, however, to demonstrate that similarities should not be limited to the measurement of enzyme levels, but should compare function as well. Studies by Ekser et al [27], and Kim et al [28] suggest that a pig liver may function adequately in a nonhuman primate, producing coagulation factors that maintain a normal coagulation profile.
Table 3.
Comparison of liver function in healthy humans and GTKO pigs*
| Human | GTKO Pig | |
|---|---|---|
| AST (IU/L) | <40 | 37.0 |
| ALT (IU/L) | <40 | 42.0 |
| ALP (IU/L) | 38–126 | 272 |
| LDH (IU/L) | <170 | 472 |
| GGT (IU/L) | <40 | 74 |
| Tot Bilirubin (mg/dL) | 0.3–1.5 | 0.2 |
| Dir Bilirubin (mg/dL) | 0.1–0.4 | 0.1 |
| Tot Protein (g/dL) | 6.3–7.7 | 5.9 |
| Albumin (g/dL) | 3.4–5.0 | 3.4 |
| Cholesterol (mg/dL) | <200 | 81 |
| Triglyceride (mg/dL) | <150 | 31 |
| Glucose (mg/dL) | 70–99 | 89 |
| PTT (sec) | 22.7–35.6 | 34.1 |
| PT (sec) | 11.3–14.5 | 13.6 |
| INR | 0.8–1.2 | 1.1 |
| D-dimer (micg/mL) | <0.45 | 0.20 |
| Fibrinogen (mg/dL) | 200–400 | 250 |
| Coagulation Factors (U/mL) | ||
| Factor II | 0.7–1.3 | 1.12 |
| Factor V | 0.7–1.5 | 6.02 |
| Factor VII | 0.6–1.6 | 2.36 |
| Factor VIII | 0.6–1.5 | 6.06 |
| Factor IX | 0.6–1.5 | 4.18 |
| Factor X | 0.7–1.5 | 1.97 |
| Factor XI | 0.6–1.4 | 4.07 |
| Factor XII | 0.5–1.7 | 4.95 |
| Plasminogen (%) | 75–150 | 3 |
| Protein C (%) | 70–140 | 11 |
| Protein S (%) | 58–128 | 11 |
| Anti-thrombin III (%) | 80–120 | 71 |
AST= aspartate transaminase, ALT= alanine transaminase, ALP= alkaline phosphatase, LDH= lactate dehydrogenase, GGT= gamma glutamyltransferase, INR= international normalized ratio, PT= prothrombin time, PTT= partial thromboplastin time, WT= wild-type, GTKO= α1,3-galactosyltransferase gene knock-out.
Lung
Although experimental experience with the xenotransplantation of pig lungs is limited, in part relating to the severe vasoconstriction that occurs in the newly-transplanted lungs, the pig lung has been demonstrated to provide adequate oxygenation and carbon dioxide exchange in nonhuman primates [29]. The upright posture of humans may also have an impact of physiological function of the pig lung after xenotransplantation. However, due to the limited survival achieved with pig lungs in nonhuman primates (<5 days), no definite conclusions can be made.
Pancreatic Islets
Porcine insulin differs from human insulin by only one amino acid, and is functionally comparable to human insulin. Porcine insulin was used for decades to treat patients with diabetes. There is good evidence, therefore, that well-functioning pig islets will be able to maintain normoglycemia in diabetic patients [30].
Neuronal cells
Although there is only one significant study, the evidence is that porcine dopamine-producing cells can reverse the clinical features of a Parkinson-like disease in monkeys [31].
Corneas
There are similarities between pig and human corneas (Table 4).
Table 4.
Comparison of parameters of corneas between humans and pigs*
| Human | Pig | ||
|---|---|---|---|
| Diameter (mm) | |||
| horizontally | 11.7 | 14.9 | |
| vertically | 10.6 | 12.4 | |
| Thickness (μm) | |||
| center | 536 | 666 | |
| periphery | 593 | 714 | |
| Reactive power (diopter) | 43.0 | 40.4 | |
| Tensile strength (MPa) | 3.81 | 3.70 | |
| Stress-strain pattern(a) | α | 42.8 | 39.3 |
| β | 2.97 | 2.97 | |
| Stress-relaxation pattern(b) | P(x100) | 85.6 | 64.6 |
| K(−) | 0.0165 | 0.0553 | |
| 1000s | 32% | 59% |
α is a scale factor. β represents the exponent of the nonlinear relationship between stress and strain
P is the value of G (t) at the end of the stress-relaxation test. K is the slope of fitted G (t)-In t line.
Adapted from Hara and Cooper [11].
CONCLUSIONS
Organ shortage is an undeniable problem in organ transplantation and is increasingly problematic. Even if we are able to increase donation rates significantly, allotransplantation will never be able to provide sufficient islets for all diabetic patients. As discussed elsewhere in this issue, approaches such as stem cell therapy or bioengineered devices are not sufficiently successful yet to consider as an alternative to allotransplantation. Xenotransplantation is much closer to meaningful clinical trials, and these could be initiated either through cellular xenotransplantation [15,30,31] or as a ‘bridge’ to liver [32] or heart [33] allotransplantation.
HIGHLIGHTS.
In the US each day, 30 dead or sick patients are removed from the waiting list
The available donors are not enough to overcome the global organ shortage
Pigs represent an alternative source of organs for humans
The pig could be a satisfactory source of organs for clinical transplantation
New technologies are facilitating the genetic engineering of pigs
Acknowledgments
FUNDING
Work on xenotransplantation in the Thomas E. Starzl Transplantation Institute at the University of Pittsburgh has been supported in part by National Institutes of Health grants U01 AI068642, R21 AI074844, and U19 AI090959, and by sponsored research agreements between the University of Pittsburgh and Revivicor, Inc., Blacksburg, VA.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTION
BE, DKCC, AJT – all participated in review of the literature, writing of the manuscript, and final approval of the manuscript
GUARANTOR
Burcin Ekser, MD, PhD
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.UNOS - United Network for Organ Sharing (UNOS) [Last accessed on February 10th, 2015]; http://www.unos.org.
- 2.OPTN - Organ Procurement and Transplantation Network. [Last accessed on February 10th, 2015]; http://optn.transplant.hrsa.gov.
- 3. [Last accessed in February 10, 2015];NIH Archives. http://history.nih.gov/research/downloads/PL98-507.pdf.
- 4.USRDS. [Last accessed in February 10, 2015];United States Renal Data System Annual Data Report. 2013 http://www.usrds.org/2013/pdf/v2_ch11_13.pdf.
- 5.López-Fraga M, Domínguez-Gil B, Capron AM, Van Assche K, Martin D, Cozzi E, et al. A needed convention against trafficking in human organs. Lancet. 2014;383:2187–2189. doi: 10.1016/S0140-6736(14)60835-7. [DOI] [PubMed] [Google Scholar]
- 6.Newsletter Transplant. [Last accessed in February 10, 2015];International figures on donation and transplantation in 2012. https://www.edqm.eu/site/newsletter_transplant_vol_18_no_1_september_2013pdf-en-31256-2.html.
- 7.Global Observatory on Organ Donation and Transplantation. [Last accessed on February 10, 2015];Data reports, 2012 data. http://www.transplant-observatory.org/Pages/Data-Reports.aspx.
- 8.Sui W, Zheng C, Yang M, Dai Y. Organ donation in China: current status, challenges, and future development. Prog Transplant. 2014;24:375–380. doi: 10.7182/pit2014730. [DOI] [PubMed] [Google Scholar]
- 9.White SL, Hirth R, Mahíllo B, Domínguez-Gil B, Delmonico FL, Noel L, et al. The global diffusion of organ transplantation: trends, drivers and policy implications. Bull World Health Organ. 2014;92:826–835. doi: 10.2471/BLT.14.137653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. [Last accessed on February 7, 2015];WHO Diabetes Programme. http://www.who.int/diabetes/en/
- 11.Hara H, Cooper DK. Xenotransplantation--the future of corneal transplantation? Cornea. 2011;30:371–378. doi: 10.1097/ICO.0b013e3181f237ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Budiani-Saberi DA, Delmonico FL. Organ trafficking and transplant tourism: a commentary on the global realities. Am J Transplant. 2008;8:925–929. doi: 10.1111/j.1600-6143.2008.02200.x. [DOI] [PubMed] [Google Scholar]
- 13.Sharif A, Singh MF, Trey T, Lavee K. Organ procurement from executed prisoners in China. Am J Transplant. 2014;14:2246–2252. doi: 10.1111/ajt.12871. [DOI] [PubMed] [Google Scholar]
- 14.Cooper DK, Gollackner B, Sachs DH. Will the pig solve the transplantation backlog? Annu Rev Med. 2002;53:133–147. doi: 10.1146/annurev.med.53.082901.103900. [DOI] [PubMed] [Google Scholar]
- 15.Ekser B, Ezzelarab M, Hara H, van der Windt DJ, Wijkstrom M, Bottino R, et al. Clinical xenotransplantation: the next medical revolution? Lancet. 2012;379:672–683. doi: 10.1016/S0140-6736(11)61091-X. [DOI] [PubMed] [Google Scholar]
- 16.Cooper DK, Ye Y, Rolf LJ, et al. The pig as potential organ donor for man. Chapter 30. Heideiberg: 1991. Xenotransplantation; pp. 481–500. [Google Scholar]
- 17.Ibrahim Z, Busch J, Awwad M, Wagner R, Wells K, Cooper DKC. Selected physiological compatibilities and incompatibilities between human and porcine systems. Xenotransplantation. 2006;13:488–499. doi: 10.1111/j.1399-3089.2006.00346.x. [DOI] [PubMed] [Google Scholar]
- 18.Mohiuddin MM, Singh AK, Corcoran PC, Hoyt RF, Thomas ML, 3rd, Ayares D, et al. Genetically engineered pigs and target-specific immunomodulation provide significant graft survival and hope for clinical cardiac xenotransplantation. J Thorac Cardiovasc Surg. 2014;148:1106–1113. doi: 10.1016/j.jtcvs.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McGregor CG, Byrne GW, Vlasin M, et al. Early cardiac function and gene expression after orthotopic cardiac xenotransplantation. Xenotransplantation. 2009;16:356. (Abstract IXA-O-2.4) [Google Scholar]
- 20.Soin B, Smith KG, Zaidi A, Cozzi E, Bradley JR, Ostlie DJ, et al. Physiological aspects of pig-to-primate renal xenotransplantation. Kidney Int. 2001;60:1592–1597. doi: 10.1046/j.1523-1755.2001.00973.x. [DOI] [PubMed] [Google Scholar]
- 21.Yamada K, Yazawa K, Shimizu A, Iwanaga T, Hisashi Y, Nuhn M, et al. Marked prolongation of porcine renal xenograft survival in baboons through the use of alpha1,3-galactosyltransferase gene-knockout donors and the cotransplantation of vascularized thymic tissue. Nat Med. 2005;11:32–34. doi: 10.1038/nm1172. [DOI] [PubMed] [Google Scholar]
- 22.Tasaki M, Shimizu A, Hanekamp I, Torabi R, Villani V, Yamada K. Rituximab treatment prevents the early development of proteinuria following pig-to-baboon xeno-kidney transplantation. J Am Soc Nephrol. 2014;25:737–744. doi: 10.1681/ASN.2013040363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cowan PJ, Cooper DKC, d’Apice AJF. Kidney xenotransplantation. Kidney Int. 2014;85:265–275. doi: 10.1038/ki.2013.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Court FG, Wemyss-Holden SA, Morrison CP, Teague BD, Laws PE, Kew J, et al. Segmental nature of the porcine liver and its potential as a model for experimental partial hepatectomy. Br J Surg. 2003;90:440–444. doi: 10.1002/bjs.4053. [DOI] [PubMed] [Google Scholar]
- 25.Ekser B, Echeverri GJ, Hassett AC, Yazer MH, Long C, Meyer M, et al. Hepatic function after genetically engineered pig liver xenotransplantation in baboons. Transplantation. 2010;90:483–493. doi: 10.1097/TP.0b013e3181e98d51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ekser B, Bianchi J, Ball S, Iwase H, Walters A, Ezzelarab M, et al. Comparison of hematologic, biochemical, and coagulation parameters in α1,3-galactosyltransferase gene-knockout pigs, wild-type pigs, and four primate species. Xenotransplantation. 2012;19:342–354. doi: 10.1111/xen.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ekser B, Long C, Echeverri GJ, Hara H, Ezzelarab M, Lin CC, et al. Impact of thrombocytopenia on survival of baboons with genetically modified pig liver transplants: clinical relevance. Am J Transplant. 2010;10:273–285. doi: 10.1111/j.1600-6143.2009.02945.x. [DOI] [PubMed] [Google Scholar]
- 28.Kim K, Schuetz C, Elias N, Veillette GR, Wamala I, Varma M, et al. Up to 9-day survival and control of thrombocytopenia following alpha1,3-galactosyl transferase knockout swine liver xenotransplantation in baboons. Xenotransplantation. 2012;19:256–264. doi: 10.1111/j.1399-3089.2012.00717.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cantu E, Balsara KR, Li B, et al. Prolonged function of macrophage, von Willibrand factor-deficient porcine pulmonary xenografts. Am J Transplant. 2007;7:66–75. doi: 10.1111/j.1600-6143.2006.01603.x. [DOI] [PubMed] [Google Scholar]
- 30.van der Windt DJ, Bottino R, Kumar G, Wijkstrom M, Hara H, Ezzelarab M, et al. Clinical islet xenotransplantation: how close are we? Diabetes. 2012;61:3046–3055. doi: 10.2337/db12-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Badin RA, Padoan A, Vadori M, et al. Long-term clinical recovery in parkinsonian monkey recipients of CTLA4-Ig transgenic porcine neural precursors. Transplantation. 2010;90(supplement 2):47. (Abstract LB-3288) [Google Scholar]
- 32.Ekser B, Gridelli B, Tector AJ, Cooper DK. Pig liver xenotransplantation as a bridge to allotransplantation: which patients might benefit? Transplantation. 2009;88:1041–1049. doi: 10.1097/TP.0b013e3181ba0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooper DK, Teuteberg JJ. Pig heart xenotransplantation as a bridge to allotransplantation. J Heart Lung Transplant. 2010;29:838–840. doi: 10.1016/j.healun.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 34.Cooper DK, Ayares D. The immense potential of xenotransplantation in surgery. Int J Surg. 2011;9:122–129. doi: 10.1016/j.ijsu.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 35.Sun Y, Ma X, Zhou D, Vacek I, Sun AM. Normalization of diabetes in spontaneously diabetic cynomologus monkeys by xenografts of microencapsulated porcine islets without immunosuppression. J Clin Invest. 1996;98:1471–1422. doi: 10.1172/JCI118929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van der Windt DJ, Bottino R, Casu A, et al. Long-term controlled normoglycemia in diabetic non-human primates after transplantation with hCD46 transgenic porcine islets. Am J Transplant. 2009;9:2716–2726. doi: 10.1111/j.1600-6143.2009.02850.x. [DOI] [PubMed] [Google Scholar]
- 37.Choi HJ, Lee JJ, Kim DH, Kim MK, Lee HJ, Ko AY, et al. Blockade of CD40–CD154 costimulatory pathway promotes long-term survival of full-thickness porcine corneal grafts in nonhuman primates: clinically applicable xenocorneal transplantation. Am J Transplant. 2015;15:628–641. doi: 10.1111/ajt.13057. [DOI] [PubMed] [Google Scholar]
- 38.Nagata H, Nishitai R, Shirota C, et al. Prolonged survival of porcine hepatocytes in cynomolgus monkeys. Gastroenterology. 2007;132:321–329. doi: 10.1053/j.gastro.2006.10.013. [DOI] [PubMed] [Google Scholar]