Abstract
Small eating behavior changes are proposed as more feasible to achieve and maintain than larger changes used in traditional behavioral weight loss studies. However, it is unclear whether overweight Black and Hispanic adults in a low-income urban setting experience small changes as feasible and what might influence feasibility. Participants' experiences in a 12-week pilot weight loss intervention were explored qualitatively to determine the feasibility of making small eating behavior changes in this population. After the intervention (69% retention), semi-structured interviews with 46 men and women (mean age 51, 50% Non-Hispanic Black, 43% Hispanic) revealed that making small eating changes was a process shaped by participants' intrapersonal and interpersonal eating environments. Participants responded to intrapersonal and interpersonal eating environmental challenges by adapting small change strategies, navigating eating environments, and negotiating household eating practices. Findings highlight how even small eating behavior changes called for adaptation, navigation, and negotiation of complex eating environments in daily life. These findings were used to improve the trial that followed and underline the importance of feasibility studies to inform community trials. Findings also add to understanding of contextual challenges and the skills needed to implement small changes in a low income, ethnic minority population.
Keywords: Weight loss intervention, Obesity, African American or Black, Hispanic or Latino, Small change, Qualitative
1. Introduction
Initially proposed as a method to prevent weight gain, a small change approach advocates small, but cumulative, lifestyle changes that may be easier to achieve and sustain than larger changes endorsed in traditional behavioral weight loss studies (Hill, 2009). Examples of typical large behavioral changes recommended to reduce weight include reducing caloric intake by 500–1000 kcal/day or increasing step count by as much as 8000 steps a day (National Heart, Lung, and Blood Institute, 2000). The small change approach has demonstrated effectiveness for weight loss among men and women in community (Lutes et al., 2012, 2008) and veteran populations (Damschroder, Lutes, Goodrich, Gillon, & Lowery, 2010; Damschroder et al., 2014), and in one-on-one, group, telephone, and worksite settings (Zinn, Schofield, & Hopkins, 2012). Successful small change interventions have also engaged vulnerable and medically complex populations (Damschroder et al., 2014), though in predominantly non-Hispanic white populations.
A small change approach may be appropriate in low-income and racial and ethnic minority populations (e.g. Tate et al., 2012) who, despite disproportionately high prevalence of obesity (Flegal, Carroll, Ogden, & Curtin, 2010), have been underrepresented in randomized controlled trials to reduce weight and have tended to achieve less weight loss in traditional behavioral interventions compared with their non-Hispanic White counterparts (Kumanyika, Obarzanek, Stevens, Hebert, & Whelton, 1991; West, Prewitt, Bursac, & Felix, 2008). These outcomes have raised questions about transferability of interventions across socially, culturally, and economically diverse populations (Diaz, Mainous, & Pope, 2007; Kumanyika, 2008; Kumanyika et al., 1991). Differences in treatment effectiveness across diverse populations (e.g. West et al., 2008) may be due, in part, to difficulties making and sustaining large behavior changes called for in traditional weight loss interventions in environments particularly unsupportive of managing weight (Swinburn & Egger, 2004). In low-income and racial and ethnic minority populations, these unsupportive environments may include the increased likelihood of living in neighborhoods with limited access to stores with affordable healthful food options and safe places to be active (Taylor, Poston, Jones, & Kraft, 2006).
The pilot weight loss intervention in the present study, Small Changes and Lasting Effects (SCALE), specifically targeted overweight Black and Hispanic adults in a low-income urban setting. SCALE was anchored in behavior changing strategies informed by food psychology, behavioral economics, and prior experiment. The strategies comprised health-promoting simple decision rules and modifications to the home eating environment (Wansink, 2004, 2010; Wansink, Just, & Payne, 2009) aimed at disrupting habitual and environmentally driven unhealthy eating behaviors (Cohen & Farley, 2008; van't Riet, Sijtsema, Dagevos, & De Bruijn, 2011) and building a bias towards healthy eating. One home eating environment modification strategy in SCALE advised storing snack foods out of sight (in a cupboard or pantry), to remove the environmental cue to eat when foods are conveniently in sight (Painter, Wansink, & Hieggelke, 2002). One SCALE simple decision rule strategy was to drink noncaloric beverages in place of sugar sweetened beverages, whose consumption is higher among Blacks and Hispanics and low-income populations (Han & Powell, 2013) and is linked to weight gain (Malik, Schulze, & Hu, 2006).
It is worth noting that, to date, small change studies have used two different but related approaches to operationalize “small”. The first approach operationalizes “small” by focusing on achieving small caloric deficits (100–200 kcal/day) through minimal reductions in food intake or boosts in energy expenditures (e.g. Damschroder et al., 2010; Lutes et al., 2008), usually tracked through food and exercise logs. The second approach equates “small” with simple behavioral strategies designed to be convenient and minimally demanding to implement. These strategies usually attempt to address specific environmental cues and pressures to eat (Gorin et al., 2013; Wansink et al., 2009) and might also result in more than a “small” caloric deficit. For example, Tate et al. (2012) evidenced a caloric deficit of ~270 kcal/day when individuals swapped caloric beverages for diet beverages. SCALE used the second of these two “small” change approaches, operationalizing “small” with simple behavioral strategies. Though the small eating behavior change strategies employed in the SCALE pilot intervention were proposed as more feasible, feasibility studies in real-life settings had not been conducted in this population and it was unclear whether participants would experience small changes as qualitatively easy to implement.
The objective of this research was to explore the feasibility of small eating behavior changes for overweight Black and Hispanic adults in an urban low-income setting. Using semi-structured qualitative interviews conducted at the end of the 12 week pilot intervention, this work examined participants' experiences making small eating behavior changes in the SCALE pilot with the aim of understanding small change feasibility and what influences that feasibility. To the authors' knowledge, this project is one of the first studies to qualitatively examine small eating behavior change feasibility in Black and Hispanic adults with the goal of building a better understanding of what shapes real world dietary change in this population. This study adds to understanding of environmental influences on eating behavior change to promote weight loss among Black and Hispanic populations. The pilot findings were used to modify and adapt the intervention procedures for the randomized control trial that followed.
2. Methods
2.1. SCALE setting and design
The data presented in this paper come from a semi-structured survey following the SCALE pilot study. The SCALE pilot study was a 12-week behavioral intervention designed to examine the feasibility of making small changes in eating and physical activity behavior to promote weight loss in a sample of overweight Black and Hispanic adults from two lower-income neighborhoods in New York City, where more than 25% of residents are obese (Roberts, Kerker, Mostashari, Van Wye, & Thorpe, 2005). This analysis used data from participants' experiences making small eating behavior changes, henceforth referred to as small changes.
At enrollment in the pilot study, participants were asked to select one of six small change strategies. The small change strategies were informed by previous research on habits and environmental cues that promote unhealthy consumption (Cohen & Farley, 2008) and potential counteracting heuristics and home eating environment modifications (Downs, Loewenstein, & Wisdom, 2009; Wansink, 2004, 2010; Wansink et al., 2009). A list of small change strategies was first evaluated and adapted for sociocultural acceptability and feasibility by focus groups conducted in a similar population (Phillips-Caesar et al., 2015). The finalized strategies were: (1) use a smaller (9″ diameter) plate at main meal; (2) make sure vegetables comprise half of the plate at main meal; (3) substitute water for sugar sweetened beverages; (4) keep snack foods out of sight (for example, in cupboards); (5) eat breakfast every day; and (6) eat dinner at home at least six days a week. For a detailed description of each of the strategies, see Phillips-Caesar et al. (2015). Participants worked with trained race- and ethnicitymatched community health workers (CHWs) and, using a standardized protocol, selected a small change strategy they were confident they could carry out, after considering potential challenges. With a CHW, each participant then set a small change goal (for example, “I will use a small plate every day for lunch”). Participants were contacted by their assigned CHW via telephone once weekly for 12 weeks and CHWs were trained to utilize problem-solving therapy to identify and define challenges, brainstorm a range of solutions, and select a desirable alternative to achieve participants' goals (Perri et al., 2001). This study was approved by the institutional review boards at Lincoln Medical and Mental Health Center, Weill Cornell Medical College and Cornell University.
Participants were recruited from two churches and three healthcare sites via flyers, tabling at events, and referrals through site gatekeepers (such as a pastor or nurse). Participants were recruited from August 2010 through February 2011. To be eligible for the study, participants had to self-identify as Black or Hispanic, be adults at least 21 years of age, and have a body mass index higher than 25 kg/m2 but less than 50 kg/m2. Exclusion criteria included pregnancy, current enrollment in another weight loss program, planning to undergo weight loss surgery within the year, active cancer, inability to control own meal content, and presenting with other advanced or untreated illnesses that might prevent full participation. All participants provided written informed consent.
2.2. Survey design and data collection
At the end of the 12-week pilot intervention, participants were interviewed by a different CHW (or research staff, as needed), to reduce the likelihood of providing socially acceptable responses. The goal was to gather information about participants' experiences making small changes to their eating behaviors in the context of daily life to shed light on the feasibility of these changes. The open-ended semi-structured interview guide was informed broadly by the socio-ecological framework by probing for individual as well as social influences on small change (Sallis & Owen, 1997) and more specifically by themes from the preliminary focus group findings related to the sociocultural acceptability of the small change strategies (Phillips-Caesar et al., 2015). Domains of inquiry included experiences with small change strategy: selection; implementation (probing especially for barriers and facilitators); reception by family, friends, and other acquaintances; and suggested improvements.
102 participants were enrolled in the pilot, 93 participants completed goal setting, 64 completed the final interview, and 46 participants gave informed consent to audio record their final interviews. Final interviews lasted between 20 and 65 min and were conducted primarily at the church or health care sites.
2.3. Data analysis
Data analysis included only those 46 participants for whom final interviews were recorded. Each of the interviews was transcribed verbatim. Fourteen of the interviews were conducted in Spanish and, after being transcribed in Spanish, were translated into English and verified by a second translator. All participants were assigned pseudonyms. Transcripts were open coded by three researchers (LA, CD, JE). The constant comparative method was used to identify emergent themes and to iteratively develop a conceptual coherence of themes to represent participants' experiences with small eating behavior changes in the intervention (Strauss & Corbin, 1998).
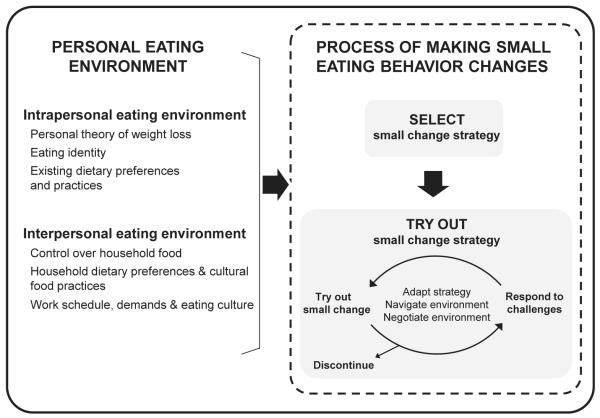
Consistent with the goal of understanding participants experiences with making small eating behavior changes, participants' descriptions of their experiences were first coded for barriers and facilitators encountered in making small changes (categories from focus groups) then for an additional emergent code for motivators. Consistent with a social ecological framework, these three codes were grouped into two emergent main categories: intrapersonal and interpersonal influences on participants' experiences, termed intrapersonal and interpersonal eating environments. Comparisons across interviews revealed instances where a single code might take the form of a barrier and a motivator for the same participant. Further analyses revealed this perceived discrepancy to be explained, in part, by the small change experience being characterized by somewhat distinct processes that included small change selection and trying out processes, whereby one aspect of the eating environment could motivate a participant to select a specific small change strategy, but subsequently pose a barrier in the trying out process. A process-oriented model was then developed, depicting the interrelated themes: intrapersonal and interpersonal eating environments acting as barriers, facilitators, and motivators along the process of making small changes and the tactics that were used by participants in this process. The quality and integrity of the analysis was strengthened by involvement of three researchers utilizing peer debriefing via regular research group meetings throughout the data analysis process and by soliciting feedback on preliminary interpretations from CHWs and other members of the research team.
3. Results
3.1. Participant characteristics
Twelve men and 34 women (total n = 46) participated in the audio-taped interviews. Participants were between the ages of 22 and 79 years (mean = 51). Half (n = 23) of the participants identified as non-Hispanic Black, 20 identified as Hispanic, and 3 participants identified their race as “other.” Half (n = 23) of the participants were not employed. Nineteen participants were married or living with a significant other in a long term relationship. Nine participants reported living alone; the median number of others living in the household was 2.1, but ranged from 0 to 11. Mean initial body mass index (BMI, kg/m2) based on CHW measured height and weight (NHLBI, 2000) was 34.5 kg/m2 and ranged from 25.8 to 49.4 kg/m2. Compared to all of those who completed the study, those who agreed to be recorded were less likely to identify as Hispanic, more likely to have attended college, and had fewer people living in their households. More than a third of participants selected the small plate strategy (n = 17), while a quarter selected the half plate vegetable strategy (n = 11). Seven participants chose to substitute water for sugar sweetened beverages (n = 7), five opted for placing snack foods out of sight (n = 5), five selected eating breakfast daily (n = 5), and only one participant chose eating dinner at home six days a week (n = 1).
3.2. Salient aspects of the intrapersonal eating environment
Personal theories of weight loss, eating identity, and existing eating practices all emerged as important components of participants' intrapersonal eating environments and were, to varying degrees, supportive or unsupportive of participants' implementation of their selected small change strategies (Fig. 1).
Fig. 1.
Conceptual model of the process of making small eating behavior changes. This figure illustrates how the process of making small eating behavior changes was shaped by salient aspects of intrapersonal and interpersonal eating environments and how participants responded to challenges from their eating environments.
3.2.1. Personal theory of weight loss
While the SCALE intervention curriculum explained how small eating changes could lead to weight loss, participants also held and discussed their own personal theories about the types of eating behavior changes they believed could produce a desired change in weight. These theories were usually informed by past advice from a health professional or previous experience with dieting attempts and weight loss. Some theories supported a small change approach, others challenged it.
Gloria (62 years, Black woman, small plate) explained: “… if you're going to try … to cut it [unhealthy food] all together, when you get it you're going to be greedy at it. I can't follow no strict diet. I said, I'm not even going to try because I'm going to mess up.” From her past experiences, strict dieting inevitably led to overeating. She hoped that “cutting down” the amount of unhealthy food, through using the small plate strategy, would be more sustainable. While Hector (46 years, Hispanic man) explained that the small change strategy he selected, eating breakfast daily, was supported by his doctor's recommendation to promote weight loss through regular eating instead of skipping meals: “… the doctor told me: I have to eat moderate, like three times a day at least.”
Some personal weight loss theories were at odds with the SCALE small change approach and tended to involve intensive dieting behaviors like eliminating all starches or red meat, or making many small changes at once. For example, Eloise's (65 years, Black woman, half plate vegetables) personal theory highlighted intense dieting measures which she perceived as more effective than small changes. After expressing disappointment with her weight loss in SCALE, she responded: “… I'm going to be drinking [diet product] milkshakes for the next three weeks. I'm serious, two milkshakes a day. And just have lettuce and tomato. I'm serious.”
3.2.2. Eating identity
Many participants communicated how self-images related to eating influenced their small change intervention experiences, describing themselves with words or phrases representing identities associated with salient eating practices, disease/health status, and geographic regions. Eating identity tended to inform the small change strategy that participants selected. For example, Eloise (65 years, Black woman) explained that her eating identity supported the half plate vegetable strategy that she chose: “… I like vegetables. I like cabbage, broccoli and stuff. I'm a Southerner, we like that.” For others, eating identity discouraged them from choosing an incompatible strategy. For example, Deborah (51 years, Black woman, half plate vegetable) said, “I love to eat food. I don't see myself eating a small plate [strategy].” Generally participants described selecting small change strategies that they saw as congruent with their eating identities.
3.2.3. Existing dietary preferences and practices
Intrapersonal eating environments were also characterized by participants' preferences for certain foods and food groups (particularly vegetables, salad, and water) and general practices like how and when foods were usually prepared, sometimes in accordance with eating identity or with specific health conditions like diabetes or high blood pressure.
“I enjoy cooking, so I cook most of it. So that's why a lot of itprobably more than half of it- was really fresh, to be honest with you. So I prepare my own food and I prepared it the right way and it was tasty and good.” [Walter, 56 years, Black man, half plate vegetables]
Others revealed that their selected strategy may not have been supported by current eating practices. For example, Gail (71 years, Black woman) selected substituting water for sugar sweetened beverages as her small change strategy, but revealed that she tended to order sugar sweetened beverages when eating outside of the home. And for many weeks during the intervention, she had been “mostly eating out.”
3.3. Salient aspects of the interpersonal eating environment
Salient aspects of participants' eating environments extended beyond individuals to include their interpersonal eating contexts (Fig. 1). Most commonly discussed were household and work eating environments and the concessions made to accommodate those social contexts, highlighting the importance of small change strategy compatibility with interpersonal eating environments.
3.3.1. Control over household food
Participants described varying levels of control over food related behaviors including food acquisition (or foods brought into the home), meal content, and food preparation. Control over food was often discussed in relationship to food roles, responsibilities, and caregiving duties including buying and preparing food for the household and extended family and acted to both constrain and facilitate small changes. Some participants reported having complete control over food, facilitating implementation of their eating behavior change strategy. For example, Walter reported, “I told her [his wife] what we were going to do and since I cook, she had no choice … She had to comply … If she wanted to eat.” Whereas Deborah ruled out hiding snacks knowing that she did not have control over them:
“That's not possible [hiding snack strategy] because my children, my family have snack everywhere. So that's a challenge for me … it's like they're adults and I have to respect them, I cannot really tell them, ‘Don't buy this because this is my house.’ I can do that, but I don't think it's ok. So that's the only thing, “cause they buy whatever they buy and it's there and sometimes you feel like eating it.”
3.3.2. Household dietary preferences and cultural food practices
Participants described how the food preferences and behaviors of others in the household and household food values created an eating context that shaped intervention experiences in both positive and negative ways. For some participants, watching how others were eating reinforced the desire to maintain their small eating behavior changes. Gloria: “To me it be a lot of food he [her husband] be eating … make me not want to eat when I look at his plate.” For other participants, usual household or cultural food practices undermined small eating behavior changes. Marco (46 years, Hispanic man, water) commented regarding his chosen small change “… I come from a custom of not drinking water” and that in his household water is not always a readily available option, making the strategy challenging to continuously carry out: “I will continue to avoid all those juices, these things that you are offered sometimes, but always are not offered alternatives, no?”
Complex household interactions with family members expressing verbal support, but also making things more challenging through their actions were common. For example, Diana (59 years, Hispanic woman, water) said, “Well my daughter's been pretty proud of me, so. My oldest daughter, she's the one that lives here … she said “Mom you know you're doing pretty good.” And also, “She'll [her daughter] buy a soda or a big bag of potatoes chips …. I won't drink it, because I know my sugar will zoom up. She's noticed, you know, that I'm more determined to do things a little bit better.””
3.3.3. Work schedule, demands, and eating culture
Participants' intervention experiences were also shaped by work schedules, demands, and the work food and eating culture. Carla (60 years, Black woman, small plate) described how a demanding work schedule and work assignment made it difficult for her to continue her small change strategy: “… I have a crazy schedule. I work evenings, Saturdays and Sundays. And that was the difficulty for me. My time schedule most of the time threw me off. And if I have a project I have to work on, that throws me off. You know I'm stressing with that grant, oh my God.” She also described how the work eating culture, in general, made it difficult to lose weight in a setting where sugary snacks and treats were often present, saying, “Like last week, we had all this cake.… this is the eating [office]; you can't lose weight in this [office].”
3.4. How intrapersonal and interpersonal eating contexts shaped process of making small changes
Two processes emerged as important experiences in the small change intervention: small change strategy selection and the trying out process. The next sections describe how both strategy selection and trying out processes were shaped by the intrapersonal and interpersonal eating environments.
3.4.1. Eating environments shaped strategy selection
Many participants described how selection of a small change strategy was informed by salient aspects of the eating environment. With knowledge of supportive or unsupportive aspects of their eating environment, participants selected or purposively avoided a specific small change strategy. For example, Edwin (65 years, Black man) selected eating breakfast based on his personal theory of weight loss:
“How did I decide this one? This way I won't eat any, no garbage, you know sweets and stuff like that … ‘Cause I know when you don't eat breakfast you ready to start eating some garbage the rest of the day.”’
Others recognized that their existing eating environments would not be supportive of specific strategies and selected another instead. For example, Alvin (58 years, Black man), who chronically skipped meals, chose not to attempt a strategy that would require “a conscious effort” like eating breakfast or dinner regularly, instead opting to try out the half plate vegetable strategy for the meals he was actually eating.
3.4.2. Eating environments shaped the trying out process
Making small changes was described as a trying out process, whereby participants figured out how their strategy meshed with their eating environment, sometimes in a series of trial and error. Participants were often met with challenges from eating environments in this process. To respond to challenges participants described tactics that fell into three major categories: adapting the strategy, navigating eating environments, and negotiating interpersonal eating environments (Fig. 1). These tactics allowed participants to avoid challenges and possibly capitalize on facilitative aspects. Participants then elected to continue or discontinue their strategy.
3.4.3. Adapting strategies
Participants reported adapting their strategy to carry it out in their eating environment. Adaptations ranged from simply not buying unhealthy snacks at all (instead of hiding them) or even replacing snacks with fruit or vegetables to modifying the small plate, half plate, and eat dinner at home strategies to their work setting by using appropriate containers and bringing food from home.
3.4.4. Navigating eating environments
Several participants also navigated their eating environments and opted to try out their strategy in settings where they had control over food and could get around food responsibilities and others' preferences, usually at work or during non-commensal meals. For some participants, having a supervisor or a work environment that was structurally supportive of his or her small change strategy facilitated the trying out process. Referring to his supervisors who allowed him to eat breakfast at his desk, Hector (46 years, Hispanic man) described, “… they know I work and I'm not goofing off so they let me do what I want to do.” Participants also got around their interpersonal eating environments by selectively disclosing their intervention participation only to specific people or only after a specific time period to avoid unwanted feelings of being judged or watched before building up confidence.
“I chose consciously not to speak about it, me personally. Because I know once I tell people, ‘Oh I'm going to watch my weight’, everybody is watching you watch your weight. It's too much pressure for me so I don't. I can do it with my sister but I don't do it here [office].” Carla
“… before, I was not comfortable. I didn't know what I was doing, but now I'm sure I'm gonna continue doing, so I can tell people.” Deborah
Participants also suggested that the CHWs were an important addition to their interpersonal eating environments, especially when family or close friends did not provide support. Participants described CHWs as being an important support system, but also making them feel accountable to someone supportive: “… like someone wants to, wanted to help you reach your goal … Like you wasn't by yourself.” Hector.
3.4.5. Negotiating eating environments
Participants negotiated interpersonal eating environments, especially control over food, to manage their food roles and responsibilities and household food preferences and practices and still accomplish their small change. Many participants described two tactics in particular: preparing two sets of meals or using their control over food to prepare healthy meals for the whole family.
“… I do not want to deprive nobody from anything because I can't have it. Then we're not going to be able to deal….I will prepare what they [her grandchildren] have to eat and I prepare my food and we eat. I eat my stuff and they eat theirs because I'm the one that's going to get sick [diabetes symptoms].” Rhonda (54 years, race/ethnicity listed as Other, small plate)
Deborah leveraged control over evening meals to contend with her family members' less healthy food preferences and practices and support her small change (half plate vegetables): “The way I'm cooking and the way I'm buying food is helping … I cook plenty of vegetable and I bake sometimes. So they [family] have no choice than eat what is there.”
Gloria described asserting food control within her food responsibilities to accomplish her small eating behavior change strategy: “… he [her husband] might say, ‘You going to cook some macaroni and cheese?’ And I tell him I'm not cooking that because I'm not eating all of that …”
3.4.6. Responding to challenges and continuing a strategy
The tactics used by participants to facilitate strategy implementation were usually to respond to challenges from the interpersonal eating environments and integrate the strategy into some aspect of their daily life. Some participants were able to integrate their strategies and continue through the course of the intervention. Deborah, for example expressed, “I'm going to continue doing this [using the half plate vegetable strategy] from now on.” Others struggled, due in part to, overwhelming challenges from the eating environment.
Some participants suggested that it became easier to make the small change over the course of the intervention. For example, when asked whether he experienced challenges in making small changes implementation, Bruce (48 years, Black man, small plate) remarked: “In the beginning, not now.”
3.4.7. Responding to challenges and abandoning a strategy
Sometimes participants tried and were unable to overcome their challenges, Tiffany (30 years, Black woman, half plate vegetables) described using several tactics to respond to a variety of eating environment challenges, but in the end, her strategy was not feasible: “I thought it would be easy, but it's more easier said than done. ‘Cause I have children and the older son don't like vegetables …So it's hard for me to cook food according to that, ‘cause everyone don't eat the same thing, so I don't wanna make too many meals … You know, waste food.” She did begin to make separate dishes, but eventually abandoned this approach due to increased effort and waste. She also tried out her small change during the day, a time when she had more control over food. However, she described making vegetables every day as a “hard task” and opted instead to visit a restaurant daily, “to eat lunch and try to get a half salad.” But that “became costly.” Ultimately, she abandoned that adaptation and her small change.
Cora (46 years, Hispanic woman), the main food preparer in her home, describes being met with conflict when trying to integrate eating behavior changes in the household, “I think for my family it was difficult … almost everyone rejected the changes. Food that I started to eat was not received well.” She ended up selecting a small change strategy that did not affect her family, using a smaller plate for her main meal.
4. Discussion
The SCALE weight loss intervention pilot provided an opportunity to investigate the feasibility of making small eating behavior changes from the point of view of overweight Black and Hispanic adults by qualitatively exploring their experiences making small changes in the context of their everyday lives. This research describes how the feasibility of making small changes was shaped by participants' intrapersonal and interpersonal eating environments. Themes highlight how even small behavior change strategies such as healthy eating rules of thumb or home environment modifications called for tactics like adapting the strategy, and navigating and negotiating the eating environment to carry out in the context of daily life. These findings are discussed and interpreted in relation to relevant literature, theoretical concepts, and improving the trial phase of the intervention.
When participants described complex eating environments that reflected both intrapersonal and interpersonal influences on the process of selecting and trying out their small changes, no one contextual factor was salient for all participants and many themes operated simultaneously to characterize a more complex version of participants' eating environments. Consistent with socialecological models of influences on health and eating behaviors, themes span two proximal dimensions: within-person and interpersonal; and highlight two physical settings: the home eating context and the work eating environment (Sallis & Owen, 1997; Swinburn & Egger, 2004). This research helps us to identify specific aspects of these two environments within a socio-ecological framework that are important to consider in this population and address in intervention design and implementation to facilitate small change feasibility.
Intrapersonal eating environment themes were consistent with previous research on eating identity, and food preferences, practices, and routines shaping food choice (Falk, Sobal, Bisogni, Connors, & Devine, 2001). The personal theory of weight loss theme described in the current study is related to a large and diverse body of qualitative research dedicated to understanding how expected outcomes from eating healthy foods are informed by past individual experiences in addition to experiences' of friends and family and communication with health professionals (Bisogni, Jastran, Seligson, & Thompson, 2012; Falk et al., 2001).
Though individual factors were salient and consistent with previous research, the current study especially emphasizes the salient pressure of the interpersonal environment and the interplay between intrapersonal and interpersonal factors and physical settings on the feasibility of small changes, in spite of the intervention focus on physical cues to unhealthy eating. This study adds to the growing body of research about how the interpersonal environment might interact with the physical environment to, for example, shape exposure to physical environmental influence (e.g. Gorin et al., 2013; Sobal, Bisogni, & Jastran, 2014). For example, the worksite was an important interpersonal eating environment in this study. Worksite aspects such as supervisor support and organization health culture and how they shape the influence of the physical work food environment might be considered when planning similar interventions (Ribisl & Reischl, 1993; Sliter, 2013).
When participants described interpersonal eating environments, issues regarding household dietary preferences and practices and control over food, especially managing commensality, desires to get along and respect others, and food roles and responsibilities were especially salient. These findings echo a number of qualitative studies that highlight the importance of spouses and children in food decisions and dietary change (Brown & Wenrich, 2012; Furst, Connors, Bisogni, Sobal & Falk, 1996; Rydén & Sydner, 2011; Wenrich, Brown, Miller-Day, Kelley, & Lengerich, 2010). These findings are also consistent with research where “lack of control over food preparation” (Gardner & Hausenblas, 2004) or family resistance to introduction of more healthful foods (Brown & Wenrich, 2012; Rydén & Sydner, 2011) acted as a barrier to making desired eating behavior changes.
Important findings were the tactics that participants used to respond to challenges from their interpersonal eating environments. Sometimes this involved making minor adaptations to the small change strategy to make it fit in their daily lives. While adaptations are sometimes discouraged to preserve intervention fidelity, this study provided an opportunity to learn from the adaptations participants used to improve the trial phase of the intervention that followed (Rogers, 2003). In addition, participants used previously documented tactics like trying to negotiate changes to meal content to get buy-in from household members (Furst et al. 1996) or producing two separate meals (Rydén & Sydner, 2011). Participants also used other negotiation tactics that are less often reported. While many participants were challenged by household food preferences and lack of control over things like snack foods, both men and women were able to assert control over household foods and accomplish small changes by taking responsibility for food acquisition or preparation of main meals. This finding runs counter to much research that women's food choices may be more influenced by household preferences than are men's (Brown & Wenrich, 2012; DeVault, 1991). Differences between previous findings and findings in the current study may be due, in part, to diversity in age range, life stage, number and role of people in the home, and expectations for partner involvement and support (Seidel, Franks, Stephens, & Rook, 2012). Additionally, the capacity to assert control over food or negotiate meal content may have been limited by tight food budgets and time constraints for both men and women: some participants expressed reluctance to try out new foods with family members to avoid wasted food and time if the new foods were disliked. Finally, participants used an innovative tactic to navigate more challenging environments and household conflicts over food. This tactic was to sidestep those unsupportive environments and try out their strategy at work or in another non-commensal space. This allowed participants to gain confidence with the strategy before subjecting themselves to others' comments.
These findings suggest potential differences in participants' experiences making small eating changes and environmental in-fluences on those changes, driven in part by interpersonal factors that might be heavily related to broad diversity in life stage and age range of participants (e.g. food responsibilities, including caring for adults versus young children). Future research will be needed in this population to determine if the strategies and tactics described in this study apply more broadly.
Lastly, making small changes was described as a process. Participants selected their strategy and most discussed responding to challenges trying it out with tactics to improve feasibility as discussed above or discontinuing their strategy. These findings suggest that even for small change strategies, there is a hurdle involved in initiating behavior change, where participants have to figure out how to change in context of daily life. Findings suggest that while challenging at first, small changes can be made a part of daily life over a twelve week period. Recognizing that this study relied on retrospective self-report, though participants were interviewed on average within two weeks after concluding the intervention, their responses may not necessarily reflect their earlier experiences during the study. Future research should explore prospectively, for example, during weekly CHW interviews, whether development of tactical skills makes it easier to make small changes as time goes on, what facilitates this and if small changes are easier than large changes to maintain, despite the initial hurdle (Rothman, Sheeran, & Wood, 2009).
Findings from this analysis suggest practical recommendations used to improve feasibility and appropriateness of this intervention for this population. First, it would be useful to help participants identify salient aspects of their intrapersonal and interpersonal eating environments that could be facilitative or pose challenges and then help them select a small change strategy that is compatible with that environment. Small change studies to date have generally used a type of tailoring process that involves matching small change strategies to baseline assessment of eating behaviors (e.g. Damschroder et al., 2014; Lutes et al., 2008; Zinn et al., 2012). However, here it appears that CHWs could assist with matching strategies not just to participants' current eating behavior, but also to complex behavioral settings that encompass the personal food environment referred to by Lowe (2003) as “the sum total of all the food-related situations individuals encounter, create, or seek out in the course of their daily lives” (p. 54S). Matching the small change strategy to behavioral settings through the use of motivational interviewing (Resnicow & McMaster, 2012) or comprehensive food setting assessment may achieve a kind of deep tailoring where the strategy is compatible with salient aspects of each participants' personal eating environment, including, for example, a participant's theory of weight loss, control over food, and work eating culture. Increased compatibility reduces ambiguity and increases appropriateness to a participant's specific situation (Rogers, 2003), hopefully facilitating self-efficacy and small change feasibility. For example, in a weight loss intervention where participants substituted either water or diet-beverages for sugar-sweetened beverages, results indicated that it may have been harder for participants to replace caloric beverages with water than with diet soft drinks, which are arguably more compatible in taste and caffeine content than water (Tate et al., 2012). In the current study, many participants' personal theories of weight loss cast doubt on the efficacy of small changes to produce a desirable amount of weight loss. Selecting a strategy more compatible with participants' theories of weight loss, for example, a strategy more consistent with traditional dieting practices, such as using a smaller plate, might reduce the “small” change ambiguity and facilitate making a small change. It might be useful for this type of assessment and tailoring to go on throughout the intervention as many eating environment aspects are dynamic. Used in an adaptive design approach, information about specific intrapersonal and interpersonal challenges may be applied to tailor obesity interventions to individual or group circumstances (Czajkowski et al., 2015).
Secondly, participants need to develop tactics or skills that will help them carry out the most compatible small change in daily life. Even when participants selected a suitable small change, they needed to employ a variety of tactics and skills to accomplish it in real life. CHWs could help participants develop tactics suitable to them at goal setting and CHW follow up meetings by providing participants with examples of successful tactics from the pilot intervention narratives (e.g. navigate challenging household environment by trying strategy during non-commensal meals to begin with) or through the use of implementation intentions (Gollwitzer & Sheeran, 2006). CHWs could also help participants strengthen general problem solving and tactical skills to promote behavior change sustainability after the intervention.
This research helps to develop a more in-depth understanding of how external factors influence eating behavior change and emphasizes the important role social, cultural, and economic eating environment factors play in eating behavior change intervention feasibility. (Kumanyika, 2008; Taylor et al. 2006). This study also suggests that even though preliminary focus groups helped tailor the intervention strategies to this population, eating contexts vary and thus small change feasibility varies within intrapersonal and interpersonal eating environments. The approach of understanding environmental influences and incorporating them into the intervention process offers the potential to improve feasibility and appropriateness of studies in similar populations.
Some limitations should also be noted. There was a 31% lost to follow up over 12 weeks, comparable to similar weight loss trials (e.g. Teixeira et al., 2004). However, this finding provided an opportunity to improve recruitment and retention techniques in the subsequent randomized trial by changing recruiting language and including more flexible follow up options (Hippolyte, Phillips-Caesar, Winston, Charlson, & Peterson, 2013; Phillips-Caesar et al., 2015). While this analysis only includes participants who could be contacted for a close-out interview, it includes participants with a range of CHW follow-ups and experiences (including those who discontinued the small change). Additionally, Hispanic participants and participants with more household members were less likely to agree to have their interviews recorded, limiting the insight we have into potential unique experiences in this group, comparisons between groups, interpersonal challenges faced, and strategies utilized to navigate household relationships. Lastly, while this analysis explored proximal factors in participants' eating contexts, considerations of broader social, cultural, physical, and political landscapes were not prompted. Through open-ended questions participants had the opportunity to discuss other upstream barriers and facilitators to implementing their small change, but future research should specifically probe for these influences and especially consider how the cultural eating environment (some descriptions of which are included in this analysis) also shapes interactions with the physical food environment.
5. Conclusions
Though other small change and personal environment modification studies have reported quantitative weight and behavior outcomes, to the authors' knowledge, this is one of the first small change studies reporting how participants experience making small changes. These findings suggest that intrapersonal and interpersonal eating environments, and especially the fit of a strategy with salient eating environments, shapes the feasibility of small changes for Black and Hispanic adults. This underlines the importance of feasibility studies to inform the design of community trials. These findings add to understanding of diverse contextual challenges and the skills needed to negotiate them that may affect the success of behavioral interventions in ethnic minority and low-income populations (Kumanyika, 2008; Taylor et al., 2006). In this way, these findings were used to modify and adapt the intervention procedures for the randomized control trial that followed.
Acknowledgments
This research was supported by the National Heart, Lung and Blood Institute of the National Institutes of Health (under award Number U01HL097843, PI: Mary Charlson) and by United States Department of Agriculture Preparing Doctoral Students to Address the Ecology of Obesity Training Grant (CREES NNF-TESHA 2008–03576, PI: Christine Olsen). These funding sources had no involvement in the study design, data collection, data analysis, writing of the report, or the decision to submit the paper for publication.
Footnotes
cmd10@cornell.edu (C.M. Devine), ew20@cornell.edu (E. Wethington), lia5@cornell.edu (L. Aceves), erp2001@med.cornell.edu (E. Phillips-Caesar), wansink@cornell.edu (B. Wansink), mecharl@med.cornell.edu (M.E. Charlson).
References
- Bisogni CA, Jastran M, Seligson M, Thompson A. How people interpret healthy eating: contributions of qualitative research. Journal of Nutrition Education and Behavior. 2012;44(4):282–301. doi: 10.1016/j.jneb.2011.11.009. http://dx.doi.org/10.1016/j.jneb.2011.11.009. [DOI] [PubMed] [Google Scholar]
- Brown JL, Wenrich TR. Intra-family role expectations and reluctance to change identified as key barriers to expanding vegetable consumption patterns during interactive family-based program for Appalachian low-income food preparers. Journal of the Academy of Nutrition and Dietetics. 2012;112(8):1188–1200. doi: 10.1016/j.jand.2012.05.003. http://dx.doi.org/10.1016/j.jand.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Cohen DA, Farley TA. Eating as an automatic behavior. Preventing Chronic Disease. 2008;5(1):1–7. [PMC free article] [PubMed] [Google Scholar]
- Czajkowski SM, Powell LH, Adler N, Naar-King S, Reynolds KD, Hunter CM, et al. for the Obesity Related Behavioral Intervention Trials (ORBIT) Consortium From ideas to efficacy: the ORBIT model for developing behavioral treatments for chronic diseases. Health Psychology. 2015 doi: 10.1037/hea0000161. http://dx.doi.org/10.1037/hea0000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damschroder LJ, Lutes LD, Goodrich DE, Gillon L, Lowery JC. A small-change approach delivered via telephone promotes weight loss in veterans: results from the ASPIRE-VA pilot study. Patient Education and Counseling. 2010;79(2):262–266. doi: 10.1016/j.pec.2009.09.025. http://dx.doi.org/10.1016/j.pec.2009.09.025. [DOI] [PubMed] [Google Scholar]
- Damschroder LJ, Lutes LD, Kirsh S, Kim HM, Gillon L, Holleman RG, et al. Small-changes obesity treatment among veterans: 12-month outcomes. American Journal of Preventive Medicine. 2014;47(5):541–553. doi: 10.1016/j.amepre.2014.06.016. http://dx.doi.org/10.1016/j.amepre.2014.06.016. [DOI] [PubMed] [Google Scholar]
- DeVault ML. Feeding the family: The social organization of caring as gendered work. The University of Chicago Press; Chicago, IL: 1991. [Google Scholar]
- Diaz VA, Mainous AG, III, Pope C. Cultural conflicts in the weight loss experience of overweight Latinos. International Journal of Obesity. 2007;31(2):328–333. doi: 10.1038/sj.ijo.0803387. http://dx.doi.org/10.1038/sj.ijo.0803387. [DOI] [PubMed] [Google Scholar]
- Downs JS, Loewenstein G, Wisdom J. Strategies for promoting healthier food choices. American Economic Review Papers & Proceedings. 2009;99(2):1–10. doi: 10.1257/aer.99.2.159. http://dx.doi.org/10.1257/aer.99.2.159. [DOI] [PubMed] [Google Scholar]
- Falk LW, Sobal J, Bisogni CA, Connors M, Devine CM. Managing healthy eating: definitions, classifications, and strategies. Health Education & Behavior. 2001;28(4):425–439. doi: 10.1177/109019810102800405. http://dx.doi.org/10.1177/109019810102800405. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. Journal of the American Medical Association. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. http://dx.doi.org/10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Furst T, Connors M, Bisogni C, Sobal J, Falk L. Food choice: a conceptual model of the process. Appetite. 1996;26(3):247–265. doi: 10.1006/appe.1996.0019. http://dx.doi.org/10.1006/appe.1996.0019. [DOI] [PubMed] [Google Scholar]
- Gardner RE, Hausenblas HA. Exercise and diet beliefs of overweight women participating in an exercise and diet program: an elicitation study using the theory of planned behavior. Journal of Applied Biobehavioral Research. 2004;9(3):188–200. http://dx.doi.org/10.1111/j.1751-9861.2004.tb00100.x. [Google Scholar]
- Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Advances in Experimental Social Psychology. 2006;38:69–119. http://dx.doi.org/10.1016/S0065-2601(06)38002-1. [Google Scholar]
- Gorin AA, Raynor HA, Fava J, Maguire K, Robichaud E, Trautvetter J, et al. Randomized controlled trial of a comprehensive home environmentfocused weight-loss program for adults. Health Psychology. 2013;32(2):128–137. doi: 10.1037/a0026959. http://dx.doi.org/10.1037/a0026959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. Journal of the Academy of Nutrition and Dietetics. 2013;113(1):43–45. doi: 10.1016/j.jand.2012.09.016. http://dx.doi.org/10.1016/j.jand.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill JO. Can a small changes approach help address the obesity epidemic? A report of the joint taskforce of the America society for nutrition (ASN), Institute of food technologists (IFT), and the international food information Council (IFIC) American Journal of Clinical Nutrition. 2009;89(2):477–484. doi: 10.3945/ajcn.2008.26566. http://dx.doi.org/10.3945/ajcn.2008.26566. [DOI] [PubMed] [Google Scholar]
- Hippolyte JM, Phillips-Caesar EG, Winston G, Charlson ME, Peterson JC. Recruitment and retention techniques for developing faith-based research partnerships, New York City, 2009–2012. Preventing Chronic Disease. 2013;10:E30. doi: 10.5888/pcd10.120142. http://dx.doi.org/10.5888/pcd10.120142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumanyika S. Ethnic minorities and weight control research priorities: where are we now and where do we need to be? Preventive Medicine. 2008;47(6):583–586. doi: 10.1016/j.ypmed.2008.09.012. http://dx.doi.org/10.1016/j.ypmed.2008.09.012. [DOI] [PubMed] [Google Scholar]
- Kumanyika S, Obarzanek E, Stevens V, Hebert P, Whelton P. Weight-loss experience of black and white participants in NHLBI-sponsored clinical trials. American Journal of Clinical Nutrition. 1991;53(6S):1631S–1638S. doi: 10.1093/ajcn/53.6.1631S. [DOI] [PubMed] [Google Scholar]
- Lowe MR. Self-regulation of energy intake in the prevention and treatment of obesity: is it feasible? Obesity Research. 2003;11(S):44S–59S. doi: 10.1038/oby.2003.223. http://dx.doi.org/10.1038/oby.2003.223. [DOI] [PubMed] [Google Scholar]
- Lutes LD, Daiss SR, Barger SD, Read M, Steinbaugh E, Winett RA. Small changes approach promotes initial and continued weight loss with a phone-based follow-up: nine-month outcomes from ASPIRES II. American Journal of Health Promotion. 2012;26(4):235–238. doi: 10.4278/ajhp.090706-QUAN-216. doi: http://dx.doi.org/10.4278/ajhp.090706-QUAN-216. [DOI] [PubMed] [Google Scholar]
- Lutes LD, Winett RA, Barger SD, Wojcik JR, Herbert WG, Nickols–Richardson SM, et al. Small changes in nutrition and physical activity promote weight loss and maintenance: 3-month evidence from the ASPIRE randomized trial. Annals of Behavioral Medicine. 2008;35(3):351–357. doi: 10.1007/s12160-008-9033-z. http://dx.doi.org/10.1007/s12160-008-9033-z. [DOI] [PubMed] [Google Scholar]
- Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. American Journal of Clinical Nutrition. 2006;84(2):274–288. doi: 10.1093/ajcn/84.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute. North American Association for the Study of Obesity . The practical guide: Identification, evaluation, and treatment of overweight and obesity in adults. National Institutes of Health; Bethesda, MD: 2000. (NIH Publication No. 00–4084) [Google Scholar]
- Painter JE, Wansink B, Hieggelke JB. How visibility and convenience influence candy consumption. Appetite. 2002;38(3):237–238. doi: 10.1006/appe.2002.0485. http://dx.doi.org/10.1006/appe.2002.0485. [DOI] [PubMed] [Google Scholar]
- Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA, Viegener BJ. Relapse prevention training and problem-solving therapy in the long-term management of obesity. Journal of Consulting and Clinical Psychology. 2001;69(4):722–726. http://dx.doi.org/10.1037/0022-006X.69.4.722. [PubMed] [Google Scholar]
- Phillips-Caesar EG, Winston G, Peterson JC, Wansink B, Devine CM, Kanna B, et al. Small changes and lasting effects (SCALE) Trial: the formation of a weight loss behavioral intervention using EVOLVE. Contemporary Clinical Trials. 2015;41(1):118–128. doi: 10.1016/j.cct.2015.01.003. http://dx.doi.org/10.1016/j.cct.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, McMaster F. Motivational Interviewing: moving from why to how with autonomy support. International Journal of Behavioral Nutrition and Physical Activity. 2012;9:19. doi: 10.1186/1479-5868-9-19. http://dx.doi.org/10.1186/1479-5868-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribisl KM, Reischl TM. Measuring the climate for health at organizations: development of the worksite health climate scales. Journal of Occupational Medicine. 1993;35(8):812–824. doi: 10.1097/00043764-199308000-00019. [DOI] [PubMed] [Google Scholar]
- van't Riet J, Sijtsema ST, Dagevos H, De Bruijn GJ. The importance of habits in eating behavior. An overview and recommendations for future research. Appetite. 2011;57(3):585–596. doi: 10.1016/j.appet.2011.07.010. http://dx.doi.org/10.1016/j.appet.2011.07.010. [DOI] [PubMed] [Google Scholar]
- Roberts M, Kerker B, Mostashari F, Van Wye G, Thorpe L. Obesity and health: risks and behaviors. NYC Vital Signs. 2005;4(2):1–4. [Google Scholar]
- Rogers EM. Diffusion of innovations. 5th ed Free Press; New York, NY: 2003. pp. 179–188.pp. 240–257. [Google Scholar]
- Rothman AJ, Sheeran P, Wood W. Reflective and automatic processes in the initiation and maintenance of dietary change. Annals of Behavioral Medicine. 2009;38(S1):S4–S17. doi: 10.1007/s12160-009-9118-3. http://dx.doi.org/10.1007/s12160-009-9118-3. [DOI] [PubMed] [Google Scholar]
- Rydén PJ, Sydner YM. Implementing and sustaining dietary change in the context of social relationships. Scandinavian Journal of Caring Sciences. 2011;25(3):583–590. doi: 10.1111/j.1471-6712.2010.00867.x. http://dx.doi.org/10.1111/j.1471-6712.2010.00867.x. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Owen N. Ecological models. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. 2nd ed Jossey-Bass; San Francisco, CA: 1997. pp. 403–424. [Google Scholar]
- Seidel A, Franks MM, Stephens MAP, Rook KS. Spouse control and type 2 diabetes management: moderating effects of dyadic expectations for spouse involvement. Family Relations. 2012;6(4):698–709. doi: 10.1111/j.1741-3729.2012.00719.x. http://dx.doi.org/10.1111/j.1741-3729.2012.00719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliter KA. Development and validation of a measure of workplace climate for healthy weight maintenance. Journal of Occupational Health Psychology. 2013;18(3):350–362. doi: 10.1037/a0033132. http://dx.doi.org/10.1037/a0033132. [DOI] [PubMed] [Google Scholar]
- Sobal J, Bisogni CA, Jastran M. Food choice is multifaceted, contextual, dynamic, multilevel, integrated, and diverse. Mind, Brain, and Education. 2014;8(1):6–12. http://dx.doi.org/10.1111/mbe.12044. [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2nd ed Sage; Thousand Oaks, CA: 1998. [Google Scholar]
- Swinburn B, Egger G. The runaway weight gain train: too many accelerators, not enough brakes. British Medical Journal. 2004;329(7468):736–739. doi: 10.1136/bmj.329.7468.736. http://dx.doi.org/10.1136/bmj.329.7468.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate DF, Turner-McGrievy G, Lyons E, Stevens J, Erickson K, Polzien K, et al. Replacing caloric beverages with water or diet beverages for weight loss in adults: main results of the choose healthy options consciously everyday (CHOICE) randomized clinical trial. American Journal of Clinical Nutrition. 2012;95(3):555–563. doi: 10.3945/ajcn.111.026278. http://dx.doi.org/10.3945/ajcn.111.026278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor WC, Poston WSC, Jones L, Kraft MK. Environmental justice: obesity, physical activity, and healthy eating. Journal of Physical Activity and Health. 2006;3(1):S30–S54. doi: 10.1123/jpah.3.s1.s30. [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Metcalfe LL, Blew RM, et al. Pretreatment predictors of attrition and successful weight management in women. International Journal of Obesity and Related Metabolic Disorders. 2004;28(9):1124–1133. doi: 10.1038/sj.ijo.0802727. http://dx.doi.org/10.1038/sj.ijo.0802727. [DOI] [PubMed] [Google Scholar]
- Wansink B. Environmental factors that increase the food intake and consumption volume of unknowing consumers. Annual Review of Nutrition. 2004;24:455–479. doi: 10.1146/annurev.nutr.24.012003.132140. http://dx.doi.org/10.1146/annurev.nutr.24.012003.132140. [DOI] [PubMed] [Google Scholar]
- Wansink B. From mindless eating to mindlessly eating better. Physiology & Behavior. 2010;100(5):454–463. doi: 10.1016/j.physbeh.2010.05.003. http://dx.doi.org/10.1016/j.physbeh.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Wansink B, Just DR, Payne CR. Mindless eating and healthy heuristics for the irrational. American Economic Review: Papers & Proceedings. 2009;99(2):165–169. doi: 10.1257/aer.99.2.165. [DOI] [PubMed] [Google Scholar]
- Wenrich TR, Brown JL, Miller-Day M, Kelley KJ, Lengerich EJ. Family members' influence on family meal vegetable choices. Journal of Nutrition Education and Behavior. 2010;42(4):225–234. doi: 10.1016/j.jneb.2009.05.006. http://dx.doi.org/10.1016/j.jneb.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West DS, Prewitt TE, Bursac Z, Felix HC. Weight loss of black, white, and Hispanic men and women in diabetes prevention program. Obesity. 2008;16(6):1413–1420. doi: 10.1038/oby.2008.224. http://dx.doi.org/10.1038/oby.2008.224. [DOI] [PubMed] [Google Scholar]
- Zinn C, Schofield GM, Hopkins WG. A “small-changes” workplace weight loss and maintenance program: examination of weight and health outcomes. Journal of Occupation and Environmental Medicine. 2012;54(10):1230–1238. doi: 10.1097/JOM.0b013e3182480591. http://dx.doi.org/10.1097/JOM.0b013e3182480591. [DOI] [PubMed] [Google Scholar]