Abstract
Cognitive diathesis stress models of depression emphasize individual styles of attributing causal explanations to negative and positive events in life. The Attributional Style Questionnaire (ASQ) has traditionally been used to measure explanatory style, defined as an individual’s habitual way of assigning causes to negative events. Explanatory flexibility, rather than focusing on the content of one’s thoughts, emphasizes the extent to which individuals are able to make different attributions depending on the particular context of each event. The underlying notion is that individuals who are better able to adapt to the cues and demands of a stressful situation may be able to respond more effectively and are thereby less vulnerable to depression. Despite evidence attesting to its relevance to depression and anxiety disorders, explanatory flexibility has yet to be examined in a purely treatment-seeking sample of patients clinically diagnosed with Axis I psychopathology. The current study examined baseline levels of explanatory flexibility, along with explanatory style, in a sample of 171 treatment-seeking patients diagnosed with either major depressive disorder (MDD), generalized anxiety disorder (GAD), or at least one other Axis I disorder. Overall, the results replicate and extend past results indicating a distinction between explanatory flexibility and explanatory style. Furthermore, patients with MDD and GAD demonstrated lower levels of explanatory flexibility relative to patients with other Axis I disorders. Thus, explanatory flexibility may assist in our understanding of the etiology, maintenance, and treatment of emotional disorders, with particular relevance to MDD and GAD.
Keywords: explanatory flexibility, explanatory style, Attributional Style Questionnaire
The reformulated learned helplessness (Abramson, Seligman, & Teasdale, 1978) as well as hopelessness theories (Abramson, Metalsky, & Alloy, 1989), both derived from the original learned helplessness theory (Seligman, 1974), are cognitive diathesis-stress models of depression that have been particularly influential in understanding the etiology, maintenance, and treatment of depression. Both models emphasize individual styles of attributing causal explanations to negative and positive events in life. Specifically, these theories maintain that vulnerability to depression arises with the development of a pessimistic explanatory style, defined as the tendency to attribute the arising of negative events to stable, global, and internal causes. Hopelessness theory (Abramson et al., 1989) emphasizes the former two dimensions and refers to this vulnerability factor as “generality,” while subsequently placing less emphasis on the dimension of internality. Taken together, learned helplessness theory (Seligman, 1974) along with its derivative theories, propose that an individual’s propensity to become depressed is associated with how the individual interprets information or attributes causes to personal life experiences.
Pessimistic explanatory style (i.e., habitually viewing negative events as arising from stable, global, and internal causes) has traditionally been assessed using the Attributional Style Questionnaire (ASQ; Peterson et al., 1982), a self-report inventory in which respondents are presented with six hypothetical positive and six hypothetical negative situations and asked to rate the cause of the event along stable, global, and internal dimensions. In accordance with hopelessness theory (Abramson et al., 1989), explanatory style can be operationalized as a “generality” score, which is computed by averaging the values of the twelve stability and globality items across negative events to produce a score ranging from one to seven; higher scores on this measure indicate a more pessimistic style of responding. Previous research has demonstrated a link between explanatory style and various aspects of emotional disorders; for example, explanatory style has been shown to correlate with symptoms of both unipolar and bipolar depression (Seligman et al., 1988) and has also been implicated in the etiology, maintenance, and treatment of other emotional disorders (Abramson et al., 1999; Alloy et al., 2000; Alloy et al., 1999; DeRubeis et al., 1990; Hollon et al., 1992).
Despite the potential clinical utility offered by explanatory style, targeting cognitive content as a specific mechanism of change may be a less fruitful approach than focusing instead on how information is processed. According to Hollon and colleagues, there are two distinguishable kinds of cognitions: cognitive structures and cognitive products (Hollon & Garber, 1988; Hollon & Kriss, 1984; Ingram & Hollon, 1986; Kendall & Ingram, 1989). Cognitive structures refer to the way in which information is processed, or represented in memory (Ingram & Hollon, 1986). Examples of cognitive structures include the components of Beck’s (1976; 1967) negative cognitive triad, or a negative schema about the self, world and future; these represent a framework, or structure through which an individual comes to organize and understand personal experiences. Cognitive products represent the end result of information processing and include, for example, negative statements about the self, directly accessible, conscious thoughts, and causal attributions. Importantly, researchers have cautioned against targeting the latter kind of cognition as a specific mechanism of change (Hollon & Kriss, 1984; Safran, Vallis, Segal, & Shaw, 1986), maintaining that targeting cognitive products is tantamount to targeting symptoms, an approach that is less likely to provide maximum clinical utility. In other words, focusing on how the individual processes information rather than the content of cognition itself may facilitate more central, “deep” change (Safran et al., 1986). Thus, researchers have recommended that treatment approaches should focus on core processes as critical change mechanisms in cognitive therapy for depression (Beck, Rush, Shaw, & Emery, 1979; Safran et al., 1986). More recent evidence has shown that patients who simply become more optimistic by changing the contents of their thoughts evidence less durable treatment gains than patients who became more realistic in their thinking (DeRubeis et al., 2005).
One construct that emphasizes how information is being processed is explanatory flexibility, which refers to how flexible or rigid individuals are at assigning causes to events (Fresco, Heimberg, Abramowitz, & Bertram, 2006a; Fresco, Rytwinski, & Craighead, 2007; Fresco, Williams, & Nugent, 2006b; Moore & Fresco, 2007). Explanatory flexibility represents the degree to which individuals are able to make effective use of both historical and contextual factors when appraising the stressful situations that arise in their lives. As with explanatory style, the underlying vulnerability of the reformulated helplessness (Abramson et al., 1978) and hopelessness theories (Abramson et al., 1989), explanatory flexibility is also assessed using the ASQ; however, whereas explanatory style is an assessment of the cognitive content of the individual, as reflected by the average of values across the stability and globality items for negative events (i.e., generality score), explanatory flexibility is operationalized as the standard deviation of an individual’s responses to negative life events along the stable and global dimensions on the ASQ (Fresco et al., 2007). A small standard deviation is conceptualized as the tendency to respond to negative situations in a more rigid fashion, whereas a large standard deviation indicates that the individual is able to view situations contextually and separately, and is therefore considered to be flexible in his or her casual attributions.
The role of rigidity in the pathogenesis of a variety of biomedical and psychological conditions has been a robust finding. For example, autonomic rigidity is associated with heart disease, hypertension, and various mood disorders (Thayer & Lane, 2002), while affective flexibility is associated with enhanced adaptation to stress and negative life events (e.g., Rosenbaum & Ben-Ari, 1985) and resilience to physical injury and illness (e.g., Miller, Shoda, & Hurley, 1996). In particular, relatively recent research characterizes generalized anxiety disorder (GAD) as an inability to respond flexibly to environmental challenges (Thayer, Friedman, & Borkovec, 1996; Thayer, Friedman, Borkovec, Johnson, & Molina, 2000). Thayer and colleagues (1996; 2000) note that a global model of anxiety should encompass the role of attention in GAD. The same mode of rigid responding is also thought to increase risk of recurrence and relapse to depression (Teasdale, 1999). Explanatory flexibility may reflect one such capacity or tendency to be flexible in one’s cognitive processing. Thus, the present study adds to the ongoing investigation of individual variations of responsiveness in the face of negative events under the premise that individuals who are able to adapt contextually and flexibly to stressful situations are less vulnerable to depression and anxiety.
Considerable evidence offers validation for explanatory flexibility as a meaningful construct that adds to the current understanding of depression (Fresco et al., 2006a; Fresco et al., 2006a; Fresco et al., 2007) and generalized anxiety disorders (Fresco, Mennin, Moore, Heimberg, & Hambrick, 2014) that is statistically distinct from explanatory style (Moore & Fresco, 2007). For example, in a sample of 78 college students randomly selected from mass testing, explanatory flexibility was found to be modestly correlated with explanatory style (r = −.27; Fresco et al., 2007). Moreover, explanatory flexibility, but not explanatory style, moderated the relationship between negative life events to levels of self-reported depression measured eight weeks later. Furthermore, Fresco and colleagues (2006b) found that explanatory flexibility and coping flexibility independently contributed to the prediction of latent negative affect, assessed via the Beck Anxiety Inventory (BDI; Beck, Epstein, Brown,& Steer, 1988) and cognitive and somatic indicators of the Beck Depression Inventory – II (BDI: Beck, Steer, & Brown, 1996). This study also found that lower explanatory flexibility scores were not simply proxies from extreme responding in terms of explanatory style. Finally, two studies have shown that emotion provocation in the form of a negative mood priming challenge was associated with reductions in explanatory flexibility among individuals with either remitted major depression (Fresco et al., 2006a) or GAD (Fresco et al., 2014) as assessed by the Generalized Anxiety Disorder Questionnaire for DSM-IV (Newman et al., 2002), but not among healthy control participants. No other studies, to the authors’ knowledge, have examined explanatory flexibility within the context of GAD.
Although previous studies have established the distinctiveness of explanatory flexibility from explanatory style and have demonstrated the useful contribution of explanatory style in understanding depression and anxiety, previous studies are limited in that the samples have been restricted to self-reported depressive and anxious psychopathology. Thus, the current study sought to extend and strengthen this work by examining explanatory flexibility in treatment-seeking patients who met diagnostic criteria as outlined in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000) for a variety of disorders. Specifically, the current study examined levels of explanatory flexibility and explanatory style (generality) in a sample of patients seeking outpatient psychotherapy for one or more clinician-assessed DSM-IV-TR Axis I diagnoses. Given the relevance of depression and anxiety to the study of explanatory style and explanatory flexibility, patients were classified into one of three groups based upon current diagnoses: MDD, GAD, or psychiatric controls (No MDD or GAD). The hypotheses of the current study were:
MDD and GAD groups together would demonstrate lower levels of explanatory flexibility compared to the psychiatric control group.
As a clinical extension of Moore and Fresco (2007), explanatory style (i.e. generality) and explanatory flexibility would illustrate a low degree of correlation.
Method
Participants and Procedures
Data were obtained from a sample (N=171) comprised primarily of college students (n = 140) with some community members (n = 31) seeking treatment within a university clinic at a large mid-western university. Of these participants, 120 were female (70.18%) and the mean age was 22.66 years (SD = 5.01). The sample consisted of 141 Caucasian participants (82.46%), 20 African-American participants (11.70%), 2 Asian participants (1.17%), 2 Hispanic participants (1.17%), 6 participants who marked “other” (3.50%), and one participant who failed to mark the item on race (0.58%). Participants completed the ASQ (Peterson et al., 1982) during intake, in addition to other baseline measures which are not included in the present analysis. All participants provided informed consent.
Clients were evaluated by clinic therapists with the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID-IV; First, Spitzer, Gibbon, & Williams, 2002) prior to treatment. The SCID-IV was administered by one of six clinical psychology graduate students who were kept blind to participants’ responses on the ASQ. Interviewers received extensive training in conducting the interview, including practicum training on administration techniques and 1 year of supervision rounds to establish accuracy of diagnoses. All diagnoses were confirmed by clinical supervisors, and diagnoses were given on a dichotomous, yes/no basis. Interrater reliability was established for the sample by having three interviewers rate each of 10 randomly selected SCID-IV interviews. The original interviewer recorded and rated the SCID-IV, while two other study interviewers, blind to the original ratings, independently rated the SCID-IV. Kappa (κ) was calculated by comparing each of the two additional ratings to the original rating, yielding two κ values for each interview. For this sample, interrater reliability across interviewers for the SCID-IV ranged from 0.79 to 0.87 (average κ = 0.83) for all diagnoses. Any discrepancies were addressed in case conference to establish consensus.
From the data obtained through SCID-IV interviews, individuals were subsequently placed into three groups based on their diagnoses. The three groups were composed of clients with MDD, with no current or lifetime history of GAD (n = 49), GAD, irrespective of current or lifetime history of MDD (n = 63), and other Axis I disorders, with no current or lifetime history of MDD or GAD (psychiatric control group; n = 59). Specifically, the psychiatric control group was comprised of individuals diagnosed with eating disorder NOS (n = 2), panic disorder without agoraphobia (n = 7), anxiety disorder NOS (n = 17), post-traumatic stress disorder (n = 8), alcohol dependence (n = 1), anorexia nervosa (n = 1), alcohol abuse (n = 2), obsessive-compulsive disorder (n = 2), bulimia nervosa (n = 2), social phobia (n = 4), and adjustment disorder (n = 13). Within the patient subgroups, rates of comorbidity were 65% (MDD), 77% (GAD), and 44% (psychiatric controls). For all individuals in either the MDD or GAD groups, MDD or GAD was identified as the primary diagnosis, allowing for other secondary and tertiary diagnoses.
The decision to allow MDD comorbidity in the GAD patient subgroup was made in accordance with previous research (Etkin & Schatzberg, 2011), suggesting that depression-only individuals may represent an endophenotype dissociable from individuals with comorbid depression and anxiety. Specifically, Etkin and Schatzberg (2011) observed an increase in ventral cingulate activity and a dampening of amygdala activity during emotion regulation in both comorbid and depression-only groups; however, the depression-only group was able to compensate for this deficit by activating the anterior lateral prefrontal cortex, allowing for the regulation of emotional conflict. In addition to neural dissociability, other research has suggested that GAD is expected to create impairments over and above impairments due to MDD (Nisita et al., 1990; Roy-Byrne, 1996). Thus, the current study grouped GAD and MDD comorbid individuals into the GAD subgroup.1
Measures
The Attributional Style Questionnaire is a self-report inventory that assesses causal attributions for six hypothetical positive and six hypothetical negative events along the dimensions of stability and globality that are each rated on a scale from 1 to 7. Higher ratings represent more pessimistic responses and more stable and global causes, while lower ratings represent more unstable and specific causes. A generality score is computed by averaging the values of the 12 stability and globality items across negative events to produce a score that ranges from 1 to 7. In addition, explanatory flexibility can be computed by determining the standard deviation of these same 12 stable and global items for negative events. The ASQ has been shown to have adequate internal consistency (α = .70 to .75; Peterson et al., 1982; Sweeney, Anderson, & Bailey, 1986) in both psychiatric and undergraduate populations. Test-retest reliability for the negative event dimensions has ranged from r = 0.52 to 0.60 (Colin, Sweeney, & Schaeffer, 1981; Peterson et al., 1982; Sweeney et al., 1986). In the current study, the ASQ demonstrated adequate internal consistency (α = .77).
The Structured Clinical Interview for DSM-IV-TR, Research Version (SCID-IV; First et al., 2002) is a widely used semi-structured interview that allows for current and lifetime diagnoses of Axis I disorders. The SCID-IV has demonstrated high inter-rater agreement (kappas) for current diagnosis with an overall weighted kappa of .82 and a range between .71 and .90 for specific diagnoses (Ventura, Liberman, Green, Shaner, & Mintz, 1998).
Results
Explanatory flexibility and explanatory style between diagnostic groups
Groups did not significantly differ in age F = (3,171) = .089, p = .966. No significant differences were found between males (M = 1.36, SD = .45) and females (M = 1.38, SD = .44) on explanatory flexibility, t(170) = −.259, p = .796, nor were there differences between males (M = 4.56, SD = .97) and females (M = 4.45, SD = .90) on explanatory style, t(170) = .737, p = .268.
Patients diagnosed with MDD, GAD, as well as patients with all other DSM-IV-TR diagnoses were compared with regard to pre-treatment levels of generality and explanatory flexibility (see Table 1 for descriptive statistics). Omnibus tests were significant for both generality, F(2, 168) = 6.97, p < .001, Cohen’s f = .33, and explanatory flexibility, F(2, 168) = 3.59, p = .03, f = .21. Follow-up planned contrasts, comparing participants with either MDD, GAD, or both, to participants diagnosed with another disorder, found significant differences for both generality, t(168) = 3.64, p < .001, d = .56, and flexibility, t(168) = 2.68, p = .008, d = .41, with both results approaching or exceeding Cohen’s convention for a medium effect size (Cohen, 1992).2 Post hoc, exploratory analyses revealed that individuals with an adjustment disorder diagnosis (n = 13), included in the psychiatric control group, displayed relatively low levels of explanatory flexibility (M = 1.35, SD = .39) in the absence of a corresponding pessimistic style (M = 3.74, SD = 1.12).
Table 1.
Pre-treatment generality and explanatory flexibility as a function of diagnostic group.
| Diagnosis | N |
Generality M (SD) |
Explanatory Flexibility M (SD) |
|---|---|---|---|
| MDD | 49 | 4.49 (.77) | 1.31 (.50) |
| GAD | 63 | 4.80 (.78) | 1.31 (.42) |
| Controls | 59 | 4.13 (1.06) | 1.50 (.40) |
Note: MDD = major depressive disorder; GAD = generalized anxiety disorder; Controls = treatment seeking patients with at least one DSM-IV-TR diagnosis other than MDD or GAD.
Comorbidity analyses
Rates of comorbidity were calculated for the sample as a whole and for each patient subgroup. Overall, 60% of the sample received two or more diagnoses. On average, comorbid individuals met criteria for one additional diagnosis (M = 1.11, SD = 1.05). Number of diagnoses was similar for patients in the MDD group (M = 1.00, SD = 1.03), GAD group (M = 1.42, SD = 1.10), and psychiatric control group (M = .78, SD = .90). A oneway ANOVA determined that there was a significant difference in number of diagnoses between groups F(2, 168) = 5.70, p = .004. However, after controlling for instances of MDD-GAD comorbidity within the GAD group (n = 26), a subsequent oneway ANOVA revealed no significant differences in number of diagnoses between groups F(2,168) = .929, p = .40. Therefore, the patient subgroups were considered to be relatively similar with respect to diagnostic comorbidity. Nonetheless, a simple linear regression was calculated to evaluate symptom severity and comorbidity in relation to explanatory flexibility and style in each of the three groups. Results indicated that the addition of comorbidity as a predictor did not improve model fit in predicting explanatory flexibility R2 = .049, F(1, 127) = 1.075, p = .302. However, the addition of comorbidity added significant variance accounted for in the criterion for explanatory style R2 = .106, F(1, 127) = 8.022, p < .01.
Relationship between explanatory flexibility and explanatory style
To replicate and extend the results of Moore and Fresco (2007), the correlations of generality and explanatory flexibility were compared between the three diagnostic groups used above (see Figure 1). Averaged across all participants, the two variables were almost completely uncorrelated, r (171) = −.05, p = .45. Similar results were obtained in participants diagnosed with either GAD or MDD, or both (see Figure 2), r (112) = −.15, p = .13, and participants diagnosed with another DSM-IV-TR disorder, r (59) = .09, p = .50. The above results are similar to findings obtained in two undergraduate, non-clinical samples (r’s = .02 and −.18; Moore & Fresco, 2007).
Figure 1. Correlation between Explanatory Style and Explanatory Flexibility across All Patients.
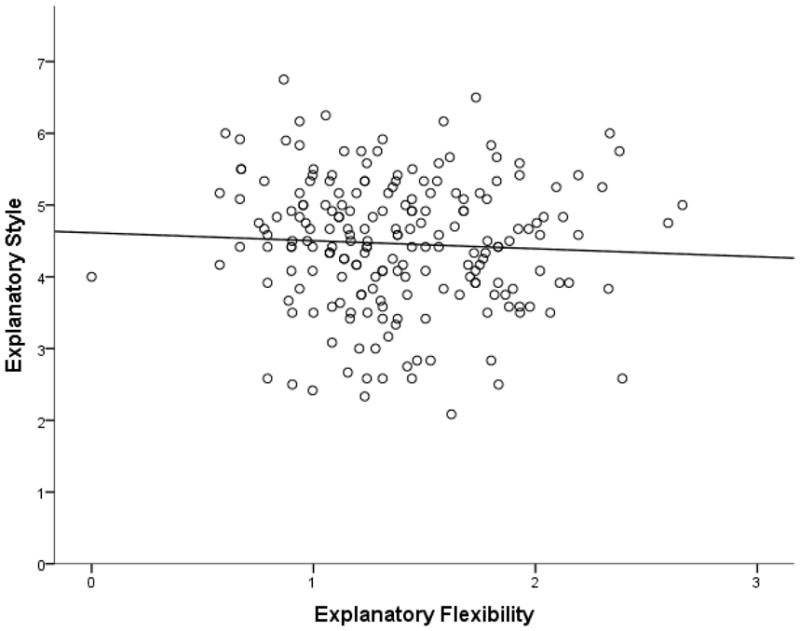
Pearson’s r = −.05.
Figure 2. Correlation between Explanatory Style and Explanatory Flexibility in MDD/GAD Patients.

Pearson’s r = −.15.
Discussion
The purpose of the current study was to examine baseline levels of explanatory flexibility and explanatory style, as measured by the ASQ, in a sample of treatment-seeking patients who met criteria for clinician assessed DSM-IV-TR disorders. A major limitation in previous work involving explanatory flexibility has been the use of samples with exclusively self-reported depressive and anxious psychopathology. It was hypothesized that MDD and GAD groups would demonstrate lower levels of explanatory flexibility compared to a psychiatric control group (Axis I diagnoses other than MDD and GAD). Additionally, it was hypothesized that explanatory flexibility and explanatory style would emerge as statistically distinct constructs, illustrated by a low degree of correlation. Findings from the current study largely support the hypotheses. First, participants with MDD and GAD were both relatively pessimistic and rigid in their attributions of causal events, as compared to patients presenting with other Axis I diagnoses. In regards to the second hypothesis, there was no significant correlation between explanatory flexibility and explanatory style, indicating that although the two constructs may be somewhat related, they remain statistically distinguishable from one another.
The findings of the current study replicate and extend previous work (Fresco et al., 2007; Moore & Fresco, 2007) demonstrating that explanatory flexibility and explanatory style are statistically distinguishable constructs measured by the ASQ. One important limitation of previous studies investigating explanatory flexibility thus far has been the use of strictly non-clinical samples. The current study illustrated that the relationship between explanatory flexibility and explanatory style (i.e., their psychometric nonequivalence) extends into clinical, treatment seeking populations.
As previously noted, the novelty of the current study was that it sought to examine explanatory flexibility in a treatment-seeking sample of patients with clinician assessed current DSM-IV-TR disorders. The findings indicated that patients presenting with MDD and GAD were both relatively pessimistic and rigid in their attributions of causal events, as compared to patients diagnosed with other Axis I disorders. These findings are consistent with previous theory in explanatory flexibility which posits that individuals with MDD (Fresco et al., 2006a; Fresco et al., 2006b; Fresco et al., 2007) and GAD (Fresco et al., 2014; Thayer et al., 2000; Thayer et al., 1996) respond rigidly to negative life events, as opposed to viewing situations contextually and separately, and therefore, enabling more flexibility in causal attributions.
Interestingly, one intriguing finding that emerged in exploratory, post hoc analyses was that individuals with an adjustment disorder diagnosis (n = 13), who were included in the psychiatric control group, were found to display relatively low levels of explanatory flexibility (M = 1.35, SD = .39) in the absence of a corresponding pessimistic style (M = 3.74, SD = 1.12).3 It is possible that these individuals were overwhelmed by an acute psychosocial stressor such that it became more difficult for them to incorporate content specific information, thus causing their attributions to be less varied and more rigid. Moreover, given that adjustment disorder is typically characterized as a disordered response to an external, psychosocial stressor, it may be that these individuals, although overwhelmed by an acute stressor, remain optimistic enough about other areas of life unrelated to the stressor, which may serve to counteract feelings of pessimism about their selves and the world. This finding might also be explained by the fact that many individuals with adjustment disorder display symptoms that are similar to that of depressive or anxiety disorders. However, more research is needed to fully address this question.
The current study, along with previous studies (Fresco et al., 2014; Fresco et al., 2007; Fresco et al., 2006a; Fresco et al., 2006b), strengthens the evidence that explanatory flexibility contributes to the understanding of the etiology, maintenance, and treatment of depression and anxiety. Explanatory flexibility has been shown to both predict long-term outcome of depressed mood (Fresco et al., 2007; Fresco, et al., 2006b) and serve as a mediator of improvement in CBT (DeRubeis et al., 1990; Hollon et al., 1992). Future research may want to focus on whether new or existing treatment approaches would benefit from including the flexibility with which one approaches negative life events as a target for treatment. Such an approach would ideally target an individual’s cognitive processing instead of cognitive content, which may allow for more durable treatment gains (Hollon et al., 2005; Hollon & Kriss, 1984; Safran et al., 1986). Treatments that invite individuals to engage in more non-judgmental and contextually-based strategies (e.g., Mindfulness-Based Cognitive Therapy; Segal, Williams, & Teasdale, 2002; Emotion Regulation Therapy (ERT; Mennin & Fresco, 2009) may be particularly suited for the integration of such metacognitive processing treatment targets. Given the present study’s contribution of demonstrating that individuals with clinically diagnosable MDD and GAD are relatively inflexible in their cognitive processing, explanatory flexibility stands as one clinically useful tool for capturing the flexibility, or rigidity of an individual’s cognitive processing.
Findings of the current study should be viewed in conjunction with its limitations. First, the sample was restricted primarily to college-aged, Caucasian, females; thus, the findings may not generalize to other populations. Second, the current study was unable to provide information regarding changes in explanatory flexibility in response to treatment. Future research will want to utilize longitudinal designs to monitor explanatory flexibility over time in response to various treatments. Third, SCID-IV inter-rater reliability was established using only 10 randomly selected cases; however, all diagnoses were made in consultation with licensed clinical psychologists, and discrepancies in diagnoses were discussed in length. Another limitation is that only SCID-IV and ASQ data were collected. Future studies may want to collect data on various mood indicators (e.g., rumination, worrying, trait anxiety, etc.) to analyze explanatory flexibility along such dimensions. Finally, responses on the ASQ are merely hypothetical responses and do not represent actual attributions made in response to real-life, negative events. A future line of research may want to examine explanatory flexibility in the context of patients responding to actual events in their lives.
In summary, findings from the current study contribute to the growing body of literature on explanatory flexibility and how it may assist in our understanding of the etiology, maintenance, and treatment of emotional disorders. The present study has established explanatory flexibility as a distinguishable construct among treatment-seeking patients presenting with a number of clinical diagnoses, with particular relevance to MDD and GAD. In future research, it will be important to corroborate existing self-report-based findings of explanatory flexibility by exploring the utility of behavioral or more objective measures. Such measures would strengthen the overall clinical utility of explanatory flexibility.
Footnotes
Analyses were also conducted using non-comorbid MDD and GAD groups (i.e., MDD without GAD and GAD without MDD). Overall findings remain consistent; MDD and GAD groups together demonstrated lower levels of explanatory flexibility, F(2, 127) = 4.61, p =.012, and were more pessimistic, F(2,127) = 4.66, p = .011, compared to psychiatric controls.
In order to further explore the effect, we conducted the same analyses using the following 4 groups: pure MDD (n = 18), pure GAD (n=16), comorbid GAD/MDD (n=26), and controls (n=46), with contrast weights of −1, −1, −2, and 4, respectively. Results support the contention that individuals with uncomplicated GAD or MDD as well as comorbid GAD and MDD evidence lower explanatory flexibility as compared to patients without GAD or MDD, t(102) = 2.71, p = .008, Cohen’s d = .26.
The study findings remain consistent regardless of including patients with adjustment disorder in the psychiatric control group.
Conflict of Interest
Ryan J. Lackner, Michael T. Moore, Julia Minerovic, and David M. Fresco declare that they have no conflict of interest.
Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Study procedures were approved by the Kent State University Institutional Review Board. Informed consent was obtained from all individual participants included in the study at the time of enrollment.
Animal Rights
No animal studies were carried out by the authors for this article.
References
- Abramson LY, Seligman MEP, Teasdale JD. Learned helplessness in humans: Critique and reformulation. Journal of Abnormal Psychology. 1978;87:49–74. [PubMed] [Google Scholar]
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Donovan P, Rose DT, Raniere D. Cognitive vulnerability to depression: Theory and evidence. Journal of Cognitive Psychotherapy. 1999;13:5–20. [Google Scholar]
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Tashman NA, Steinberg LD, Donovan P. Depressogenic cognitive styles: Predictive validity, information processing and personality characteristics, and developmental origins. Behaviour Research and Therapy. 1999;37:503–531. doi: 10.1016/s0005-7967(98)00157-0. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Hogan ME, Whitehouse WG, Rose DT, Robinson MS, Lapkin JB. The Temple-Wisconsin Cognitive Vulnerability to Depression Project: lifetime history of axis I psychopathology in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2000;109:403. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. Vol. 32. University of Pennsylvania Press; 1967. [Google Scholar]
- Beck AT. Cognitive theory and the emotional disorders. New York, NY: International Universities Press; 1976. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the beck depression inventory-II 1996 [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Colin S, Sweeney PD, Schaeffer DE. The causality of causal attributions in depression: A cross-lagged panel correlational analysis. Journal of Abnormal Psychology. 1981;90:14–22. doi: 10.1037//0021-843x.90.1.14. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Evans MD, Hollon SD, Garvey MJ, Grove WM, Tuason VB. How does cognitive therapy work? Cognitive change and symptom change in cognitive therapy and pharmacotherapy for depression. Journal of Consulting and Clinical Psychology. 1990;58:862. doi: 10.1037//0022-006x.58.6.862. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, Gallop R. Cognitive therapy vs medications in the treatment of moderate to severe depression. Archives of General Psychiatry. 2005;62:409. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- Etkin A, Schatzberg AF. Common abnormalities and disorder-specific compensation during implicit regulation of emotional processing in generalized anxiety and major depressive disorders. American Journal of Psychiatry. 2011;168:968–978. doi: 10.1176/appi.ajp.2011.10091290. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; Nov, 2002. [Google Scholar]
- Fresco DM, Heimberg RG, Abramowitz A, Bertram TL. The effect of a negative mood priming challenge on dysfunctional attitudes, explanatory style, and explanatory flexibility. British Journal of Clinical Psychology. 2006a;45:167–183. doi: 10.1348/014466505X35137. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Mennin DS, Moore MT, Heimberg RG, Hambrick J. Changes in Explanatory Flexibility Among Individuals with Generalized Anxiety Disorder in an Emotion Evocation Challenge. Cognitive Therapy and Research. 2014;38:416–427. [Google Scholar]
- Fresco DM, Williams NL, Nugent NR. Flexibility and negative affect: Examining the associations of explanatory flexibility and coping flexibility to each other and to depression and anxiety. Cognitive Therapy and Research. 2006b;30:201–210. [Google Scholar]
- Fresco DM, Rytwinski NK, Craighead LW. Explanatory flexibility and negative life events interact to predict depression symptoms. Journal of Social and Clinical Psychology. 2007;26:595–608. [Google Scholar]
- Hollon SD, DeRubeis RJ, Evans MD, Wiemer MJ, Garvey MJ, Grove WM, Tuason VB. Cognitive therapy and pharmacotherapy for depression: Singly and in combination. Archives of General Psychiatry. 1992;49:774. doi: 10.1001/archpsyc.1992.01820100018004. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Garber J. Cognitive therapy. In: Abramson LY, editor. Social cognition and clinical psychology: A synthesis. New York, NY: Guildford Press; 1988. pp. 204–253. [Google Scholar]
- Hollon SD, Kriss MR. Cognitive factors in clinical research and practice. Clinical Psychology Review. 1984;4:35–76. [Google Scholar]
- Hollon SD, DeRubeis RJ, Shelton RC, Amsterdam JD, Salomon RM, O’Reardon JP, Gallop R. Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Archives of General Psychiatry. 2005;62:417. doi: 10.1001/archpsyc.62.4.417. [DOI] [PubMed] [Google Scholar]
- Ingram RE, Hollon SD. Cognitive therapy for depression from an information processing perspective. In: Ingram RE, editor. Information processing approaches to clinical. Personality, psychopathology, and psychotherapy series. San Diego, CA: Academic Press; 1986. pp. 259–281. [Google Scholar]
- Kendall PC, Ingram RE. Cognitive-behavioral perspectives: Theory and research on depression and anxiety. In: Kendall PC, Watson D, editors. Anxiety and depression: Distinctive and overlapping features. New York, NY: Academic Press; 1989. [Google Scholar]
- Mennin DS, Fresco DM. Emotion regulation as an integrative framework for understanding and treating psychopathology. Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment. 2009:356–379. [Google Scholar]
- Miller SM, Shoda Y, Hurley K. Applying cognitive-social theory to health-protective behavior: Breast self-examination in cancer screening. Psychological Bulletin. 1996;119:70–94. doi: 10.1037/0033-2909.119.1.70. [DOI] [PubMed] [Google Scholar]
- Moore MT, Fresco DM. The relationship of explanatory flexibility to explanatory style. Behavior Therapy. 2007;38:325–332. doi: 10.1016/j.beth.2006.06.007. [DOI] [PubMed] [Google Scholar]
- Newman MG, Zuellig AR, Kachin KE, Constantino MJ, Przeworski A, Erickson T, Cashman-McGrath L. Preliminary reliability and validity of the Generalized Anxiety Disorder Questionnaire-IV: A revised self-report diagnostic measure of generalized anxiety disorder. Behavior Therapy. 2002;33:215–233. [Google Scholar]
- Nisita C, Petracca A, Akiskal HS, Galli L, Gepponi I, Cassano GB. Delimitation of generalized anxiety disorder: clinical comparisons with panic and major depressive disorders. Comprehensive Psychiatry. 1990;31:409–415. doi: 10.1016/0010-440x(90)90025-n. [DOI] [PubMed] [Google Scholar]
- Peterson C, Semmel A, von Baeyer C, Abramson LY, Metalsky GI, Seligman ME. The attributional style questionnaire. Cognitive Therapy and Research. 1982;6:287–299. [Google Scholar]
- Rosenbaum M, Ben-Ari K. Learned helplessness and learned resourcefulness. Effects of noncontingent success and failure on individuals differing in self-control skills. Journal of Personality and Social Psychology. 1985;48:198–215. doi: 10.1037//0022-3514.48.1.198. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP. Generalized anxiety and mixed anxiety-depression: Association with disability and health care utilization. Journal of Clinical Psychiatry. 1996 [PubMed] [Google Scholar]
- Safran JD, Vallis TM, Segal ZV, Shaw BF. Assessment of core cognitive processes in cognitive therapy. Cognitive Therapy and Research. 1986;10:509–526. [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: The Guilford Press; 2002. [Google Scholar]
- Seligman ME. Depression and learned helplessness. In: Friedman RJ, Katz MM, editors. The psychology of depression: contemporary theory and research. Oxford: John Wiley & Sons; 1974. [Google Scholar]
- Seligman ME, Castellon C, Cacciola J, Schulman P, Luborsky L, Ollove M, Downing R. Explanatory style change during cognitive therapy for unipolar depression. Journal of Abnormal Psychology. 1988;97:13. doi: 10.1037//0021-843x.97.1.13. [DOI] [PubMed] [Google Scholar]
- Sweeney PD, Anderson K, Bailey S. Attributional style in depression: a meta-analytic review. Journal of Personality and Social Psychology. 1986;50:974. doi: 10.1037//0022-3514.50.5.974. [DOI] [PubMed] [Google Scholar]
- Teasdale JD. Emotional processing, three modes of mind and the prevention of relapse in depression. Behaviour Research and Therapy. 1999;37:S53–S77. doi: 10.1016/s0005-7967(99)00050-9. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Lane RD. Perseverative thinking and health: Neurovisceral concomitants. Psychology and Health. 2002;17:685–695. [Google Scholar]
- Thayer JF, Friedman BH, Borkovec TD. Autonomic characteristics of generalized anxiety disorder and worry. Biological Psychiatry. 1996;39:255–266. doi: 10.1016/0006-3223(95)00136-0. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Friedman BH, Borkovec TD, Johnsen BH, Molina S. Phasic heart period reactions to cued threat and nonthreat stimuli in generalized anxiety disorder. Psychophysiology. 2000;37:361–368. [PubMed] [Google Scholar]
- Ventura J, Liberman RP, Green MF, Shaner A, Mintz J. Training and quality assurance with the Structured Clinical Interview for DSM-IV (SCID-I/P) Psychiatry Research. 1998;79:163–173. doi: 10.1016/s0165-1781(98)00038-9. [DOI] [PubMed] [Google Scholar]


