Abstract
STUDY DESIGN
Cross-sectional.
OBJECTIVES
To compare differences in glenohumeral joint angular motion and linear translations between symptomatic and asymptomatic individuals during shoulder motion performed in 3 planes of humerothoracic elevation.
BACKGROUND
Numerous clinical theories have linked abnormal glenohumeral kinematics, including decreased glenohumeral external rotation and increased superior translation, to individuals with shoulder pain and impingement diagnoses. However, relatively few studies have investigated glenohumeral joint angular motion and linear translations in this population.
METHODS
Transcortical bone pins were inserted into the scapula and humerus of 12 a symptomatic and 10 symptomatic participants for direct bone-fixed tracking using electromagnetic sensors. Glenohumeral joint angular positions and linear translations were calculated during active shoulder flexion, abduction, and scapular plane abduction.
RESULTS
Differences between groups in angular positions were limited to glenohumeral elevation, coinciding with a reduction in scapulothoracic upward rotation. Symptomatic participants demonstrated 1.4 mm more anterior glenohumeral translation between 90° and 120° of shoulder flexion and an average of 1 mm more inferior glenohumeral translation throughout shoulder abduction.
CONCLUSION
Differences in glenohumeral kinematics exist between symptomatic and a symptomatic individuals. The clinical implications of these differences are not yet understood, and more research is needed to understand the relationship between abnormal kinematics, shoulder pain, and pathoanatomy.
Keywords: biomechanics, glenohumeral translations, impingement syndrome
The clinical diagnosis of impingement is the most common diagnostic label for shoulder pain.43 However, the diagnosis is so broadly applied that different tissue pathologies and various and often conflicting pathomechanics may contribute to the pain.4,28 While subtypes of mechanical shoulder impingement (compression and mechanical abrasion of the rotator cuff tendons) have been described biomechanically, they are not well distinguished clinically. Some maintain that a diagnosis of impingement includes all sources of shoulder pain, excluding only a few other conditions such as adhesive capsulitis, gross instability, or cervical referred pain.18 However, without a better understanding of the underlying pathomechanics of the condition, the identification of more specific diagnostic labels is impeded.
Methodological differences and limitations of studies exploring kinematics in individuals with shoulder impingement limit our understanding of the multifactorial etiology of the diagnosis. For example, excessive superior glenohumeral translation is a pathomechanical factor theorized to relate to mechanical shoulder impingement because it may lead to subacromial rotator cuff compression.6,24,31 However, only 1 study provides data to support this theory in patients diagnosed with impingement,6 and that study is limited by 2-dimensional methodology, which may result in inaccurate or incomplete descriptions of joint position.
Abnormalities in anterior/posterior glenohumeral translations are also theorized to be a cause of mechanical impingement.24,40,45 However, few studies have investigated the potential differences in glenohumeral translations between symptomatic and asymptomatic individuals. Surface-based electromagnetic methods are often utilized because, like superior/inferior glenohumeral translations, anterior/posterior translations are challenging to accurately quantify with 2-dimensional methods. However, surface-based measurement techniques, in general, are limited by skin-motion artifact.13,17,25 Because glenohumeral translations are small in magnitude,2,10,24 the impact of errors from surface sensors may be substantial.
Insufficient glenohumeral external rotation during arm raising is also theorized to approximate the greater tuberosity to the acromion, leading to mechanical impingement.5,8,22,28 However, few studies have directly measured differences in external rotation between symptomatic and asymptomatic individuals.21,23 Furthermore, measures of glenohumeral axial rotation are particularly susceptible to skin-motion artifact,13 making potential group differences difficult to identify.
Identifying differences in glenohumeral kinematics in individuals with shoulder pain requires a more accurate and comprehensive approach to address the methodological limitations of previous studies. Therefore, the purpose of this study was to compare differences in glenohumeral joint angular motion and linear translations between symptomatic and asymptomatic individuals during shoulder motion performed in 3 planes of humerothoracic elevation. In combination with a companion article,20 the results of this study allow for a comprehensive investigation into shoulder kinematics associated with shoulder pain and the diagnostic label of impingement.
METHODS
Participants
Ten symptomatic and 12 asymptomatic participants were recruited from community and university settings to participate in this study. Participant demographics are summarized in TABLE 1. The study was approved by the Institutional Review Board of the University of Minnesota, and written informed consent was obtained from all participants prior to testing.
TABLE 1.
Demographic Data*
| Characteristic | Asymptomatic (n = 12) | Symptomatic (n = 10) | P Value |
|---|---|---|---|
| Age, y | 29.3 ± 6.8 | 35.7 ± 13.4 | .165 |
| Gender (male), n | 7 | 5 | 1.000 |
| Height, cm | 173.6 ± 8.1 | 170.3 ± 10.7 | .438 |
| Mass, kg | 77.5 ± 13.8 | 78.6 ± 11.3 | .842 |
| Body mass index, kg/m2 | 25.7 ± 4.3 | 27.3 ± 4.5 | .418 |
| Handedness (right), n | 11 | 10 | 1.000 |
| Dominant side tested, n | 2 | 8 | .008 |
| DASH (0-100) | … | 21.4 ± 10.8 | … |
| Optional work module (0-100) | … | 20.3 ± 22.3 | … |
| Optional sports module (0-100) | … | 49.2 ± 27.0 | … |
| Symptom duration, y | … | 10.0 ± 7.9 | … |
| NPRS (usual shoulder joint symptoms) (0-10) | … | 2.7 ± 1.7 | … |
| NPRS during testing (at bone pin site) (0-10) | 1.9 ± 0.9 | 2.6 ± 2.1 | .104 |
Abbreviations: DASH, Disabilities of the Arm, Shoulder and Hand questionnaire; NPRS, numeric pain rating scale.
Values are mean ± SD unless otherwise indicated.
Potential symptomatic participants were screened by a physical therapist to determine eligibility, based on inclusion/exclusion criteria consistent with a clinical presentation of impingement syndrome.29,35 Symptomatic individuals were included if they were between the ages of 18 and 60 years and had current anterolateral shoulder pain during active motion for more than 1 week in duration. Additionally, potential symptomatic individuals were eligible for inclusion if shoulder pain was provoked during resisted shoulder internal or external rotation, if more than 2 impingement signs were positive (Hawkins-Kennedy, Neer, Jobe),14,16,30 and if evidence of scapular dyskinesia was observed during arm raising or lowering. Potential symptomatic individuals were excluded if screening revealed a 25% or greater reduction of internal or external rotation range of motion in the symptomatic shoulder compared to the contralateral side,38 if shoulder symptoms were provoked during cervical screening, or if drop-arm or apprehension signs were positive. Additionally, symptomatic individuals were excluded if they had a history of shoulder surgery; fracture of the clavicle, scapula, or humerus; labral or rotator cuff tears; known joint diseases; or if their shoulder pain began after a traumatic injury.
To be included in the asymptomatic group, potential participants were required to be 18 to 60 years old and without a history of shoulder pain, shoulder-girdle fractures, dislocations, or separations. Potential participants were excluded from the asymptomatic group if screening identified abnormal or asymmetrical loss of shoulder range of motion, shoulder pain provocation during any impingement tests, or observable scapular dyskinesia.
Procedures
Data were collected utilizing the Flock of Birds miniBIRD electromagnetic system (Ascension Technology Corporation, Shelburne, VT) synced with MotionMonitor software (Innovative Sports Training, Inc, Chicago, IL). Sensors were secured to transcortical bone pins placed into the scapula and humerus, as previously described27 (APPENDIX FIGURE 1, available online). The technical reference frames of the electromagnetic sensors were transformed into clinically meaningful local coordinate systems by palpating and digitizing anatomical landmarks according to the recommendations of the International Society of Biomechanics.46 To represent scapular position in a manner that is more consistent with clinical descriptions, the posterior aspect of the acromioclavicular joint was used rather than the posterolateral acromion.26 Humerothoracic motion was defined as the humerus moving relative to the thorax, resulting in plane of elevation (flexion, scapular plane abduction, abduction), elevation, and axial rotation using a yx'y” rotation sequence.46 Glenohumeral joint angular motion was defined as the humerus moving relative to the scapula, resulting in elevation, plane of elevation (elevation anterior or posterior to the plane defined by the scapula) (FIGURE 1), and axial rotation using an xz'y” rotation sequence.37 Glenohumeral joint angular positions were identified at 5° increments of humerothoracic elevation to create descriptive figures. For statistical analysis, data were reduced to include values at 30°, 60°, 90°, and 120° for flexion and scapular plane abduction. However, because not all participants reached 120° of humerothoracic elevation for shoulder abduction, data were analyzed only to 110° of elevation for this plane. Data were not analyzed below 30° of humerothoracic elevation because the trunk prevents a true 0° position, and an insufficient number of participants' data were available to produce a mean value that was representative.
FIGURE 1.

Glenohumeral plane of elevation describes the anterior/posterior position of the humerus relative to the plane of the scapula. Reprinted with permission from Ludewig et al27 (http://www.jbjs.org).
Glenohumeral translations were described as linear changes in the position of the estimated humeral head center relative to the origin of the scapular reference frame between 2 angles of humerothoracic elevation. To estimate the location of the glenohumeral joint center of rotation, the shoulder was moved through small arcs of passive motion, and a least-squares algorithm was used to find the centroid of minimal translation.1 The resulting glenohumeral translations were defined as anterior/posterior translation and superior/inferior translation of the humeral head relative to the glenoid occurring during intervals of humerothoracic elevation: 30°–60°, 60°–90°, and 90°–120° for shoulder flexion and scapular plane abduction, and 30°–60°, 60°–90°, and 90°–110° for shoulder abduction.
Motion testing was performed in a controlled manner, as described previously.20 Each participant performed 2 repetitions each of shoulder flexion, abduction, and scapular plane abduction, which was defined as 40° anterior to the coronal plane.
Statistical Analysis
Trial-to-trial reliability was calculated using intraclass correlation coefficients (ICC1,1)42 and standard error of measurement.9 After establishing reliability, an average value was calculated for each participant at each angle of humerothoracic elevation, phase of raising and lowering of the arm, and plane of shoulder humerothoracic elevation (flexion, scapular abduction, and abduction). The assumption of normality was tested prior to statistical analysis by inspecting skewness and kurtosis.
The primary statistical analysis utilized 3-factor, mixed-model analyses of variance (ANOVA) for each dependent variable of glenohumeral angular positions and linear translations. The between-subject factor was group (a symptomatic and symptomatic), and the within-subject factors were phase (raising and lowering) and angle of elevation (30°, 60°, 90°, and 110°/120°) for glenohumeral angular positions or elevation intervals (30°–60°, 60°–90°, and 90°–110°/120°) for translations. This analysis was conducted for each plane of movement (abduction, flexion, and scapular plane abduction). Translation data for the lowering phase were transformed by multiplying by −1 to prevent confounding interactions with phase, due to the change in the direction of translations between raising and lowering. Each ANOVA model was analyzed sequentially, with higher-order effects involving the group factor given priority.20 In the presence of interactions, contrast statements were used for pairwise comparisons. To prevent alpha inflation due to multiple comparisons, Tukey-Kramer adjustments were used when appropriate. Baseline demographic information was compared using independent, 2-sample t tests and Fisher exact tests. Independent, 2-sample t tests were also performed to assess for differences in glenohumeral joint angular position during a relaxed standing posture. The type I error rate was set a priori at .05. All statistical analyses were performed using SAS Version 9.3 (SAS Institute Inc, Cary, NC).
RESULTS
Group differences were not found between glenohumeral angular positions during a relaxed standing posture with the arm at the side (TABLE 2). ICCs for glenohumeral rotations ranged from 0.76 to 0.95 (APPENDIX TABLE 1, available online). With the exception of glenohumeral plane of elevation and axial rotation during shoulder abduction, standard error of measurement values were generally less than 3°. Trial-to-trial reliability for translations was excellent, with ICCs ranging from 0.97 to 1.0 and standard error of measurement values less than or equal to 1 mm.
Table 2.
Glenohumeral Angular Positions in Relaxed Standing Posture
| Asymptomatic* | Symptomatic* | P Value | |
|---|---|---|---|
| Humeral elevation | −0.8 ± 1.1 | 2.3 ± 1.4 | .097 |
| Plane of elevation | 3.1 ± 2.3 | −0.4 ± 1.4 | .231 |
| External rotation | 14.1 ± 4.1 | 11.6 ± 2.0 | .615 |
Values are mean ± standard error in degrees.
Glenohumeral Angular Positions
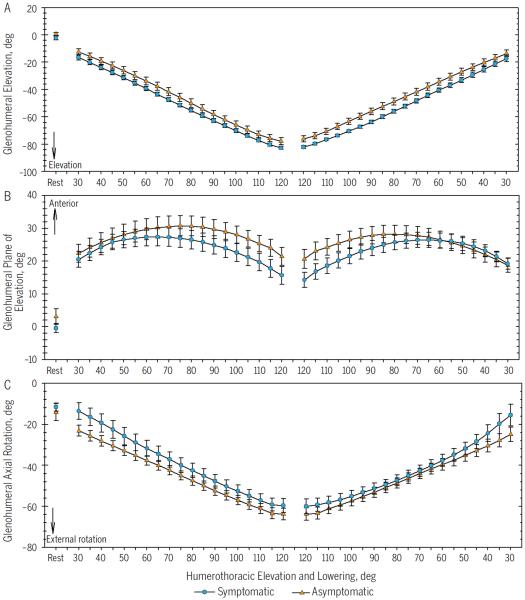
The humerus consistently elevated relative to the glenoid (glenohumeral elevation) with increasing angles of humerothoracic elevation, regardless of the plane of motion (FIGURE 2A; APPENDIX FIGURES 2A and 3A, available online). Group differences existed during shoulder scapular plane abduction and depended on the angle of humerothoracic elevation (P = .005, F = 4.68, df = 3,58) (FIGURE 2A). The symptomatic group had 6.8° more glenohumeral elevation at 30° of humerothoracic elevation (P = .006, F = 8.23, df = 1,58) and 5.6° more glenohumeral elevation at 60° of humerothoracic elevation (P = .022, F = 5.53, df = 1,58).
FIGURE 2.
Glenohumeral joint motion during shoulder scapular plane abduction: (A) elevation, (B) plane of elevation, (C) axial rotation. The symptomatic group had significantly more glenohumeral elevation than the asymptomatic group at 30° and 60°, regardless of the phase (raising/lowering). Values are mean and unpooled standard error in degrees.
The plane of glenohumeral elevation varied depending on the plane of humerothoracic motion in which the participants moved. On average, the plane of glenohumeral elevation was posterior to the plane of the scapula during shoulder abduction (APPENDIX FIGURE 2B, available online), anterior to the plane of the scapula during shoulder flexion (APPENDIX FIGURE 3B, available online), and slightly anterior to the plane of the scapula during shoulder scapular plane abduction (FIGURE 2B). Group differences during shoulder flexion depended on the angle of humerothoracic elevation (P = .006, F = 4.55, df = 3,57). The differences between groups increased as humerothoracic elevation increased, with the humerus of symptomatic participants tending to be less anterior to the plane of the scapula compared to the asymptomatic participants. However, the groups were not found to be significantly different during specific pairwise follow-ups, despite a 7° difference at 120° of humerothoracic elevation (P = .066) (APPENDIX FIGURE 3B, available online).
During both shoulder scapular plane abduction and flexion, the humerus consistently externally rotated relative to the glenoid with increasing angles of humerothoracic elevation (FIGURE 2C; APPENDIX FIGURE 3C, available online). However, during shoulder abduction, the humerus showed a pattern of increasing external rotation until approximately 55° of humerothoracic elevation, followed by decreasing external rotation, or relative internal rotation, for the remainder of the motion (APPENDIX FIGURE 2C, available online). No differences were found between groups at any angle of humerothoracic elevation or between phases of motion.
Glenohumeral Translations
The humeral head consistently translated anteriorly relative to the glenoid during shoulder abduction (FIGURE 3A) and scapular plane abduction (FIGURE 4A) in both the asymptomatic and symptomatic groups. However, during shoulder flexion, both groups demonstrated patterns of slight posterior glenohumeral translation during the 30°–60° interval, followed by anterior translation until 120° of humerothoracic elevation (FIGURE 5A). Differences between groups in the magnitude of glenohumeral anterior translation during shoulder flexion were only significant during the interval between 90° and 120° of humerothoracic elevation, when the symptomatic group demonstrated 1.4 mm more anterior glenohumeral translation (P = .001, F = 8.41, df = 2,37). During shoulder abduction, differences between groups in anterior glenohumeral translation depended on the interval of motion (FIGURE 3A). However, the mean difference between groups in anterior glenohumeral translation during the 30°–60° interval did not reach statistical significance (P = .070, F = 3.48, df = 1,38).
FIGURE 3.
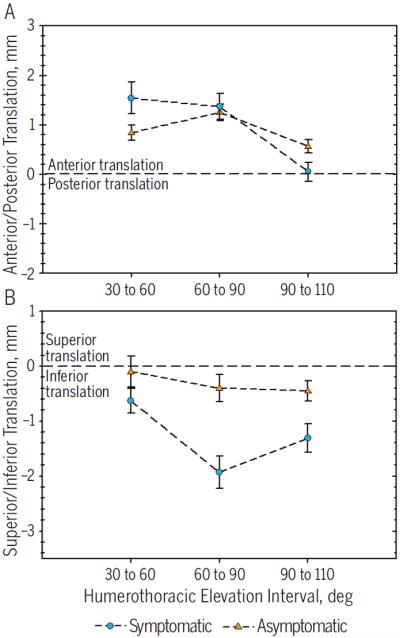
Translations of the humeral head relative to the glenoid during shoulder abduction: (A) anterior/posterior, (B) superior/inferior. On average, the symptomatic group had 1 mm more inferior glenohumeral translation than the asymptomatic group. Positive values indicate anterior and superior translation. Values are mean and unpooled standard error in millimeters.
FIGURE 4.
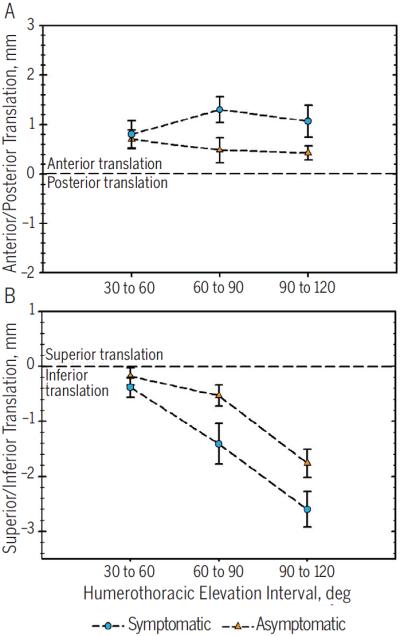
Translations of the humeral head relative to the glenoid during shoulder scapular plane abduction: (A) anterior/posterior, (B) superior/inferior. Positive values indicate anterior and superior translation. Values are mean and unpooled standard error in millimeters.
FIGURE 5.

Translations of the humeral head relative to the glenoid during shoulder flexion: (A) anterior/posterior, (B) superior/inferior. The symptomatic group had 1.4 mm more anterior glenohumeral translation than the asymptomatic group during the interval between 90° and 120° of humerothoracic elevation. Positive values indicate anterior and superior translation. Values are mean and unpooled standard error in millimeters.
Average patterns of superior/inferior glenohumeral translation varied between planes of humerothoracic elevation. During shoulder abduction, the humeral head translated inferiorly relative to the glenoid in both groups, with the symptomatic group having an average of 1.0 mm more translation across all ranges of motion (P = .022, F = 6.18, df = 1,20) (FIGURE 3B). Group differences in inferior glenohumeral translation were not significant during scapular plane abduction (FIGURE 4B) or flexion (FIGURE 5B).
DISCUSSION
The study of glenohumeral joint kinematics is essential to understanding the pathomechanics associated with conditions such as mechanical impingement syndrome. Despite this, few studies have directly investigated glenohumeral kinematics beyond scapulohumeral rhythm and 2-dimensional glenohumeral translations. Furthermore, to our knowledge, none have done so while simultaneously measuring sternoclavicular, acromioclavicular, and scapulothoracic joint kinematics. The results of this study and its companion article20 provide highly accurate measures of shoulder complex kinematics obtained using bone-fixed tracking. The simultaneous collection of multijoint kinematics also facilitates the development of biomechanical theories regarding differences in shoulder kinematics between asymptomatic individuals and those with a clinical presentation consistent with impingement syndrome.
The results of the current study indicate that the differences between groups in glenohumeral kinematics relate to differences in scapulothoracic kinematics. Specifically, during shoulder scapular plane abduction, the symptomatic group demonstrated 7° and 6° more glenohumeral elevation at 30° and 60° of humerothoracic elevation, respectively. In the companion article,20 it was reported that the symptomatic participants also demonstrated 7° and 3° less scapulothoracic upward rotation at 30° and 60° of humerothoracic elevation, respectively. Because these values were obtained from the same positions of humerothoracic elevation, it is expected that a decrease in scapulothoracic upward rotation would correspond to an increase in glenohumeral elevation, although the magnitudes may differ slightly due to the 3-D nature of the motion. The companion article also describes how a reduction in scapulothoracic upward rotation could be related to sternoclavicular and acromioclavicular motion through coupled mechanisms.20 From a biomechanical standpoint, this indicates that the coupled mechanics of the sternoclavicular, acromioclavicular, and scapulothoracic joints influence glenohumeral joint kinematics when positioning the hand in space.
The finding of increased glenohumeral elevation in response to decreased scapulothoracic upward rotation may also provide insight to an important clinical concept. While causality cannot be assumed in this study, these findings may indicate the presence of compensatory mechanisms from which movement impairments may perpetuate throughout the shoulder complex. For example, a case study investigating shoulder complex kinematics in an individual with end-stage glenohumeral osteoarthritis found that a reduction in glenohumeral elevation occurred with a concomitant increase in scapulothoracic and acromioclavicular upward rotation and posterior tilt.3 Together with this case study, the results of the current study indicate that movement impairments at 1 joint within the shoulder complex should not be considered in isolation. Future research is needed to investigate how conditions such as glenohumeral hypermobility and hypomobility relate to changes in sternoclavicular, acromioclavicular, and scapulothoracic kinematics, and how these impairments can be best assessed during a clinical examination.
Numerous researchers and clinicians have theorized that a decrease in glenohumeral external rotation during humeral elevation is related to mechanical impingement, as it prevents clearance of the greater tuberosity and the rotator cuff tendons from under the acromion.5,8,22,28 While group differences in glenohumeral axial rotation were not found in the current study, the experimental setup might have impacted this result. To control for the plane of motion, the participants prepositioned their arm into axial rotation prior to the initiation of elevation in the desired plane. Prepositioning for both groups in this manner negates differences that might otherwise occur during unrestrained shoulder elevation.
Numerous clinical theories have been proposed that relate altered glenohumeral translations to impingement syndrome, including both increased superior glenohumeral translation28,41 and increased anterior or decreased posterior glenohumeral translation.28,40 Interestingly, symptomatic participants in the current study demonstrated an average of 1 mm more inferior glenohumeral translation during abduction than asymptomatic controls. While initially this may seem contradictory to previous literature,6,31,47 careful analysis of these studies suggests that little in vivo data exist to support the clinical theory that increased superior glenohumeral translation is related to impingement. In particular, most studies identifying more superior glenohumeral translations included individuals with known rotator cuff tears,31,47 which alter glenohumeral mechanics.
Only 2 studies have investigated glenohumeral translations in individuals with impingement syndrome.6,24 While Deutsch et al6 found increased superior glenohumeral translations in individuals with impingement, the authors measured translations using 2-dimensional radiographs, which are prone to projection error when translations occur out of the radiographic plane. The only other investigation to compare individuals with impingement to asymptomatic controls did not find a difference in superior/inferior glenohumeral translations between groups.24 Ultimately, the lack of consistent evidence linking greater superior glenohumeral translations to shoulder pain and impingement suggests that clinicians should be cautious about making assumptions regarding uniform movement deviations occurring in patients diagnosed with impingement syndrome.
Clinically, the impact of a 1-mm difference in glenohumeral inferior translations is unclear. Though small, the magnitude must be considered within the context of the available subacromial space. Giphart et al11 studied acromiohumeral distance using biplane fluoroscopy and found that the rotator cuff tendons were in a potential position for compression under the acromion between 34° and 72° of shoulder scapular plane abduction and 36° and 65° of shoulder flexion. At 72° of scapular plane abduction and 65° of flexion, the distance between the undersurface of the acromion and the footprint was a minimum of 3 mm and 3.5 mm, respectively. Therefore, the 1 mm more inferior glenohumeral translation in the symptomatic group may serve as a compensatory strategy to maintain adequate subacromial space and avoid tendon compression during this critical range of motion. However, it is not yet known whether greater inferior glenohumeral translation positively or negatively impacts internal impingement of the tendon articular surface relative to the glenoid. Furthermore, the effect of the increased glenohumeral elevation observed in the symptomatic group at 30° and 60° of humerothoracic elevation during shoulder scapular plane abduction may also influence the available subacromial space. Given that the increased glenohumeral elevation is paired with reduced scapulothoracic upward rotation, it is likely that the range of humerothoracic elevation where the rotator cuff tendons are closest to the acromial undersurface shifts relative to the angles reported by Giphart et al.11
Compared to superior/inferior translations, even less is known about anterior/posterior glenohumeral translations in symptomatic individuals. Only the study by Ludewig and Cook24 compared anterior/posterior glenohumeral translations in symptomatic and asymptomatic individuals in the absence of rotator cuff tears or primary glenohumeral joint instability. During scapular plane abduction, the authors reported that the symptomatic group demonstrated more anterior glenohumeral translation between 30° and 60° of humerothoracic elevation and less posterior translation for the remainder of the motion. The results of the current study differ from the pattern of translation previously reported by Ludewig and Cook,23 as both groups of participants in the current study demonstrated consistent anterior glenohumeral translation during shoulder scapular plane abduction. Furthermore, group differences in anterior/posterior glenohumeral translation were not observed during scapular plane abduction. Methodological differences in the definition and measurement of translations and differences in participant samples likely influenced this disagreement. In particular, the current study described translations of a fixed glenohumeral joint center, whereas the previous work reported translations along a moving instantaneous axis of rotation.23
The results of the current study indicate that the symptomatic group had 1.4 mm more anterior glenohumeral translation between 90° and 120° of humerothoracic elevation during shoulder flexion. The finding of greater anterior glenohumeral translation in the symptomatic group may relate to glenohumeral plane of elevation (FIGURE 1). Given that the plane of humerothoracic elevation, thus humeral position, was controlled by the experimental setup, glenohumeral plane of elevation primarily represents the scapula internally or externally rotating on the humerus. Theoretically, if the humerus is positioned less anteriorly relative to the plane of the scapula, less joint congruency is available to support the humerus on the glenoid and more anterior translation may occur. This theory is supported by the finding that the symptomatic group tended to be in 7° less anterior plane of elevation at 120° of humerothoracic elevation during shoulder flexion, corresponding to the interval in which greater anterior glenohumeral translations were observed.
The presence of greater anterior glenohumeral translation at higher angles of elevation may relate to the pathomechanics of shoulder pain and mechanical impingement. Internal impingement has been found to occur at humerothoracic angles above 110°, when the undersurface of the rotator cuff comes into contact with the glenoid rim.7,34,44 While often described as resulting from a combination of shoulder abduction and full external rotation,12,32,44 several studies have found that internal impingement can occur at higher angles without extreme shoulder axial rotation.7,34,36,44 The addition of a sheer stress to the tendon resulting from greater anterior glenohumeral translation at higher angles of humerothoracic elevation may be particularly detrimental because, compared to the bursal side, the undersurface of the rotator cuff has less tolerance to mechanical stress and is particularly susceptible to sheer forces.19 While the results of this study cannot confirm that internal impingement occurred in these participants, these findings provide potential direction for future investigations aiming to understand the relationship between glenohumeral translations and mechanical impingement of the rotator cuff tendons.
The larger magnitudes of glenohumeral translations in the symptomatic group compared to the asymptomatic group suggest this sample of participants might have presented with subtle glenohumeral hypermobility, which has been theorized to be a potential contributor to shoulder pain and a diagnosis of impingement.28,40 During the physical examination prior to data collection, 3 of the 10 symptomatic participants tested positive for laxity tests (sulcus and/or anterior/posterior load and shift). Exploratory analysis indicated that these 3 participants were not outliers, and the sample data were not found to deviate from a normal distribution. Therefore, the clinical exam findings alone do not appear adequately sensitive to detect increased glenohumeral translations during movement. Furthermore, the presence of laxity on special tests has never been directly linked to increased glenohumeral translations during movement. Objective clinical measures that identify specific movement impairments need to be validated to help clinicians relate the results of the physical examination to functional movement impairments and specific intervention strategies.
Although the finding of greater translations in the symptomatic group differs from the results of Deutsch et al,6 it may be expected, given the multifactorial etiology of impingement.28,40 Without measurement of distances between the rotator cuff footprints and acromion and glenoid, direct mechanical contact cannot be assumed by the presence of symptoms and the diagnosis of impingement syndrome. Additionally, the diagnostic label of impingement has become increasingly challenged, given the largely inhomogeneous patient presentations and the potential for varying movement impairments and pathoanatomical involvement.4,33,39 This is further supported by the high variability of movement patterns between symptomatic individuals observed in this study (APPENDIX TABLES 2 and 3, available online), which directly influences the selection of interventions and treatment goals. For example, 2 commonly considered pathomechanical causes of mechanical impingement are glenohumeral hypermobility and hypomobility.15,28,40 While both findings have been associated with the same clinical diagnosis of impingement, treatment approaches for these opposing movement impairments are considerably different. Therefore, it is likely that subgroups of patients exist within the diagnosis of impingement, and clustering these subgroups by movement impairments would greatly assist the clinician in selecting appropriate manual therapy and exercise-based interventions.
This study has several limitations that should be considered and are discussed in detail in the companion article.20 Briefly, despite the small sample size, consistent and statistically significant differences were found due to the precision of the measurement method. However, given the multifactorial nature of a shoulder impingement diagnosis, the movement deviations identified in this investigation may not apply to all patients presenting with this diagnosis.
As previously noted, the symptomatic and asymptomatic groups differed in regard to arm dominance.20 However, no data exist to suggest that glenohumeral angular position or linear translations differ between dominant and nondominant shoulders. Additionally, glenohumeral translation data were described by calculating an average glenohumeral joint center of rotation. The root-mean-square variance from the calculated center of rotation was controlled to be less than 1 cm. Because the glenohumeral joint center is known not to be a fixed point during shoulder motion, this variance needs to be allowed, but controlled, to provide the most representative centroid to define the fixed joint location that will be tracked. It should also be noted, however, that the average-center method may result in an overestimation of translations compared to an instantaneous-center approach, because the true glenohumeral joint center of rotation is not fixed throughout the motion. Despite this, the average-center approach was used because it is more consistent with clinical descriptions of glenohumeral translations than an instantaneous-center approach.
Finally, the small sample size and between-subject variability limit the statistical power to detect group differences. This limitation was observed in significant interactions that were not always detectable in specific follow-up comparisons between groups. For example, a significant group-by-angle interaction was found for glenohumeral plane of elevation during shoulder flexion, and a mean difference of 7° at 120° of humerothoracic elevation was not significant during a pairwise follow-up test. Using a 5° difference, thought to represent a clinically meaningful difference, and the variance found in the present study, a 24% power was detected. This low power indicates a high probability of a type II error and is likely due to the high between-subject variability associated with this motion.
In summary, physical therapists frequently encounter patients with a diagnosis of impingement due to the broad usage of the diagnostic label in individuals with shoulder pain. Our study adds to the existing data,6,24 providing support for various theories of glenohumeral pathomechanics in these patients. Not unexpectedly, there was substantial variability in the patterns of movements described among participants. This variability should be considered when performing a movement examination for these patients. The study by Deutsch et al6 provides support that some patients may demonstrate greater superior glenohumeral translation during shoulder elevation, possibly contributing to subacromial mechanical impingement. Our data, however, provide support for the theory that other subgroups of movement impairments exist, including people with glenohumeral translations that differ from what has been classically described. Our participants also demonstrated greater glenohumeral elevation related to reduced scapulothoracic upward rotation.20 While greater inferior glenohumeral translation may be a beneficial compensation to reduce potential subacromial compression, the other movement deviations identified are believed to increase the potential for rotator cuff compression or mechanical impingement.
Future research is needed to cluster movement impairments into clear and informative diagnostic labels that guide clinical decision making. Additionally, our data demonstrated differences in glenohumeral translations between groups that were not detected by standard clinical laxity testing. More research is needed to refine and validate clinical examination methods so that movement impairments can be effectively used to guide treatment.
CONCLUSION
Differences in glenohumeral kinematics exist between symptomatic and asymptomatic individuals. Group differences in glenohumeral angular positions were limited to elevation of the arm, coinciding with a reduction in scapulothoracic upward rotation reported in the companion paper.20 Symptomatic participants had greater inferior glenohumeral translations during abduction and greater anterior glenohumeral translations during flexion. The clinical implications of these differences are not yet fully understood, and more research is needed to understand the relationship between kinematic abnormalities, pathoanatomy, shoulder pain, and conditions such as mechanical impingement.
KEY POINTS.
FINDINGS: Compared to the asymptomatic group, the symptomatic group had increased glenohumeral inferior and anterior translations and increased glenohumeral elevation.
IMPLICATIONS: Patients with a clinical presentation consistent with impingement syndrome may present with increased glenohumeral translations that may or may not be detectable during a physical examination.
CAUTION: This study was limited by a small sample size. The diagnostic label of impingement is very broad and multifactorial, which may result in subgroups of patients with different patterns of movement.
ACKNOWLEDGEMENTS
The authors would like to thank the Foundation for Physical Therapy for its support in this project through the Florence P. Kendall Doctoral Scholarship (R.L.L., J.L.S.). The project was also supported by award number K01HD042491 from the Eunice Kennedy Shriver National Institutes of Child Health and Human Development (P.M.L.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institutes of Child Health and Human Development or the National Institutes of Health. This project was also supported by a predoctoral training grant (5T32AR050938-09) through the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R.L.L.).
This study was approved by the Institutional Review Board of the University of Minnesota. This study was funded by grants NIH/NCMRR K01HD042491 (P.M.L.), NIH/NIAMS 5T32AR050938-09 (R.L.L.), and by the Foundation for Physical Therapy (R.L.L. and J.L.S.). The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
ONLINE APPENDIX
JOINT-SPECIFIC PATTERNS OF MOTION
TABLE 2 presents descriptive classifications of trends in glenohumeral joint position changes during humerothoracic elevation. This was accomplished by categorizing individual participants' patterns of motion from rest to 120°. The following operational definitions were used:
Constant: a near-linear change in position over time (eg, constantly elevating)
Changing: inconsistency in the direction of position change over time (eg, internally, then externally rotating)
No change: less than 1° change in joint position over the range of motion
TABLE 1.
Intraclass Correlation Coefficients for Trial-to-Trial Reliability*
| Asymptomatic | Symptomatic | |||||
|---|---|---|---|---|---|---|
| Abduction | Flexion | SAB | Abduction | Flexion | SAB | |
| Glenohumeral joint position | ||||||
| Elevation | 0.86 (2.1) | 0.95 (1.7) | 0.92 (1.1) | 0.78 (2.2) | 0.76 (2.1) | 0.91 (1.7) |
| Plane of elevation | 0.87 (2.6) | 0.95 (2.0) | 0.94 (2.1) | 0.89 (6.7) | 0.90 (2.3) | 0.86 (2.9) |
| Axial rotation | 0.92 (3.0) | 0.92 (2.5) | 0.94 (2.3) | 0.86 (7.3) | 0.95 (2.6) | 0.92 (2.8) |
| Glenohumeral translation | ||||||
| Anterior/posterior | 1.00 (0.5) | 0.99 (1.0) | 1.00 (0.7) | 0.99 (1.7) | 0.99 (0.7) | 0.99 (0.8) |
| Superior/inferior | 0.97 (0.6) | 0.98 (1.1) | 0.99 (0.7) | 0.98 (1.9) | 0.97 (0.9) | 0.98 (0.7) |
Abbreviation: SAB, scapular plane abduction.
Values are intraclass correlation coefficient (standard error of measurement in degrees for position and mm for translations). Values represent the average reliability across all phases (raising/lowering) and angles of humerothoracic elevation for joint position (30°, 60°, 90°, 110°/120°) or intervals of humerothoracic elevation for translations (30°–60°, 60°–90°, 90°–110°/120°).
TABLE 2.
Patterns of Glenohumeral Joint Angular Position*
| Abduction | Flexion | Scapular Plane Abduction | ||||
|---|---|---|---|---|---|---|
| Asymptomatic (n = 12) | Symptomatic (n = 10) | Asymptomatic (n = 12) | Symptomatic (n = 10) | Asymptomatic (n = 12) | Symptomatic (n = 10) | |
| Elevation | ||||||
| Constant elevation | 12 (100) | 10 (100) | 12 (100) | 10 (100) | 12 (100) | 10 (100) |
| Plane of elevation | ||||||
| Decreasing (more posterior) | 5 (42) | 8 (80) | 0 (0) | 1 (10) | 2 (17) | 7 (70) |
| Increasing (more anterior) | 0 (0) | 0 (0) | 1 (8) | 0 (0) | 3 (25) | 0 (0) |
| Changing | 7 (58) | 1 (10) | 11 (92) | 8 (80) | 3 (25) | 2 (20) |
| No change | 0 (0) | 1 (10) | 0 (0) | 1 (10) | 4 (33) | 1 (10) |
| Glenohumeral IR/ER | ||||||
| Constant IR | 7 (58) | 3 (30) | 0 (0) | 0 (0) | 0 (0) | 1 (10) |
| Constant ER | 0 (0) | 1 (10) | 12 (100) | 10 (100) | 9 (75) | 8 (80) |
| Changing IR/ER | 5 (42) | 4 (40) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| No change | 0 (0) | 2 (20) | 0 (0) | 0 (0) | 3 (25) | 1 (10) |
Abbreviations: ER, external rotation; IR, internal rotation.
Values are n (%) of participants demonstrating each pattern of motion.
TABLE 3.
Patterns of Glenohumeral Joint Linear Translations*
| Abduction | Flexion | Scapular Plane Abduction | ||||
|---|---|---|---|---|---|---|
| Asymptomatic (n = 11) | Symptomatic (n = 9) | Asymptomatic (n = 10) | Symptomatic (n = 9) | Asymptomatic (n = 11) | Symptomatic (n = 9) | |
| Translation | ||||||
| Anterior | 11 (100) | 7 (78) | 8 (80) | 7 (78) | 8 (73) | 6 (67) |
| Posterior | 0 (0) | 2 (22) | 2 (20) | 2 (22) | 3 (27) | 3 (33) |
| Superior | 3 (27) | 1 (11) | 2 (20) | 1 (11) | 1 (9) | 1 (11) |
| Inferior | 8 (73) | 8 (89) | 8 (80) | 8 (89) | 10 (91) | 8 (89) |
Values are n (%) of participants demonstrating each pattern of motion.
FIGURE 1.

Experimental setup with bone-pin insertion into clavicle, scapula, and humerus.
FIGURE 2.
Glenohumeral joint motion during shoulder abduction: (A) elevation, (B) plane of elevation, (C) axial rotation. Values are mean and unpooled standard error in degrees.
FIGURE 3.
Glenohumeral joint motion during shoulder flexion: (A) elevation, (B) plane of elevation, (C) axial rotation. Values are mean and unpooled standard error in degrees.
REFERENCES
- 1.An KN, Korinek SL, Kilpela T, Edis S. Kinematic and kinetic analysis of push-up exercise. Biomed Sci Instrum. 1990;26:53–57. [PubMed] [Google Scholar]
- 2.Bey MJ, Kline SK, Zauel R, Lock TR, Kolowich PA. Measuring dynamic in-vivo glenohumeral joint kinematics: technique and preliminary results. J Biomech. 2008;41:711–714. doi: 10.1016/j.jbiomech.2007.09.029. http://dx.doi.org/10.1016/j.jbiomech.2007.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braman JP, Thomas BM, LaPrade RF, Phadke V, Ludewig PM. Three-dimensional in vivo kinematics of an osteoarthritic shoulder before and after total shoulder arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010;18:1774–1778. doi: 10.1007/s00167-010-1167-4. http://dx.doi.org/10.1007/s00167-010-1167-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braman JP, Zhao KD, Lawrence RL, Harrison AK, Ludewig PM. Shoulder impingement revisited: evolution of diagnostic understanding in orthopedic surgery and physical therapy. Med Biol Eng Comput. 2014;52:211–219. doi: 10.1007/s11517-013-1074-1. http://dx.doi.org/10.1007/s11517-013-1074-1. [DOI] [PubMed] [Google Scholar]
- 5.Brossmann J, Preidler KW, Pedowitz RA, White LM, Trudell D, Resnick D. Shoulder impingement syndrome: influence of shoulder position on rotator cuff impingement—an anatomic study. AJR Am J Roentgenol. 1996;167:1511–1515. doi: 10.2214/ajr.167.6.8956588. http://dx.doi.org/10.2214/ajr.167.6.8956588. [DOI] [PubMed] [Google Scholar]
- 6.Deutsch A, Altchek DW, Schwartz E, Otis JC, Warren RF. Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5:186–193. doi: 10.1016/s1058-2746(05)80004-7. [DOI] [PubMed] [Google Scholar]
- 7.Edelson G, Teitz C. Internal impingement in the shoulder. J Shoulder Elbow Surg. 2000;9:308–315. doi: 10.1067/mse.2000.105449. http://dx.doi.org/10.1067/mse.2000.105449. [DOI] [PubMed] [Google Scholar]
- 8.Flatow EL, Soslowsky LJ, Ticker JB, et al. Excursion of the rotator cuff under the acromion. Patterns of subacromial contact. Am J Sports Med. 1994;22:779–788. doi: 10.1177/036354659402200609. [DOI] [PubMed] [Google Scholar]
- 9.Fleiss JL. The Design and Analysis of Clinical Experiments. John Wiley & Sons; New York, NY: 1986. Reliability of measurement; pp. 1–32. [Google Scholar]
- 10.Giphart JE, Brunkhorst JP, Horn NH, Shelburne KB, Torry MR, Millett PJ. Effect of plane of arm elevation on glenohumeral kinematics: a normative biplane fluoroscopy study. J Bone Joint Surg Am. 2013;95:238–245. doi: 10.2106/JBJS.J.01875. http://dx.doi.org/10.2106/JBJS.J.01875. [DOI] [PubMed] [Google Scholar]
- 11.Giphart JE, van der Meijden OA, Millett PJ. The effects of arm elevation on the 3-dimensional acromiohumeral distance: a biplane fluoroscopy study with normative data. J Shoulder Elbow Surg. 2012;21:1593–1600. doi: 10.1016/j.jse.2011.11.023. http://dx.doi.org/10.1016/j.jse.2011.11.023. [DOI] [PubMed] [Google Scholar]
- 12.Gold GE, Pappas GP, Blemker SS, et al. Abduction and external rotation in shoulder impingement: an open MR study on healthy volunteers–initial experience. Radiology. 2007;244:815–822. doi: 10.1148/radiol.2443060998. http://dx.doi.org/10.1148/radiol.2443060998. [DOI] [PubMed] [Google Scholar]
- 13.Hamming D, Braman JP, Phadke V, LaPrade RF, Ludewig PM. The accuracy of measuring glenohumeral motion with a surface humeral cuff. J Biomech. 2012;45:1161–1168. doi: 10.1016/j.jbiomech.2012.02.003. http://dx.doi.org/10.1016/j.jbiomech.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hawkins RJ, Abrams JS. Impingement syndrome in the absence of rotator cuff tear (stages 1 and 2) Orthop Clin North Am. 1987;18:373–382. [PubMed] [Google Scholar]
- 15.Heyworth BE, Williams RJ., 3rd Internal impingement of the shoulder. Am J Sports Med. 2009;37:1024–1037. doi: 10.1177/0363546508324966. http://dx.doi.org/10.1177/0363546508324966. [DOI] [PubMed] [Google Scholar]
- 16.Jobe FW, Pink M. Classification and treatment of shoulder dysfunction in the overhead athlete. J Orthop Sports Phys Ther. 1993;18:427–432. doi: 10.2519/jospt.1993.18.2.427. http://dx.doi.org/10.2519/jospt.1993.18.2.427. [DOI] [PubMed] [Google Scholar]
- 17.Karduna AR, McClure PW, Michener LA, Sennett B. Dynamic measurements of three-dimensional scapular kinematics: a validation study. J Biomech Eng. 2001;123:184–190. doi: 10.1115/1.1351892. [DOI] [PubMed] [Google Scholar]
- 18.Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the `scapular summit. Br J Sports Med. 2013;47:877–885. doi: 10.1136/bjsports-2013-092425. http://dx.doi.org/10.1136/bjsports-2013-092425. [DOI] [PubMed] [Google Scholar]
- 19.Lake SP, Miller KS, Elliott DM, Soslowsky LJ. Tensile properties and fiber alignment of human supraspinatus tendon in the transverse direction demonstrate inhomogeneity, nonlinearity, and regional isotropy. J Biomech. 2010;43:727–732. doi: 10.1016/j.jbiomech.2009.10.017. http://dx.doi.org/10.1016/j.jbiomech.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawrence RL, Braman JP, LaPrade RF, Ludewig PM. Comparison of 3-dimensional shoulder complex kinematics in individuals with and without shoulder pain, part 1: sternoclavicular, acromioclavicular, and scapulothoracic joints. J Orthop Sports Phys Ther. 2014;44:636–645. doi: 10.2519/jospt.2014.5339. http://dx.doi.org/10.2519/jospt.2014.5339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin JJ, Hanten WP, Olson SL, et al. Functional activity characteristics of individuals with shoulder dysfunctions. J Electromyogr Kinesiol. 2005;15:576–586. doi: 10.1016/j.jelekin.2005.01.006. http://dx.doi.org/10.1016/j.jelekin.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 22.Ludewig PM, Braman JP. Shoulder impingement: biomechanical considerations in rehabilitation. Man Ther. 2011;16:33–39. doi: 10.1016/j.math.2010.08.004. http://dx.doi.org/10.1016/j.math.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 24.Ludewig PM, Cook TM. Translations of the humerus in persons with shoulder impingement symptoms. J Orthop Sports Phys Ther. 2002;32:248–259. doi: 10.2519/jospt.2002.32.6.248. http://dx.doi.org/10.2519/jospt.2002.32.6.248. [DOI] [PubMed] [Google Scholar]
- 25.Ludewig PM, Cook TM, Shields RK. Comparison of surface sensor and bone-fixed measurement of humeral motion. J Appl Biomech. 2002;18:163–170. [Google Scholar]
- 26.Ludewig PM, Hassett DR, LaPrade RF, Camargo PR, Braman JP. Comparison of scapular local coordinate systems. Clin Biomech (Bristol, Avon) 2010;25:415–421. doi: 10.1016/j.clinbiomech.2010.01.015. http://dx.doi.org/10.1016/j.clinbiomech.2010.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ludewig PM, Phadke V, Braman JP, Hassett DR, Cieminski CJ, LaPrade RF. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg Am. 2009;91:378–389. doi: 10.2106/JBJS.G.01483. http://dx.doi.org/10.2106/JBJS.G.01483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol, Avon) 2003;18:369–379. doi: 10.1016/s0268-0033(03)00047-0. [DOI] [PubMed] [Google Scholar]
- 29.Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90:1898–1903. doi: 10.1016/j.apmr.2009.05.015. http://dx.doi.org/10.1016/j.apmr.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 30.Neer CS., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54:41–50. [PubMed] [Google Scholar]
- 31.Paletta GA, Jr., Warner JJ, Warren RF, Deutsch A, Altchek DW. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elbow Surg. 1997;6:516–527. doi: 10.1016/s1058-2746(97)90084-7. http://dx.doi.org/10.1016/S1058-2746(97)90084-7. [DOI] [PubMed] [Google Scholar]
- 32.Paley KJ, Jobe FW, Pink MM, Kvitne RS, ElAttrache NS. Arthroscopic findings in the overhand throwing athlete: evidence for posterior internal impingement of the rotator cuff. Arthroscopy. 2000;16:35–40. doi: 10.1016/s0749-8063(00)90125-7. http://dx.doi.org/10.1016/S0749-8063(00)90125-7. [DOI] [PubMed] [Google Scholar]
- 33.Papadonikolakis A, McKenna M, Warme W, Martin BI, Matsen FA., 3rd Published evidence relevant to the diagnosis of impingement syndrome of the shoulder. J Bone Joint Surg Am. 2011;93:1827–1832. doi: 10.2106/JBJS.J.01748. http://dx.doi.org/10.2106/JBJS.J.01748. [DOI] [PubMed] [Google Scholar]
- 34.Pappas GP, Blemker SS, Beaulieu CF, McAdams TR, Whalen ST, Gold GE. In vivo anatomy of the Neer and Hawkins sign positions for shoulder impingement. J Shoulder Elbow Surg. 2006;15:40–49. doi: 10.1016/j.jse.2005.04.007. http://dx.doi.org/10.1016/j.jse.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 35.Park HB, Yokota A, Gill HS, El Rassi G, Mc-Farland EG. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Joint Surg Am. 2005;87:1446–1455. doi: 10.2106/JBJS.D.02335. http://dx.doi.org/10.2106/JBJS.D.02335. [DOI] [PubMed] [Google Scholar]
- 36.Petersen BW, Nystrom CS, Pham TD, et al. Effects of elevation angle and plane of motion on subacromial and internal impingement [abstract] J Orthop Sports Phys Ther. 2010;40:A68. http://dx.doi.org/10.2519/jospt.2010.40.1.A52. [Google Scholar]
- 37.Phadke V, Braman JP, LaPrade RF, Ludewig PM. Comparison of glenohumeral motion using different rotation sequences. J Biomech. 2011;44:700–705. doi: 10.1016/j.jbiomech.2010.10.042. http://dx.doi.org/10.1016/j.jbiomech.2010.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rundquist PJ, Anderson DD, Guanche CA, Ludewig PM. Shoulder kinematics in subjects with frozen shoulder. Arch Phys Med Rehabil. 2003;84:1473–1479. doi: 10.1016/s0003-9993(03)00359-9. [DOI] [PubMed] [Google Scholar]
- 39.Schellingerhout JM, Verhagen AP, Thomas S, Koes BW. Lack of uniformity in diagnostic labeling of shoulder pain: time for a different approach. Man Ther. 2008;13:478–483. doi: 10.1016/j.math.2008.04.005. http://dx.doi.org/10.1016/j.math.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 40.Seitz AL, McClure PW, Finucane S, Board-man ND, 3rd, Michener LA. Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both? Clin Biomech (Bristol, Avon) 2011;26:1–12. doi: 10.1016/j.clinbiomech.2010.08.001. http://dx.doi.org/10.1016/j.clinbiomech.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 41.Sharkey NA, Marder RA. The rotator cuff opposes superior translation of the humeral head. Am J Sports Med. 1995;23:270–275. doi: 10.1177/036354659502300303. [DOI] [PubMed] [Google Scholar]
- 42.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 43.van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and manage ment. Ann Rheum Dis. 1995;54:959–964. doi: 10.1136/ard.54.12.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walch G, Boileau P, Noel E, Donell ST. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg. 1992;1:238–245. doi: 10.1016/S1058-2746(09)80065-7. http://dx.doi.org/10.1016/S1058-2746(09)80065-7. [DOI] [PubMed] [Google Scholar]
- 45.Warner JJ, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Patterns of flexibility, laxity, and strength in normal shoulders and shoulders with instability and impingement. Am J Sports Med. 1990;18:366–375. doi: 10.1177/036354659001800406. [DOI] [PubMed] [Google Scholar]
- 46.Wu G, van der Helm FC, Veeger HE, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38:981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]
- 47.Yamaguchi K, Sher JS, Andersen WK, et al. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9:6–11. doi: 10.1016/s1058-2746(00)90002-8. [DOI] [PubMed] [Google Scholar]