Abstract
Background
Post-traumatic stress disorder (PTSD) in Veterans is associated with increased sexual risk behaviors, but the nature of this association is not well understood. Typical PTSD measurement deriving a summary estimate of symptom severity over a period of time precludes inferences about symptom variability, and whether momentary changes in symptom severity predict risk behavior.
Methods
We assessed the feasibility of measuring daily PTSD symptoms, substance use, and high-risk sexual behavior in Veterans using ecological momentary assessment (EMA). Feasibility indicators were survey completion, PTSD symptom variability, and variability in rates of substance use and sexual risk behavior. Nine male Veterans completed web-based questionnaires by cell phone three times per day for 28 days.
Results
Median within-day survey completion rates maintained near 90%, and PTSD symptoms showed high within-person variability, ranging up to 59 points on the 80-point scale. Six Veterans reported alcohol or substance use, and substance users reported use of more than one drug. Eight Veterans reported 1 to 28 high-risk sexual events. Heightened PTSD-related negative affect and externalizing behaviors preceded high-risk sexual events. Greater PTSD symptom instability was associated with having multiple sexual partners in the 28-day period.
Limitations
These results are preliminary, given this small sample size, and multiple comparisons, and should be verified with larger Veteran samples.
Conclusions
Results support the feasibility and utility of using of EMA to better understand the relationship between PTSD symptoms and sexual risk behavior in Veterans. Specific antecedent-risk behavior patterns provide promise for focused clinical interventions.
Keywords: PTSD, Veterans, Sexual Risk, HIV, Substance Use, EMA
Introduction
Of the 1.9 million Veterans returning from Operations Enduring Freedom, Iraqi Freedom, and New Dawn (OEF/OIF/OND), approximately 13% (over 250,000) have screened positive for post-traumatic stress disorder (PTSD) (Dursa, Reinhard, Barth, & Schneiderman, 2014), a multi-factored disorder associated with elevated rates of risk-taking behavior in Veterans (Boscarino, 2006; Drescher, Rosen, Burling, & Foy, 2003; Jacobson et al., 2008; Kuhn, Drescher, Ruzek, & Rosen, 2010), including high-risk sexual behavior. In recent studies, OEF/OIF Veterans with PTSD reported high rates of recent unprotected sex, sex under the influence of drugs or alcohol, and sex with casual and multiple partners (Strom et al., 2012), and were 57% more likely than Veterans without PTSD to report recently risking getting a sexually transmitted disease (Adler, Britt, Castro, McGurk, & Bliese, 2011). This information is particularly relevant in light of studies identifying elevated rates of HIV (Owens et al., 2007; Valdiserri, Rodriguez, & Holodniy, 2008) and other sexually transmitted infections (Goulet, 2013) among Veterans, and underutilization of available HIV testing (Goulet, 2013; Valdiserri et al., 2008).
Despite a pressing need to improve health outcomes for Veterans, the nature of the relationship between PTSD symptoms and high-risk sexual behavior is not well understood, in part because of how PTSD is measured. For example, the PTSD Checklist for the Diagnostic and Statistical Manual – 5th edition (PCL-5) (Weathers et al., 2013) derives a single estimate of past-month symptom severity. This aggregation precludes inferences about symptom variability across days, and how severity at a given moment, or instability over time, may predict high-risk sexual events.
Ecological momentary assessment (EMA) techniques involve repeatedly assessing momentary experiences in real time (Shiffman, Stone, & Hufford, 2008; Stone & Shiffman, 1994). These techniques produce rich longitudinal data that permit insight into event sequences that cannot be explored with summary, cross-sectional data. EMA of PTSD symptoms and high-risk sexual behavior can elucidate Veterans’ day-to-day experiences of symptoms and how these relate temporally to sexual risk events.
A small number of recent studies have demonstrated the feasibility of assessing daily PTSD symptoms in OEF/OIF/OND Veterans. In one study, Veterans had high completion rates (86%) with four daily assessments of PTSD symptoms (using PCL-IV), affect, and substance use over a 28-day period using telephone-delivered interactive voice response recording, when cell phones were provided to them (Possemato et al., 2012). Using palm-top computers, Gaher and colleagues (2014) measured PTSD symptoms with an adapted PCL-IV-symptom checklist 8 times per day for 2 weeks, demonstrating good (70%) compliance with randomly-prompted surveys, and a significant positive relationship between PTSD symptoms recorded during the day and evening alcohol use. Both studies reported significant decreases in PTSD symptoms over the course of the study.
Using a daily life-charting instrument, a small study involving combat-exposed Veterans compared self-ratings of worst PTSD symptoms within symptom clusters to monthly symptom ratings, finding these were highly correlated (Westermeyer et al., 2015).
To our knowledge, no study has combined daily PTSD measures with assessment of high-risk sexual behavior in Veterans. This study is the first in a series of planned studies applying EMA techniques to assess PTSD symptoms and high-risk sexual behavior in real time, and model the temporal relationship between these variables in OEF/OIF/OND Veterans. In this study, we evaluated the feasibility of assessing, by web-based survey, daily PTSD symptoms, high-risk sexual behavior, and substance use in a sample of male Veterans. Feasibility was assessed with regard to daily survey completion, variability in PTSD symptoms, rates of self-reported high-risk sexual events and substance use.
Methods
All study procedures were approved by the Institutional Review Boards of VA Connecticut Healthcare System and Yale University.
Participants
Veterans were recruited between April and August, 2014 from two Department of Veterans Affairs (VA) outpatient clinics in Connecticut. Potential participants were Veterans applying for service-connection benefits for PTSD, and Veterans receiving PTSD-related outpatient treatment. Inclusion criteria were male gender, OEF/OIF/OND Veteran status, reliable access to phone and internet for 28 days, demonstration of understanding of the terms of participation as outlined in the consent form, and self-reported high-risk sexual behavior in the past 28 days, defined as unprotected vaginal, anal, or oral sex, or sex under the influence of drugs or alcohol with a partner who was not a legal spouse or cohabitating partner with whom the participant had an exclusive sexual relationship (Meyers et al., 2008)
Ten Veterans consented to participate, and one withdrew before completing any assessments. The nine who participated had a mean age of 34 years (SD=8.44, Range 24–51); four (44%) identified as White Non-Hispanic; four (44%) were Black Non-Hispanic, and one (11%) was Hispanic.
EMA procedures
Following orientation to EMA procedures, Veterans received three calls per day, randomly timed within the three 5-hour intervals between 7am and 10pm, for 28 days. Each call prompted completion of a web-based survey at that time.
The survey, created with REDCap survey software (Harris et al., 2009), comprised assessments of PTSD symptoms and substance use in the past two hours, and high-risk sexual behavior since the last completed survey. Participants completed surveys using their own smartphones or computers. Entries were automatically date-and time-stamped.
PCL-5 (Weathers et al., 2013): The standard 20-item assessment was amended to inquire about PTSD symptoms in the last 2 hours (rather than past month). The instrument’s seven symptom dimensions (using standard-scored items) assess severity of re-experiencing (items 1–5), avoidance (items 6–7), negative affect (items 8–11), anhedonia (items 12–14), externalizing behaviors (items 15–16), anxious arousal (items 17–18), and dysphoric arousal (items 19–20) symptoms (Armour et al., 2014). High-risk Sexual Behavior: Items inquired about sexual events since the last completed survey, including the number and types of sexual contact (oral, vaginal, and anal), partner characteristics (gender, regular/not regular partner), substance use at the time of sexual event, and condom use. For this study, regular partner was defined as the person with whom the participant regularly had sex. All other partners were defined as not regular partners.
Substance Use: The number of standard alcoholic drinks consumed, and any use of marijuana, cocaine, opiates, and “other” drugs in the past 2 hours were recorded.
Participants were paid $2.50 for each survey completed within the day of the call prompt, and an additional $2.50 for each day that all three surveys were completed within 2 hours of prompts.
Qualitative interview
Following the EMA period, participants were interviewed about the acceptability of daily calls, accessibility of the web-based survey, content of survey items, and reasons for skipped items. With participant consent, interviews were audio-recorded and transcribed. Participants who completed interviews were compensated $20.
All payment was made at the end of study participation, with total payment ranging from $117.50 to $280 of the possible $300 (M = $222, SD=$59).
Data analysis
EMA survey completion was calculated as the percentage of prompted surveys completed within the same calendar day, and within 2 hours of the call prompt. Pearson’s correlation coefficient estimated the linear relationship between the number of surveys completed over 28 days and overall PTSD symptom severity and symptom instability (measures described below).
High-risk sexual behavior was summarized as the total number of high-risk events, and the number of concurrent sexual partners.
Drug and alcohol use were summarized as the percentage of participants using each substance and the within-person percentage of completed questionnaires in which use of any substance was endorsed. Alcohol use to intoxication was defined as five or more drinks recorded for a 2-hour window (NIAAA, 2004), and was differentiated from drinking less than that amount.
Overall PTSD symptom severity was measured by the within-person mean of all momentary PCL-5 sum scores. Daily variability in symptom severity was assessed as the within-person standard deviation and range of PCL-5 sum scores, and the mean square successive difference (MSSD) between PCL-5 scores, a measure of symptom instability that takes into account both overall variability and statistical non-independence of scores over time (Jahng, Wood, & Trull, 2008). MSSD was computed for each participant as the mean of the squared differences between each pair of adjacent PCL-5 scores.
Changes in PTSD symptom severity and instability that might have suggested reactivity to daily assessment were evaluated. The mean of all momentary PCL-5 sum scores, and MSSD were calculated for each of four weeks and change in these measures over time was assessed by repeated measures ANOVA.
As a preliminary assessment of the temporal relationship between PTSD symptoms and risk behavior, PCL total and subscale sum scores were averaged within person for intervals immediately preceding risky sexual events and intervals not preceding those events, and paired t-tests estimated the mean difference. Mean Cohen’s d effect sizes (within-person mean difference in PCL scores between risk- and non-risk intervals divided by the standard deviation of scores for non-risk intervals), were also calculated.
Independent samples t-test compared symptom instability (MSSD) for participants reporting multiple sexual partners to those who did not. Correlation analysis estimated the linear relationship between MSSD and number of risk events.
For this small-sample, exploratory study, all statistical tests used an alpha level of .10.
Results
Survey Completion
Rates of survey completion within the day of the prompt ranged from 42% to 99% (28–day Mdn = 90.5%). Median weekly completion rates were 90%, 88%, 90%, and 93% for weeks 1–4, respectively. Completion rates within 2 hours of the call prompt were lower at 79%, 74%, 81%, and 52% for weeks 1–4, respectively. The number of surveys completed was not significantly correlated with overall PTSD symptom severity (r=−.55, p=.12), nor with symptom instability (MSSD; r=.23, p=.55).
Risk Behavior
All participants reported sexual events with female partners only. One reported only condom-protected sexual events, and thus no high-risk events. Eight participants (89%) reported unprotected sex with a non-cohabiting partner (range 1–28 events). Five of the eight participants (63%) reported sex under the influence of drugs or alcohol with a non-cohabiting partner (range 1 – 15 events), and four (50%) reported unprotected sex with more than one person in the 28-day period.
Four participants (44%) reported drug use, six (67%) reported any alcohol use, and three (33%) reported binge drinking. All drug-use reporters recorded use of more than one drug, and the majority (3/4, 75%) reported opiate use. The proportion of completed surveys in which any drug use was reported ranged from 24% to 75%. Among alcohol users, drinking was reported in 1% to 82% of completed surveys, and binge drinking was reported in 1% to 21% of completed surveys among the three participants reporting any.
PTSD Symptoms
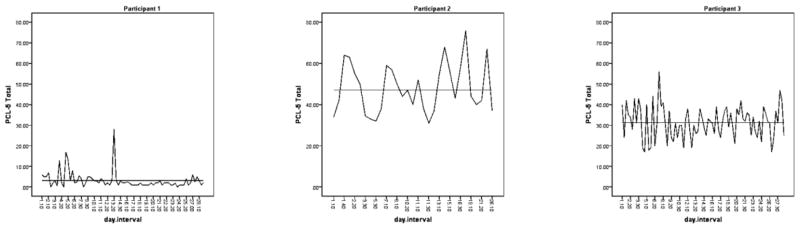
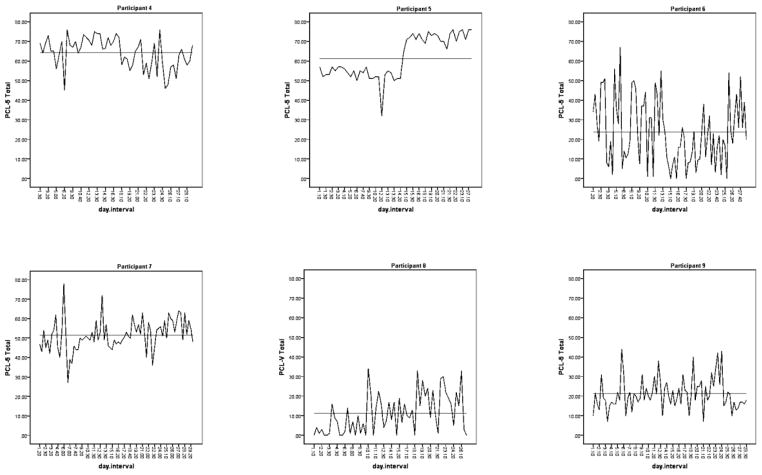
Participants’ PTSD symptom severity varied across intervals by 28 or more points on the 80-point scale (M = 38.8, SD=9.6; Mean within-person SD = 8.77, SD Range=4.00 – 15.20) (Figure 1). PCL-5 score range was unrelated to mean symptom severity (r=.17; p=.67) and number of surveys completed (r=.18; p=.64). MSSD ranged from 28 to 411 (M=134, SD=115); symptom instability was unrelated to mean symptom severity (r=−.18, p=.63), and mean lag between adjacent intervals (r−.09, p=.82). Within-person mean PTSD symptom severity and level of instability remained consistent across weeks of the study (F=0.78, p=.44; F=0.88, p=.42, respectively), suggesting no systematic reactivity to daily assessment.
Figure 1.
Daily and mean PCL-5 sum score over 28-day EMA period.
Factors Associated with High-Risk Sexual Behavior
Among 7 participants who recorded at least two sexual risk events in 28 days (i.e., had an opportunity to demonstrate patterned behavior), PCL-5-rated negative affect and externalizing behaviors subscale scores were significantly higher in questionnaires preceding a recorded sexual risk event than in questionnaires preceding no recorded sexual risk event (negative affect Mean Difference = 0.55, p=.04; Mean d = 0.31; externalizing behaviors Mean Difference = 0.31, p=.04, Mean d=.20). No other PCL-5 subscale score, nor total score, differed significantly by high-risk sexual event occurrence.
PTSD symptom instability was positively related to having multiple sexual partners (MSSD mean difference = 139; p=.07; Mean d = 1.57), but was unrelated to number of risk events (r=−.03; p=.93)
Interview Responses
Eight participants (89%) completed interviews and one (11%) could not be contacted. Interviewed participants reported that survey items were acceptable, no items were intentionally skipped, and participants independently estimated survey completion to take 2 – 3 minutes. All used their cell phones for the majority of prompted surveys, and found the survey accessible and easy to navigate.
Two participants questioned the need for item redundancy; items inquiring about PTSD symptoms and negative affect were similar. Two participants reported more anxiety during the EMA period than preceding weeks as a result of answering daily questions about their PTSD symptoms.
Participants reported delaying the survey at inconvenient times, and occasionally forgetting to take the survey after a delay. One participant recommended using texts instead of calls to prompt survey completion.
Discussion
This study provides preliminary evidence for the feasibility of enrolling and retaining male Veterans in a 28-day EMA study assessing daily PTSD symptoms and high-risk sexual behavior. All Veterans completed surveys using their own smartphones and none reported difficulties accessing the survey. The option to defer surveys, and their brevity, contributed to survey acceptability.
Within-day survey completion rates were comparable to rates reported in similar EMA studies requiring multiple daily surveys for two or more weeks (Hensel, Fortenberry, Harezlak, & Craig, 2012; Holt, Litt, & Cooney, 2012; Possemato et al., 2012; Shrier, Shih, & Beardslee, 2005). Lower completion rates within the 2-hour window, especially in the final week of the 28-day period, suggested the need to support sustained prompt-contingent recording in order to avoid potential bias due to non-random sampling.
The range and patterns of variability in PTSD symptoms were not anticipated, and we believe have not been illustrated in this detail previously in Veterans. These results suggest there may be an additional dimension to the PTSD course, over and above level of symptom severity that may be of importance for clinical intervention. Contrary to previous studies (Gaher et al., 2014; Possemato et al., 2012), systematic change in PTSD symptoms over the course of the study was not observed.
The specific association of PTSD-related negative affect and externalizing behaviors with subsequent sexual risk-taking events may inform clinical interventions that target symptom patterns at critical moments in time. Two interpretations of the association between PTSD symptom instability and multiple sexual partners are proposed: either that unstable symptoms predispose Veterans to this sexual risk, or that symptom instability is associated with another factor (e.g., impulsivity) that is associated with having multiple sexual partners.
Feasibility data and feedback from in-person interviews informed adaptations to a pilot EMA study with 45 Veterans, currently underway. Adaptations include using text-message prompts with an imbedded survey link, reducing the time window to 15 minutes for differential survey payment, and explicitly informing participants about the potential for increased anxiety during participation. Overall, the data suggested the promise of an EMA approach to understanding temporal relationships in that the 28-days of assessing participants with a recent history of sexual risk behavior was sufficient to record multiple high-risk sexual events, a range of symptom severities, and time-varying conditions around the time of sexual risk-taking.
These findings are tentative given the small sample size and potential spuriousness of multiple-comparison results, and additional studies with larger samples of OEF/OIF/OND Veterans will be useful to further evaluate the utility of the EMA approach in elucidating potentially complex sequences of PTSD symptoms and sexual risk behaviors in this population.
Highlights.
Veterans had 90.5% median completion of daily surveys of PTSD and sexual behavior
Veterans reported accessibility and acceptability of daily web-based assessments
PTSD symptoms varied substantially within person over 28 days
PTSD-related negative affect and externalizing behaviors preceded sexual risk-taking
PTSD symptom instability was associated with having concurrent sexual partners
Acknowledgments
This study was funded by the VA VISN-1 Pain Research, Informatics, Multi-morbidities, and Education (PRIME) Center; LIPS #96-008
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Anne C. Black, Email: anne.black@yale.edu, VA Connecticut Healthcare System, 950 Campbell Avenue 116A-4, West Haven, CT 06516; Phone: 203-932-5711 x2575; Fax: 203-479-8119.
Ned L. Cooney, Email: ned.cooney@va.gov, VA Connecticut Healthcare System, 555 Willard Avenue, 116A-3; Newington, CT 06111, Phone: 860-594-6339.
Amy C. Justice, Email: amy.justice2@va.gov, VA Connecticut Healthcare System, 950 Campbell Avenue, West Haven, CT 06516; Phone: 203-932-5711 x 3541.
Lynn E. Fiellin, Email: lynn.fiellin@yale.edu, Yale School of Medicine; 367 Cedar St, New Haven, CT 06510-3222; Phone: (203) 737-3347.
Robert H. Pietrzak, Email: robert.pietrzak@yale.edu, VA Connecticut Healthcare System; 950 Campbell Avenue 151E; West Haven, CT 06516; Phone: 860-638-7467.
Christina M. Lazar, Email: christina.lazar@yale.edu, VA Connecticut Healthcare System, 950 Campbell Avenue 116A-4, West Haven, CT 06516; Phone: 203-932-5711 x4833.
Marc I. Rosen, Email: marc.rosen@yale.edu, VA Connecticut Healthcare System, 950 Campbell Avenue 116A-4, West Haven, CT 06516; Phone: 203-932-5711 x2112.
References
- Adler Amy B, Britt Thomas W, Castro Carl Andrew, McGurk Dennis, Bliese Paul D. Effect of transition home from combat on risk-taking and health-related behaviors. Journal of Traumatic Stress. 2011;24(4):381–389. doi: 10.1002/jts.20665. [DOI] [PubMed] [Google Scholar]
- Armour Cherie, Tsai Jack, Durham Tory A, Charak Ruby, Biehn Tracey L, Elhai Jon D, Pietrzak Robert H. Dimensional structure of DSM-5 posttraumatic stress symptoms: support for a hybrid Anhedonia and Externalizing Behaviors model. Journal of psychiatric research. 2014 doi: 10.1016/j.jpsychires.2014.10.012. [DOI] [PubMed] [Google Scholar]
- Boscarino Joseph A. Posttraumatic stress disorder and mortality among US Army veterans 30 years after military service. Annals of epidemiology. 2006;16(4):248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Drescher Kent D, Rosen Craig S, Burling Thomas A, Foy David W. Causes of death among male veterans who received residential treatment for PTSD. Journal of Traumatic Stress. 2003;16(6):535–543. doi: 10.1023/B:JOTS.0000004076.62793.79. [DOI] [PubMed] [Google Scholar]
- Dursa Erin K, Reinhard Matthew J, Barth Shannon K, Schneiderman Aaron I. Prevalence of a Positive Screen for PTSD Among OEF/OIF and OEF/OIF-Era Veterans in a Large Population-Based Cohort. Journal of traumatic stress. 2014;27(5):542–549. doi: 10.1002/jts.21956. [DOI] [PubMed] [Google Scholar]
- Gaher Raluca M, Simons Jeffrey S, Hahn Austin M, Hofman Nicole L, Hansen Jamie, Buchkoski Jerome. An experience sampling study of PTSD and alcohol-related problems. Psychology of addictive behaviors. 2014;28(4):1013. doi: 10.1037/a0037257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulet Joseph. High STI rates among returning veterans, but low rates of HIV testing. Paper presented at the 141st APHA Annual Meeting; November 2–November 6, 2013.2013. [Google Scholar]
- Harris Paul A, Taylor Robert, Thielke Robert, Payne Jonathon, Gonzalez Nathaniel, Conde Jose G. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensel Devon, Fortenberry James, Harezlak Jaroslaw, Craig Dorothy. The feasibility of cell phone based electronic diaries for STI/HIV research. BMC Medical Research Methodology. 2012;12(1):75. doi: 10.1186/1471-2288-12-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt LJ, Litt MD, Cooney NL. Prospective analysis of early lapse to drinking and smoking among individuals in concurrent alcohol and tobacco treatment. Psychol Addict Behav. 2012;26(3):561–572. doi: 10.1037/a0026039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson Isabel G, Ryan Margaret AK, Hooper Tomoko I, Smith Tyler C, Amoroso Paul J, Boyko Edward J, Bell Nicole S. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA: the journal of the American Medical Association. 2008;300(6):663–675. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahng Seungmin, Wood Phillip K, Trull Timothy J. Analysis of affective instability in ecological momentary assessment: Indices using successive difference and group comparison via multilevel modeling. Psychological methods. 2008;13(4):354. doi: 10.1037/a0014173. [DOI] [PubMed] [Google Scholar]
- Kuhn Eric, Drescher Kent, Ruzek Josef, Rosen Craig. Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. Journal of Traumatic Stress. 2010;23(3):399–402. doi: 10.1002/jts.20536. [DOI] [PubMed] [Google Scholar]
- Meyers David, Wolff Tracy, Gregory Kimberly, Marion Lucy, Moyer Virginia, Nelson Heidi, Sawaya George F. USPSTF recommendations for STI screening. American family physician. 2008;77(6):819–824. [PubMed] [Google Scholar]
- NIAAA. Newsletter. 2004;(3):4. [Google Scholar]
- Owens DK, Sundaram V, Lazzeroni LC, Douglass LR, Sanders GD, Taylor K, Holodniy M. Prevalence of HIV infection among inpatients and outpatients in Department of Veterans Affairs health care systems: implications for screening programs for HIV. Am J Public Health. 2007;97(12):2173–2178. doi: 10.2105/ajph.2007.110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Possemato Kyle, Kaier Emily, Wade Michael, Lantinga Larry J, Maisto Stephen A, Ouimette Paige. Assessing daily fluctuations in posttraumatic stress disorder symptoms and substance use with interactive voice response technology: Protocol compliance and reactions. Psychological services. 2012;9(2):185. doi: 10.1037/a0027144. [DOI] [PubMed] [Google Scholar]
- Shiffman Saul, Stone Arthur A, Hufford Michael R. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Shrier Lydia A, Shih Mei-Chiung, Beardslee William R. Affect and sexual behavior in adolescents: a review of the literature and comparison of momentary sampling with diary and retrospective self-report methods of measurement. Pediatrics. 2005;115(5):e573–e581. doi: 10.1542/peds.2004-2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone Arthur A, Shiffman Saul. Ecological momentary assessment (EMA) in behavorial medicine. Annals of Behavioral Medicine 1994 [Google Scholar]
- Strom Thad Q, Leskela Jennie, James Lisa M, Thuras Paul D, Voller Emily, Weigel Rebecca, Holz Kenna Bolton. An exploratory examination of risk-taking behavior and PTSD symptom severity in a veteran sample. Military medicine. 2012;177(4):390–396. doi: 10.7205/milmed-d-11-00133. [DOI] [PubMed] [Google Scholar]
- Valdiserri Ronald O, Rodriguez Fred, Holodniy Mark. Frequency of HIV screening in the Veterans Health Administration: Implications for early diagnosis of HIV infection. AIDS Education & Prevention. 2008;20(3):258–264. doi: 10.1521/aeap.2008.20.3.258. [DOI] [PubMed] [Google Scholar]
- Weathers Frank W, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) 2013 http://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp.
- Westermeyer Joseph, Shiroma Paulo, Thuras Paul, Kattar Karen, Johnson David, Crosby Ross D. Daily versus monthly reporting of post-traumatic symptoms: a study of reliability across time and instruments. Psychiatry research. 2015;227(2):309–312. doi: 10.1016/j.psychres.2015.03.017. [DOI] [PubMed] [Google Scholar]