Abstract
Background
Electrosurgery is a modality that is widely used in surgery, whose use has resulted in injuries, OR fires and even death. The SAGES has established the FUSE program to address the knowledge gap in the proper and safe usage of electrosurgical devices. Complementing it, we have developed the Virtual Electrosurgery Skill Trainer (VEST©), which is designed to train subjects in both cognitive and motor skills necessary to safely operate electrosurgical devices. The objective of this study is to asses the face validity of the VEST© simulator.
Methods
Sixty-three subjects were recruited at the 2014 SAGES Learning Center. They all completed the monopolar electrosurgery module on the VEST© simulator. At the end of the study, subjects assessed the face validity with questions that were scored on a 5-point Likert scale.
Results
The subjects were divided into two groups; FUSE experience (n = 15) and no FUSE experience (n = 48). The median score for both the groups was 4 or higher on all questions and 5 on questions on effectiveness of VEST© in aiding learning electrosurgery fundamentals. Questions on using the simulator in their own skills lab and recommending it to their peers also scored at 5. Mann-Whitney U test showed no significant difference (p > 0.05) indicating a general agreement. 46 % of the respondents preferred VEST compared to 52 % who preferred animal model and 2 % preferred both for training in electrosurgery.
Conclusion
This study demonstrated the face validity of the VEST © simulator. High scores showed that the simulator was visually realistic and reproduced lifelike tissue effects and the features were adequate enough to provide high realism. The self-learning instructional material was also found to be very useful in learning the fundamentals of electrosurgery. Adding more modules would increase the applicability of the VEST© simulator.
Keywords: Electrosurgery, FUSE, 3D virtual reality (VR), Virtual Electrosurgery Skill Trainer (VEST), force feedback
INTRODUCTION
Electrosurgery is the application of radio frequency (RF) energy through the tissue to generate heat to achieve hemostasis, tissue dissection and ablation. Electrosurgery has been a popular modality in surgery ever since Harvey Cushing and Willian Bovie introduced it in the early 20th century [1]. As minimally invasive surgery (MIS) has become popular in the last two decades, energy based devices that includes electrosurgery have been widely used in nearly all (MIS) procedures. The incidence of injury in laparoscopic surgery is between 1 to 2 cases per 1000 operations with monopolar electrosurgery being the main cause [2]. Nearly 70% electrosurgical injuries are not noticed at the time of surgery because they can occur outside of the laparoscopic viewing area [3]. Using energy-based devices has lead to complications and even death [4], [5]. Surgical fires are also a major concern with the use of energy devices in the operating room. There are about 550 – 650 reported cases of OR fires in USA and it has been listed as the third in the 2009 edition of ECRI’s Health Devices guide’s top 10 technology hazards [6]. Of the reported cases, electrosurgical equipment is the source for 68% of the cases. [7].
In a recently conducted survey based study has found that even experienced surgeons lack in knowledge on the usage and complications of energy based devices [8]. Though there is an established program for training in both cognitive and motor skills for laparoscopic and endoscopic surgery [9], [10], none exist for the usage of energy based devices. Realizing the importance in reducing this knowledge gap, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) has developed the Fundamental use of Surgical Energy (FUSE) program (http://www.Fuseprogram.org) with educational material and validated assessment [11]–[13].
In this work we present the face validation of the Virtual Electrosurgery Skill Trainer (VEST©) that we are developing as part of the NIH funded R01 project. The VEST© is designed to train surgeons in both motor and cognitive skills required to safely operate electrosurgical tools in both open and minimally invasive procedures. A robust VEST© interactive learning modules could eventually compliment the FUSE curriculum.
Methods
The VEST© simulator consists of a 3D interactive display along with a tissue pad to provide force feedback and an interactive simulation that simulated the physics of electrosurgery interactions and effects such as smoke and electrical spark.
Interface
The VEST© interface shown in (Figure 1) consists of a high-quality stereoscopic 3D LCD display with integrated infrared cameras for accurate and low-latency head tracking (Zspace from Zspace Inc.). A retro reflective marker attached to the polarized stereo glass that user wears to see in 3D is used to track the head motion. The head tracking allows for dynamic updates to the displayed image to correspond to the user’s eye position, providing an enhanced 3D effect due to parallax. The VEST© simulator also supports traditional 2D display for rendering electrosurgery simulations for laparoscopic surgery. The user interacts with a specialized stylus with integrated infrared LED that tracks their motion. The programmable button on the stylus activates the electrosurgery in the VEST© simulator.
Figure 1.
The VEST interface with 3D stereoscopic display, tissue pad and iPad ESU interface
A height adjustable tissue pad made from a 3D printed platform and filled with artificial tissue is used for providing the sensation of contact with tissues while interacting with the simulator. The tissue pad is placed in front of the 3D LCD display and the simulation is synchronized such that both the physical stylus and the virtual tool that the stylus controls in the simulation makes simultaneous contact on the physical and virtual tissues.
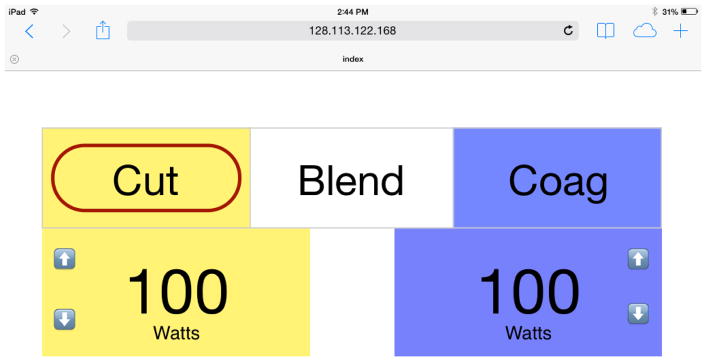
Another important aspect in training on the principles of electrosurgery is the ability to learn the tissue effects for various power settings and modes of operations such as cutting, coagulation and blend. In the VEST© simulator, an Ipad mini (Apple Inc.) is used as a virtual electrosurgery unit (ESU). The virtual ESU is designed as a generic interface with main functionalities displayed on a webpage designed using HTML5 and javascript whose screen capture shown in Figure 2. The user can select between the cutting, coagulation and blend modes and can also change the power using the up and down arrows. Both the virtual tissue simulation and the ESU server were run on the same computer and a local wireless network was used to connect the iPad mini to the server.
Figure 2.
The screen capture from the iPad ESU interface
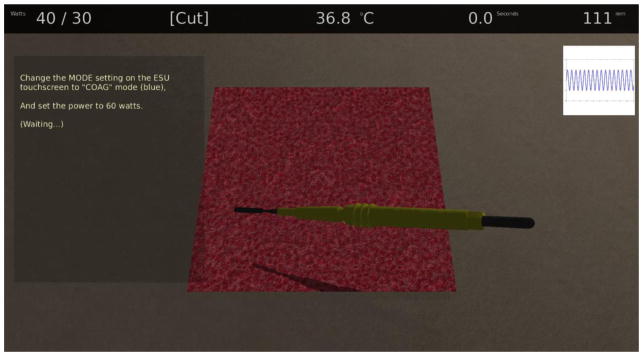
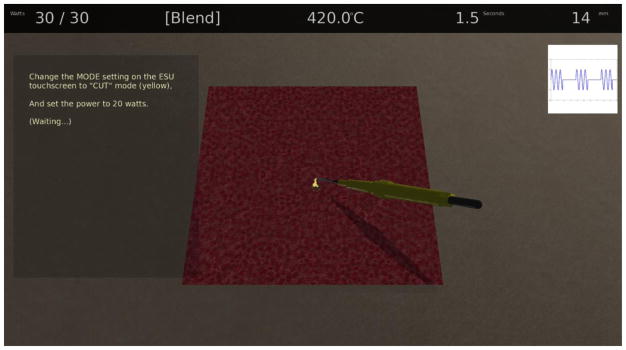
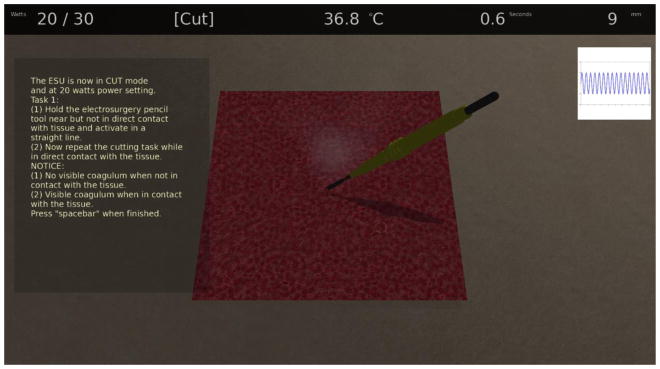
Figure 3 shows the actual screen that is displayed on the 3D display (double buffered rendering switched off for illustration purpose but user will see in 3D with polarized glasses).
Figure 3.
VEST simulator display showing various features
As the VEST© simulator was designed to provide both motor and cognitive skills training, the display was optimized to provide maximum information and self-learning interactive didactic information to the user. At the top of the display, a horizontal bar provided information on the current power settings in watts for both cutting and coagulation modes, the current chosen mode of operation, current tissue temperature at the operating point, duration of contact with the tissue and the distance of the tool tip from the tissue surface. A waveform displayed on the top right side of the screen reflects the selected mode of operation. At the center of the screen, the virtual tissue was displayed on which the user can interact with the virtual tool. Currently three different tools, electrosurgery pencil with blunt and small tip as well as a L-Hook can be used in the VEST© simulator. On the left of the tissue model on a transparent pane the instructional and didactic materials are displayed. The content of those panes change in real-time based on the user’s interaction. For example in Figure 3, the pane is displaying the instruction to change the ESU mode to coagulation and change the power to 60 Watts.
Electrosurgery Interaction Simulation
In order to implement the monopolar electrosurgery interactions that include cutting, coagulation and fulguration, we have modeled the monopolar electrosurgery procedure. Our model consists of a surface mesh that represented liver tissue on which two-dimensional heat accumulation and heat diffusion was calculated at each time step when interacted with an electrosurgery pencil with either a flat or small tip electrode. The heat accumulation and heat diffusion of tissue can be calculated by equation (1) according to power and pencil-tip’s spatial position.
| (1) |
Where ΔQ is heat change, P is power applied tissue, D is duty cycle, r is the radius of contact, Δt is the time step, ΔQd is heat diffusion, d is the non-contact distance between pencil tip and tissue. With the heat change, the temperature change ΔT of each point or voxel can be calculated
| (2) |
Where c the specific heat capacity of tissue, ρ is the tissue density, ΔV is the volume of each voxel. Combining equation (1) and (2), the temperature of each point can be obtained. The accumulated temperature along with the modes of the operation (cutting, coagulation or blend) is used to decide what should happen to the virtual tissue in the VEST© simulator.
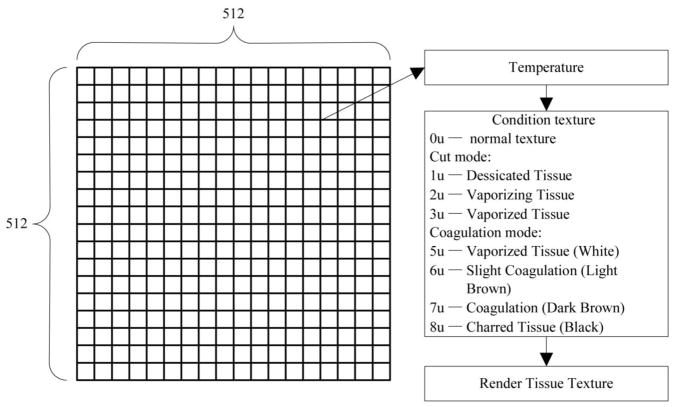
The tissue effects are rendered in real-time using the shader language that ran on the GPU(graphical processor interface). In order to perform this operation a condition texture with the same size as the virtual tissue is used for showing temperature effects. Figure 3 shows the condition texture whose size was 512 × 512 in our current simulation. In total there were 8 different conditions that were used to manipulate the texture and the temperature threshold based on the current mode of operation was decided based on the values shown in Table 1. In our current simulation only the cutting and coagulation modes were used. Besides the condition texture map, the cutting depth of tissue based on the power is also calculated and transferred to the shader program for rendering.
Table 1.
Temperature threshold and tissue effects used for simulation in the VEST simulator
| Cutting Mode | Coagulation Mode | ||
|---|---|---|---|
| Temperature (°C) | Tissue Effects | Temperature (°C) | Tissue Effects |
| < 60 | Normal tissue | < 80 | Normal tissue |
| 60 | Vaporizing tissue | 80 | Vaporized tissue (white) |
| 80 | Vaporized tissue (cutting tissue) | 100 | Slight coagulation (light brown) |
| 100 | Desiccated tissue | 150 | Coagulation (dark brown) |
| 200 | Charred tissue (black) | ||
Simulation of spark and smoke effects
If the electrosurgical tool is activated while not in direct contact with the tissue, the resulting electrical field can induce a breakdown of the intervening air-gap, resulting in visible arcing. Such arcs provide useful visual feedback to the surgeon of both the flow of current and the proximity of the electrosurgical tool relative to the tissue. To simulate electrical discharge, a Lindenmayer system (L-system) grammar for representing the three-dimensional electrical breakdown geometry was developed [14]. The breakdown geometry was embedded within a three-dimensional Eulerian representation of the state of the air, storing the ion and particulate densities and the air temperature, for the region between the electrosurgical instrument and the tissue. The Eulerian representation of the air-gap was evolved using semi-Lagrangian advection and diffusion, with buoyancy effects due to temperature differences between regions of air. This approach provided a realistic model of time-evolving electrical arcs with substantially less computation time. Figure 5 shows the spark effect as rendered in the VEST© simulator.
Figure 5.
Sparking effect in the VEST simulator
Smoke is generated when tissue is burned through dissection or fulguration. We used particle system with fluid dynamics to simulate the growth and dissipation of the smoke. Ray casting was then used to display the 3D sliced volumetric smoke texture (air-borne particulate density) [15]. Figure 6 shows a screen shot with smoke generated while interacting with the virtual tissue.
Figure 6.
Smoke effect in the VEST simulator
Experiment Design
The face validation of the VEST© was an opportunistic study with as many subjects as possible was recruited to rate the features of the simulator. A 5-point Likert Scale [16] questionnaire with response choices depending on the questions such as “1 - don’t agree ” to “5 - Agree”, “1 - not realistic” to “5 - very realistic and “1 - not useful” to “5 - very useful” was used to gauge the response from the subjects. The questionnaire consisted of questions related to the utility and the realism of tasks VEST© simulator. The simulator was pilot tested and the questionnaire were finalized by authors DBJ, SDS, JO, AM and HW prior to the study. Institutional Review Board (IRB) approval was then obtained to perform this study at the Learning Center of the 2014 Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) meeting held in April at the Salt Lake City, UT.
Participants
This was an opportunistic study and as many subjects as possible with varying surgical experience were recruited at the Learning Center. To encourage subject enrollment, two iPad mini’s were presented to two lucky participants selected using a raffle at the conclusion of the study on the last day of the conference.
Task and Procedure
After obtaining verbal consent for the study, subjects were asked to fill out a questionnaire detailing the demographics and their previous laparoscopic surgery and laparoscopic simulators experience and exposure to FUSE materials and whether they have taken the FUSE course and passed the exam. After this the subjects were given an overview of all the features of the VEST© simulator. The position of the iPad was changed to either left or the right side of the subject based on the dominant hand the subject was going to use to perform the study. Once the subjects were familiar with the simulator they were then asked to go through the monopolar electrosurgery module that includes cutting and coagulation (See appendix 1 for details of the monopolar electrosurgery module). At the end of the session, the subjects completed the 5-point Likert scale face validation feedback questionnaire.
RESULTS
Demographics
There were a total of 63 subjects participated in this study (50 Males and 13 Females). The surgical experience ranged from medical student to attending (Medical student = 5, PGY1 = 3, PGY2 = 4, PGY3 = 6, PGY4 = 7, PGY5 = 5, Fellow = 4 and Attending = 29). Of the 63 subjects, 15 subjects had read the SAGES FUSE manual and 6 subjects had taken the FUSE exam. When asked questions related to electrosurgery experience, 59 subjects stated that they have used electrosurgery equipment and 52 of them have adjusted the electrosurgery settings in an operating room at least once. Based on the demographics, the subjects were classified in to two groups, Group 1 (n = 48, no FUSE experience) and Group 2 ( n = 15, read FUSE manual or taken FUSE exam).
Face Validation
The subject’s response to face validation questions on a 5-point Likert scales were grouped and the median and mode (most frequent response) were computed. The responses were then compared using Mann-Whitney U test.
For questions related to the effectiveness of VEST in aiding learning electrosurgery fundamentals (Table 2), subjects from both groups rated all the questions very highly (median sores greater than 4). Specifically, subject’s median scores for both the groups were 5 for questions on VEST more effective than learning from textbooks, it is more enjoyable than learning from books, would use it in the skills lab if available and would also recommend to others who are interested in learning the fundamentals of electrosurgery. For questions related to better understanding of electrosurgical principles and changing practices after using VEST, the median scores were 4 for both the groups. Mann-Whitney U test showed that there was no significant difference between the responses between the two groups (p > 0.05) indicating a general consensus.
Table 2.
Face validation results for the utility of the VEST simulator
| Questionnaire | Group 1 | Group 2 | Mann Whitney U Test p values | ||
|---|---|---|---|---|---|
| Median Score | Most Frequent Response (Mode) | Median Score | Most Frequent Response (Mode) | ||
| 1. I feel I have a better understanding of electrosurgical principles after using the VEST simulator | 4 | 5 | 4 | 4 | 0.076 |
| 2. I feel learning electrosurgical principles with the VEST simulator is more effective than just textbooks alone | 5 | 5 | 5 | 5 | 0.754 |
| 3. Using the VEST simulator to learn electrosurgical principles is more enjoyable than just using textbooks | 5 | 5 | 5 | 5 | 0.785 |
| 4. If the VEST simulator was available to me in my skills lab, I would use it | 5 | 5 | 5 | 5 | 0.754 |
| 5. I would recommend the VEST simulator to others who are interested in learning electrosurgical principles and practicing techniques | 5 | 5 | 5 | 5 | 0.65 |
| 6. After using the VEST simulator, I will change my practices in the OR | 4 | 5 | 4 | 4 | 0.526 |
Table 3 shows the median and mode of the ratings for questions related to the characteristics of the VEST simulator. The median ratings were 4 for both the groups for questions on realism of tissue effects, instrument handling, force feedback, usefulness of force feedback and usefulness of VEST in learning hand eye coordination. Mann-Whitney U test showed that there was no significant difference between the responses between the two groups (p > 0.05) indicating a general consensus.
Table 3.
Face validation results for the realism of tasks and features in the VEST simulator
| Questionnaire | Group 1 | Group 2 | Mann | ||
|---|---|---|---|---|---|
| Median Score | Most Frequent Response (Mode) | Median Score | Most Frequent Response (Mode) | Whitney U Test p values | |
| 1. Compared to actual surgery, tissue effects in the simulator are | 4 | 4 | 4 | 4 | 0.767 |
| 2. Compared to actual surgery, the instrument handling on the simulator is | 4 | 4 | 4 | 4 | 0.391 |
| 3. Please rate the degree of overall realism of the VEST simulation (how it looks AND feels), compared to the corresponding surgical task | 4 | 4 | 4 | 4 | 0.389 |
| 4. Please rate the quality of the force feedback (sensation of feeling the tools on the target and in the task space) in the VEST simulator compared to actual surgery | 4 | 4 | 4 | 4 | 0.822 |
| 5. Please rate the degree of usefulness of the force feedback (sensation of feeling the tools on the target and in the task space) in the VEST simulator in helping your performance | 4 | 4 | 4 | 4 | 0.957 |
| 6. Please rate the usefulness of the VEST simulator in learning hand-eye coordination skills, compared to an animal model. If you have never used an animal model for skills training, please circle “Don’t know”. | 4 | 4 | 4 | 3 | 0.709 |
| 7. Please rate the degree of overall usefulness of the VEST simulator in learning electrosurgical techniques and principles compared to an animal model | 4 | 4 | 4 | 4 | 0.431 |
For the question on whether they would prefer the VEST or the animal model for electrosurgical skill training, a total of 55 participants responded of which 29 subjects (52%) preferred the animal model, 26 subjects (46%) preferred the VEST simulator and 1 subject (2 %) preferred both.
DISCUSSION
Electrosurgery is the process in which high frequency electric current (300 – 500 KHz) is passed through the tissue to generate heat to coagulate, desiccate, vaporize or fulgurate tissues. In monopolar electrosurgery device is used, the electrical energy is passed out through an active electrode, through the tissue and in to dispersive electrode placed on the body, which returns the current to the ESU and closes the circuit. In bipolar electrosurgery both active and return electrodes are located in the same tool and only a small area of tissue, which are being manipulated, closes the circuit by conducting the electricity. In order to properly and safely use electrosurgery in surgery, one has to thoroughly understand the effects of passing high frequency current on tissues, selecting different modes of operations (cutting, coagulation and blend) and different power settings. Moreover the position and orientation of the tools tip and its proximity to tissue also has significant effect due to variations in current density at the tool tip. For proper use of electrosurgery requires motor, cognitive and decision-making skills. Ideally there should be a simulator than can train surgeons and other operating room personnel in all of these three aspects.
The purpose for the simulation is to increase patient safety through injury avoidance. Monopolar electrosurgery is shown to have higher and larger temperature and thermal spread [17]. The monopolar electrosurgery has also lead to post operative complications even in common procedure like laparoscopic cholecystectomy [18], [19]. The use of monopolar electrosurgery has even lead to death [4], [5]. Further details on complications from using monopolar and bipolar electrosurgery and other energy sources in surgery can be found here [20].
The lack of content knowledge in usage and complications of energy based devices even for experts with several years of surgical experience was apparent in the study conducted by Feldman et al. [8]. In this study, a pre questionnaire that consisted of 11 questions chosen from a total of 79 questions that were prepared by domain matter experts covering eleven sections of the FUSE pilot postgraduate curriculum and was administered to the SAGES leadership who were attending the FUSE and Quality, Outcome and Safety (QOS) committee meetings and the board of directors. Of the 48 expert subjects, the median percentage of correct answers was 59 % with subjects answering poorly on knowledge of electrosurgery nomenclature and settings, handling operating room fire and recognizing thermal injury. The VEST simulator with self-learning didactic modules presented in this work is designed to address this knowledge gap.
As a first step in developing the VEST simulator, an online survey with FUSE committee members as subjects was conducted on seven representative tasks namely, dissection, fulguration, bipolar coaptative coagulation, traction and bipolar dissection, traction and monopolar dissection, monopolar coaptative coagulation and inspection [21]. The survey assessed each of the seven tasks on seven different aspects that include face, content, construct and predictive validity, motor skills and privileging. The results from the survey showed that all of the tasks are important and indicative of important technical skills with bimanual tasks showing highest agreement and the inspection task the least. Based on the survey the tasks for the VEST simulator was chosen as the first two tasks of monopolar dissection and fulguration. Further didactic modules with instructions were added to make it interactive and self learning.
Madani et al. [22], showed the effectiveness of a goal-directed bench-top training for enhancing the learning of the principles of the FUSE curriculum. In their randomized controlled study, both the control group who had access to wet lab, electrosurgery equipment and steak tissue and the intervention group who underwent a goal-directed training with bench-top models that was specifically selected to compliment the didactic components showed significant improvement after training with the intervention group showing significant retention of the concepts after three months compared to the control group. The study showed that hands-on components are very useful tool in learning and retaining fundamentals of the electrosurgery primarily helping in retaining the knowledge as described in the “pyramid of learning” by Dale et al. [23], [24]. Using frozen steak tissues for learning tissue effects are not ideal since ex-vivo tissues doesn’t retain the same properties of in-vivo tissues that has blood supply and maintained at body temperature. Performing electrosurgery on a ex-vivo tissue would generate lot of smoke and will be very uncomfortable for the trainees and also has potential health hazard, Moreover, a trained supervisor is needed to conduct a training with physical model. On the contrary, VEST simulator uses physics based simulation that can reproduce tissue effects that one would see in real tissue. Also virtual smoke generated creates enhanced realism without any adverse health effect. The didactic module in VEST is designed to be self-learning and doesn’t need any supervision.
The face validation results in our study showed that the subjects with varying experience rated very high (median scores 4 or 5) on both the ability of VEST simulator in learning electrosurgery skills and also on the quality of the simulation in the current version of the simulator. Subjects also gave feedback on the improvements to simulator including adding separate button for cutting and coagulation operations, adding blend modes, improving the depth perception and adding three dimensional models such as gall bladder and liver as opposed to two dimensional tissue surface model. We will add these improvements in the next version of the VEST simulator.
CONCLUSION
Face validity for the cut and coag modules of the VEST simulator was established. The simulator was found to be visually realistic and reproduced lifelike tissue effects as rated by the study subjects. The self-learning instructional material was also found to be useful in learning the fundamentals of electrosurgery. The next step includes comparing the VEST simulator with the didactic lecture to a group that has only the lecture and a group that has had the lecture and physical simulator module. Moreover, we plan to add several modules to the VEST simulator, such as bipolar electrosurgery, direct and capacitive coupling, and insulation failures. Future studies have been planned to validate these modules.
Figure 4.
Condition texture used in the VEST simulator
Acknowledgments
Funding information: This work was supported by NIH/NIBIB 2R01EB005807, 5R01EB010037, 1R01EB009362, 1R01EB014305.
This project was supported by National Institutes of Health (NIH) Grant NIH/NIBIB 2R01EB005807, 5R01EB010037, 1R01EB009362, 1R01EB014305.
We thank Mr. Adam Ryason, graduate student at the Center for Modeling, Simulation and Imaging in Medicine (CeMSIM) for 3D printing and assembling the tissue pad.
Appendix
Monopolar Electrosurgery Learning Objective
1. Learning Objectives
Difference in waveforms between cutting and coagulation settings
Different power settings and its effect on both cutting and coagulation
2. Cutting Mode
Cutting mode is a continuous, relatively low-voltage waveform (Wave form shown on the side of the screen). An incision is made by a process known as linear vaporization. Vaporization occurs when the cellular temperature is between 100 – 200 degrees Celsius. As the cell burst, or vaporize a steam pocket is made which results in an incision without significant tissue effect to the surrounding tissues. This is done when the electrosurgical instrument is held very close to, but not in direct contact to the target tissue.
In contrast, if the instrument is held in contact with the tissue, the current density decreases, resulting in less tissue effect. At temperature 60–95 the cellular protein bonds break and the tissue undergoes coagulation.
Task 1a: Set the electrosurgical pencil to Pure “cutting” on 20 Watts. Hold it near but not in direct contact with tissues and activate in a straight line.
Task 1b: Now repeat the task while in direct contact with the tissue and activate it in a straight line.
Notice:
No visible coagulum when not in contact with the tissue
Visible coagulum when in contact with the tissue
Task 2a: Set the electrosurgical pencil to Pure “cutting” on 40 Watts. Hold it near but not in direct contact with tissues and activate in a straight line.
Task 2b: Now repeat the task while in direct contact with the tissue and activate it in a straight line.
Notice:
No visible coagulum and larger incision compared to the power setting of 20 watts when not in contact with the tissue.
Formation of black coagulum and no incision when in contact with the tissue.
3. Coagulation Mode
“Coagulation” mode is an interrupted, high voltage wave form (Wave form shown on the side of the screen). Compared to “cutting” there is an uneven and unpredictable coagulation pattern. The more superficial layers of the tissue become rapidly coagulated, increasing impedance, thereby preventing further transmission of the energy to the deeper layers of the tissue. There is not reliable sealing of vessels When this is used without direct tissue contact, with high voltage, very high temperatures are reached, resulting in fulguration, which is useful for superficial coagulation of small capillaries and raw surfaces, such as the gallbladder fossa of the liver.
Task 3a: Set the electrosurgical pencil to Pure “coagulation” on 60. Hold it in contact with the tissue and activate it in a painting like manner across the tissue.
Task 3b: Now repeat the task but hold it near and do not make contact with the tissue.
Notice:
When in contact, formation of black coagulum which flakes off when contact is released.
When not in contact, formation of widespread black coagulum
Footnotes
NOTE: Accepted for poster presentation at the 2015 SAGES meeting
DISCLOSURE
Dr. Daniel B. Jones is the chair of the SAGES FUSE committee and consultant to Allurion and Intuitive Surgical. Dr. Schwaitzberg has served on advisory panels and has received an honorarium from Stryker and Olympus. He has served on advisory panels for Neatstitch and Surgicquest, Arch Therapeutics Acuity Bio and Human Extensions. He has also received a grant from Ethicon. Drs. Sankaranarayanan and De serve as members in the SAGES FUSE committee. Mr Li, Drs. Miller, Wakily, Jones and Olasky have no conflicts of interest or financial ties to disclose.
References
- 1.Cushing H, Bovie WT S. P. C. of Chicago, . Electro-surgery as an Aid to the Removal of Intracranial Tumors: With a Preliminary Note on a New Surgical Current Generator. Surgical Publishing Company; 1928. [Google Scholar]
- 2.Nduka CC, Super PA, Monson JR, Darzi AW. Cause and prevention of electrosurgical injuries in laparoscopy. J Am Coll Surg. 1994 Aug;179(2):161–170. [PubMed] [Google Scholar]
- 3.Lee J. Update on Electrosurgery. Outpatient Surgery. 2002 Feb 2;3 [Google Scholar]
- 4.Willson PD, McAnena OJ, Peters EE. A fatal complication of diathermy in laparoscopic surgery. Minim Invasive Ther Allied Technol. 1994 Jan;3(1):19–20. [Google Scholar]
- 5.Peterson HB, Ory HW, Greenspan JR, Tyler CW. Deaths associated with laparoscopic sterilization by unipolar electrocoagulating devices, 1978 and 1979. Am J Obstet Gynecol. 1981 Jan;139(2):141–143. doi: 10.1016/0002-9378(81)90435-x. [DOI] [PubMed] [Google Scholar]
- 6.ECRI Institute. 2010 top 10 technology hazards. Health Devices. 2009 Nov;38(11) [PubMed] [Google Scholar]
- 7.Hart SR, Yajnik A, Ashford J, Springer R, Harvey S. Operating Room Fire Safety. Ochsner J. 2011;11(1):37–42. [PMC free article] [PubMed] [Google Scholar]
- 8.Feldman LS, Fuchshuber P, Jones DB, Mischna J, Schwaitzberg SD FUSE (Fundamental Use of Surgical Energy™) Task Force. Surgeons don’t know what they don’t know about the safe use of energy in surgery. Surg Endosc. 2012 Oct;26(10):2735–2739. doi: 10.1007/s00464-012-2263-y. [DOI] [PubMed] [Google Scholar]
- 9.Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K SAGES FLS Committee. Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery. 2004 Jan;135(1):21–27. doi: 10.1016/s0039-6060(03)00156-9. [DOI] [PubMed] [Google Scholar]
- 10.Hazey JW, Marks JM, Mellinger JD, Trus TL, Chand B, Delaney CP, Dunkin BJ, Fanelli RD, Fried GM, Martinez JM, Pearl JP, Poulose BK, Sillin LF, Vassiliou MC, Melvin WS. Why fundamentals of endoscopic surgery (FES)? Surg Endosc. 2014 Mar;28(3):701–703. doi: 10.1007/s00464-013-3299-3. [DOI] [PubMed] [Google Scholar]
- 11.Feldman L, Fuchshuber P, Jones DB. The SAGES Manual on the Fundamental Use of Surgical Energy (FUSE) Springer Science & Business Media; 2012. [Google Scholar]
- 12.Madani A, Jones DB, Fuchshuber P, Robinson TN, Feldman LS. Fundamental Use of Surgical Energy™ (FUSE): a curriculum on surgical energy-based devices. Surg Endosc. 2014 Jun; doi: 10.1007/s00464-014-3623-6. [DOI] [PubMed] [Google Scholar]
- 13.Feldman LS, Brunt LM, Fuchshuber P, Jones DB, Jones SB, Mischna J, Munro MG, Rozner MA, Schwaitzberg SD SAGES FUSE™ Committee. Rationale for the fundamental use of surgical Energy™ (FUSE) curriculum assessment: focus on safety. Surg Endosc. 2013 Nov;27(11):4054–4059. doi: 10.1007/s00464-013-3059-4. [DOI] [PubMed] [Google Scholar]
- 14.Lindenmayer A. Mathematical models for cellular interactions in development. I. Filaments with one-sided inputs. J Theor Biol. 1968 Mar;18(3):280–299. doi: 10.1016/0022-5193(68)90079-9. [DOI] [PubMed] [Google Scholar]
- 15.Crane K, Llamas I, Tariq S. GPU Gems 3. 2. Addison-Wesley Professional; 2007. GPU Gems 3 - Chapter 30. Real-Time Simulation and Rendering of 3D Fluids. [Google Scholar]
- 16.Likert A technique for the measurement of attitudes. Arch Psychol. 1932;22(140):1–55. [Google Scholar]
- 17.Sutton PA, Awad S, Perkins AC, Lobo DN. Comparison of lateral thermal spread using monopolar and bipolar diathermy, the Harmonic Scalpel™ and the Ligasure™. Br J Surg. 2010;97(3):428–433. doi: 10.1002/bjs.6901. [DOI] [PubMed] [Google Scholar]
- 18.Polychronidis A, Tsaroucha AK, Karayiannakis AJ, Perente S, Efstathiou E, Simopoulos C. Delayed perforation of the large bowel due to thermal injury during laparoscopic cholecystectomy. J Int Med Res. 2005 Jun;33(3):360–363. doi: 10.1177/147323000503300312. [DOI] [PubMed] [Google Scholar]
- 19.Willson PD, van der Walt JD, Moxon D, Rogers J. Port site electrosurgical (diathermy) burns during surgical laparoscopy. Surg Endosc. 1997 Jun;11(6):653–654. doi: 10.1007/s004649900414. [DOI] [PubMed] [Google Scholar]
- 20.Sankaranarayanan G, Resapu RR, Jones DB, Schwaitzberg S, De S. Common uses and cited complications of energy in surgery. Surg Endosc. 2013 Sep;27(9):3056–3072. doi: 10.1007/s00464-013-2823-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Allen BF, Jones DB, Schwaitzberg SD, Suvranu D. Survey-based analysis of fundamental tasks for effective use of electrosurgical instruments. Surg Endosc. 2014 Apr;28(4):1166–1172. doi: 10.1007/s00464-013-3301-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Madani A, Watanabe Y, Vassiliou MC, Fuchshuber P, Jones DB, Schwaitzberg SD, Fried GM, Feldman LS. Impact of a hands-on component on learning in the Fundamental Use of Surgical Energy™ (FUSE) curriculum: a randomized-controlled trial in surgical trainees. Surg Endosc. 2014 May; doi: 10.1007/s00464-014-3544-4. [DOI] [PubMed] [Google Scholar]
- 23.Dale E. Audiovisual Methods in Teaching. 3. Jan, 1969. [Google Scholar]
- 24.Masters K. Edgar Dale’s Pyramid of Learning in medical education: a literature review. Med Teach. 2013 Nov;35(11):e1584–1593. doi: 10.3109/0142159X.2013.800636. [DOI] [PubMed] [Google Scholar]