Summary
Background
Leptin, an adipocyte-derived circulating cytokine that signals nutritional status, may play a role in the development of psoriasis and its associated systemic diseases. Patients with psoriasis have significantly decreased serum leptin levels compared with controls.
Aim
To investigate the effect of two commonly used anti-psoriatic biological drugs, adalimumab and ustekinumab, on leptin and leptin receptor expression in human macrophages.
Methods
THP-1 differentiated macrophages were cultured under the following conditions: (i) untreated control, (ii) adalimumab 5 μg/mL, (iii) ustekinumab 1 μg/mL, and (iv) ustekinumab 5 μg/mL Expression of leptin and leptin receptors were measured using real-time quantitative PCR and immunoblotting techniques.
Results
The presence of either adalimumab or ustekinumab in growth medium significantly upregulated expression of leptin receptor in THP-1 human macrophages to 1.98 ± 0.47 and 2.09 ± 0.24, respectively (n = 3, P < 0.01) versus 1.12 ± 0.19 for untreated control cells. However, only ustekinumab at a concentration of 5 μg/ml, augmented expression of leptin to 1.99 ± 0.56 (n = 3, P < 0.01) versus control untreated cells.
Conclusions
Enhanced leptin and leptin receptor expression in macrophages exposed to therapeutic levels of ustekinumab suggest a novel immunomodulatory mechanism for this biological drug. Further mechanistic studies may yield targeted treatment using the leptin pathway, which could reduce the common obesity-related complications of psoriasis while alleviating symptoms and improving prognosis.
Introduction
Psoriasis is a chronic inflammatory skin disease characterized by epidermal hyperproliferation and immunological disturbance.1 Recent studies support the role of interleukin (IL)-23, a heterodimeric cytokine of the IL-12 family, in the progression of psoriasis and other autoimmune diseases.2,3 IL-23 produced by human dendritic cells drives the differentiation and proliferation of T helper (Th)17 cells,4 which in turn produce a number of pro-inflammatory cytokines, including IL-17A, IL-17F and IL-22, which have been found to be more abundant in both lesional and nonlesional skin of patients with psoriasis.3
Bioactive adipocytokines, including leptin, adiponectin, resistin and visfatin, participate in maintaining energy balance and glucose homeostasis, and in modulating inflammatory responses. Recently, adipocytokines have been associated with progression of psoriasis, obesity, metabolic comorbidities and cardiovascular disease.5,6 Serum leptin levels may be useful biomarkers in monitoring therapeutic efficacy and risk of comorbidities such as atherosclerosis and metabolic syndrome. This study investigates the effect of two commonly used anti-psoriatic biological drugs, adalimumab [a tumour necrosis factor (TNF)-α inhibitor) and ustekinumab (an IL-12/23 inhibitor) on leptin and leptin receptor expression at the cellular level.
Methods
Experimental conditions
We assessed inhibition of IL-12/23 by ustekinumab, using adalimumab at therapeutic concentration for comparison. THP-1 adherent macrophages were incubated under the following conditions: (i) untreated control, (ii) adalimumab 5 μg/mL, (iii) ustekinumab 1 μg/mL, and (iv) ustekinumab 5 μg/mL. Total protein lysates and RNA were then isolated, as indicated in the supplementary methods online.
Gene expression analysis
Total RNA (1 μg) from each experimental condition was reverse-transcribed into cDNA. Equal amounts of cDNA were then taken for real-time quantitative PCR amplification using specific primers for leptin and the leptin receptor. The fold change in expression level of target gene relative to the GAPDH at various time points was calculated using the 2-ΔΔCT method. A melting-curve analysis was performed to assess specificity of the amplified PCR products.
Protein extraction and western blotting
Total cell lysates were prepared using RIPA lysis buffer, containing protease inhibitor cocktail (10 μL per 1000 μL of buffer) (for full details, see the supplementary methods section online). Protein samples (20 μg/lane) were fractionated in 10% sodium dodecyl sulfate-polyacrylamide gel electophoresis, and transferred onto a polyvinylidene fluoride membrane. Leptin primary antibody utilized at 1:1000 dilution in blocking solution. Glyceraldehyde 3-phosphate dehydrogenase was detected as a loading control. Band intensities for immunoblot protein samples were quantified using Kodak Digital Science 1D, version 2.0.3.
Statistical analysis
All data were analysed by one-way analysis of variance with Bonferroni correction, using Graphpad Prism (v5.01; GraphPad, San Diego, CA, USA),. P < 0.05 was considered significant.
Results
Adalimumab and ustekinumab increases leptin receptor expression
The presence of adalimumab significantly (P < 0.01) upregulated expression of the leptin receptor in THP-1 human macrophages to 1.98 ± 0.47 versus 1.12 ± 0.19 for untreated control cells (n = 3 in each group).
Ustekinumab increased expression of the leptin receptor in a concentration-dependent manner, reaching 2.09 ± 0.24 (P < 0.01; n = 3) at the 5 μg/mL concentration (Fig. 1).
Figure 1.
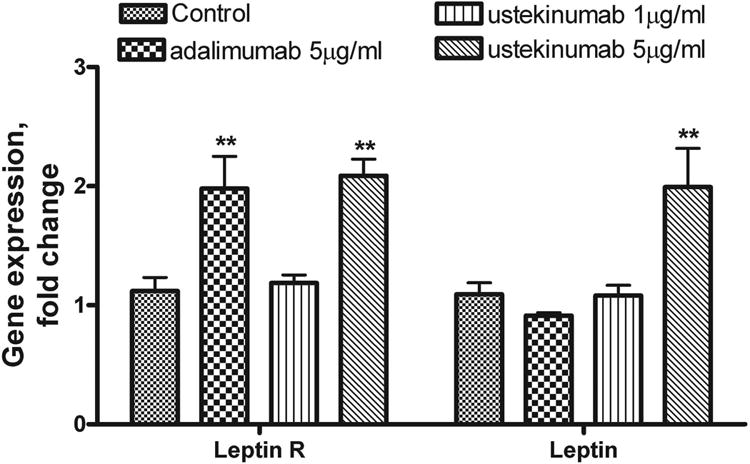
Gene expression of leptin and leptin receptor in THP-1 macrophages exposed to adalimumab and ustekinumab: THP-1 macrophages were incubated for 18 h under the following conditions: (a) untreated control, (b) adalimumab 5 μg/mL, (c) ustekinumab 1 μg/mL, (d) ustekinumab 5 μg/mLL. Quantitative analysis for changes in leptin and leptin receptor mRNA level was performed using RT-PCR with GAPDH message as an internal standard. All results are presented as means ± SEM of three independent experiments. **P < 0.01 vs. control.
Ustekinumab, but not adalimumab, increases leptin expression in THP-1 macrophages
Adalimumab 5 μg/mL and ustekinumab 1 μg/ml did not change the expression of leptin in THP-1 macrophages compared with control untreated macrophages. However, at a concentration of 5 μg/mL, ustekinumab increased leptin expression to 1.99 ± 0.56 (P < 0.01; n = 3) (Fig. 1).
Gene expression analysis was confirmed by Western blot. In all experiments, treated THP-1 macrophages were compared with untreated control macrophages. Protein expression by untreated control cells was set at 100%. Thus, only ustekinumab at a concentration of 5 μg/ml, augmented expression of leptin to 161.1 ± 18.7% versus control (P < 0.01; n = 3 in each group) (Fig. 2).
Figure 2.
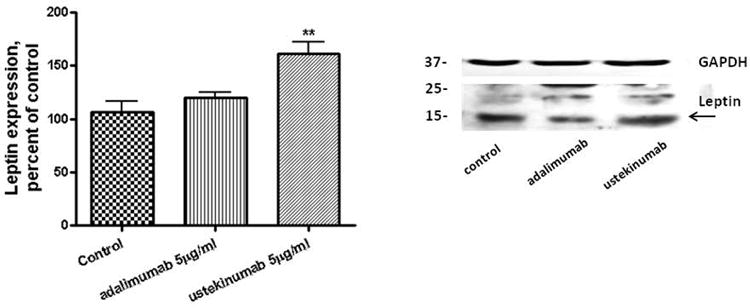
Leptin expression increased in THP-1 macrophages in the presence of ustekinumab: THP-1 macrophages were incubated for 18 h under the conditions above. Protein expression was analysed by Western blot and band intensities were calculated using GAPDH as a loading control. All results are presented as means ± SEM of three independent experiments. **P < 0.01 vs. control.
Discussion
This study shows that in cultured THP-1 macrophages, biological drugs used to treat psoriasis and psoriatic arthritis (PsA) increase leptin receptor expression. Although previous studies investigating the effect of TNF-α inhibitors on adiponectin levels have been contradictory,7 our study shows that TNF-α blockade with adalimumab increased expression of the leptin receptor in macrophages. Similarly, leptin receptor expression level increased in a concentration-dependent manner in macrophages treated with ustekinumab, an IL-12/23 inhibitor. Interestingly, neither adalimumab nor low-dose ustekinumab increased leptin, but higher doses of ustekinumab (5 μg/mL) significantly increased leptin expression.
Although median serum leptin concentrations in humans are in the 1 μg/mL range, mean peak serum concentration is between 3.1 and 14.1 μg/mL.8 Adalimumab is considered therapeutic at concentrations between 5 and 12 μg/mL, 7, 9 while ustekinumab is considered effective at concentration range of 0.70 to 1.45 μg/mL. 8, 9 Our findings are therefore applicable in a clinically relevant concentration range.
Previous studies have suggested that leptin plays a role in the development of psoriasis and its associated systemic diseases.5,6 Elevated adiponectin levels have been suggested to protect patients with inflammatory diseases from the harmful effects of their condition.7 This study suggests that one mechanism by which biologicals may function in the treatment of psoriasis and its extracutaneous manifestations is by upregulating the leptin receptor. Furthermore, ustekinumab may have the additional benefit of increasing leptin expression. These findings apply to THP-1 macrophages investigated in this study; however, more specific studies on peripheral blood mononuclear cells from patients with psoriasis will soon be conducted.
Interestingly, a recent study on patients with chronic psoriasis revealed that in contrast to patients treated with infliximab (a TNF-α inhibitor), patients treated with ustekinumab did not experience an increase in body mass index (BMI). The authors suggested the infliximab-related BMI increases may in part be due to blockade of TNF-α catabolic effects.10 Our study reveals perhaps another explanation for why treatment with ustekinumab has not been linked to BMI increases compared with treatment with a TNF-α inhibitor, namely upregulation of leptin expression.
Conclusion
This study sheds light on the possible role of leptin in immune-mediated systemic diseases such as psoriasis and PsA. Metabolic changes provoked by leptin may be beneficial or, in some situations, harmful, e.g. when it stimulates cytokine production. Recent research has examined a possible role for the polyphenolic compound resveratrol in mitigating adverse effects of leptin in inflammatory states. Further studies identifying the mechanism of action of leptin as well as the pathway through which ustekinumab alters expression of leptin and its receptor could allow for more specific treatments that could prevent systemic disease manifestations and ultimately decrease morbidity and mortality.
Supplementary Material
Learning points.
Leptin is an adipostatic circulating hormone produced in white adipose tissue, which may play a role in the development of psoriasis and its associated diseases.
Two commonly used biological drugs used in the treatment of psoriasis are adalimumab (TNF-α inhibitor) and ustekinumab (IL-12/23 inhibitor).
We found that both adalimumab and ustekinumab upregulate expression of the leptin receptor in THP-1 macrophages.
Ustekinumab also increased the expression of leptin in treated cells.
Acknowledgments
This work was supported by R21 AT007032–01A1 from The National Center for Complementary and Alternative Medicine and by the Elizabeth Daniell Research Fund.
References
- 1.Onumah N, Kircik L. Psoriasis and its comorbidities. J Drugs Dermatol. 2012;11(Suppl):s5–10. [PubMed] [Google Scholar]
- 2.Yin X, Cheng H, Zhang R, et al. Combined effect of five single nucleotide polymorphisms related to IL23/Th17 pathway in the risk of psoriasis. Immunogenetics. 2014;66:215–18. doi: 10.1007/s00251-013-0756-z. [DOI] [PubMed] [Google Scholar]
- 3.Wilson NJ, Boniface K, Chan JR, et al. Development, cytokine profile and function of human interleukin 17–producing helper T cells. Nat Immunol. 2007;8:950–7. doi: 10.1038/ni1497. [DOI] [PubMed] [Google Scholar]
- 4.Eijnden SV, Goriely S, DeWit D, et al. IL-23 up-regulates IL-10 and induces IL-17 synthesis by polyclonally activated naive T cells in human. Eur J Immunol. 2005;35:469–75. doi: 10.1002/eji.200425677. [DOI] [PubMed] [Google Scholar]
- 5.Eder L, Jayakar J, Pollock R, et al. Serum adipokines in patients with psoriatic arthritis and psoriasis alone and their correlation with disease activity. Ann Rheum Dis. 2013;72:1956–61. doi: 10.1136/annrheumdis-2012-202325. [DOI] [PubMed] [Google Scholar]
- 6.Dalamaga M, Papadavid E. Adipocytokines and psoriasis: Insights into mechanisms linking obesity and inflammation to psoriasis. World J Dermatol. 2013;2:27–31. [Google Scholar]
- 7.Engvall IL, Tengstrand B, Brismar K, et al. Infliximab therapy increases body fat mass in early rheumatoid arthritis independently of changes in disease activity and levels of leptin and adiponectin: a randomised study over 21 months. Arthritis Res Ther. 2010;12:1–11. doi: 10.1186/ar3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lebwohl M, Yeilding N, Szapary P, et al. Impact of weight on the efficacy and safety of ustekinumab in patients with moderate to severe psoriasis: rationale for dosing recommendations. J Am Acad Dermatol. 2010;63:571–9. doi: 10.1016/j.jaad.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Gisondi P, Conti A, Galdo G, et al. Ustekinumab does not increase body mass index in patients with chronic plaque psoriasis: a prospective cohort study. Br J Dermatol. 2013;168:1124–7. doi: 10.1111/bjd.12235. [DOI] [PubMed] [Google Scholar]
- 10.Krieckaert CL, Nair SC, Nurmohamed MT, et al. Personalised treatment using serum drug levels of adalimumab in patients with rheumatoid arthritis: an evaluation of costs and effects. Ann Rheum Dis. 2015;74:361–58. doi: 10.1136/annrheumdis-2013-204101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


