Abstract
Background
African Americans endure disproportionately high advanced cancer rates and also are disproportionately represented in the lower socioeconomic strata. These individuals work to manage symptoms in order to function and have a satisfactory quality of life.
Objective
The purpose of this study was to discover what low-income African American adults with advanced cancer do on a day-to-day basis to relieve and manage symptoms. This study viewed the individuals as experts and asked them not what they are told to do, but rather what they actually do.
Methods
A purposive sample of 27 individuals participated in semi-structured interviews conducted by two research interviewers. This qualitative descriptive approach used content analysis to develop themes to describe symptom self-management.
Results
Participants described two approaches: making continual adjustments and finding stability through spirituality. In seeking comfort from the distress of their symptoms, they were constantly altering their activities and fine-tuning strategies. They adjusted medical regimens and changed the speed and selection of daily activities, including comfort measures and diet modifications. In contrast, their spirituality was a consistent presence in their lives that provided balance to their unstable symptom experience.
Conclusions
This study illustrates that people with advanced cancer actively engage in multiple complex self-management strategies in response to symptoms.
Implication for Practice
As providers assess how individuals manage their symptoms, they must find ways to support those efforts. Providers then will recognize the challenges faced by advanced cancer patients in obtaining the best quality of life while managing multiple symptoms, activities, and family responsibilities.
African Americans face an exceptionally high burden of cancer. African Americans are more likely to develop cancer than any other racial or ethnic group, and the 5-year survival rate for African American adults is less than that for White adults—both overall (60% versus 69%) and within each stage of disease and for nearly every type of cancer.1 Death rates for all cancers combined continue to be higher among African Americans than Whites.1 Unfortunately, the cancer experience for many is compounded by a poor economic status, which in itself is a powerful gauge of health and well-being. African Americans are disproportionately represented in the lower socioeconomic strata: 35% of African Americans live in poverty compared to 13% of Whites.2
Cancer, particularly advanced-stage cancer, is associated with disease-related and treatment-related symptoms. Most individuals with advanced cancer have a high frequency of multiple distressful symptoms with moderate to high severity, often requiring multiple medications and management strategies.3–5 Common symptoms include pain, fatigue, and lack of appetite, all of which can negatively affect a person’s overall quality of life and ability to perform common daily activities. Distressful symptoms may result in the suffering of patients as well as their relatives and caregivers—such symptoms include long-term disability, costly hospital admissions, financial hardship, and social isolation.6 Challenges faced by advanced cancer patients, specifically African Americans, in obtaining the best quality of life while managing multiple symptoms, activities, and family responsibilities has not been fully addressed in the literature.
More information about the symptom experience for African Americans is needed given that the disparities in cancer experience of African Americans extend to include the symptom experience.7–9 Eversley and colleagues compared African Americans to other racial and ethnic groups and found that African Americans often report greater pain and higher number of symptoms compared to Whites and persons of Latino ethnicity.7 For example, being African American is associated with adverse symptoms and decreased survival among individuals with lung cancer.8 Research shows that many individuals with cancer do not receive the optimal help they need to manage symptoms, and they often report unmet needs.10,11 African American women with breast cancer are more likely to report unmet needs related to symptom management than women from other racial and ethnic groups.9 In addition, physicians often underestimate pain severity and undertreat pain in African Americans.12
Symptom management is complex because symptoms rarely occur in isolation and individuals with cancer must learn to evaluate and manage a variety of co-occurring symptoms. Symptom management strategies are actions used to avoid a negative outcome through interactions with the health care system or from self-care strategies.13 Symptom management is a dynamic process, often requiring changes in strategies over time in response to their effectiveness or the changing state of the symptom experience. The UCSF Symptom Management Conceptual Model describes the complexity of symptom management strategies by examining the what, when, where, why, how much, and how.13 The focus of this study was to ask the individuals themselves to describe these aspects of the strategies they use to manage their symptoms. These actions are collectively called “symptom self-management” and have also been described in the literature as self-care strategies, self-care behaviors, self-care measures, and self-care activities,14–18 although these concepts are not specific to only symptom management. Symptom self-management activities are done by an individual to relieve or control symptoms and can be initiated by the individual or a healthcare provider.
Though the importance of self-management strategies has been recognized, it has been minimally studied from the patient perspective.19 A systematic review exploring self-care at the end of life stage found that, to date, no published research had used a patient-centered approach to explore the elements of self-care strategies.20 Although the review found evidence of how people manage their end-of-life care, individuals were offered a list of specific behaviors from which they chose the ones they used. None of the studies asked individuals to identify how they managed illnesses themselves. The objective of this study was to discover what individuals do on a day-to-day basis to relieve and manage symptoms. The current study viewed the individuals living with advanced cancer as experts and asked them not what they were told to do, but what they actually did. Additionally, this study narrated the experience of low-income African Americans, an underserved community with a high disease burden, whose perspectives are rarely included in research.
Methods
A descriptive qualitative approach was used in this study to provide an insiders’ account of managing multiple symptoms related to advanced cancer.21,22 Data collection was conducted via in-depth, semi-structured interviews of symptomatic African American individuals with advanced-stage cancer to gather information about self-management strategies. The goal of using this qualitative approach was to learn about strategies used to manage symptoms directly from African American individuals experiencing the symptoms, not just what providers had prescribed.
Sample and Setting
A total of 59 individuals were recruited from oncology clinics in a cancer center of a large urban public hospital in a large southeastern city. Participants who met the following criteria were invited to participate in the study: (a) 21 years or older; (b) self-identified English speaker; (c) self-identification as Black (African American or other ancestry); (d) living in a personal residence, not in a skilled care facility or hospital; (e) diagnosed with advanced cancer, defined as metastatic or locally advanced refractory disease per medical record review; (f) experiencing at least two symptoms of moderate severity per the Edmonton Symptom Assessment Scale (ESAS); (g) impoverished (self-report of personal income below Federal poverty level); (h) determined mentally competent to give informed consent by health care provider; and (i) being physically able to tolerate a one- to two-hour interview as determined by the individual’s health care provider.
Moderate symptom severity was determined as a score of 4 or higher for at least two symptoms on the ESAS. On the ESAS, the severity of each symptom is rated on a visual analogue numerical scale of 0 to 10 (0 = no symptom, 10 = worst possible symptom). Using a score of 4 as the minimum cut-off was based on prior research indicating that a 4 on a 0 to 10 scale is most often equivalent to moderate severity across multiple symptoms.23 The ESAS has been thoroughly tested (test-retest, content validity, concurrent validity, predictive validity, and sensitivity and specificity), mostly in individuals with advanced cancer, and has been found to be both valid and reliable in the assessment of symptoms in cancer.24–26 The ESAS measures nine symptoms: pain, fatigue, nausea, anorexia, dyspnea, drowsiness, insomnia, depression, and anxiety. A tenth symptom, feelings of well-being, and an optional eleventh symptom, constipation, were also assessed.
Procedures
The study protocol was approved by the institutional review boards at the university and hospital. Participants were recruited over ten months, from August 2010 to May 2011. At each clinic, a health care provider introduced potential participants to the study and determined whether the individual was competent to give consent, able to physically tolerate the interview, and interested in learning more about the study from the research staff. After an introduction to the study and the consent process, eligible participants chose an interview location—either at his or her home or in a private conference room adjacent to the clinic. Of the 59 participants who were screened, 16 did not meet eligibility requirements: three were not interested, two had cancer that was not advanced, nine did not meet symptom criteria, one did not self identify as African American, and one was unable to talk. An additional 16 eligible individuals were scheduled for an interview but did not complete it: one individual died prior to the scheduled interview, two were admitted to the hospital prior to the scheduled interview, and one individual was too sick to be interviewed at the scheduled time. The remaining 12 individuals were not able to be interviewed due to lack of communication and follow up despite multiple attempts to contact them. Twenty-seven individuals successfully completed the study.
Eleven interviews were conducted at the clinic or hospital and 16 interviews were conducted at the participants’ home. All but two interviews were completed with two interviewers present—the PI (a White female nurse researcher) and an African American retired female nurse who had worked most recently as an organizer for a residential community. The second interviewer was included with the intention of increasing the level of trust with the interview process, as she brought a perspective more grounded in the participants’ community. All interviews were audio recorded, then transcribed by a professional transcriptionist. The interviews lasted approximately 60 minutes on average, with a range of 22 to 82 minutes. An interview guide, based on a literature review, was used during the interview process, which included opened ended questions and suggested probes to use if needed. Sample questions are as follows: (1) What do you do to make the (symptom) better? (2) Tell me about how you manage these symptoms. (3) Describe a time when you were able to make your (symptom) better. (4) After living with this (symptom), what advice would you give to someone else that just experienced this (symptom)?
At the conclusion of the interviews, the participants were thanked and compensated for their input and time. As recommended by a Community Advisory Board, the participants were each given a $20 gift card to a local grocery store. In addition, they also received a coupon for free parking at the clinic or a coupon redeemable for two public transportation rides.
Analysis
Content analysis27,28 was used to analyze the data and began with the researcher reading and rereading the transcripts to get a sense of the big picture. Then, the researcher began open coding and identified codes that reflected one key thought. Selected examples of participants’ words were used to establish properties of each code and were organized in a codebook. In this early phase, the first author and two additional persons (a clinician in palliative care and a skilled qualitative researcher) coded the interviews. The dialogue among the coders during this process allowed for exploration of what the codes represented and assisted with the next phase in which categories were created. Categories were used to reduce the number of codes by grouping similar codes into broader categories. Categories were created by examining how different codes were related and linked as well as how codes were different and did not belong in the same category. These categories were then used to organize and group codes into meaningful clusters or themes. This thematic organization was validated with two qualitative experts to corroborate findings, discuss the analytical decision-making process, and work through any inconsistencies in the interpretation of the data.
For this study, validity was examined at two levels—procedural and analytical—through transparency in each phase of the study. All processes, collaborations, and data decisions were documented as part of an audit trail. The analysis process was checked frequently in discussions with two qualitative experts to look for distortion of validity.
Results
The demographic and clinical characteristics of the 27 participants are summarized in Tables 1 and 2. Participants’ cancer diagnoses varied considerably, although the most common cancers represented were breast (9) and lung (8). Most participants were recruited from the palliative care clinic, and the others came from various oncology clinics. About half of the participants in the sample had received palliative care support.
Table 1.
Demographic Characteristics (n=27)
| Variable | M(range) | n | % |
|---|---|---|---|
| Age: mean (range) | 57 (30–79) | ||
| Gender | |||
| Female | 18 | 63 | |
| Male | 9 | 37 | |
| Marital Status | |||
| Single | 14 | 52 | |
| Divorced/separated | 7 | 26 | |
| Married | 3 | 11 | |
| Widowed | 2 | 7 | |
| In a committed relationship (established partner but not married) | 1 | 4 | |
| Residence | |||
| Own home or apartment | 15 | 56 | |
| Family member’s home or apartment | 10 | 37 | |
| Non family member’s home or apt. | 2 | 7 | |
| Number in Household | |||
| One | 7 | 26 | |
| Two to three | 12 | 44 | |
| Four to five | 6 | 22 | |
| Six to eight | 0 | 0 | |
| Nine to ten | 2 | 7 | |
| Education | |||
| Less than high school | 10 | 37 | |
| High school graduate | 10 | 37 | |
| Some college | 2 | 8 | |
| College graduate | 3 | 11 | |
| Graduate School | 2 | 8 | |
| Health Insurance Type | |||
| Medicaid | 11 | 41 | |
| Medicare and Medicaid | 5 | 19 | |
| Medicare | 2 | 7 | |
| No insurance | 8 | 30 | |
| Other | 1 | 4 |
Table 2.
Clinical Characteristics (n=27)
| Variable | n | % |
|---|---|---|
| Cancer Diagnosis | ||
| Breast | 9 | 33 |
| Lung | 8 | 30 |
| Prostate | 3 | 11 |
| Ovarian | 3 | 11 |
| Cervical | 1 | 4 |
| Leiomyosarcoma | 1 | 4 |
| Renal Cell | 1 | 4 |
| Vocal Cord | 1 | 4 |
| Recruitment Source | ||
| Palliative Care Clinic | 13 | 48 |
| Breast Cancer Clinic | 5 | 19 |
| Lung Cancer Clinic | 5 | 19 |
| General Oncology Clinic | 2 | 11 |
| Gynecology Oncology Clinic | 1 | 4 |
| Radiation Oncology Clinic | 1 | 4 |
| Served by palliative care clinic | ||
| Yes | 14 | 52 |
| No | 13 | 48 |
| Co-morbidities per self report | ||
| None | 8 | 30 |
| Hypertension | 15 | 56 |
| Respiratory Disease | 5 | 19 |
| Diabetes | 3 | 11 |
| Cardiac Disease | 3 | 11 |
| Deep Vein Thrombosis | 2 | 7 |
| Lupus | 1 | 4 |
| Stroke | 1 | 4 |
| Arthritis | 1 | 4 |
| Vascular Disease | 1 | 4 |
| Gout | 1 | 4 |
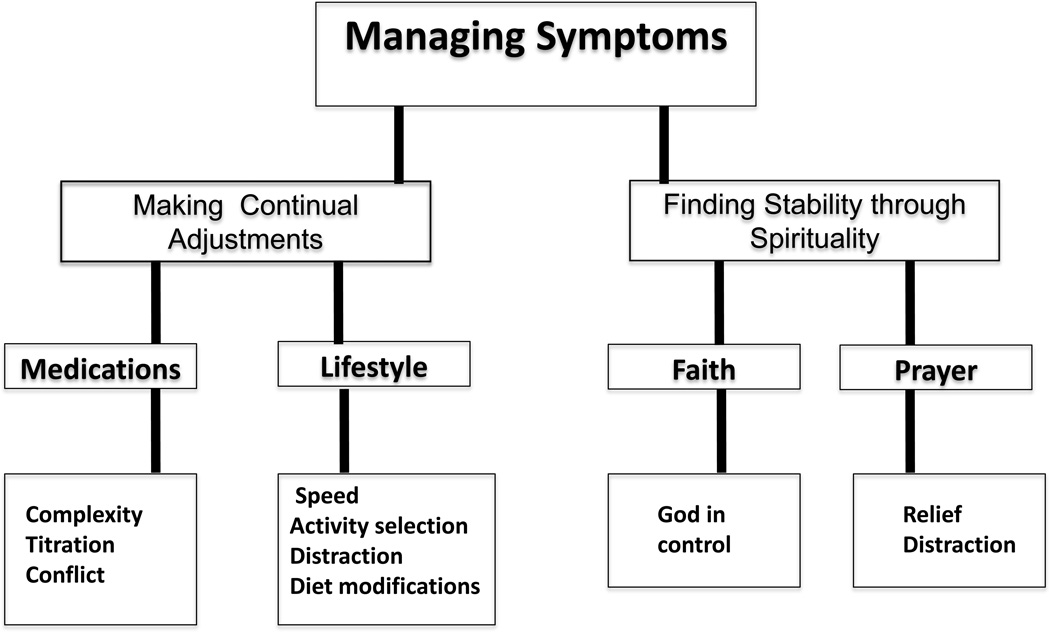
Participants described numerous strategies to manage their multiple symptoms. The most common symptoms included pain, tiredness, anorexia, shortness of breath, depressed mood, sleep difficulties, nausea, and constipation. A full description of the symptom experience is reported elsewhere.29 Overall, two main themes described how study participants managed their symptoms: making continual adjustments and finding stability through spirituality (See Figure 1). The adjustment theme relates to participants’ need to constantly make changes and regulate activities for the purpose of finding symptom relief. To the participants, the symptoms signaled that something needed to be done–be it medication adjustment or a change in daily activities–and individuals then responded to the signal. In seeking comfort from the distress of their symptoms, they were constantly altering their activities and fine-tuning strategies. In contrast to shifting activities, their spirituality was an unceasing presence in their lives that provided balance to their unstable symptom experience. Faith and prayer were a constant for the participants and provided comfort and a sense of stability. While the symptom management adjustments added a certain amount of unpredictability to their lives, their faith provided a source of calmness and peace.
Figure 1.
Medications- complexity, titration, and conflict
Participants with symptoms often self-administered medications to provide symptom relief. With prescription medications, physicians wrote the order, but the participants held the responsibility of taking the medications and often adjusted the medications to suit their needs. Medications adjustments included differentiating the type, dose, and timing of the medication, and the participants found this challenging to manage. Participants took medications for pain, cough, sleep, anorexia, wheezing, insomnia, constipation, nausea, high blood pressure, neuropathy, blood clots, depression, anxiety, and as part of their cancer treatment. The medication regimens that most of the participants took for co-morbidities were complex, and when medications to relieve symptoms were added, the complexity escalated. All of these medications required knowledge, which was most often provided by health care providers.
In specific, participants frequently discussed different types of opiates and the principles of administering opiate medications. They spoke of long- versus short-acting medications as well as around-the-clock dosing and as-needed dosing. However, for multiple reasons, the participants took the medications based on their own assessments of need and benefit, sometimes disregarding the instructions from the provider. In particular, participants monitored their pain and activity and then decided how to take their pain medication. They decided which medication to take, how much to take, and the timing. Some participants took less and some took more than their provider prescribed as they adjusted the dose based on symptom intensity. Participants recognized the need to listen to their bodies, and they often based their medication intake on the intensity of their symptoms. This frequently meant disregarding the prescription instructions, illustrated in this example of an individual prescribed an extended release opiate: “I felt myself how the pain was doing me. I felt how, it was coming on, my body was telling me, letting me know when that pain was coming up or whatever, you know, and that’s when I start taking them. And then I see the schedule they have me on, well that’s what they wanted me to do, take it when I don’t have pain, and ah, I didn’t want to take it if I didn’t have pain.”
Along with the medications prescribed by the physicians, a few participants mentioned the use of over-the-counter medications for symptom management, which further added to the complexity of their medication regimen. Specifically, participants used Goody’s Powders™ and ibuprofen for pain, as well as over-the-counter suppositories, Maalox™, and Milk of Magnesium™ for constipation. The most common category of over-the-counter medications was topical ointments and liniments such as Watkins camphor, sports creams, Icy Hot™ ointment, and green rubbing alcohol. Medications for symptoms, whether prescribed by a physician or not, in addition to medications to treat co-morbidities, created a complex management activity for many participants.
In addition, participants titrated the dose of pain medication they took based on the side effects of the medications, such as drowsiness and constipation. One person spoke of the effect of her pain medication on her cognitive ability and her continual assessment of her ability to adequately negotiate the bus while on pain medication: “So I still take pain medication for that (pain). But I try not to take it too often, because then you can’t be, you know, bright enough to ride the bus. You’re too tired.” Participants often experienced an internal conflict between the need to take medication to reduce pain and the desire to avoid the side effects of the pain medication that impacted their ability to function. One participant, who was the sole caregiver for her three school-age children, felt conflicted about driving and taking her medications: “I mostly don’t try to take my medication, cause I don’t have nobody to drive for me. But I’m always going to have to take medication because I’m always in pain.” Although pain medication was the main medication discussed, others also spoke of titrating medications for depression and constipation.
The internal conflict about medication was further demonstrated by participants’ reluctance to take medications for reasons other than side effects. Participants described general dislike of medications—yet when they experienced symptoms, they had no choice but to take the medications for relief. A few participants expressed concern about taking pain medication and addiction. These individuals shared how they carefully limited their dose, sometimes resulting in suffering: “So I will suffer sometimes not to be dependent on it. I don’t want to have to say, you know, it’s three hours gone by; I’ve got to take this pain medication. I’ll let it go another three and just deal with it. I don’t want—I just am determined I’m not going to be addicted to anything.” Overall, the participants reported that the medications were effective at reducing symptoms, but many described an internal debate: they did not want to take the medication for various reasons, but knew they needed to take it.
Lifestyle Modifications- speed, activity selection, distraction, and diet modifications
In response to their symptoms, study participants made changes to their lifestyle. Similar to adjusting medications, participants adjusted their activities based on symptoms and clues from their bodies. They adjusted the speed of their activities or type of activities in search of symptom relief: “I listen to my body because if you don’t, you’re putting stress on your body, you’re putting stress on yourself. You have to listen to your body. When your body start aching, it meaning it’s time for you to sit down and relax, and to get yourself together, because it’s only going to get worse, meaning the pain because I have pain if I’m standing up for a long period of time, walking. It’s, you know, whatever I’m doing, I have a time limit because my body tells me.”
Life slowed down for many of the study participants. The need to rest resulted in a new pattern or schedule for the day. Because schedules had to be rearranged and tasks took longer to complete, participants shifted their daily timelines. Symptoms affected the amount of work they completed and impacted their ability to care for themselves and families, do household chores, and navigate hospital visits. Individuals said they had no choice but to curtail activities because of symptoms, mostly pain and extreme tiredness. The tiredness often overwhelmed many of these participants who described a busy life prior to cancer. One participant described her life before cancer as very busy and active; she often balanced two jobs and managed a family. Now with pain and shortness of breath, she said she could only do a little activity at a time and then had to rest. Many adjusted their activities and made time for a brief respite, but still faced the tasks that had to be done as they worked through their symptoms. “I get in this chair and sit down when I get tired and lean back for a few minutes, and then I get up and do what I got to do, before it comes over me again, and it does come, all day long.” Cognitive changes also required participants to adjust to a slower pace. One participant spoke of her inability to recall words in a conversation. Before cancer, she wrote grants and worked under time constraints, but she accepted that she now needed more time to communicate.
Despite not feeling well, participants needed to continue to care for themselves and their family and plan out their day. Many changed the activities they participated in, sometimes eliminating activities or trying new activities. At times, the presence of symptoms meant an activity could no longer be completed, at any speed, which often led to sadness and frustration. Activities impacted included self-care, housekeeping, church attendance, and travel. Many spoke of not being able to drive or take the bus because of pain or weakness. Some individuals participated in new activities to provide comfort or distraction. For comfort, many participants applied heat or pressure wraps to a painful area. Aromatherapy and breathing exercises were also used to decrease anxiety.
Others spoke of participating in activities to distract themselves, which acted as a way to decrease pain and depressed mood. Activities mentioned included watching television, talking to friends or family, playing with their children, listening to music, singing, exercise, and doing puzzles. One participant who had unrelieved pain and shortness of breath that severely limited her activities spoke of doing word puzzles to distract herself from the pain: “When I’m concentrating on the word I’m looking for I don’t think about pain and stuff. I still have them. I know I have them, but just like it ease it up and I know that’s something I can do.”
Most participants spoke of adjusting their diet in order to manage their symptoms. For participants, the new focus of eating was often to relieve symptoms, such as anorexia, constipation, nausea, pain, and tiredness. Many adjusted their eating habits in terms of both food selection and quantity, as they tried to treat their symptoms. For constipation, participants increased their intake of vegetables, fruits, water, and herbal teas. Many ate lighter meals. To reduce pain, participants decreased sugary foods and caffeine. To manage sore throats and mouths, individuals ate soft, bland food. One participant spoke of using the condiment mustard to treat pain caused by abdominal bloating, which was advice she had received from her mother. Others made adjustments in their diet to decrease nausea or manage their inability to taste food. Participants drank ginger teas, ginger ale, and peppermint tea as effective treatments for nausea. Decreasing the size of portions also reduced nausea for some. Some participants used liquid nutritional supplements to increase their caloric intake, either by mouth or by a feeding tube. Overall, this group recognized the relationship between their diet and symptoms as well as their general health. They carefully evaluated their diets and then made adjustments, although some identified financial barriers to obtaining organic and fresh foods.
Finding Stability through Spirituality
Almost all of those interviewed discussed using their faith to help manage the symptoms they were experiencing. Spirituality provided a stable foundation in the face of the constantly changing adjustments they needed to make to respond to their symptoms. Participants possessed a strong belief and trust in a higher power, which provided comfort. Faith was demonstrated through acts of private religiosity, such as praying, reading the bible, and listening to religious programs. Participation in these activities often provided symptom relief. Participants used prayer as a strategy to solve personal problems and decrease symptoms. However, participants did not talk about attending church or other acts of public religiosity.
Faith- God in control
Individuals spoke about faith as an anchor in their lives that provided reassurance and comfort. They felt a higher power was in control of their lives despite the suffering they experienced from their symptoms: “Sometimes I let my mind go and get off my religion, and then it hits me. What in the world are you thinking about? You know God is in control, and that’s what He’s there for, to help us, you know. So I start dwelling on Him, and I’ll even get my Bible and read Him and what have you. And it’s, maybe it’s in my mind, but I start to feel better.” On numerous occasions, participants explained the power of their faith and its control in their lives. Cancer, and sometimes symptoms, robbed them of control, but they felt their faith was in control—making them feel positive and strong.
Prayer-relief and distraction
Prayer served as an active exchange. Participants used prayer to receive support and symptom relief. When individuals described how they prayed, some spoke of talking to their God when they were lonely and no one else was around. Many described how their prayers were answered and how they had experienced miracles. Some participants prayed for symptom relief and others prayed to distract themselves from the symptoms; both methods decreased the distress associated with symptoms. Prayer resulted in decreased pain, fear, worry, depressed mood, tiredness, anorexia, and sleep issues—prayer improved participants’ overall well-being. Participants often referred to prayer as being like a medication or a fuel. Prayer gave them relief from pain in the middle of night when sleeping proved difficult. One person noted, “That’s the time to talk, when you hurting. Maybe that is the reason it goes away.” Some used prayer as a distraction—something to get their mind off of their pain. Prayer blocked out pain: “These pains is still here, but I can block em out by talking with God.”
Discussion
The purpose of this study was to explore the symptom self-management practices of low-income African American adults with advanced cancer. The findings provide a detailed description of how African Americans with advanced cancer living in poverty manage multiple symptoms on a day-to-day basis. Often research on the poor addresses access to care issues, including barriers. In contrast, this study looked at how these individuals who had access to care from a safety net hospital managed symptoms at home. Overall, the individuals in this study were resourceful and engaged. During the interviews, most participants did not address the financial challenges in their lives as they discussed how they managed symptoms except when they discussed the expense of fresh and organic foods. Even though all of the participants had advanced cancer (metastatic or locally advanced refractory disease), they were still involved and engaged in self-managing their symptoms. These actions taken in response to their symptoms was supported by the stability of their faith and the comforting influence of their prayers. Although many challenges were apparent in the participants’ lives, the individuals generally maintained positive attitudes that were often directly related to their spirituality. Their belief that the course of their lives was in the hands of their God freed them to concentrate on their immediate needs and sustained their efforts to manage their demanding daily regimens of self-care.
These findings contribute to the literature on symptom self-management. The strategies shared by the study participants were described as outlined in the UCSF Symptom Management Model (the what, where, and how).13 One important component of the participants’ experience was the need to constantly monitor their symptoms and adjust their strategies. Wilde and Garvin’s30 concept analysis of self-monitoring is useful in interpreting the current study’s findings. Self-monitoring includes awareness of symptoms, sensations, daily activities, and cognitive processes—each of which provides information for action. The medications and lifestyle adjustments identified in this study required participants to demonstrate diligence in monitoring symptoms so that they could make appropriate changes and find symptom relief.
The continuum of self-management practices was illustrated in this study. Some of the strategies came from the individual’s prior experiences, family suggestions, or trial and error. Other strategies, such as medications, were prescribed by health care providers. Adjustments to the prescribed medications was a major strategy participants employed to care for their symptoms. Most individuals managed multiple medications for symptom relief in addition to other medications for co-morbidities, resulting in a complex regimen. Individuals discussed the challenges of titrating their pain medication appropriately and managing medication side effects. Similar work by Schumacher and colleagues31 showed that individuals struggled in many areas when they attempted to take a regimen of pain medication at home. Similarly to the findings of this study, participants made decisions about which drug to take, how much to take, and the timing of the drug administration. This research therefore offers important descriptions of an element frequently missing from the palliative care literature—the complexity of medication regimens for symptom relief that patients with advanced cancer must manage at home. Providers seek to tailor symptom management regimens for patients, but patients often then tailor the providers’ prescriptions to fit their own changing symptom profiles and day-to-day experiences.
Previous studies on cancer pain management in minorities identified similar themes related to reluctance to take pain medication and concerns about possible addiction.32–34 The national dialogue about drug abuse and the over-prescription of opioids conflates with the issue of pain treatment. The problem of opiate abuse is discussed in the medical community35 and lay media36 and thus may influence individuals who have been prescribed opiates to treat their cancer pain, as well as their social network. Despite these beliefs about drug use, one study found under-use of opiates (20%) was more common than over-use (9%), consistent with research on adherence to other medications.37 In light of these issues, continued discussion about the use of medications to treat cancer symptoms is needed across our society. Although the patients were living with advanced cancer and pain, they expressed reluctance to take the medications the doctors had prescribed.
Participants found that lifestyle adjustments required finding a balance between symptom relief and participation in the normal day-to-day activities that sustained them prior to their cancer experience. One study describing self-care activities at the end of life stage found that the desire to maintain normality, even when seriously ill, was very important.38 Participants of the current study modified their lifestyle by resting, slowing down, and making changes to activities and diet; however, they worked hard to stay engaged and connected to their “normal” life. This “trade-off” phenomenon has been described by others as an individual’s struggle to both obtain symptom relief and maintain functionality in their lives.39 In a study of the daily activities of women with metastatic breast cancer, the women remained very active, yet also reported a high frequency of taking naps and resting.40 These findings are similar to those from the current study, in which the need to rest influenced the amount of daily work the participant was able to complete.
This study describes the multiple adjustments participants made to their diet in order to manage symptoms, similar to the findings from qualitative and quantitative work by Hopkinson and colleagues.41,42 While Hopkinson’s work focused on the challenges of eating for those with advanced cancer, the current study adds to these findings by describing in detail the daily diet adjustments participants made specifically to relieve symptoms. Overall, participants expressed a longing for their life before cancer, where the pleasure of eating was a normal part of their day without the complications of symptoms.
The use of spiritual beliefs and practices by African Americans to cope with serious health problems, such as depression, cancer, heart disease and mental illness, has been well documented.43–45 The current study corroborates this earlier literature, as participants identified spirituality as a major strategy used specifically to manage symptoms. Without being prompted during the interviews for this study, participants described how they prayed as part of their symptom management and how they derived comfort, courage, and hope from their faith. Whereas most participants of the current study used prayer as a strategy to solve personal problems and minimize symptoms, they attended church services and interacted with church members only minimally, perhaps due to the severity of their illness. Balboni and colleagues43 found that illness-related physical limitations caused their sample of 230 individuals (19% African American) with advanced cancer to be less engaged with religious communities, which may help explain the current findings.
The findings of this qualitative study must be considered in light of several methodological limitations. The sample was a small, purposive sample, and the data included the perceptions of low-income individuals within one hospital system in one city in the Southeast. The single interview design did not provide information on how individuals’ strategies of symptom management changed over time. In addition, selection bias cannot be ruled out, which may have resulted in a more active and engaged sample of individuals with advanced cancer. The initial contact with potential participants was through a health care provider who made the decision whether to consider the individual fit for the study. When recruiting sick, vulnerable individuals, health care providers can serve as gatekeepers, protecting their more sick and vulnerable clients from any extra activities. In addition, the focus of the study was on individuals with few financial resources, but participants were not asked specifically how financial challenges impacted their ability to care for their symptoms. Including this question would have given a more complete picture of the participants’ experience. In contrast, spirituality was not included in any of the interview questions, but all of the participants described this strategy to manage symptoms. More information about their religious background and affiliation would have been helpful but was not collected.
Implications
Based on the findings of this study, providers should assess how individuals manage their symptoms and find ways to support those efforts. Providers must recognize the expertise of the person living with cancer in regard to his or her own care and incorporate this into their treatment regimen. Providers who form partnerships with patients and families can enable and empower patients and families to achieve their own goals of care. Taking this patient-centered approach, providers can support patients’ efforts and determine how prescribed treatments, such as medications, interact with the individuals’ personal strategies. In contrast to labeling patients as non-adherent, providers should take care to recognize the challenges faced by advanced cancer patients in obtaining the best quality of life possible while managing multiple symptoms, activities, and family responsibilities. Additionally, health care providers should consider the importance of spirituality for individuals with advanced cancer. In this study, individuals often mentioned prayer as the primary way they managed their pain, with medications and other strategies as supplemental to this spiritual strategy. Cancer patients report that health care providers do not recognize, treat, or offer appropriate referrals to address spiritual needs, despite that patients are seeking this intervention.46,47 Progress has been made in integrating spirituality into clinicians’ practice, as demonstrated by the development of National Competencies in Spirituality and Health education, but further work is needed.47
The findings of this study point to many fertile areas for additional research. Further research on individuals with cancer must include adequate representation of low-income African Americans and other minorities. For too long, researchers have recruited predominantly White, middle- to upper-class, well-educated individuals to participate in research. Researchers must reach out to the African American community to build trust and develop meaningful, community-engaged research. In addition, studies rarely include participants’ income status as a variable, leaving the reader to assume that it is of little importance. Overall, low-income study participants from any community need greater representation in research, especially in the areas of cancer support and end-of-life care.
Research has been done to test interventions that improve quality of life and decrease symptoms throughout the cancer continuum; however, few studies have focused on interventions at the end of life stage.48 In addition, interventions have been built to support and educate patients how to “self manage” their care, but that care is orchestrated by health care providers and often does not originate with the patient. Interventions that include strategies originating with the patient, where the provider and patient partner together, have potential to improve patient acceptance and sustainability. Specifically, when managing symptoms—especially pain—a greater understanding of the tasks required to manage complex medication regimens is needed. Interventions are needed that assist patients in managing multiple medications for symptoms and comorbidities. The skills needed to titrate medication based on symptom severity require greater understanding of the patient perspective. In addition, further work should focus on how spirituality can be incorporated into the medical care of African Americans with cancer. A community-based participatory research approach, where individuals with cancer collaborate with members of the religious community, clinicians, and researchers to develop and test interventions, would be in an important area of research.
Individuals with advanced cancer, specifically low-income African Americans, are actively engaged day-to-day in making adjustments in medications and activities to find symptom relief. Faith and prayer supplement continual adjustments by providing comfort and support. Information gained from the patient perspective can help guide care and research in symptom self-management with the end goal of assisting individuals with advanced cancer live out their days as fully, productively, and comfortably as possible.
Acknowledgements
The authors thank all participants who were so willing to share their story. They also thank Rachel Whitworth, Pat Martin, and Laura Waddle for their help with the study.
Funding statement: Dr. Yeager was a recipient of the Doctoral Scholarship in Cancer Nursing from the American Cancer Society and also supported by training award, F31NR011383, from the National Institute of Nursing Research during the time that this work developed. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
Conflict of interest statement: No conflict of interest related to this manuscript has been declared by the authors.
Contributor Information
Katherine A. Yeager, Nell Hodgson Woodruff School of Nursing, Emory University.
Susan Bauer-Wu, University of Virginia School of Nursing.
Colleen DiIorio, Rollins School of Public Health, Emory University.
Tammie E. Quest, Department of Veteran’s Affairs; Department of Emergency Medicine, Emory University.
Claire E. Sterk, Rollins School of Public Health, Emory University.
Catherine Vena, Nell Hodgson Woodruff School of Nursing, Emory University.
References
- 1.Cancer Facts & Figures for African Americans 2013–2014. Atlanta: American Cancer Society; 2013. American Cancer Society. [Google Scholar]
- 2.Kaiser Family Foundation. Poverty Rate by Race/Ethnicity. [Accessed 10/17/13, 2013];2013 http://kff.org/other/state-indicator/poverty-rate-by-raceethnicity. [Google Scholar]
- 3.Riechelmann RP, Krzyzanowska MK, O'Carroll A, Zimmermann C. Symptom and medication profiles among cancer patients attending a palliative care clinic. Support Care Cancer. 2007;15(12):1407–1412. doi: 10.1007/s00520-007-0253-8. [DOI] [PubMed] [Google Scholar]
- 4.Tsai JS, Wu CH, Chiu TY, Hu WY, Chen CY. Symptom patterns of advanced cancer patients in a palliative care unit. Palliative Medicine. 2006;20(6):617–622. doi: 10.1177/0269216306071065. [DOI] [PubMed] [Google Scholar]
- 5.Walsh D, Donnelly S, Rybicki L. The symptoms of advanced cancer: relationship to age, gender, and performance status in 1,000 patients. Support Care Cancer. 2000;8(3):175–179. doi: 10.1007/s005200050281. [DOI] [PubMed] [Google Scholar]
- 6.Sherwood PR, Donovan HS, Rosenzweig M, Hamilton R, Bender CM. A house of cards: the impact of treatment costs on women with breast and ovarian cancer. Cancer Nurs. 2008;31(6):470–477. doi: 10.1097/01.NCC.0000339255.75947.a8. [DOI] [PubMed] [Google Scholar]
- 7.Eversley R, Estrin D, Dibble S, Wardlaw L, Pedrosa M, Favila-Penney W. Post-treatment symptoms among ethnic minority breast cancer survivors. Oncology Nursing Forum. 2005;32(2):250–256. doi: 10.1188/05.ONF.250-256. [DOI] [PubMed] [Google Scholar]
- 8.Tammemagi CM, Neslund-Dudas C, Simoff M, Kvale P. Lung carcinoma symptoms--an independent predictor of survival and an important mediator of African-American disparity in survival. Cancer. 2004;101(7):1655–1663. doi: 10.1002/cncr.20547. [DOI] [PubMed] [Google Scholar]
- 9.Yoon J, Malin J, Tisnado D, et al. Symptom management after breast cancer treatment: is it influenced by patient characteristics? Breast Cancer Research and Treatment. 2008;108(1):69. doi: 10.1007/s10549-007-9580-1. [DOI] [PubMed] [Google Scholar]
- 10.Morasso G, Capelli M, Viterbori P, et al. Psychological and symptom distress in terminal cancer patients with met and unmet needs. J Pain Symptom Manag. 1999 Jun;17(6):402–409. doi: 10.1016/s0885-3924(99)00034-2. [DOI] [PubMed] [Google Scholar]
- 11.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291(1):88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 12.Anderson KO, Mendoza TR, Valero V, et al. Minority cancer patients and their providers: pain management attitudes and practice. Cancer. 2000;88(8):1929–1938. [PubMed] [Google Scholar]
- 13.Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. J Adv Nurs. 2001;33(5):668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- 14.Borthwick D, Knowles G, McNamara S, Dea RO, Stroner P. Assessing fatigue and self-care strategies in patients receiving radiotherapy for non-small cell lung cancer. Eur J Oncol Nurs. 2003;7(4):231–241. doi: 10.1016/s1462-3889(03)00046-2. [DOI] [PubMed] [Google Scholar]
- 15.Richard AA, Shea K. Delineation of self-care and associated concepts. J. Nurs. Scholarsh. 2011;43(3):255–264. doi: 10.1111/j.1547-5069.2011.01404.x. [DOI] [PubMed] [Google Scholar]
- 16.Richardson A, Ream EK. Self-care behaviours initiated by chemotherapy patients in response to fatigue. Int J Nurs Stud. 1997;34(1):35–43. doi: 10.1016/s0020-7489(96)00031-4. [DOI] [PubMed] [Google Scholar]
- 17.Williams PD, Piamjariyakul U, Ducey K, et al. Cancer treatment, symptom monitoring, and self-care in adults - Pilot study. Cancer Nurs. 2006;29(5):347–355. doi: 10.1097/00002820-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Landers M, McCarthy G, Livingstone V, Savage E. Patients' bowel symptom experiences and self-care strategies following sphincter-saving surgery for rectal cancer. J Clin Nurs. 2014;23(15–16):2343–2354. doi: 10.1111/jocn.12516. [DOI] [PubMed] [Google Scholar]
- 19.Dodd MJ, Miaskowski C. The PRO-SELF program: A self-care intervention program for patients receiving cancer treatment. Seminars in Oncology Nursing. 2000;16(4):300–308. doi: 10.1053/sonu.2000.16586. [DOI] [PubMed] [Google Scholar]
- 20.Johnston B, McGill M, Milligan S, McElroy D, Foster C, Kearney N. Self care and end of life care in advanced cancer: Literature review. Eur J Oncol Nurs. 2009;13(5):386–398. doi: 10.1016/j.ejon.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 21.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 22.Sandelowski M. What's in a name? Qualitative description revisited. Res Nurs Health. 2010;33(1):77–84. doi: 10.1002/nur.20362. [DOI] [PubMed] [Google Scholar]
- 23.Given B, Given CW, Sikorskii A, et al. Establishing mild, moderate, and severe scores for cancer-related symptoms: how consistent and clinically meaningful are interference-based severity cut-points? J Pain Symptom Manage. 2008;35(2):126–135. doi: 10.1016/j.jpainsymman.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7(2):6–9. [PubMed] [Google Scholar]
- 25.Chang VT, Hwang SS, Feuerman M. Validation of the Edmonton Symptom Assessment Scale. Cancer. 2000;88(9):2164–2171. doi: 10.1002/(sici)1097-0142(20000501)88:9<2164::aid-cncr24>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 26.Richardson LA, Jones GW. A review of the reliability and validity of the Edmonton Symptom Assessment System. Curr Oncol. 2009;16(1):55. doi: 10.3747/co.v16i1.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 28.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 29.Yeager KA, Bauer-Wu S, Vena C. 2012 Science of Eliminating Health Disparities Summit. Washington, DC: 2012. Dec 17–19, The Symptom Experience of Low-Income African Americans with Advanced Cancer. [Google Scholar]
- 30.Wilde MH, Garvin S. A concept analysis of self-monitoring. J Adv Nurs. 2007;57(3):339–350. doi: 10.1111/j.1365-2648.2006.04089.x. [DOI] [PubMed] [Google Scholar]
- 31.Schumacher KL, Koresawa S, West C, et al. Putting cancer pain management regimens into practice at home. Journal of Pain & Symptom Management. 2002;23(5):369–382. doi: 10.1016/s0885-3924(02)00385-8. [DOI] [PubMed] [Google Scholar]
- 32.Anderson KO, Richman SP, Hurley J, et al. Cancer pain management among underserved minority outpatients: perceived needs and barriers to optimal control. Cancer. 2002;94(8):2295–2304. doi: 10.1002/cncr.10414. [DOI] [PubMed] [Google Scholar]
- 33.Meghani SH, Keane A. Preference for analgesic treatment for cancer pain among African Americans. J Pain Symptom Manag. 2007;34(2):136–147. doi: 10.1016/j.jpainsymman.2006.10.019. [DOI] [PubMed] [Google Scholar]
- 34.Rhee YO, Kim E, Kim B. Assessment of pain and analgesic use in African American cancer patients: Factors related to adherence to analgesics. J Immigr Minor Health. 2012;14(6):1045–1051. doi: 10.1007/s10903-012-9582-x. [DOI] [PubMed] [Google Scholar]
- 35.Gagnon AM, Kahan M, Srivastava A. Opioid use and abuse: Is there a problem? Clin J Pain. 2007;23(8):661–662. doi: 10.1097/AJP.0b013e31814b1d46. [DOI] [PubMed] [Google Scholar]
- 36.Deadly Dose: Dr. Sanjay Gupta Reports [transcript] CNN television. 2012 Nov 18; [Google Scholar]
- 37.Lewis ET, Combs A, Trafton JA. Reasons for under-use of prescribed opioid medications by patients in pain. Pain Med. 2010;11(6):861–871. doi: 10.1111/j.1526-4637.2010.00868.x. [DOI] [PubMed] [Google Scholar]
- 38.Johnston BM, Milligan S, Foster C, Kearney N. Self-care and end of life care-patients' and carers' experience a qualitative study utilising serial triangulated interviews. Support Care Cancer. 2012;20(8):1619–1627. doi: 10.1007/s00520-011-1252-3. [DOI] [PubMed] [Google Scholar]
- 39.Flemming K. The use of morphine to treat cancer-related pain: A synthesis of quantitative and qualitative research. J Pain Symptom Manag. 2010;39(1):139–154. doi: 10.1016/j.jpainsymman.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 40.DeSanto-Madeya S, Bauer-Wu S, Gross A. Activities of daily living in women with advanced breast cancer. Oncology Nursing Forum. 2007;34(4):841–846. doi: 10.1188/07.ONF.841-846. [DOI] [PubMed] [Google Scholar]
- 41.Hopkinson J, Corner J. Helping patients with advanced cancer live with concerns about eating: a challenge for palliative care professionals. Journal of Pain & Symptom Management. 2006;31(4):293–305. doi: 10.1016/j.jpainsymman.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 42.Hopkinson JB. How people with advanced cancer manage changing eating habits. J Adv Nurs. 2007;59(5):454–462. doi: 10.1111/j.1365-2648.2007.04283.x. [DOI] [PubMed] [Google Scholar]
- 43.Balboni TA, Vanderwerker LC, Block SD, et al. Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. Journal of Clinical Oncology. 2007;25(5):555–560. doi: 10.1200/JCO.2006.07.9046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnson KS, Elbert-Avila KI, Tulsky JA. The influence of spiritual beliefs and practices on the treatment preferences of African Americans: a review of the literature. J Am Geriatr Soc. 2005;53(4):711–719. doi: 10.1111/j.1532-5415.2005.53224.x. [DOI] [PubMed] [Google Scholar]
- 45.Koenig HG. Religion and medicine IV: religion, physical health, and clinical implications. Int J Psychiatry Med. 2001;31(3):321–336. doi: 10.2190/X28K-GDAY-75QV-G69N. [DOI] [PubMed] [Google Scholar]
- 46.Puchalski CM. Spirituality in the cancer trajectory. Annals of Oncology. 2012 Apr;23(Suppl 3):49–55. doi: 10.1093/annonc/mds088. [DOI] [PubMed] [Google Scholar]
- 47.Puchalski CM. Integrating spirituality into patient care: an essential element of personcentered care. Polskie Archiwum Medycyny Wewnetrznej. 2013;123(9):491–497. [PubMed] [Google Scholar]
- 48.McCorkle R, Ercolano E, Lazenby M, et al. Self-management: Enabling and empowering patients living with cancer as a chronic illness. Cancer. 2011;61 doi: 10.3322/caac.20093. [DOI] [PMC free article] [PubMed] [Google Scholar]