Abstract
Reduced cardiovascular responses to psychological stressors have been found to be associated with both obesity and negative affect in adults, but have been less well studied in children and adolescent populations. These findings have most often been interpreted as reflecting reduced sympathetic nervous system response, perhaps associated with heightened baseline sympathetic activation among the obese and those manifesting negative affect. However, obesity and negative affect may themselves be correlated, raising the question of whether they both independently affect cardiovascular reactivity. The present study thus examined the separate effects of obesity and negative affect on both cardiovascular and skin conductance responses to stress (e.g., during a serial subtraction math task) in adolescents, while controlling for baseline levels of autonomic activity during rest. Both obesity and negative affect had independent and negative associations with cardiovascular reactivity, such that reduced stress responses were apparent for obese adolescents and those with high levels of negative affect. In contrast, neither obesity nor negative affect was related to skin conductance responses to stress, implicating specifically noradrenergic mechanisms rather than sympathetic mechanisms generally as being deficient. Moreover, baseline heart rate was unrelated to obesity in this sample, which suggests that heightened baseline of sympathetic activity is not necessary for the reduced cardiovascular reactivity to stress.
Keywords: Heart rate reactivity, Obesity, Negative affect
1. Introduction
The ability of the body to increase energy outlay under stress is an important adaptive process. In particular, in the well-functioning organism, heart rate increases under both physical and psychological stress (Rieger et al., 2014). Past research has indicated that certain characteristics of individuals are associated with a reduced ability to increase cardiac function under stress. One frequent finding is that individuals with a higher body mass index (BMI), a measure of general adiposity as indicated by weight in kilograms divided by height in meters squared, show lowered heart rate (HR) reactivity under conditions of psychological stress, such as increased mental workload (Carroll et al., 2008; Phillips et al., 2012; Phillips et al., 2013). One of the more prominent explanations suggested for this relationship to obesity has been a blunted sympathetic nervous system response (Carroll et al., 2008; Phillips, 2011; Phillips et al., 2013; Singh & Shen, 2013), specifically due to high basal cardiovascular activity, which could dysregulate beta- adrenergic receptor response (Singh & Shen, 2013; Phillips et al. 2012). Another explanation, possibly related to the first, lies in an obese individual’s higher level of chronic stress, which might result in impaired hypothalamic-pituitary-adrenal (HPA) axis activity and thus the body’s ability to maintain allostasis (Singh & Shen, 2013).
A second set of findings relates reduced cardiac activity under stress to negative affect, particularly depression and social inhibition (de Rooij, et al., 2009; Phillips, 2011; Phillips et al., 2013; Carroll et al., 2007). Such reduced reactivity has been associated with dysregulation and suboptimal functioning of the areas of the brain related to motivation, as similar studies indicate a blunted response to reward (Phillips et al., 2013). As with the blunted HR reactivity seen among the obese, blunted HR response in negative affect has been related to decreased beta adrenergic receptor responsiveness (Phillips et al. 2012), perhaps due to high basal sympathetic activity as evidenced by higher concentrations of plasma noradrenaline, and thus to a reduced capacity to respond to stress (Phillips et al., 2013; Yu et al., 2008). Gillespie et al. (2005) and Xu et al. (2011) suggest that adiposity, through a chain reaction of increased cytokines, decreased glucocorticoids, and increased cortisol concentrations, dysregulates the HPA axis, an impairment that is often associated with depression.
There appears to have been little attention to the possibility that these two correlates of reduced HR reactivity—obesity and negative affect—are themselves intertwined in their effects on HR reactivity. To our knowledge, there have been few studies that examined the relationship between obesity and negative affect. Leckie and Withers (1967) reported higher levels of depressed mood among the obese, and Pasco et al. (2013) also observed a positive correlation between BMI and negative affect (2013); see Preiss, Brennan, and Clarke (2013) for a recent review. In cultural beauty standards in America, the obese in particular are looked upon as not only being unattractive, but also are likely to be seen as lazy, less intelligent, and less motivated (Ayers, 2008; Xu et al., 2011; Puhl et al., 2013; Hebl et al., 2012; Bradley et al., 2008). Therefore, not surprisingly, persons of high body mass index, particularly the obese, are more likely to be depressed and socially inhibited due to social ostracization and bullying (Phillips et al., 2013; Xu et al., 2011; Bradley et al., 2008). Phillips (2011) investigated the effects of both BMI and depression on cardiovascular reactivity and found that when each was used as a covariate in the analysis of the effects of the other, both higher BMI and higher depression were associated with lower levels of reactivity. However, the relationship between depression ad obesity was not itself examined.
The question therefore arises whether high BMI and negative affect independently act to reduce heart rate reactivity, or whether they are both manifestations of essentially the same process. One purpose of the present investigation was to determine if these factors are in fact independent predictors of HR reactivity under psychological stress.
A second issue arises from the fact that studies of reduced heart rate reactivity associated with either high BMI or negative affect appear to have largely included only adults. Obesity rates in the United States have grown to alarming levels, as approximately one third of adults and 17% of children and adolescents in the general population are now obese (Ogden et al., 2012, 2014). Furthermore, this growth has been paralleled in the rising rates of psychological distress in adolescents, such as major depressive disorder (Twenge et al., 2010). Because childhood and adolescent obesity and psychological distress are currently of considerable concern in American society (Pasco et al., 2013; Ayers, 2008; Xu et al., 2011; Hebl et al., 2012), it is important to know whether the reduction of heart rate reactivity associated with obesity seen in adults is also observable in younger individuals. Working orking with adolescents approximately 13–16 years old, Barnes et al. (1998) studied the effects of central adiposity (waist-to-hip ratio) on reactivity of systolic and diastolic blood pressure, cardiac output, and peripheral resistance, but not heart rate. They found that when BMI was statistically controlled, higher levels of obesity were associated with greater blood pressure reactivity. Goldbacher, Matthews, and Salomon (2005) studied adolescents 14–16 years old and also found that when BMI was used as a covariate, another measure of central adiposity, higher waist circumference, was positively associated with greater systolic and diastolic blood pressure reactivity to stress. Interestingly, BMI itself was negatively associated with blood pressure response – patients with lower BMI values were more responsive. Heart rate was measured in this study, but results were not reported. Thus, the second purpose of this study was to investigate the interrelationships of negative affect and BMI on heart rate reactivity in adolescents aged 14–16.
A third question of interest is the generality of the reduced reactivity to stressors seen in obesity or negative affect. Increased cardiovascular activity in response to stress is a component of increased sympathetic nervous system activity and/or vagal withdrawal, responses that are adrenergically mediated, but increases in response to stress would also be expected in other aspects of sympathetic activity, including in skin conductance level, which is entirely under sympathetic control but is cholinergically mediated (Boucsein, 2012; Dawson, Schell, and Filion, 2007). The question thus arises as to whether the reduced reactivity seen in obesity and negative affect is limited to those sympathetic responses which are adrenergically mediated or whether it extends more broadly to include the skin conductance response.
The present study involved three research hypotheses. First, we predicted that the negative associations of HR reactivity to both BMI and negative affect seen in adults would also be found in adolescents. That is, we predicted that adolescents with higher BMI would have lower heart rate reactivity than those that have lower BMI, and that adolescents with higher negative affect would have lower heart rate reactivity than those with lower negative affect. Second, we predicted that that high BMI and negative affect influence HR reactivity independently of one another, although perhaps through the same mechanism. Finally, we predicted that the negative correlations of BMI and negative affect with HR reactivity would not be seen for skin conductance reactivity, since skin conductance is cholinergically mediated at the receptor site (Boucsin, 2014) and therefore presumably would not be affected by the reduced beta adrenergic receptor responsiveness (Phillips et al. 2012) thought to be responsible for the reduced HR reactivity seen in obesity and in negative affect.
2. Method
2.1 Participants
The participants in the present analyses were participants in a longitudinal twin study at the University of Southern California (Twin Study of Risk Factors for Antisocial Behavior - RFAB). The participants were selected on the basis of being twins. The RFAB is a longitudinal study of the interplay of genetic, environmental, social, and biological factors on the development of antisocial and aggressive behavior from childhood to young adulthood. Participating families were recruited from the Los Angeles community and the sample is representative of the ethnic and socio-economic diversity of the greater Los Angeles area. To date four waves of data have been collected and analyzed and the total sample contains 1,569 participants (780 twins and triplets). On the first assessment (Wave 1) the twins were 9–10 years old (N = 614, mean age = 9.59, s.d. = 0.58). On the second assessment (Wave 2), the twins were 11–13 years old (N = 445, mean age = 11.79, s.d. = 0.92). On the third assessment (Wave 3), the twins were 14–16 years old (N = 604, mean age = 14.82, s.d. = 0.83), and during Wave 4 the twins were 16–18 years old (N = 504, mean age = 17.22, s.d. = 1.23). Informed consent and assent were obtained from all participants. More detailed information regarding participant recruitment and design can be found elsewhere (Baker et al., 2002, 2006).
Analyses presented here are based on data collected during a single assessment when the participants were 14–16 years old (N = 490 with all necessary data, mean age = 14.6 years, s.d. = 0.56). The sample was composed of 51.1% females and 48.9% male and contained both monozygotic (MZ) and dizygotic (DZ) twins. 75% were twin pairs, with the remainder being singletons for which their co-twin’s data on obesity, affect or autonomic responding were not available. In spite of the sample being composed of twin pairs, the present analyses were based on individuals and did not examine twin correlations since these were not directly related to the primary research questions. As described in the analysis section below, hierarchical mixed-model analyses were used for all analyses to account for the non- independence of observations due to the paired nature of the sample.
2.2 Recording Autonomic Variables
2.2.1 Cardiovascular Responses
Heart rate (HR) was recorded using self-adhesive disposable electrocardiogram (ECG) electrodes. The electrode sites were cleaned with a cotton pad and 70% b/V isopropyl rubbing alcohol. Electrodes were then placed between the first and second ribs on either side of the chest. Alligator clips with 48″ lead wires were then attached to the tabs of the electrodes. The ECG signal was recorded using a James Long system electrocardiogram amplifier. Data were stored for off line analysis of HR during both resting states and during tasks.
2.2.2 Skin Conductance Level (SCL)
SCL was also measured using the James Long system. Silver-silver chloride electrodes were secured on the distal phalanges of the index and middle fingers of the participants’ non-dominant hands using adhesive electrode collars. The electrodes were then further secured with waterproof tape wrapped about the fingers. K-Y lubricating jelly was used as the conducting medium.
2.3 Tasks and Measures
Participants of this study visited the laboratory for a comprehensive assessment which included the psychophysiological recording of HR and SCL (both during resting states as well as during several tasks), in addition to interviews and questionnaire surveys about their behavior and affect. The present analyses are based on data taken from an initial Rest period and the Trier Social Stress Test (TSST; Kirschbaum et al., 1993), consisting of a mental arithmetic task and a speech task, as explained below. Among the interviews and surveys were questions pertaining to each participant’s body composition (height and weight—used to assess obesity) as well as their behavior and affect. The tasks and measures utilized in the analyses presented in this paper are described below. Other tasks included a measure of orienting to nonsignal auditory stimuli of various kinds, a go-no go reaction time task, and an oddball task for the measurement of cortical evoked potentials.
2.3.1. Rest
Prior to engaging in any tasks in the stress testing portion of the study, participants were instructed to sit and be as still as possible for 180 seconds while HR and SCL were recorded. Second by second values of HR and SCL were derived, from which average Resting HR and SCL were then calculated as baseline autonomic measures.
2.3.2 Math Stressor Task
Participants were asked to perform a mental arithmetic task by sequentially subtracting 13 from the number 1,023 for 180 s. Constant critical feedback was given during the task which required participants to restart the task if they responded incorrectly or too slowly. HR and SCL were recorded throughout the duration of the task at one-second intervals. Minute-by-minute averages for HR and SCL for the task were then calculated, and total average HR and SCL were also calculated.
2.3.3 Speech Stressor Task
The speech stressor task consisted of giving the participants the beginning of a story and giving them 180 s in which to prepare an exciting conclusion to the story. The participants then spoke their conclusions into a microphone in the presence of the experimenter for 180 s. The participants were told that their performance was being videotaped and that it would be reviewed for originality, excitingness, and overall speaking skills. HR and SCL were recorded throughout the duration of the task at one-second intervals. Minute-by-minute averages for HR and SCL for the preparation and speaking portion of the task were then calculated, and total average HR and SCL for each portion were also calculated.
2.4 Dependent and Predictor Variable Measurements
2.4.1. HR and SCL
Changes in HR and SCL between the rest period and Trier stressor tasks were computed, in order to be used as dependent variables in analyses. Average HR during rest was subtracted from average HR during the math task to determine each participant’s HR Reactivity to the math stressor, and average HR during rest was subtracted from average HR during the preparation portion of the speech stressor task to determine HR Reactivity to the speech stressor. HR during the preparation portion of the task was used since participants often fidgeted with their hands and used gestures during the speaking portion of the task, which could create artifacts in the HR and SCL recording. Similarly, average SCL during rest was subtracted from average SCL during math task to determine each participant’s SCL Reactivity in response to the math stressor, and average SCL during rest was subtracted from average SCL during the preparation portion of the speech task to determine each participant’s SCL Reactivity to the speech stressor.
2.4.2 Body Mass Index (BMI)
Height, weight, and age were documented to calculate BMI-z scores based on the Center for Disease Control (CDC) growth charts. These standard scores provide an inexpensive and noninvasive means of measuring obesity, and are adjusted for the participant’s age and gender (Heo et. al, 2014). This adjustment is important since a given BMI may or may not be indicative of overweight or obesity, given the subject’s gender and/or age. Based on the CDC cutoffs, less than 1% of our sample was underweight, 72% was of a healthy weight, 14% was overweight, and 13% was obese, an obesity rate slightly less than that of the general U.S. child and adolescent population of 16.9% (Ogden et al., 2012a, b).
2.4.3 Measures of negative affect
To assess negative affect, participants were asked to complete the Youth Self-Report (YSR) questionnaire, which contains 112 items using a three-point scale (0=absent, 1=occurs sometimes, and 2=occurs often) (Achenbach, 1991). The Internalizing subscale was used as the measure of negative affect, as it contains items reflecting anxiety, depression, social inhibition, and somatic concerns (e.g. “I feel too fearful or anxious, I feel unhappy, sad or depressed”; “I would rather be alone than with others” ; “I feel tired”.) Based on available normative data (Achenbach, 1991), our participants’ average Internalizing T scores (mean = 48.5, s.d. = 10.0) is very close to the reported normative mean (mean = 45.5, s.d. = 10.3).
2.5 Statistical Analysis
Simple Pearson Correlation analysis first used to evaluate relationships among measures of HR Reactivity, base level HR, BMI-z scores, and the YSR Internalizing scale scores, and among measures of SCL Reactivity, base level SCL, BMI-z scores, and the YSR Internalizing scores. Partial correlation coefficients were then calculated to assess the relationship between each predictor variable and HR or SCL Reactivity with the other predictors statistically controlled. Finally and most definitively, because the participant sample consisted primarily of non-independent observations (i.e., twin pairs), Mixed Model analysis (SPSS 19) was used to asses dependence of observations.
3. Results
3.1 Descriptive Statistics
Descriptive statistics (means and standard deviations) for all variables used in the present analyses are shown in Table 1.
Table 1.
Descriptive Statistics (Mean and s.d.) for Body Mass Index (BMI), Youth Self-Report (YSR) Internalizing, Heart Rate (HR), and Skin Conductance (SCL) Variables (N=490)
| Variable | Mean | s.d. |
|---|---|---|
| BMI scores | 22.32 | 4.58 |
| BMI z-scores | 0.50 | 0.95 |
| YSR Internalizing scores | 10.66 | 7.72 |
| YSR Internalizing T scores | 48.50 | 10.02 |
| Resting HR (BMP) | 75.83 | 11.34 |
| HR Reactivity, math task (BMP) | 6.84 | 8.58 |
| HR Reactivity, speech task (BMP) | 5.58 | 8.44 |
| Resting SCL (μS) | 8.70 | 4.11 |
| SCL Reactivity, math task (μS) | 3.40 | 2.24 |
| SCL Reactivity, speech task (μS) | 3.32 | 2.23 |
Notes: BMP = beats per minute; μS = microsiemens
3.2 Reactivity to Stressors
To verify that both the math and speech stressors produced significant increases in HR and SCL, repeated measures t tests were carried out on both variables for both stressors. For HR, both math and speech stressors produced significant increases (for math, mean = 6.84 beats per minute, t = 17.66, df = 489, p < .001, and for speech mean = 5.58 BMP, t = 14.63, df = 489, p < .001.) For SCL, both stressors also produced significant increases (for math, mean = 3.40 microseimens, t = 31.06, df = 489, p < .001, and for speech, mean = 3.23 microseimens, t = 32.07, df = 489, p < .001.)
3.3 Correlations among HR reactivity, base level HR, BMI, and YSR Internalizing
To investigate whether the negative relationships of BMI and YSR Internalizing score with HR reactivity seen in adults also extended to adolescents, simple Pearson’s correlations were first computed. We also examined the correlation between HR reactivity during the math and speech stressors and Resting HR, since these two may be related. The Law of initial values (LIV) relating HR reactivity under stress to base level HR is complex, but when base level HR is high, negative correlations may be seen (Berntson, Cacioppo, & Quigley, 1991; Filipovsky, Ducimetiere, & Safar, 1992). Given that LIV effects might have reduced HR reactivity in individuals whose base level was quite high, a negative correlation between Resting HR and HR Reactivity was possible, and some investigators (e.g. Phillips et al. 2012) have found Resting HR to be higher among the obese. As can be seen in Table 2, Resting HR and HR Reactivity to both stressors were in fact negatively correlated for these 14–16 year old participants.
Table 2.
Correlations among HR Reactivity during Trier Stressors and Predictor Variables (Resting HR, BMI, YSR Internalizing)
| Resting HR | BMI z Score | YSR Internalizing | |
|---|---|---|---|
| HR Reactivity, math | −.22 *** | −.23*** | −.16 *** |
| HR Reactivity, speech | −.13** | −.13** | −.11 * |
| Resting HR | .01 | .10 * | |
| BMI z score | .09 m |
Notes: df = 488
p < .05
p < .005
p < .001 m p < .0
As expected, HR Reactivity scores during the math stressor were negatively correlated with Resting HR, with BMI z-scores, and with YSR Internalizing scores. The predictor variables were also intercorrelated in some cases, with Resting HR positively correlated with YSR Internalizing, and the positive correlation between BMI z-scores and YSR Internalizing approaching significance. To test whether BMI-z scores, Resting HR, and YSR Internalizing scores independently predicted HR Reactivity during the math stressor when the other factors were controlled, partial correlations were next computed. Controlling for Resting HR and YSR Internalizing, BMI-z scores remained significantly and inversely correlated to Reactivity scores (r = −.22, df = 486, p < .001). HR Reactivity also remained significantly correlated with both YSR Internalizing (r = −.13, df = 486, p = .004) and Resting HR (r =−.22, df = 486, p < .001) when other factors were controlled.
HR Reactivity during the speech task was significantly less than that during the math task (t = 4.04, df = 489, p < .001), indicating that this was the less stressful of the two tasks. Perhaps because HR Reactivity was lower, negative correlations between Reactivity, Resting HR, BMI z-scores, and YSR Internalizing scores, while still significant, were lower in magnitude than they were for the math stressor (see Table 2). As for the math stressor task, partial correlations between each predictor and HR Reactivity to the speech stressor were computed, controlling for other predictors. Controlling for Resting HR and YSR Internalizing, BMI-z scores remained significantly and inversely correlated to HR Reactivity scores (r = −.12, df = 486, p < .01). HR Reactivity also remained significantly correlated with Resting HR (r = −.12, df = 486, p < .01) when other factors were controlled. However, the partial correlation of HR Reactivity to the speech stressor and YRS Internalizing was only of marginal significance (r = −.09, p < .06).
3.4 Mixed Model Analysis
3.4.1 Mixed Model Analysis of HR Reactivity to the Math Stressor
In order to account for the dependence of observations (twin pairs) in this sample, mixed-model analyses were next used to confirm the prediction of HR Reactivity during the stressor by Resting HR, BMI, and YSR Internalizing scores. Given the moderate correlation between twins for the HR Reactivity scores (r = .32, df = 182, p < 0.001 for the Math stressor), mixed model approaches are important in evaluating the relationships of HR Reactivity to the predictors. Therefore, to test the independence of each of the three predictors of HR response to stress, a mixed model multiple regression analysis was performed (SPSS linear regressions mixed model), where each predictor was evaluated by entering it last in the regression equation and comparing model fit. Consistent with the partial correlation analysis, mixed model multiple regression results showed that Resting HR, BMI-z scores, and YSR Internalizing scores each showed significant and independent contributions to HR Reactivity, as shown in Table 3.
Table 3.
Mixed Model Multiple Regression Analysis of HR Reactivity during Math Task Predicted by Resting HR, BMI z scores, and YSR Internalizing Scores
| Predictor | Beta | Standardized Beta (se) | t | df | p |
|---|---|---|---|---|---|
| Resting HR | −0.18 | −.23 (0.04) | −5.49 | 472.14 | <.001 |
| BMI z score | −1.69 | −.19 (0.05) | −4.24 | 436.60 | <.001 |
| YSR Internalizing | −0.09 | −.11 (0.04) | −2.60 | 460.65 | .01 |
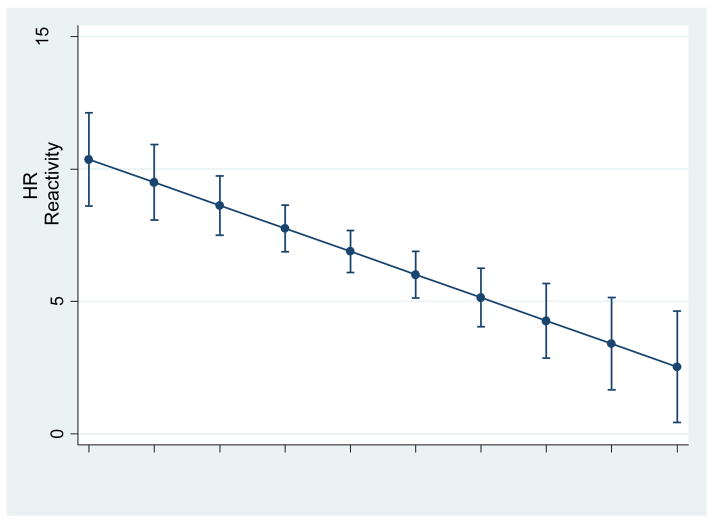
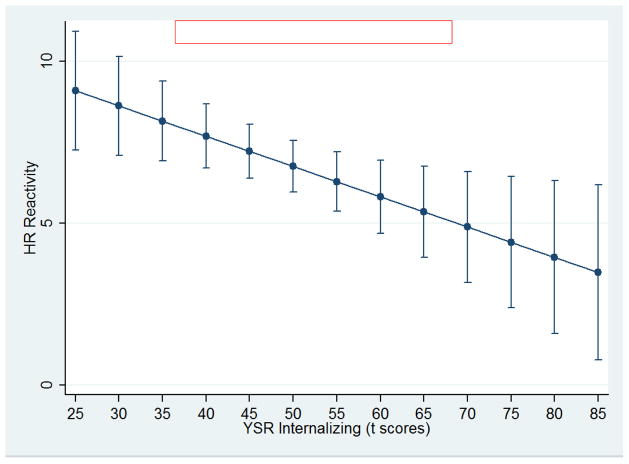
The regression line relating HR Reactivity under stress to BMI-z scores is presented graphically in Figure 1, which also shows the 95% confidence intervals of the errors of estimate at various points on the line, and the regression line relating HR Reactivity to YSR Internalizing scores is presented graphically in Figure 2, which also shows the 95% confidence intervals for the errors of estimate. These regression lines are based on the regression coefficients for the regression of HR Reactivity on BMI-z scores and YSR Internalizing scores respectively taken from the multiple regression analysis. AS Figures 1 and 2 indicate, there is an inverse relationship between HR Reactivity with both BMI and the YSR Internalizing scores. That is, lower HR Reactivity is associated with higher levels of obesity and YSR Internalizing problems in these adolescent youth.
Figure 1.
Heart rate Reactivity in beats per minute during stress predicted from BMI z scores, with 95% confidence intervals of predicted values
Figure 2.
Heart rate Reactivity in Beats per minute during stress predicted from YSR Internalizing scores, with 95% confidence intervals of predicted values
3.4.2 1Mixed Model Analysis of HR Reactivity to the Speech Stressor
A mixed model analysis of regression for the speech stressor task using resting HR, BMI z-scores, and YSR Internalizing scores as predictors was also conducted. Consistent with the results for the math stressor, all three predictors were all found to be independently inversely related to HR reactivity, as seen in Table 4. However, the level of significance for each predictor is for the speech stressor lower than for the math stressor in each case, with the regression coefficient for BMI z-scores being of only marginal significance (p = .06)
Table 4.
Mixed Model Multiple Regression Analysis of HR Reactivity during Speech Task Predicted by Resting HR, BMI z scores, and YSR Internalizing Scores
| Predictor | Beta | Standardized Beta (se) | t | df | p |
|---|---|---|---|---|---|
| Resting HR | −0.09 | −.13 (0.04) | −3.01 | 433.06 | <.005 |
| BMI z score | −0.73 | −.08 (0.40) | −1.89 | 399.14 | .06 |
| YSR Internalizing | −0.09 | −.10 (0.04) | −2.43 | 419.88 | .02 |
3.5 SCL
Next, a parallel analysis to that carried out for HR was performed using change in skin conductance level as a measure to examine whether or not resting skin conductance levels, BMI z-scores and YSR Internalizing scores affected sympathetic nervous system responses generally or whether their effects were specific to cardiac reactivity. Pearson’s correlation analysis revealed no correlations even approaching significance between SCL Reactivity, Resting SCL, BMI z-scores, or YSR Internalizing scores for either the math or the speech stressors, although both stressors produced significant reactivity in SCL (significantly higher SCL during the stressor than during rest. Furthermore, mixed model multiple regression analysis also indicated that base SCL, BMI-z scores and YSR Internalizing behaviors did not significantly predict skin conductance Reactivity.
4. Discussion
One of the primary objectives of this study was to observe whether obesity and YSR Internalizing scores act independently of one another to affect cardiovascular stress response. While one field of study has found that a blunted stress response was observed in more obese individuals (Carroll et al., 2008; Phillips, 2011; Phillips et al., 2013; Singh & Shen, 2013; Salomon et al, 2009), and another field has found the same negative relationship between depression, internalizing behaviors or loneliness and stress response (Cacioppo et al., 2002; Chida & Hamer, 2008; Hawkley et al., 2003; Phillips, 2011; Phillips et al., 2013; Spies et al. 2011; Ruttle et al. 2011), the activity of both of these factors collectively, and whether they work independently of one another to reduce cardiac response to stress, has not yet been observed. In addition, taking the Law of Initial Values (LIV) into account, we have also considered the possibility that Resting HR could itself be related to reduced cardiac reactivity, as well as to obesity and YSR Internalizing, and consequently could influence the relationship of both YSR Internalizing and obesity to an individual’s stress response.
Consistent with our hypothesis, our first primary finding was that Resting HR, BMI-z scores, and YSR Internalizing behaviors all independently work to reduce cardiac reactivity to stress. This is supported by partial correlation analysis, which indicated that each of the factors has a significant influence in an individual’s cardiac response to stress when the effect of other factors are controlled. Furthermore, the independence of the effects of Resting HR, BMI-z, and YSR Internalizing scores in reducing cardiac stress response is reinforced by the multiple regression analysis, which adjusted for the fact that our participant sample was composed largely of twins, and which indicated that each of the three factors separately was predictive of cardiac reactivity.
Our second principle finding was that the effects of BMI-z and YSR Internalizing on cardiac reactivity in adults can also be seen in adolescent youth. The dominant interpretation of this finding has been one of reduced sympathetic system activity, with a high level of basal HR acting to reduce beta-adrenergic receptor sensitivity, an example of law of initial value action (Carroll et al., 2008; Phillips et al., 2013; Singh & Shen, 2013). Previous studies have found elevated basal HR associated with obesity in children and adolescents (Baba et al. 2007; Jiang et al., 1995; Sorof et al., 2002) and in adults (Frank et al. 1986; Lee et al., 2014; Phillips et al., 2012), although there have also been negative findings (Carroll et al., 2008; Kopelman, 2000). Basal HR has also been found to be elevated in depression (Moser et al., 1996) in adults. We did not find a positive relationship between BMI and Resting HR in these 14–16 year old children, although a small but significant positive correlation between Resting HR and YSR internalizing scores was seen. Therefore, the negative relationship between BMI and HR reactivity in these participants is not dependent upon higher basal HR. This is consistent with Carroll et al. (2008) who found that obesity was associated with reduced HR reactivity but not with higher basal HR, and that reduced reactivity could predict the likelihood of becoming obese in the next in the next five years in both adolescents and adults who were not initially obese; therefore, it seems possible that the reduced HR reactivity in our participants associated with obesity may predict in turn higher basal HR at a later time. High basal HR and obesity are both associated with lowered HR reactivity, but these two effects appear to be independent of one another.
Our third dominant finding was that skin conductance reactivity to stress is not affected by BMI-z or YSR Internalizing scores, which suggests that the reduced sympathetic activity to stress reflected by the reduced HR response may be specific to noradrenergically mediated responses, since the skin conductance response, unique among sympathetic responses, is entirely cholenergically mediated (Boucsein, 2012). This is consistent with the suggestion by Spraul et al. (1993) that the blunted cardiovascular response is associated with a blunted noradrenergic response to stress. Previous studies have reported that, in moments of acute stress, noradrenergic activity promotes reorganization of neural resources to areas of the brain that are involved in attentional reorienting, vigilant perceptual intake, and autonomic-neuroendocrine control (Hermans et al., 2011). The reduced cardiac response may thus be reflective of a more general reduced ability to respond to task demands.
The fact that these relationships exist between reduced HR Reactivity to these fairly mild laboratory stressors and obesity and internalizing in adolescents, similar to those seen in adults, and the finding that obesity five years later may be predicted by reduced HR Reactivity (Carroll et al., 2008), make these findings of potential clinical interest. Both obesity and depression are significant health problems in our society (Ogden et al., 2012, 2014; Twenge et al., 2010; Kessler et al., 2005). Any early predictors of these disorders are potentially of value in identifying persons at risk and making prophylactic treatment possible, particularly a predictor such as HR Reactivity to a mild stressor which can be easily, inexpensively, and noninvasively measured.
Directions for further future research would include determining how early in life these relationships begin to appear. At what point in life is reduced HR reactivity associated with obesity and/or negative affect, or of particular importance, at what point is it predictive of these outcomes? Is reduced cardiac reactivity a marker for later health consequences, observable before the onset of negative affect or the beginning of obesity? If it does indeed reflect a general reduced ability to respond to task demands, particularly stressful task demands, can this be detected in time to take corrective action while the child is still young? In the case of obesity and depression, does significant weight loss or successful long-term treatment of depression normalize cardiac reactivity as well?
Limitations of the present study are that we only used one stressor that produced a strong HR response and one that produced a somewhat weaker response. But other investigators using such stressors as the Stroop task (Phillips et al., 2012; de Rooji et al., 2010), mirror tracing (Phillips et al., 2012; de Rooji et al., 2010) and speech (Phillips et al., 2012; de Rooji, et al., 2010 have found similar results. Our results do suggest that the stronger the stressor, and thus the greater the HR Reactivity that would be expected, the stronger will be the relationship seen between reduced HR Reactivity and obesity and negative affect.
Highlights.
Heart rate reactivity during a math task among adolescents was studied.
Effects of base level heart rate, body mass index, and Internalizing were assessed.
Heart reactivity was negatively related to base HR, BMI, and Internalizing.
Basal HR, BMI, and Internalizing all independently predicted low reactivity.
Lowered reactivity in skin conductance response was not found.
Acknowledgments
The authors wish to thank Nicholas Jackson for assistance with statistical analysis, and all of the twins for their participation. This research was supported by an NIMH grant to Laura Baker, principal investigator (MH058354).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Integrative Guide for the 1991 CBCL 14–18, YSR and TRF Profiles. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Ayers SF. Obesity bias and adolescents’ perceptions. Journal of Physical Education, Recreat & Danc. 2008;82(6):8. [Google Scholar]
- Baba R, Koketsu M, Nagashima M, Inasaka H, Yoshinaga M, Yokota M. Adolescent obesity adversely affects blood pressure and resting heart rate. Circulation J. 2007;71:722–726. doi: 10.1253/circj.71.722. [DOI] [PubMed] [Google Scholar]
- Baker LA, Jacobson KC, Raine A, Lozano DI, Bezdjian S. Genetic and environmental bases of childhood antisocial behavior: A multi-informant twin study. J Abnorm Psychol. 2002;116(2):219–235. doi: 10.1037/0021-843X.116.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker LA, Barton M, Lozano DI, Raine A, Fowler JH. The Southern California twin register at the University of Southern California. Twin Res Hum Genetics. 2006;9(6):933–940. doi: 10.1375/183242706779462912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes VA, Treiber FA, Davis H, Kelley TR, Strong WB. Central adiposity and hemodynamic functioning at rest and during stress in adolescents. International Journal of Obesity. 1998;22(11):1079–1983. doi: 10.1038/sj.ijo.0800730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berntson GG, Cacioppo JT, Quigley KS. Autonomic determinism: the modes of autonomic control, the doctrine of autonomic space, and the laws of autonomic constraint. Psychol Rev. 1991;98(4):459–487. doi: 10.1037/0033-295x.98.4.459. [DOI] [PubMed] [Google Scholar]
- Boucsein W. Electrodermal activity. 2. New York: Springer; 2012. [Google Scholar]
- Bradley RH, Houts R, Nader PR, O’Brien M, Belsky J, Crosnoe R. The relationship between body mass index and behavior in children. J Pediatr. 2008;153:629–634. doi: 10.1016/j.jpeds.2008.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalsky RB, Malarkey WB, VanCauter E, Berntson GG. Loneliness and health: Potential mechanisms. Psychosom Med. 2002;64:407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Carroll D, Phillips AC, Hunt K, Der G. Symptoms of depression and cardiovascular reactions to acute psychological stress: Evidence from a population study. Biol Psychol. 2007;75:68–74. doi: 10.1016/j.biopsycho.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Carroll D, Phillips AC, Der G. Body mass index, abdominal adiposity, obesity, and cardiovascular reactions to psychological stress in a large community sample. Psychosom Med. 2008;70:653–660. doi: 10.1097/PSY.0b013e31817b9382. [DOI] [PubMed] [Google Scholar]
- Chida Y, Hamer M. Chronic psychosocial factors and acute physiological responses to laboratory-induced stress in healthy populations: A qualitative review of 30 years of investigations. Psychol Bull. 2008;134:829–885. doi: 10.1037/a0013342. [DOI] [PubMed] [Google Scholar]
- Dawson ME, Schell AM, Filion DL. The electrodermal system. In: Cacioppo JT, Tassinary LG, Berntson GG, editors. Handbook of psychophysiology. 3. New York, NY: Cambridge University Press; 2007. pp. 159–181. [Google Scholar]
- de Rooij SR, Schene AH, Phillips DI, Roseboom TJ. Depression and anxiety: Associations with biological and perceived stress reactivity to psychological stress protocol in a middle-aged population. Psychoneuroendo. 2010;35:866–77. doi: 10.1016/j.psyneuen.2009.11.011. [DOI] [PubMed] [Google Scholar]
- Filipovsky J, Ducimetiere P, Safar ME. Prognostic significance of exercise blood pressure and heart rate in middle-aged men. Hypertension. 1992;20:333–339. doi: 10.1161/01.hyp.20.3.333. [DOI] [PubMed] [Google Scholar]
- Frank S, Colliver JA, Frank A. The electrocardiogram in obesity: Statistical analysis of 1,029 patients. J Am Coll Cardiol. 1986;7(2):295–299. doi: 10.1016/s0735-1097(86)80494-6. [DOI] [PubMed] [Google Scholar]
- Gillespie CF, Nemeroff CB. Hypercortisolemia and depression. Psychosom Med. 2005;S67:26–28. doi: 10.1097/01.psy.0000163456.22154.d2. [DOI] [PubMed] [Google Scholar]
- Goldbacher EM, Matthews KA, Salomon K. Central adiposity is associated with cardiovascular reactivity to stress in adolescents. Health Psychology. 2005;24(4):375–384. doi: 10.1037/0278-6133.24.4.375. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG, Cacioppo JT. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. J Pers Soc Psychol. 2003;85:105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- Hebl MR, Ruggs EN, Singletary SL, Beal DJ. Perceptions of obesity across the lifespan. Obesity. 2012;15(2):846–852. doi: 10.1038/oby.2008.458. [DOI] [PubMed] [Google Scholar]
- Heo M, Wyle-Rosett J, Pietrobelli A, Kabat GC, Rohan TE, Faith MS. U.S. pediatric population-level associations of DXA-measured percentage of body fat with four BMI metrics with cut-offs. Int J Obesity. 2014;38:60–68. doi: 10.1038/ijo.2013.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermans EJ, van Marle HJF, Ossewaarde L, Henckens MJAG, Qin S, van Kesteren MTR, Schoots VC, Cousijn H, Rijpkema M, Ostenveld R, Fernandez G. Stress-related noradrenergic activity prompts large-scale neural network reconfiguration. Science. 2011;334:1151–1153. doi: 10.1126/science.1209603. [DOI] [PubMed] [Google Scholar]
- Jiang X, Srinivasan SR, Urbina E, Berenson GS. Hyperdynamic circulation and cardiovascular risk in children and adolescents: The Bogalusa heart study. Circulation. 1995;91:1101–1106. doi: 10.1161/01.cir.91.4.1101. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke KM, Hellhammer DH. The ‘Trier Social Stress Test’—a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28(1–2):76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- Kopelman PG. Obesity as a medical problem. Nature. 2000;404:635–643. doi: 10.1038/35007508. [DOI] [PubMed] [Google Scholar]
- Lee JF, Harrison ML, Christmas KM, Kim K, Hurr C, Matthew Brothers R. Elevated resting heart rate and reduced orthostatic tolerance in obese humans. Clin Auto Res. 2014;24:39–46. doi: 10.1007/s10286-013-0222-x. [DOI] [PubMed] [Google Scholar]
- Leckie EV, Withers RFJ. Obesity and depression. J Psychosom Res. 1967;11:107–115. doi: 10.1016/0022-3999(67)90063-3. [DOI] [PubMed] [Google Scholar]
- Moser M, Lehofer M, Hoehn-Saric R, McLeod DR, Hildebrant G, Steinbrenner B, Voica M, Leibman P, Zapotoczky HG. Increased heart rate in depressed subjects in spite of unchanged autonomic balance? J Affect Disorders. 1996;48:115–124. doi: 10.1016/s0165-0327(97)00164-x. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. J Amer Med Assoc. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the Unied Sttes, 2011–2012. J Amer Med Assoc. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasco JA, Williams LJ, Jacka FN, Brennan SL, Berk M. Obesity and the relationship with positive and negative affect. Aust NZ J Psychiat. 2013;45(50):477–482. doi: 10.1177/0004867413483371. [DOI] [PubMed] [Google Scholar]
- Phillips AC. Blunted cardiovascular activity relates to depression, obesity, and self-reported health. Biol Psychol. 2011;86:106–113. doi: 10.1016/j.biopsycho.2010.03.016. [DOI] [PubMed] [Google Scholar]
- Phillips AC, Ginty AT, Hughes BM. The other side of the coin: Blunted cardiovascular and cortisol reactivity are associated with negative health outcomes. Int J Psychophysiol. 2013;90:1–7. doi: 10.1016/j.ijpsycho.2013.02.002. [DOI] [PubMed] [Google Scholar]
- Phillips AC, Roseboom TJ, Carroll D, Rouu SR. Cardiovascular and cortisol reactions to acute psychological stress and adiposity: Cross-sectional and prospective associations in the Dutch famine birth cohort study. Psychosom Med. 2012;74:669–210. doi: 10.1097/PSY.0b013e31825e3b91. [DOI] [PubMed] [Google Scholar]
- Preiss K, Brennan L, Clarke D. A systematic review of variables associated with the relationship between obesity and depression. Obes Rev. 2013;14:906–918. doi: 10.1111/obr.12052. [DOI] [PubMed] [Google Scholar]
- Puhl R, Peterson JL, Luedicke J. Fighting obesity or obese persons? Public perceptions of obesity-related health messages. Int J Obesity. 2013;37:774–782. doi: 10.1038/ijo.2012.156. [DOI] [PubMed] [Google Scholar]
- Rieger A, Stoll R, Kreuzfeld S, Behrens K, Weippert M. Heart rate and heart rate variability as indirect markets of surgeons’ intraoperative stress. Int Arch Occ Env Hea. 2014;87:165–174. doi: 10.1007/s00420-013-0847-z. [DOI] [PubMed] [Google Scholar]
- Ruttle PL, Shirtcliff EA, Serbin LA, Fisher DB, Stack DM, Schwartzman AE. Disentangling psychobiological mechanisms underlying internalizing and externalizing behaviors in youth: longitudinal and concurrent associations with cortisol. Horm Behav. 2011;59:123–132. doi: 10.1016/j.yhbeh.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon K, Clift A, Karlsdottir M, Rottenberg J. Major depressive disorder is associated with attenuated cardiovascular reactivity and impaired recovery among those free of cardiovascular disease. Health Psychol. 2009;28:157–165. doi: 10.1037/a0013001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh K, Shen BJ. Abdominal obesity and chronic stress interact to predict blunted cardiovascular reactivity. Int J Psychophysiol. 2013;90:73–79. doi: 10.1016/j.ijpsycho.2013.03.010. [DOI] [PubMed] [Google Scholar]
- Sorof JM, Poffenbarger T, Franco K, Bernard L, Portman RJ. Isolated systolic hypertension, obesity, and hyperkinetic hemodynamic states in children. J Pediatr. 2002;140:660–666. doi: 10.1067/mpd.2002.125228. [DOI] [PubMed] [Google Scholar]
- Spies LA, Margolin G, Susman EJ, Gordis EB. Adolescents’ cortisol reactivity and subjective distress in response to family conflict: The moderating role of internalizing symptoms. J Adolescent Health. 2011;49:386–392. doi: 10.1016/j.jadohealth.2011.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spraul M, Ravussin E, Fontvielle AM, Rising R, Larson DE, Anderson EA. Reduced sympathetic nervous activity: A potential mechanism predisposing to body weight gain. J Clin Invest. 1993;92:1730–1735. doi: 10.1172/JCI116760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM, Gentile B, DeWall CN, Ma D, Lacefield K, Schurtz DR. Birth cohort increases in psychopathology among young Americans, 1938–2007: A cross-temporal meta-analysis on the MMPI. Clin Psychol. 2010;30:145–154. doi: 10.1016/j.cpr.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Xu Q, Anderson D, Lurie-Beck J. The relationship between abdominal obesity and depression in the general population: A systematic review and meta-analysis. Obes Res, Clin Pract. 2011;5:267–278. doi: 10.1016/j.orcp.2011.04.007. [DOI] [PubMed] [Google Scholar]
- Yu BH, Kang EH, Ziegler MG, Mills PJ, Dimsdale JE. Mood states, sympathetic activity, and in vivo beta-adrenergic receptor function in a normal population. Depress Anxiety. 2008;25(7):559–564. doi: 10.1002/da.20338. [DOI] [PMC free article] [PubMed] [Google Scholar]