Abstract
Background
Suicidal ideation is the most proximal risk factor for suicide and can indicate extreme psychological distress; identification of its predictors is important for possible intervention. Depression and stressful or traumatic life events (STLEs), which are more common among HIV-infected individuals than the general population, may serve as triggers for suicidal thoughts.
Methods
A randomized controlled trial testing the effect of evidence-based decision support for depression treatment on antiretroviral adherence (the SLAM DUNC study) included monthly assessments of incident STLEs, and quarterly assessments of suicidal ideation (SI). We examined the association between STLEs and SI during up to one year of follow-up among 289 Southeastern US-based participants active in the study between 7/1/2011 and 4/1/2014, accounting for time-varying confounding by depressive severity with the use of marginal structural models.
Results
Participants were mostly male (70%) and black (62%), with a median age of 45 years, and experienced a mean of 2.36 total STLEs (range: 0–12) and 0.48 severe STLEs (range: 0–3) per month. Every additional STLE was associated with an increase in SI prevalence of 7% (prevalence ratio (PR) (95% confidence interval (CI)): 1.07 (1.00, 1.14)), and every additional severe STLE with an increase in SI prevalence of 19% (RR (95% CI): 1.19 (1.00, 1.42)).
Limitations
There was a substantial amount of missing data and the exposures and outcomes were obtained via self-report; methods were tailored to address these potential limitations.
Conclusions
STLEs were associated with increased SI prevalence, which is an important risk factor for suicide attempts and completions.
Keywords: stress, trauma, suicidal ideation, depression, HIV
INTRODUCTION
Suicidal ideation (SI), whether passive (thoughts that life is not worth living or that an individual wishes to be dead) or active (thoughts of ending one’s life with or without a plan),1 is one of the strongest and most proximal risk factors for suicide attempts and deaths by suicide. SI is strongly associated with depression,2 and both SI and depression are more common among persons with chronic diseases, such as HIV, than among the general population.3–5 A population of persons with both HIV and depression, therefore, may be at particularly high risk for experiencing SI. Identification of risk factors and triggers for SI in this population would allow for targeted interventions aimed at reducing the incidence of SI. This could help prevent some suicide attempts and deaths by suicide; however, the majority of the benefit of preventing SI would be in preventing or alleviating the potential extreme psychological distress that can come along with it.
Stressful or traumatic life events (STLEs), which are common among persons with HIV,6–8 may trigger suicidal thoughts and lead to an increase in SI in HIV-infected populations with depression already susceptible to such thoughts. STLEs include events related to relationship changes; estrangement from family; health concerns; death or illness of family or friends; financial, legal, or employment difficulties; safety concerns; and life transitions. The high burden of STLEs in populations of HIV-infected adults has been demonstrated in prior studies. HIV-infected participants in the Coping with HIV/AIDS in the Southeast (CHASE) study reported medians of nine incident stressful events and three incident severely stressful events over two years of follow-up.8 A secondary, cross-sectional analysis of data from a randomized trial found HIV-infected participants at 13 clinical sites throughout the US experienced a mean of 5.6 STLEs per month; financial problems were the most common STLE, followed by unemployment.9 A small, cross-sectional study of 105 HIV-infected men and women in a southern US state found that participants had experienced a mean of 3.15 STLEs in the prior six months.10
These and other studies among persons with HIV have identified associations between STLEs and negative clinical and behavioral outcomes, such as decreased medication adherence, virologic failure, and increased sexually risky behavior, but SI as an outcome has not been examined previously in this population. While a relationship between STLEs and increased SI has been found in other studies, this has mainly been studied among children or adolescents, and methodological differences have led to varying results and conclusions.11–13 No existing studies have examined this relationship among adults with both HIV and depression. The current study was carried out to examine the association between STLEs and SI over one year of follow-up among adults in the Southeastern US with HIV and depression while accounting for time-varying confounding of the association by depressive severity.
METHODS
Study Sample
Data for this study came from the Strategies to Link Antidepressant and Antiretroviral Management at Duke University, the University of Alabama-Birmingham, Northern Outreach Clinic (Henderson, NC), and the University of North Carolina-Chapel Hill (SLAM DUNC) Study, a randomized, controlled trial testing the effect of evidence-based decision support for depression treatment on ARV adherence, which has been described previously.14 The study population is made up of adult (age 18–65 years) HIV-infected patients with depression who attended the infectious disease clinics at Duke University; the University of Alabama at Birmingham (UAB); Northern Outreach Clinic (NOC) in Henderson, North Carolina; and the University of North Carolina at Chapel Hill (UNC). The present analysis is restricted to participants under observation between July 1, 2011 and March 31, 2014 (n=289). This time period corresponds to when data on STLEs were collected. Participants were followed for up to 12 months, with brief monthly contact for completion of antiretroviral medication pill counts and assessment of STLEs, and longer quarterly interviews to assess other outcomes. All study procedures were approved by the Institutional Review Boards at UNC, Duke University, and UAB.
Measures
Suicidal Ideation
SI was measured with the Hamilton Rating Scale for Depression (HAM-D) during telephone interviews conducted at enrollment and at three, six, nine, and twelve months post-enrollment. The HAM-D, the most widely used depressive severity measure in research settings, consists of 17 open-ended sections assessing different facets of depressive symptoms experienced during the past seven days.15–17 The third section addresses SI by asking whether the individual has 1) had thoughts that life is not worth living, 2) had thoughts that s/he would be better off dead, 3) had thoughts of hurting or killing himself/herself, and/or 4) actually tried to hurt or kill himself/herself. Additional probes were asked based on the participant’s responses to these questions. One score is obtained from the four questions and additional probes of the SI section, and ranges from 0–4 as follows: (0): no symptoms; (1): feels that life is not worth living; (2): wishes that s/he were dead, or had thoughts about hurting self; (3): suicidal ideas of gesture (has a plan, or began suicide attempt but stopped); (4): a suicide attempt during the past week. As our focus was ideation, we did not include any scores of 4 as SI (there were no suicide attempts among SLAM DUNC participants). Responses falling between two scores were scored conservatively (given the lower score) by the interviewers. Scores were dichotomized to indicate any suicidal ideation (score >0) vs. none (score of 0).
Stressful or Traumatic Life Events
STLEs were assessed during monthly telephone calls with participants using a modified version of the Life Events Survey (LES).10,18 Only those events from the LES considered moderately or severely stressful based on prior research are included in this assessment.19,20 Participants were asked whether they had experienced any of 46 events, from within nine different categories, during the prior month. STLE categories were: 1) romantic relationship changes; 2) estrangement from family; 3) death or major illness of a family member or close friend; 4) major illness, injury, or hospitalization; 5) employment difficulties; 6) financial difficulties; 7) legal difficulties; 8) life transitions; 9) safety concerns. It was not required that an event was newly reported; STLEs here therefore capture both acute events and chronic, ongoing stressors. The number of STLEs reported in the three months prior to each SI measurement were summed to create a continuous count variable. In instances where more than three STLE measurements took place in those three months, the three most recent measurements were used, since the quarterly interviews were designed to cover that period. Additionally, based on prior work,8 STLEs limited to the most severe events (divorce or separation, death or major illness of an immediate family member, major financial problems, time in jail, and sexual and physical assault) were combined to create both continuous (number of severe events) and dichotomous (any vs. none) variables.
Additional Covariates
Depressive severity was measured with the HAM-D15–17 at baseline and every three months thereafter, during scheduled, telephone-based interviews. Scoring of the HAM-D ranges from 0 to 50;16 however, scores were recalculated to exclude the SI section, resulting in scores ranging from 0 to 46. Coding of scores was kept continuous to retain information.
Other covariates used in the analysis were age, sex, drug and/or alcohol abuse or dependence, HIV-related physical symptoms, mental health functioning, CD4 count, psychiatric comorbidities, HIV-care self-efficacy, stress coping style, and employment status. Sex and age were assessed at study enrollment. Drug and alcohol dependence and abuse were assessed at baseline and at six- and twelvemonth follow-ups with the alcohol and substance dependence and abuse sections of the Mini International Neuropsychiatric Interview (MINI), a widely used psychiatric diagnostic instrument. A single variable indicating any abuse or dependence of drugs and/or alcohol, versus none, was also created.21 HIV-related physical symptoms were measured at baseline and every three months using the HIV Symptom Inventory22 to indicate the total number of symptoms, coded discretely. Mental health functioning was also measured at baseline and at six- and twelve-month follow-ups using the Short Form-12, scored on a 0–100 scale (with higher numbers indicating greater functionality; US population mean=50, one standard deviation (SD)=10).23,24 CD4 count was measured at baseline and at six and twelve months post-baseline. Psychiatric comorbidities were measured at baseline using the MINI, and dichotomized to indicate any comorbidity (e.g. dysthymia, anxiety disorder) other than depression vs. none. HIV-related self-efficacy was measured at baseline and every three months using the managing depression/mood, managing symptoms, communicating with health care provider, getting support/help, and managing fatigue subscales of the HIV Self-Efficacy questionnaire.25 Also at baseline and every three months, stress coping style was assessed with the Brief COPE instrument, which contains 18 examples of coping strategies; participants used a four-point Likert scale to rate how often they used each strategy: “Not at all,” “A little bit,” “A medium amount,” or “A lot.”26,27 Employment status was assessed at baseline and every three months thereafter; in analyses it was dichotomized to indicate employed vs. unemployed. We theorized that the SLAM DUNC intervention would be expected to work through its effects on mental health function, HIV care self-efficacy, and stress coping style, and because we included these variables in our analyses we did not control for study arm.
Statistical Analysis
Primary Analysis
The associations between each coding of STLEs and SI were estimated using Poisson models with robust variance (instead of a log-binomial model due to model convergence issues28), clustered by participant to account for repeated observations among individuals. These models yielded estimates of the prevalence ratio of experiencing SI associated with higher numbers of STLEs. To deal with non-trivial amounts of missing data, multiple imputation was combined with inverse-probability-of-observation weighting.29,30 Among completed interviews only, missing values for all variables included in analyses were imputed using multiple imputation by chained equations.31 Ten cycles of imputation were carried out per imputed dataset; 50 datasets were imputed and analyzed. After imputation, to address potential selection bias due to excluding uncompleted contacts, inverse-probability-of-observation weights were calculated for the inverse probability of completing a given interview conditional on measured covariates, using a logistic model. Baseline and time-updated variables found to be statistically significantly associated (at alpha=0.05) with completion in bivariable analyses were included in the model. The inverse-probability-of-observation weights were stabilized by the marginal probability of interview completion.
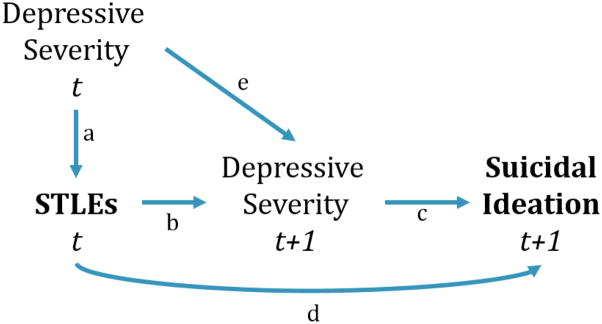
Depressive severity was theorized to act as both a time-varying confounder and mediator of the relationship between STLEs and SI over time. Depression may increase the incidence of certain STLEs (e.g., employment, financial, and legal difficulties) and also increase the risk of SI, suggesting that an estimate that does not account for confounding by depression would be biased (see Figure 1, arrows a and e). However, STLEs would be expected to affect SI in part by leading to depression. This observation implies that (subsequent) depression is a mediator of the STLE-SI relationship and an analysis that adjusts for time-varying depression would block part of the causal pathway (Figure 1, arrows b and c), leading to a biased estimate of the total effect of interest. To remove bias due to time-varying confounding by prior depression while avoiding blocking the pathway through subsequent depression, inverse-probability-of-exposure weights were calculated, for the inverse probability of exposure to STLEs. Applying these weights to the analysis models allowed us to break the association between prior depressive severity and STLEs, corresponding to arrow a in Figure 1, without blocking the mediating pathway from STLEs through subsequent depressive severity to SI (arrows b and c).
Figure 1.
Conceptual Model of the Relationship between Stressful or Traumatic Life Events, Depressive Severity, and Suicidal Ideation.
In the inverse-probability-of-exposure weight calculation, the denominator probabilities were conditional on baseline and lagged SI; lagged STLEs; current, baseline, and lagged depressive severity; and current and baseline confounders of the STLE-adherence relationship. Logistic regression was used to calculate the inverse-probability-of-exposure weights for the dichotomous exposure, while ordinal logistic regression was used to calculate the weights for continuously-coded exposures, categorized into deciles (for overall STLEs) and tertiles (for severe STLEs). All exposure weights were stabilized by the marginal probabilities of exposure. The inverse-probability-of-exposure weights were combined by multiplication with the inverse-probability-of-observation weights to create final (“full”) weights for each observation, which were applied to the analysis models. Only completed interviews were included in analyses; the weights were applied to allow the included interviews to represent the full sample. In sensitivity analyses, to assess any effects of extreme weights on the magnitude and precision of estimates, the full weights were truncated at the 1st and 99th percentiles.32 To assess the extent to which time-varying confounding affected the estimates, these models were compared to multivariable models that adjusted for all inputs into the weighting models but did not use the weights themselves.
RESULTS
Study Population
Two hundred eighty-nine participants were enrolled in the SLAM DUNC study while STLEs were being measured. Most participants (70%) were male, 62% were black, and 97% were non-Hispanic. The median (interquartile range [IQR]) age was 45 (37–51), and participants reported contracting HIV, on average, 11 years prior to study enrollment. Eighty-seven percent had at least high school-level education, 78% were single, and 27% were employed at enrollment. Eighty-five (34%) participants reported any SI at the baseline interview; the vast majority of these, 83 participants, had a score of one or two, corresponding to passive SI (Table 1).
Table 1.
Study sample characteristics (n=289)
| Variable | n (%) | Median (IQR) | Missing |
|---|---|---|---|
| Sex | 0 | ||
| Male | 204 (71) | ||
| Female | 85 (29) | ||
| Age, years | 45 (37–51) | 0 | |
| Marital status | 3 | ||
| Married/cohabitating | 62 (22) | ||
| Single | 224 (78) | ||
| Race | 0 | ||
| White | 100 (35) | ||
| Black | 179 (62) | ||
| Other | 10 (3) | ||
| Ethnicity | 7 | ||
| Hispanic | 13 (5) | ||
| Non-Hispanic | 276 (95) | ||
| Education | 4 | ||
| Less than HS grad | 38 (14) | ||
| High school grad | 110 (38) | ||
| More than high school | 137 (48) | ||
| Monthly household income, $ | 1,000 (674–1,900) | 19 | |
| Monthly household income, log10 | 3.0 (2.8–3.3) | ||
| Currently employed | 77 (27) | 4 | |
| Years since HIV diagnosis | 11 (4–17) | 12 | |
| HIV RNA viral load, log10 | 1.4 (1.4–2.1) | 26 | |
| Viral load <48 copies/mL | 177 (61) | ||
| CD4 count, cells/mm3 | 549 (331–784) | 35 | |
| Depression score | 21 (15–25) | 37 | |
| Suicidal ideation* | 36 | ||
| Any (score >0) | 85 (34) | ||
| 0 | 168 (66) | ||
| 1 | 31 (12) | ||
| 2 | 52 (21) | ||
| 3 | 1 (0.4) | ||
| 4 | 1 (0.4) |
Scores: 0=absent, 1=feels life not worth living, 2=wishes that he/she was dead, or had thoughts about hurting self, 3=suicidal ideas of gesture, 4=suicide attempt in past week
Participants completed between zero and four (the maximum possible number) interviews after enrollment (median=2, IQR=0–3). Five hundred six (49%) of the total possible 1,041 quarterly interviews were completed and therefore included in analyses. Interview completion was higher during the first six months of follow-up, with 51% and 54% of 3- and 6-month interviews completed, compared to 44% and 46% of 9- and 12-month interviews, respectively. The 289 participants reported a total of 2,270 STLEs, a mean of 2.36 events per month or 7.08 events per quarter; the number of STLEs experienced in a month ranged from 0 to 12, with a median (IQR) of 2 (0–4). Four hundred fifty-seven severe STLEs were reported, a mean of 0.48 events per month. Financial difficulties were most commonly reported, with 1.23 events/month, followed by illness, injury, or hospitalization of the participant (0.27 events/month) and employment difficulties (0.25 events/month). Legal troubles were reported with the least frequency (0.03 events/month) (Table 2).
Table 2.
Description of Stressful or Traumatic Life Events (STLEs)
| Total Number of STLEs | ||
|---|---|---|
| Per person-month | Per person-year | |
| Type of STLE | 2.36 | 28.32 |
| Financial difficulties | 1.23 | 14.76 |
| Major illness, injury, or hospitalization | 0.27 | 3.24 |
| Employment difficulties | 0.25 | 3.00 |
| Death or illness of family member or friend | 0.24 | 2.88 |
| Safety concerns | 0.10 | 1.20 |
| Romantic relationship changes | 0.09 | 1.08 |
| Estrangement from family | 0.08 | 0.96 |
| Life transitions | 0.06 | 0.72 |
| Legal difficulties | 0.03 | 0.36 |
| Total # of severe STLEs* | 0.48 | 5.76 |
Includes: divorce or separation, death or illness of immediate family member, major financial problems, time in jail, and sexual and physical assault
Missing Data
Age, sex, baseline marital status, and psychiatric comorbidity data were available for all participants. Multiple imputation was used to impute missing baseline values for <1% of alcohol dependency and adaptive coping; 1% of employment status; 2% of self-efficacy, SF12 mental functioning and HIV-related symptoms; 5% of SI; 6% of HAM-D; and 13% of CD4 count values. For post-baseline variables, values were imputed for <1% of SI and HAM-D, 1% of HIV-related symptoms, and 7% of drug and/or alcohol abuse or dependence.
In calculating the inverse-probability-of-observation weights, baseline predictors of completing interviews were age, employment, CD4 count, self-efficacy, SF12 mental functioning score, alcohol dependence, and adaptive coping. A time-updated variable indicating whether the previous contact was completed was also included in the weighting model. For additional stabilization, lagged STLE variables were added to both the numerators and denominators of the weights. Cubic splines for all continuous variables were also included in the denominators. These weights all had means close to one and tight ranges (Table 3).
Table 3.
Weight Distribution
| Exposure Coding | Inverse-Probability-of-Observation Weights | Inverse-Probability-of-Exposure Weights | Full Weights* | |||
|---|---|---|---|---|---|---|
| Mean (SD) | Min, Max | Mean (SD) | Min, Max | Mean (SD) | Min, Max | |
| All STLEs, continuous | 1.02 (0.15) | 0.81, 2.31 | 0.95 (1.84) | 0.09, 128.98 | 0.97 (1.98) | 0.08, 124.47 |
| Severe STLEs, continuous | 1.02 (0.16) | 0.78, 2.20 | 1.00 (1.10) | 0.27, 55.02 | 1.00 (1.10) | 0.22, 57.98 |
| Severe STLEs, dichotomous | 1.02 (0.16) | 0.84, 2.23 | 0.99 (0.72) | 0.41, 24.26 | 0.99 (0.73) | 0.37, 22.76 |
Product of inverse-probability-of-observation and inverse-probability-of-exposure weights
STLEs=Stressful or traumatic life events, SD=Standard deviation
Exposure and Full Weights
The inverse-probability-of-exposure weights for the continuous, overall STLE exposure had a mean of 0.95 (SD=1.84) and a range of 0.09 to 128.98. The combined inverse-probability-of-observation/inverse probability-of-exposure weights, or “full weights,” had a mean of 0.97 (SD=1.98) and range of 0.08 to 124.47 for the overall, continuous STLE exposure model. Weights for the other exposure measures were similarly well-behaved (Table 3).
Primary Outcomes
Greater numbers of STLEs, both overall and severe, were associated with increased prevalence of experiencing SI. In the final weighted model, each additional STLE was associated with a 7% increase in prevalence of SI (prevalence ratio (PR): 1.07, 95% confidence interval (CI): 1.00, 1.14), while each additional severe STLE was associated with a 19% increase in prevalence of SI (PR: 1.19, 95% CI: 1.00, 1.42). Experiencing any severe STLE vs. none suggested an increased prevalence of SI (PR: 1.17, 95% CI: 0.64, 2.15) (Table 4).
Table 4.
Associations of Stressful or Traumatic Life Events with Suicidal Ideation
| All STLEs | Suicidal Ideation PR (95% CI) | ||
|---|---|---|---|
| Crude | Multivariable Adjusted | Inverse-probability Weighted | |
| Per 1-unit increase | 1.08 (1.06, 1.11) | 1.04 (1.01, 1.07) | 1.07 (1.00, 1.14) |
| Severe STLEs | |||
| Per 1-unit increase | 1.33 (1.22, 1.45) | 1.10 (0.94, 1.28) | 1.19 (1.00, 1.42) |
| Any vs. none | 2.52 (1.51, 4.19) | 1.18 (0.70, 2.00) | 1.17 (0.64, 2.15) |
STLEs=Stressful or traumatic life events, PR=prevalence ratio
For the continuously-measured exposures, crude results were further from the null than weighted results, while multivariable-adjusted results were all closer to the null. Truncating weights at the 1st and 99th percentiles did not qualitatively change the estimates for the continuously-measured exposures, but it did increase their precision, as expected.32 For the dichotomous exposure, however, the estimate was biased away from the null and more precise than with the original weights.
DISCUSSION
STLEs were common in this population of adults with depression and HIV in the Southeastern US, and associated with higher prevalence of experiencing SI. For each additional STLE per month there was a 7% increase in prevalence of SI, and for each additional severe STLE there was a 19% increase in prevalence of SI (Table 4). These prevalence ratios correspond to important increases in prevalence in a population in which SI was reported in 23% of observations with at least one STLE and 27% of observations with at least one severe STLE.
Little is known about the burden of STLEs in this type of population of persons with both HIV and depression. The burden of STLEs in this sample was higher than that in HIV-infected populations without depression in similar settings (the Southeastern US), which might be expected under the hypothesis that depression can affect STLEs. While our participants experienced more than two STLEs per month, on average, and one severe STLE every two months, Mugavero, et al found a median of nine STLEs and three severe STLEs over nearly two years of follow-up,8 and Leserman, et al found a mean of roughly three STLEs in a six-month period.10 In a more nationally representative study of HIV-infected adults, however, the number of STLEs participants experienced per month was more than twice the number our participants experienced.9 The baseline burden of SI in this population was also in line with that found in related populations. Badiee, et al. found a SI prevalence of 26% in an HIV-infected population (without depression), and Gaynes, et al. found a prevalence of 45% in depressed patients in primary care (HIV-uninfected).33,34 Taken together with the existing evidence, our results highlight the clinical importance of understanding the burden and impact of both STLEs and SI, and the need to assess for and respond to them.
In a review of the existing studies assessing the relationship between STLEs and SI, Liu, et al. indicate that while most studies found a positive association, a few found a negative or null association, and methodological flaws were common. Most of the studies they reviewed were conducted among children or adolescents, and none were among HIV-infected persons.11 They concluded that the seemingly positive association should be viewed as preliminary, and that studies were needed assessing the relationship over time using multiple brief intervals of measurement. In a study of predictors of SI in a random sample of South Australians, Goldney, et al. found elevated risk of SI associated with experiencing a psychosocial event (RR: 2.21, 95% CI: 1.48, 2.38) and with experiencing a traumatic event (RR: 2.49, 95% CI: 1.49, 4.18). Both estimates are stronger than ours; however, these estimates are from univariate analyses and therefore might be exaggerated by confounding.35 In contrast to these estimates indicating a strong association, other studies found no association between STLEs and SI.36,37 The current study provides a methodologically rigorous assessment of the STLE-SI association over time, with brief intervals in which STLEs were measured proximal to when SI was measured using a standardized tool. Our finding of a positive relationship between STLEs and SI is in line with the majority of the evidence in the existing literature, and provides the first known assessment of this relationship in an HIV-infected population.
The use of inverse-probability-of-exposure weights allowed us to account for time-varying confounding by depressive severity. As it was theorized to be both a mediator and a confounder of the STLE-SI association, we wanted our estimate of the total effect of STLEs on SI to include the portion that works through current depression while removing confounding from prior depression.38 Including concurrent and lagged depressive scores in the denominators of the exposure weights yielded marginal estimates of the associations of interest. The crude, unweighted estimates for the continuous exposures were further from the null, which can be interpreted as being confounded upwards by prior depressive severity. The multivariable-adjusted estimates, also unweighted, were nearly all closer to the null than the weighted estimates, suggesting that adjusting for depressive severity not only blocked the confounding by prior depressive severity but also blocked the mediating pathways through subsequent depressive severity. The weighted estimates thus allowed us to block confounding while allowing mediation, to obtain more accurate results.
A strength of this study was that STLEs and SI were measured close in time, and at multiple times over the course of follow-up, allowing for assessments of recent stressors and subsequent SI. This is an improvement over the measurement of most prior studies that have used cross-sectional measurement and/or long recall periods for measurement of STLEs.8,10 As both STLEs and SI were measured by self-report, there is the potential for dependent measurement error, but they were measured during different interviews and in different contexts, which should have helped avoid some of the possibility of bias.
The large amount of missing data resulting from low retention during follow-up in the SLAM DUNC study is a limitation of this study. To address it, we used a combination of multiple imputation and inverse-probability-of-observation weighting, based on observed predictors of missingness, to address the potential for selection bias arising from these missing data. This approach should be less biased than a complete case analysis, and the two-pronged approach helped to mitigate the potential bias resulting from misspecification of models in either prong. There is, however, the possibility that missingness could also be a function of unobserved characteristics. If missingness were associated both with higher numbers of STLEs and with higher prevalence of SI, for example, the present analysis would likely have underestimated the actual association of STLEs with SI; however, overestimation is also a possibility. We also cannot exclude the possibility of misspecification of the weighting models, the imputation models, or both.
Another potential limitation is the inclusion of both acute events and chronic stressors in our exposure, which might elicit different reactions and coping mechanisms in different individuals. Additionally, the outcome captured both new and ongoing instances of SI, which may have differing associations with STLEs. Due to our relatively small sample size, however, and because we did not have information about timing of onset or duration, we kept all reported STLEs and SI in the measures of exposure and outcome, respectively, limiting our ability to tease apart incidence and prevalence. This presents an important next step in assessing the relationship between both acute and chronic stressors and onset of SI and highlights the importance of collecting additional data about timing.
The inclusion of STLE and SI history in the denominators of the inverse probability of exposure weights permitted us to estimate the association between the most recent STLEs (in the past three months) and current SI at each time point, independent of prior history. From the perspective of a hypothetical randomized controlled trial, this would correspond to random assignment of STLEs over a three-month period and assessment of SI at the end of three months, repeated multiple times. The inverse of the reported PR could therefore be thought of as the impact on SI of an intervention to reduce STLEs over a three-month period.
SI was common in this population of HIV-infected adults with depression, and STLEs, which were also common, were identified as important risks factor for SI. Efforts to reduce exposure to STLEs or to improve individuals’ skills for coping with STLEs could therefore help reduce SI and improve psychological wellbeing. Studies have shown that interventions aimed at improving depression care and initiating expressive writing about STLEs were associated with fewer STLEs39 and improved health and quality of life,40 respectively. Other interventions focused on reducing the incidence of STLEs and developing skills to cope with STLEs could be developed for HIV-infected populations, which independently of STLEs are also more prone to depression and therefore to SI. Interventions could also focus on increasing provider awareness and assessment of STLEs to better target those patients at increased risk of SI to receive more intense support services. Overall, such efforts could play an important role in reducing SI, which can indicate psychological distress and is also one of the strongest and most proximal risk factors for suicide attempts and deaths by suicide.
HIGHLIGHTS.
Stressful or traumatic life events are common among people with HIV and depression
Stressful or traumatic life events are associated with increased suicidal ideation
Interventions to prevent/cope with stress could reduce suicidal ideation
Acknowledgments
Financial support
This study was supported by grant R01MH086362 of the National Institute of Mental Health and the National Institute for Nursing Research, National Institutes of Health, Bethesda, MD, USA, and by training grant #5T32AI070114-08 of the National Institute of Mental Health. Support was also provided by the Centers for AIDS Research at the University of North Carolina at Chapel Hill, Duke University, and the University of Alabama at Birmingham NIH-funded programs (P30- AI50410; P30-AI064518; and P30-AI027767). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Julie K. O’Donnell, University of North Carolina at Chapel Hill, Department of Epidemiology
Bradley N. Gaynes, University of North Carolina at Chapel Hill School of Medicine, Department of Psychiatry
Stephen R. Cole, University of North Carolina at Chapel Hill, Department of Epidemiology
Andrew Edmonds, University of North Carolina at Chapel Hill, Department of Epidemiology.
Nathan M. Thielman, Duke University, Center for Health Policy, Duke Global Health Institute
E. Byrd Quinlivan, University of North Carolina at Chapel Hill, Institute for Global Health, Infectious Diseases and Center for AIDS Research.
Kristen Shirey, Duke University School of Medicine, Department of Psychiatry.
Amy D. Heine, University of North Carolina at Chapel Hill, Institute for Global Health and Infectious Diseases
Riddhi Modi, University of Alabama at Birmingham, Division of Infectious Diseases.
Brian W. Pence, University of North Carolina at Chapel Hill, Department of Epidemiology
References
- 1.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999 Jul;56(7):617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 2.Goldney RD, Dal Grande E, Fisher LJ, Wilson D. Population attributable risk of major depression for suicidal ideation in a random and representative community sample. Journal of affective disorders. 2003 May;74(3):267–272. doi: 10.1016/s0165-0327(02)00017-4. [DOI] [PubMed] [Google Scholar]
- 3.Pence BW, O’Donnell JK, Gaynes BN. Falling through the cracks: the gaps between depression prevalence, diagnosis, treatment, and response in HIV care. AIDS. 2012 Mar 13;26(5):656–658. doi: 10.1097/QAD.0b013e3283519aae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Preventing chronic disease. 2005 Jan;2(1):A14. [PMC free article] [PubMed] [Google Scholar]
- 5.Ickovics JR, Hamburger ME, Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA : the journal of the American Medical Association. 2001 Mar 21;285(11):1466–1474. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]
- 6.Wong MD, Sarkisian CA, Davis C, Kinsler J, Cunningham WE. The association between life chaos, health care use, and health status among HIV-infected persons. Journal of general internal medicine. 2007 Sep;22(9):1286–1291. doi: 10.1007/s11606-007-0265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reif S, Mugavero M, Raper J, et al. Highly stressed: stressful and traumatic experiences among individuals with HIV/AIDS in the Deep South. AIDS care. 2011 Feb;23(2):152–162. doi: 10.1080/09540121.2010.498872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mugavero MJ, Raper JL, Reif S, et al. Overload: impact of incident stressful events on antiretroviral medication adherence and virologic failure in a longitudinal, multisite human immunodeficiency virus cohort study. Psychosomatic medicine. 2009 Nov;71(9):920–926. doi: 10.1097/PSY.0b013e3181bfe8d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Corless IB, Voss J, Guarino AJ, et al. The Impact of Stressful Life Events, Symptom Status, and Adherence Concerns on Quality of Life in People Living With HIV. The Journal of the Association of Nurses in AIDS Care : JANAC. 2013 Mar 6; doi: 10.1016/j.jana.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leserman J, Ironson G, O’Cleirigh C, Fordiani JM, Balbin E. Stressful life events and adherence in HIV. AIDS patient care and STDs. 2008 May;22(5):403–411. doi: 10.1089/apc.2007.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu RT, Miller I. Life events and suicidal ideation and behavior: a systematic review. Clinical psychology review. 2014 Apr;34(3):181–192. doi: 10.1016/j.cpr.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Appelqvist-Schmidlechner K, Henriksson M, Joukamaa M, Parkkola K, Upanne M, Stengard E. Psychosocial factors associated with suicidal ideation among young men exempted from compulsory military or civil service. Scandinavian journal of public health. 2011 Dec;39(8):870–879. doi: 10.1177/1403494811421223. [DOI] [PubMed] [Google Scholar]
- 13.Stein DJ, Chiu WT, Hwang I, et al. Cross-national analysis of the associations between traumatic events and suicidal behavior: findings from the WHO World Mental Health Surveys. PloS one. 2010;5(5):e10574. doi: 10.1371/journal.pone.0010574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pence BW, Gaynes BN, Williams Q, et al. Assessing the effect of Measurement-Based Care depression treatment on HIV medication adherence and health outcomes: Rationale and design of the SLAM DUNC Study. Contemp Clin Trials. 2012 Jul;33(4):828–838. doi: 10.1016/j.cct.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamilton M. Rating depressive patients. The Journal of clinical psychiatry. 1980 Dec;41(12 Pt 2):21–24. [PubMed] [Google Scholar]
- 16.Hamilton M. A rating scale for depression. Journal of neurology, neurosurgery, and psychiatry. 1960 Feb;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zimmerman M, Chelminski I, Posternak M. A review of studies of the Hamilton depression rating scale in healthy controls: implications for the definition of remission in treatment studies of depression. The Journal of nervous and mental disease. 2004 Sep;192(9):595–601. doi: 10.1097/01.nmd.0000138226.22761.39. [DOI] [PubMed] [Google Scholar]
- 18.Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the Life Experiences Survey. Journal of consulting and clinical psychology. 1978 Oct;46(5):932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- 19.Leserman J, Petitto JM, Gu H, et al. Progression to AIDS, a clinical AIDS condition and mortality: psychosocial and physiological predictors. Psychological medicine. 2002 Aug;32(6):1059–1073. doi: 10.1017/s0033291702005949. [DOI] [PubMed] [Google Scholar]
- 20.Leserman J, Whetten K, Lowe K, Stangl D, Swartz MS, Thielman NM. How trauma, recent stressful events, and PTSD affect functional health status and health utilization in HIV-infected patients in the south. Psychosomatic medicine. 2005 May-Jun;67(3):500–507. doi: 10.1097/01.psy.0000160459.78182.d9. [DOI] [PubMed] [Google Scholar]
- 21.Lecrubier Y, Sheehan DV, Weiller E, et al. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Eur Psychiat. 1997;12(5):224–231. [Google Scholar]
- 22.Bing EG, Burnam A, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiat. 2001 Aug;58(8):721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- 23.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996 Mar;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Ware J, Kosinski M, Turner-Bowker D, Gandek B. How to score version 2 of the SF-12 health survey. Lincoln, RI: Quality Metric Incorporated and Health Assessment Lab; 2002. [Google Scholar]
- 25.Shively M, Smith TL, Bormann J, Gifford AL. Evaluating Self-Efficacy for HIV Disease Management Skills. AIDS & Behavior. 2002;6(4):371–379. [Google Scholar]
- 26.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of personality and social psychology. 1989 Feb;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 27.Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. International journal of behavioral medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 28.Yelland LN, Salter AB, Ryan P. Performance of the modified Poisson regression approach for estimating relative risks from clustered prospective data. Am J Epidemiol. 2011 Oct 15;174(8):984–992. doi: 10.1093/aje/kwr183. [DOI] [PubMed] [Google Scholar]
- 29.Moodie EE, Delaney JA, Lefebvre G, Platt RW. Missing confounding data in marginal structural models: a comparison of inverse probability weighting and multiple imputation. The international journal of biostatistics. 2008;4(1):Article 13. doi: 10.2202/1557-4679.1106. [DOI] [PubMed] [Google Scholar]
- 30.Seaman SR, White IR, Copas AJ, Li L. Combining multiple imputation and inverse-probability weighting. Biometrics. 2012 Mar;68(1):129–137. doi: 10.1111/j.1541-0420.2011.01666.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Statistics in medicine. 2011 Feb 20;30(4):377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 32.Cole SR, Hernan MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008 Sep 15;168(6):656–664. doi: 10.1093/aje/kwn164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Badiee J, Moore DJ, Atkinson JH, et al. Lifetime suicidal ideation and attempt are common among HIV plus individuals. Journal of affective disorders. 2012 Feb;136(3):993–999. doi: 10.1016/j.jad.2011.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gaynes BN, Rush AJ, Trivedi M, et al. A direct comparison of presenting characteristics of depressed outpatients from primary vs. specialty care settings: preliminary findings from the STAR*D clinical trial. General hospital psychiatry. 2005 Mar-Apr;27(2):87–96. doi: 10.1016/j.genhosppsych.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 35.Goldney RD, Wilson D, Dal Grande E, Fisher LJ, McFarlane AC. Suicidal ideation in a random community sample: attributable risk due to depression and psychosocial and traumatic events. The Australian and New Zealand journal of psychiatry. 2000 Feb;34(1):98–106. doi: 10.1046/j.1440-1614.2000.00646.x. [DOI] [PubMed] [Google Scholar]
- 36.McKeown RE, Garrison CZ, Cuffe SP, Waller JL, Jackson KL, Addy CL. Incidence and predictors of suicidal behaviors in a longitudinal sample of young adolescents. J Am Acad Child Psy. 1998 Jun;37(6):612–619. doi: 10.1097/00004583-199806000-00011. [DOI] [PubMed] [Google Scholar]
- 37.Reinecke MA, DuBois DL. Socioenvironmental and cognitive risk and resources: Relations to mood and suicidality among inpatient adolescents. Journal of Cognitive Psychotherapy: An International Quarterly. 2001;15(3):195–222. [Google Scholar]
- 38.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000 Sep;11(5):550–560. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Sherbourne CD, Edelen MO, Zhou A, Bird C, Duan N, Wells KB. How a therapy-based quality improvement intervention for depression affected life events and psychological well-being over time: a 9-year longitudinal analysis. Medical care. 2008 Jan;46(1):78–84. doi: 10.1097/MLR.0b013e318148478d. [DOI] [PubMed] [Google Scholar]
- 40.Andersson MA, Conley CS. Optimizing the perceived benefits and health outcomes of writing about traumatic life events. Stress and health : journal of the International Society for the Investigation of Stress. 2013 Feb;29(1):40–49. doi: 10.1002/smi.2423. [DOI] [PubMed] [Google Scholar]