Abstract
Objective
Technologies are not always successfully implemented into practise. We elicited experiences of acute care providers with the introduction of technology and identified barriers and facilitators in the implementation process.
Methods
A qualitative study using one-on-one interviews among a purposeful sample of 19 physicians and nurses within ten emergency departments and intensive care units was performed. Grounded theory, iterative data analysis and the constant comparative method were used to inductively generate ideas and build theories.
Results
Five major categories emerged: decision-making factors, the impact on practise, technology's perceived value, facilitators and barriers to implementation. Barriers included negative experiences, age, infrequent use, and access difficulties. A positive outlook, sufficient training, support staff, and user friendliness were facilitators.
Conclusions
This study describes strategies implicated in the successful implementation of newly adopted technology in acute care settings. Improved implementation methods and evaluation of implementation processes are necessary for successful adoption of new technology.
Keywords: Technology, Implementation, Adoption, Emergency department, Intensive care unit
1. Introduction
While implementation science has been established for decades, this area of research has become increasingly relevant due to the large and sometimes persistent gaps between the appearance of medical evidence and its acceptance and use in practise. Much of this research has focused on the implementation of practise guidelines or behavioural health programmes [1-6]. Medical technology, however, is advancing at a rapid rate and requires equal attention [7, 8]. Health care providers are inundated with new technology and devices at national conferences and exhibitions, in the literature, and through colleagues or vendors [9].
Whereas adoption refers to the initial decision to use or purchase a technology, implementation deals with the actual use of that technology in practise. Technology adoption can be a challenge, entailing approval by individuals or committees and meeting budgetary requirements [13, 14]. Systems or devices may be purchased for use in a specific clinical setting, but fail to be successfully implemented or used to their full potential [10, 11]. It is not uncommon for the same technology to thrive in one institution yet fail in another, perhaps due to differences in the implementation process [12]. Ideally, once a technology is identified for adoption, the efforts expended and the capital invested to bring it online should not be undermined by poor planning and execution of efforts to incorporate such new devices into practise. Further, once a technology is adopted, it is not uncommon to find that a structured process that properly evaluates how well the technology has been integrated has not been put into place [15]. In some cases, the newly adopted technology is purchased and brought to a unit but not successfully integrated [13, 16].
In order to better understand how to implement newly adopted technology successfully in the future, it is important to understand the reasons why implementation of newly adopted technology may fail or succeed in the healthcare setting. Intensive care units (ICUs) and emergency departments (EDs) are unique areas within the hospital. These units typically have access to a wide array of technology and medical devices and utilize technology at high rates.
This is the first study to examine the experiences and attitudes of physician and nurse providers in acute care settings regarding the introduction and implementation of newly adopted technology. Because, ultimately, providers make the final decision about what to use and what not to use at the patient's bedside, it is vitally important to understand their experience in implementing newly adopted technologies. Knowledge of what providers perceive to be facilitators and barriers in the successful introduction of technology will allow hospital administrators and staff to identify, purchase, and successfully adopt technologies without wasting healthcare dollars and resources. This study provides key insights into both successful implementation strategies and key pitfalls to avoid that will be of use to nurse and physician leaders in the ICU and ED as they implement technology in these unique settings.
2. Materials and Methods
2.1 Overview
A qualitative, exploratory study was conducted at five hospitals in Connecticut in order to better understand the facilitators and barriers associated with the implementation of new technology in ICUs and EDs. Sites were purposely selected to reflect a range of clinical settings and included Yale-New Haven Hospital, an urban, tertiary care, academic center; Yale-New Haven Children's Hospital, a non-freestanding, academic children's hospital; Connecticut Children's Medical Center, a free-standing, academic children's hospital; Bridgeport Hospital, an urban, private hospital; and Norwalk Hospital, a suburban, community hospital [17]. Data collection ran from July 2012 through December 2012.
2.2 Participants
Purposeful and snowball sampling was employed in an effort to enroll participants that were likely to have had an opportunity to use newly adopted technology for patient care [17, 18]. Unlike random sampling, purposeful sampling refers to the deliberate selection of participants who have unique insights, are willing to share their opinions, and have the experiences necessary to discuss the topic of interest. In snowball sampling, individuals identify potential subjects who they feel would provide new or useful information to the study. Departmental heads and nurse managers from each unit were contacted by the principal investigator (ML) and asked to identify eligible participants. These were team members who spent the majority of their time in a clinical role. At least one doctor and one nurse from the ED and ICU of each hospital were targeted for enrollment. Participants also were asked to identify other key decision makers or technology users to be included in the study. Individuals were contacted by telephone or email and a written information sheet was provided. Demographic information was collected from all participants.
2.3 Data Collection Techniques
Interviews took place within the participants’ own institution. A research associate with experience in qualitative interviewing (PS) performed all interviews. The institutional review board of each participating hospital approved the study prior to the interviews and waived the need for written consent. A semi-structured interview guide was used and piloted with one nurse and one physician [17]. The interview explored providers’ experiences with and attitudes toward using newly adopted technology and assessed facilitators and barriers that may impact the implementation of newly adopted technology [18]. Technologies discussed were chosen by the participants and not restricted based on degree of evidence for use or length of time available on the market.
The interviews, which lasted an average of 30 minutes, were audio-recorded and professionally transcribed. Missing text from the transcriptions was compared to the original audio recordings and re-transcribed for completeness. The interview guide was subsequently modified in an iterative process based on new understanding from successive interviews. All subjects received a small monetary incentive at the end of the interview.
2.4 Data Analysis
The principles of grounded theory were applied, including iterative data analysis and the constant comparative method, such that the data was used to inductively generate ideas and build theories [17, 19]. Grounded theory centers around the generation of hypothesis or theories without first determining a theoretical construct. Data analysis is iterative, or repetitive, in that data is being collected and analyzed simultaneously over time and the same methods are repeated with each cycle. The constant comparative method involves examining and refining concepts that emerge from the data by comparing codes that are being newly assigned to the text to previously assigned codes and assessing whether the concepts are congruent or a new theory is emerging. Three investigators (ML, AR, JK) read and independently coded each transcript. The coding team then met and reviewed each transcript line-by-line. Discrepancies in coding were discussed until group consensus on the data was established. Data collection and coding occurred simultaneously, thus the list of codes was iteratively revised and applied to incoming data. When the coding process was complete, related concepts were combined into categories and developed into themes consistent with a grounded theory approach in order to describe key issues and experiences discussed by the participants [17, 20, 21] . An iterative process of data analysis occurred such that codes were revised, added, and deleted as the code structure was refined [22].
Changes to the initial interview guide based on the inductive analysis were justified and explained in order to assure reliability and reproducibility [17]. Recruitment and interviews continued until data reached theoretical saturation, that is that no new themes emerged [18]. Once the code structure was finalized, the primary author reviewed all transcripts to ensure that the data was coded consistently and the senior author (AA) reviewed selected transcripts in the process of triangulation [17]. An audit trail was created to provide systematic and detailed documentation of analytical decision-making during this process (Appendix 1). HyperResearch (ResearchWare, Inc.), a qualitative analysis software tool, was used as an organizational tool to support the analysis of data. This allowed for collating of data by type of participant, unit, and hospital.
3. Results
Nineteen acute care providers from ten hospital units were interviewed (table 1). Five major categories and 35 codes emerged from the interview transcripts (table 2). In talking about newly adopted bedside technology, participants used an array of examples such as electronic medical records, bedside ultrasound, point of care testing devices, and venous catheters.
Table 1.
Participant characteristics
| Variable | n (%) |
|---|---|
| Unit and Provider Type | |
| Emergency Department | 9 (47) |
| Physician | 5 (26) |
| Nurse | 4 (21) |
| Intensive Care Unit | 10 (53) |
| Physician | 5 (26) |
| Nurse | 5 (26) |
| Mean Age in years, n (Min, Max) | 43 (27, 62) |
| Mean Years on Unit, n (Min, Max) | 9.5 (1, 40) |
Table 2.
Major categories that emerged from the transcripts.
| Theme |
|---|
| 1. Decision-making factors in adoption |
| 2. Impact of technology on providers' practice |
| 3. Perceived positive value of technology |
| 4. Facilitators of technology implementation |
| 5. Barriers to technology implementation |
3.1 Decision-Making Factors
The methods and reasons for adoption of new technologies described by our subjects were often varied and poorly understood by clinical staff, but new technology was more often supported when providers were involved on the ground level. The driving force for the decision to adopt a technology could arise from an individual level (when an individual has an interest in a technology) or a unit level (when the technology is being introduced to fill a gap or solve a problem). Both nurses and physicians described their ability to initiate the introduction of technology. When a newly adopted technology is introduced in an acute care setting, there are often discussions that guide the use of that technology, or implementation decisions. These decisions could include specific guidelines and instructions for use or rules about supervision. Overall, however, there was a lack of awareness about the process involved in the adoption and implementation of new technology by all participants. Comments by staff often referred to people at a higher level in the organizational chain or participants made educated guesses about the details involved in these decisions. Respondents mentioned a variety of venues for information on technology ranging from people within their unit or within their institution, regional and national colleagues, conference settings and evidence-based literature.
A key finding related to decision-making was the contrast observed in participant receptiveness when a staff buy-in process was in place versus a mandated change. In general, physicians and nurses appreciated being a part of the decision-making process instead of having decisions thrust upon them without any apparent input. Buy-in, including the ability to trial technology, was seen as a positive factor in adoption and implementation. This is contrasted with an unexpected change or mandate to use newly adopted technology, which is typically seen as frustrating and stressful in the workplace. These feelings typically came about when discussing technology that was frequently used and had a major impact on practise. Staff champions, or early adopters, helped to initiate the adoption of technology. These individuals typically spearheaded the introduction of a device and were enthusiastic about its presentation. However, the presence of positive influences such as buy-in or early adopters did not always ensure the successful adoption and implementation of technology. Illustrative quotes are provided in table 3.
Table 3.
Illustrative quotes are provided for several codes in each major category
| Category | Illustrative Quote |
|---|---|
| Decision-Making Factors | |
| Driving force behind the adoption of new technology | Sometimes if there's an error, that prompts an action. So they now have bedside screening; the nurses are playing with a device now to barcode the labs (at the) bedside, because to avoid the error of somebody's labs getting mislabeled. So lab mislabeling would be the problem; what's the solution? Well, let's try and do bedside barcoding. |
| Implementation decisions surrounding newly adoped technology | I wrote a three-page statement about (how to) use this is in the medical ICU, what it would be used for, what the expectations would be in terms of training and oversight. |
| Staff buy-in prior to adoption of technology | She does involve the staff in a lot of decision-making for, ‘Let's trial this, tell me what you think of this technology. What do you think? Do you think we should use it?’ New defibrillator pads, new whatever, whatever it is, small or big. She always involves the staff and values their opinion. And I think that's huge in us being receptive to new technology. |
| Mandated use of newly adopted technology | It seemed like I worked on Friday, I was off for a weekend, I didn't hear anything about new IVs, and I came back on Monday and all the old IVs were gone and there were new IVs. And they said, ‘These are the new IVs. There is an instruction hour at 12:00 to 1:00. You're going to learn how to use them’ ...but the issue is when you've been using other IVs for four years and you have a patient come in who is hemodynamically unstable with no access, and you're trying to learn how to use new IVs, when previously you could put a 16 gauge in a rock and now you're fumbling around with new IVs and the patient is unstable. And you had no warning that you were getting new IVs. That could be a little frustrating. |
| Early adopters promote new technology | There was an individual within our division, a physician who was very excited about this and felt that it held a lot of promise. So, this one individual sort of reached out to the company, reached out to some other intensivists who speak on behalf of the company in the field who came and visited, did an in-service, talked about it. We ended up trialing it. Some people felt that it was reasonably useful, so we bought the monitor, but we just don't use it that much. |
| Impact on Practice | |
| Major changes to overall practice due to new technology | I think the one that has had the biggest impact on care is this mobile heartbeat phone that we've started to use on the clinical units, and that allows us to communicate with each other, provides us with text messages to each other about patient updates...It was something that was really a major change in how we communicate with each other. |
| Who decides to use the technology | Generally speaking, everybody has things that they prefer to use and others don't. Some find certain information more reliable than other information. And you just find trends of staff. This one doctor might use this technology more often, but the other ones don't. |
| Adaptation of technology for different purposes or populations | A lot of the technology that makes its way to the PICU has originally started in the adult unit....the studies and data supports use in adults, but then when you look at controlled trials, if there are any kids, there's really not a whole lot of data. So, then when you go and try to start using them, it doesn't, the technology is not necessarily the same for kids as it is for adults. And so, some of these things, they just don't work, and I don't know why, but it's kind of the nature of the beast |
| Positive Value of Technology | |
| Perceived positive value of technology | A day after the training we actually had an indication for use, and we used it very successfully, and it was received very well. The patient was resuscitated really because of it... it was kind of exciting to see a patient benefit from it. Now everybody's kind of ‘Let's go, let's use it, we want to use it now’. |
| Lack of perceived value of technology | They gave us a lot of clinical support, but the machine... I don't think the staff saw the value. That was really the key. |
| Technology Facilitators | |
| Superusers and technology support during introduction of new technology | I think you really become an expert user and then train other people. I think it's peer to peer at that point. You're getting other people up and running with a new product. |
| Ramp up period needed to become facile with new technology | I don't use it for ocular measurements of the nerve sheath...there is a learning curve that I don't anticipate getting good at quickly enough to make it useful. |
| Positive outlook on technology in general | I love it. I like new technologies that are useful, that fill a role, fill a need, and especially if they enhance patient safety. It's exciting. We're in ICU, we're tech junkies. We love that stuff. We like our new toys. |
| Technology Barriers | |
| Negative emotions surrounding newly adopted technology | The nurses just didn't like it. I thought it was a wonderful idea. It made a lot of sense. It seemed to be a safer way to do things. It seemed likely that it would save money by not requiring the use of X-rays after you place these tubes. And the nurses just consistently said they didn't like it, they didn't trust it. They had to get X-rays anyways...And we stopped. |
| Older age impacting perception and use of technology | I think that the younger group is definitely much quicker to embrace the technology and they seem to just adapt to it much more rapidly. The more senior group is a little bit slower, but we come along. A good example is the iPhones - we're using these mobile heartbeat iPhones. If you don't own your own personal iPhone, it was a little hard to adapt. |
| Low frequency use of technology is a barrier | It's usually more anxiety-provoking because especially if it's not something you use a lot. You might get trained in it, but you might not use it for a couple months or something. And then to try and do that in a moment where maybe it's an emergency, that's anxiety-provoking, because you don't feel proficient at it. |
| Negative experiences with technology discourage future use | I just refused to use it, because every time I tried to get one of those phones during the pilot process, I couldn't sign in. I don't know if my code didn't work, but there was always something wrong with it. There was always something wrong where it wasn't a smooth transition to using it. So I didn't. |
| Inadequate knowledge acquisition is a concern to practitioners | In all of clinical medicine, but in the ICU especially, we have this tendency to employ technology that we understand quite poorly. And then when we don't understand the technology well we are likely to commit a lot of errors in the interpretation of the data that those technologies generate. And when we do that I think we start providing bad care... Pulse oximetry is a great example of that...I see pulse oximetry poorly used almost every day, and that is a genuinely dangerous thing, because we just make treatment decisions based on bad data. And when you start to do that then I think you're going to make a lot of mistakes, and I think that is a potentially dangerous thing to start to do. |
| Insufficient support during introduction negatively impacts use of technology | I will say that sometimes some tools or machines show up and no one really knows how to use it, and that doesn't start a new technology off on the right foot.... It just kind of appeared. So, when that happens, people get frustrated and I think it probably doesn't lead to it being accepted well. |
3.2 Impact on Practise
Newly adopted technology impacted practise variably; however no single factor consistently applied to all technologies among our participants. Technology could be perceived as leading a major change in overall practise or only a minor change in practise. These impacts were independent of how often a technology was used, and could have either a positive or a negative impact. However, even when technology had a perceived benefit, it was not always enough of an impetus to impact practise. Participants mentioned how specific technologies on the unit are only used by certain providers or in certain patient populations, as compared to other technology that is used by all providers or is applied to all patients, such as electronic medical records or patient monitors. These limitations may be a function of the technology itself or due to limitations in knowledge about the applications of the technology.
Team dynamics such as who decides when or how a newly adopted technology should be used were also discussed. There were two facets to this concept: provider decision-making and policies for the use of technology. In some cases, a decision was made that technology should be used as a standard of practise. This is in contrast to an individual provider's decision to use a technology when they feel it is warranted, when it would be beneficial, or when they are comfortable using the device. Another concept that was established was the adaptation of technology. Some technologies grew in functionality over a period of time within a unit or crossed between units, providers or patients. However, if adaptation occurred without evidence of benefit in these other settings, for example in children versus adults, it may not prove as useful (table 3).
3.3 Positive Value of Technology
Technology was typically perceived in a positive light if it was felt to be beneficial to providers, to patients, or to trainees. Benefits covered numerous aspects of patient care and job satisfaction, such as workflow, safety, and communication. Physician participants also discussed the benefits of additional patient information, improvements in diagnostic accuracy and procedural skills. These advantages were balanced against the perceived disadvantages of a device such as size of the device, pain for the patient, or difficulty with use. Benefits that are clearly visible may make staff more enthusiastic about implementation (table 3). The perceived value of newly adopted technology had to also exceed the actual cost of the technology itself.
As science advances and evidence accumulates, it is sometimes the case that technology or devices become the standard of care. Implementation of newly adopted technology seems to be particularly difficult when there is a lack of perceived value or minimal perceived value by staff (table 3).
3.4 Technology Facilitators and Barriers
The last major categories related to how technology facilitators and barriers played a role in successful implementation. Implementation of new technology was facilitated when a strong educational foundation and support system was available. This included initial training on a device, the availability of superusers and technology support staff to assist providers, and later on the availability of a jumpstart guide or annual validation to refresh a user's memory on operating the technology. Most often support personnel supplied by the company producing the technology was available for only a limited amount of time. On the other hand, superusers were typically people on the unit with advanced knowledge of and comfort with the device (table 3).
In contrast, the implementation of newly adopted technology was hindered if staff felt there was insufficient support available to them or inadequate knowledge acquisition. A lack of technical support to address difficulties with use was also problematic as was the timing of education and support, for example if education occurred too far in advance or if support personnel were only available at certain times of the day when the technology was not in use (table 3).
Some providers were self-aware of inadequate knowledge acquisition and hesitant to use newly adopted technology for this reason. Other providers discouraged the use of technology because they feared staff members did not fully understand how to use a device correctly or interpret the data they received and may become inappropriately reliant on this information (table 3).
Some facilitators and barriers were related to personal characteristics of the users. Facilitators included the users’ baseline abilities with technology and having a positive outlook, whereas barriers included age, learner fatigue, and negative emotions such as resistance to change, fear of errors, and anxiety related to performance. A provider's feelings about technology in general can influence their ability to trial a newly adopted device and the implementation process (table 3). However, despite a positive attitude about newly adopted technology and change, providers sometimes experienced learner fatigue from being repeatedly introduced to new technologies or other institutional changes.
Other characteristics have to do with the technology itself, such as the ramp up period or its learning curve, its user friendliness, or negative experiences with the device. Although most people described the ramp up period as the learning curve needed to feel comfortable using a device, some respondents also discussed how the length of this period could inhibit use and implementation (table 3). The user friendliness of a device also seemed to impact implementation and use. Providers did not use devices that are more complex as readily as more simplistic, less time consuming technology. In contrast, once providers have had a negative experience with a newly adopted device, implementation may be impacted (table 3).
Whether a newly adopted technology had a high frequency of use or a low frequency of use, as well as it's availability or lack thereof as might be seen with storage problems, could also impact implementation. For example, when a device was not used often it could lead to lack of comfort (table 3). This low frequency of use led to a problem with availability.
4. Discussion
The continual influx of innovative, technological advances is a predictable and inevitable characteristic of working in acute care settings. Acute care providers have a range of attitudes and beliefs about the adoption and implementation of these new tools. This study provides useful information to nurse and physician leaders of ICUs and EDs regarding successful implementation of newly adopted technology in these settings. In particular, our data suggest several key strategies to improve the implementation process including input from staff regarding the newly adopted technology, appropriate education about the technology, assuring accessibility to the technology, and early evaluation and feedback to staff (figure 1).
Figure 1.
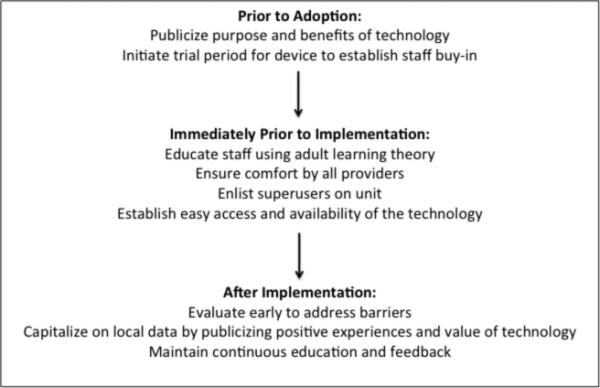
Strategic plan for implementation of new technology
Certain traits that have been shown to be pertinent to the adoption process did not emerge as strong factors for implementation in our study, whereas others continued to be important. For instance, many of Rogers’ well-known attributes of innovation that have been correlated with rates of adoption were not as strongly linked to implementation among our participants [23]. Of Rogers’ principles, compatibility and complexity paralleled the category of positive value of technology and the codes for baseline abilities and user friendliness, respectively. Unlike in other reports, the presence of an early adopter or staff champion was not frequently mentioned by our subjects as being influential in the success or failure of newly adopted technology implementation, but was helpful in decision-making or adoption [24-26]. This may suggest that further research needs to be performed on implementation factors separate from adoption characteristics.
Clinical pathways or practise guidelines have been assessed in acute care settings and have identified similar barriers to those noted by our study subjects [1, 27-29]. Cabana categorized barriers to uptake as being internal, such as lack of awareness, or external, such as lack of support [30]. In contrast to Cabana, newly adopted technologies are typically physical devices and our subjects described awareness of their presence whether or not they were successful. However, inadequate knowledge about a technology's functions and applications remained a barrier. Likewise, most newly adopted technology necessitated some form of education; inadequate support after this introduction was problematic. Our results suggest that continuous and timely education and feedback about newly adopted technology is a key factor in successful implementation. Seen here and in a prior study of neonatal ICU technology implementation, staff feelings of unease without sufficient education and knowledge of newly adopted technology applications and functions can be addressed with various educational programmes or through support personnel [13]. The need for support and education is typically balanced with the complexity of a device and the frequency with which it is used. Education needs to be thoughtful in order to be effective and reach the audience, and standard methods often fail [29, 30]. Adult learning theory, clinical case-based formats and problem solving techniques may be beneficial in education for newly adopted technology [31]. While older adults are increasingly using technology in their personal lives, age emerged as a barrier to use in this study [32]. Older individuals may be specifically targeted with technological support and efforts to reduce resistance or fear.
Contrary to other reports, once adopted, the cost of a device did not often influence its use among our participants [26]. However, negative experiences with technology, such as malfunctions or inaccuracies, were cited by both physicians and nurses and present a particular challenge. Such negative events can thwart implementation efforts once experienced by a user [33]. It may be difficult to overcome other barriers to uptake such as negative emotions or resistance, and to find ways to incorporate newly adopted technology into the current practise patterns of healthcare providers [26, 28, 29]. Jones focused on the role of management in reducing resistance through facilitation of employee participation [34]. While this is one approach, it may not be as feasible within a disjointed and continuously running healthcare system when not all providers work under the same management team, such as the physicians and nurses studied here. Alternative methods will need to be studied. Rycroft-Malone noted that skepticism is natural due to the inconclusive nature of much of scientific evidence, but that providers should reflect upon their own practise to determine what is working and what requires change or innovation [35]. The patient experience and their preferences can also be valuable in this process [30]. To that end, our pediatric providers discussed potential resistance to newly adopted technology on behalf of the patients and parents, which has emerged in other pediatric studies as well [26]. Overall, the ability to clearly state the problem being addressed and the potential benefits of the newly adopted technology to staff members will help pave the path for successful implementation.
One interesting concept that emerged in this study was whether the use of newly adopted technology was part of a standardized policy or based on an individuals personal preference. Administrators may feel that developing or incorporating newly adopted technology into patient care policies may automatically ensure effective implementation, however this does not negate the barriers to implementation and is not always successful [36-39]. A poorly thought-out approach may also lead to wasting of resources if providers fail to use the information generated by newly adopted technology or if unanticipated negative consequences occur unchecked. While clearly written policies are found to be helpful by some, they may also invoke resistance if staff members feel that use is being mandated [26, 40]. The use of incentive programmes has been described to balance these decisions [38]. Enabling early trial periods, eliciting staff feedback and facilitating staff buy in during the initial decision making process was a key implementation strategy that emerged in our study.
The ability to evaluate and monitor the implementation process is a valuable, and often missed, opportunity to enhance the adoption process [13, 15, 25, 28]. Early and continued evaluation of technology implementation could be an invaluable opportunity to address potential problems or institute further education before failure or dis-adoption occurs [30, 41]. Similar to how buy-in and trial periods are valuable to the decision-making process, early input on provider experiences, impact on practise, and consideration of practical issues such as storage can improve the chances of success of implementation [12]. The issue of storage is unique to technology and guidelines that utilize technology. To avoid this potential barrier, devices must be frequently stocked and easy to locate [29]. Similarly, it is valuable to enlist peers as superusers to be a source of continuous support and knowledge on the unit.
Implementation is a complex process and is not completely understood [42, 43]. Methods to improve implementation and knowledge translation specific to the ED and ICU are just beginning to be explored [42, 44-46]. Physicians and nurses naturally function in different roles and may use technology in different ways. Similarly, the way representatives of these professions approach newly adopted technology, solicit evidence or opinions, and work in teams may vary [12, 28, 47]. To that end, a multidisciplinary approach will be necessary in the creation of a sound and successful implementation process in order to target the learning objectives, baseline abilities and priorities of different healthcare providers [1]. Further research in effective implementation strategies will be necessary to promote the use of newly adopted technologies in acute care settings.
Our study has several limitations. The goal of qualitative inquiry is to generate ideas and hypotheses, which may later be used to inform quantitative studies. While the categories and codes generated in this study reflect the experiences of our participants, they are not meant to be generalizable to all acute care providers. However, we purposefully sampled both physicians and nurses who provide direct patient care in a variety of hospital settings such that a wide array of experiences and beliefs might be captured. While we solicited participants who primarily provided patient care, we did not ask participants to quantify their clinical hours and we did not exclude staff members who also held administrative positions, such as medical directors. Similarly, we did not statistically evaluate the differences in opinions between the different types of providers and different units, as this is not the objective of qualitative research.
5. Conclusions
Physicians and nurses in the ED and ICU described substantial variability with their experiences surrounding the introduction of newly adopted technology. This study describes several key strategies implicated in the successful implementation of newly adopted technology in acute care settings, such as preemptive staff buy-in, continual education and support, and gathering and promotion of encouraging local data. These strategies can be developed to meet the unique needs of the staff and the technology to be introduced in order to improve the likelihood of a successful implementation period. Improving implementation methods and enhancing evaluation of the implementation process are necessary for successful adoption of technology.
Acknowledgments
Melissa Langhan received an honorarium from Oridion Capnography in 2011 for participation at an expert panel meeting. She received funding from the Yale University Department of Pediatrics and the CTSA Grant Number UL1 RR024139 from the National Center for Research Resources (NCRR) and the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Appendix: Audit Trail
8.28.12
Participants: M. Langhan, A. Riera, A. Asnes, P. Schaeffer
Reviewed interview transcripts 1-3
- Discussed Interview Guide:
- ○ Ice breaker question revised to ask about a person's role on the unit to warm up to technology questions
- ○ Decision to not rephrase question on non-use based on ICU RN response
Plan for completion of interviews at Yale
10.12.12
Participants: ML, PS, AA, AR
Review of transcripts 11 and 12.
- Interview Guide:
- ○ Rephrasing question 5 – changed term “abandoned” and framed as technology that is present but not used (“Think of all the technologies that are available to you, which do you use the least”).
- ○ Decision to split “easier/harder” into 2 questions.
- Coding:
- ○ Discussion of major themes emerging from transcripts and initial concepts for codes
- ○ Discussion of initial code structure development
- ○ Leads to development of initial code structure with 6 main themes and 30 codes.
11.16.12
Participants: ML, J. Kurtz
Transcripts 1-4 reviewed.
- Code discussion:
- ○ Should we add code for ethical pressure? Stems from reps, but this has more to do with adoption and not implementation so will not include a code at this point.
- ○ Intended use vs. actual use – is there a code for this?
- ○ Perception of use- not needed. Where does this tie in?
- ○ New codes added: 3c Initial training as a technology facilitator
- ○ Code for negative consequences (5b) merged into code for emotions such as fear/anxiety (5a)
11.28.12
Participants: ML, AR, JK
Transcripts 7 and 8 reviewed.
- Code discussion:
- ○ Code 1 clarified as relating to ADOPTION of technology vs. implementation.
- ○ 1d (Mandates) split into 2 separate codes – 1d Buy in and 1e Mandates.
- ○ New theme 6 specific to capnography – reasons for non-use of this technology.
- ○ Code 4g (misunderstanding or lack of understanding of how technology is used) incorporated under theme 6.
- ○ Code 6a for high frequency use moved to facilitator code 3g.
- ○ Code 6b for low frequency use moved to barrier code 5e.
- ○ Expanded definition of 5a (negative emotions) to include general resistance, skepticism and culture change.
- ○ Code 4d (Major vs. Minor) split into two codes, 4d Major impact and 4e Minor impact.
- ○ Overall perception of value added to theme 2.
- ○ Differentiation between brand new vs. improved technology incorporated into 3b and 3f.
- ○ Decision-making pulled out into new code 4f: Who decides?
- ○ 5e Negative experiences – Supply/demand issues incorporated here.
12.4.12
Participants: ML, AR, JK
Reviewed transcript 5 and 6.
- Code discussion:
- ○ Code 2 is defined as POSITIVE comments only
- ○ Added 6e – Reference to literature or evidence for non-use of capnography
- ○ Added 1f adapter code – early adapters vs. late adapters
12.12.12
Participants: ML, AR, JK
Reviewed transcripts 13 and 14.
- Code discussion:
- ○ Added code 3h: Positive outlook.
- ○ Added code 3i: Jump start guide.
1.4.13
Participants: ML, AR, JK
Reviewed transcripts 15 and 16.
- Code discussion:
- ○ Created code 2f: “So What” when no value to new technology is implied
- ○ More clearly defined cost in 2e as actual monetary issue ($$)
- ○ Collapsed codes 3a (Superusers) and 3d (Tech support) into one category as these were frequently double coded
- ○ Included other sources of info in 3i such as refreshers, articles, etc.
1.9.13
○ Participants: ML, AR, JK
○ Reviewed transcripts 17 and 18.
- ○ Code discussion:
- ○ Clarified code 2f to include failure to meet expectations
- ○ Added code 5h: Insufficient support (education, training)
1.31.13
○ Participants: ML, AR, JK
○ Reviewed transcripts 9, 10 and 19.
- ○ Code discussion:
- ○ Will merge 1gi and 1gii as just 1g
- ○ Adding code 6h in capnography theme– lack of availability or difficulty with set up leading to non use
○ Final code structure agreed upon
Footnotes
Declaration of Interest:
The remaining authors report no declarations of interest.
Contributor Information
Melissa L. Langhan, Department of Pediatrics, Section of Emergency Medicine, Yale University School of Medicine.
Antonio Riera, Department of Pediatrics, Section of Emergency Medicine, Yale University School of Medicine.
Jordan C. Kurtz, St. George's University School of Medicine.
Paula Schaeffer, Department of Pediatrics, Yale University School of Medicine.
Andrea G. Asnes, Department of Pediatrics, Yale University School of Medicine.
References
- 1.Krimsky WS, Mroz IB, McIlwaine JK, et al. A model for increasing patient safety in the intensive care unit: increasing the implementation rates of proven safety measures. Qual Saf Health Care. 2009;18(1):74–80. doi: 10.1136/qshc.2007.024844. [DOI] [PubMed] [Google Scholar]
- 2.Bowen SA, Saunders RP, Richter DL, et al. Assessing levels of adaptation during implementation of evidence-based interventions: introducing the Rogers-Rutten framework. Health Educ Behav. 2010;37(6):815–830. doi: 10.1177/1090198110366002. [DOI] [PubMed] [Google Scholar]
- 3.Duff LA, Kitson AL, Seers K, et al. Clinical guidelines: an introduction to their development and implementation. J Adv Nurs. 1996;23(5):887–895. doi: 10.1046/j.1365-2648.1996.00875.x. [DOI] [PubMed] [Google Scholar]
- 4.Gale BV, Schaffer MA. Organizational readiness for evidence-based practise. J Nurs Adm. 2009;39(2):91–97. doi: 10.1097/NNA.0b013e318195a48d. [DOI] [PubMed] [Google Scholar]
- 5.Hader JM, White R, Lewis S, et al. Doctors' views of clinical practise guidelines: a qualitative exploration using innovation theory. J Eval Clin Pract. 2007;13(4):601–606. doi: 10.1111/j.1365-2753.2007.00856.x. [DOI] [PubMed] [Google Scholar]
- 6.Hovmand PS, Gillespie DF. Implementation of evidence-based practise and organizational performance. J Behav Health Serv Res. 2010;37(1):79–94. doi: 10.1007/s11414-008-9154-y. [DOI] [PubMed] [Google Scholar]
- 7.Rhea S. 2010 outlook. Devices: time for innovation. Mod Healthc. 2010;40(1):25. [PubMed] [Google Scholar]
- 8.Bergsland J. Major innovations and trends in the medical device sector. Acta Inform Med. 2012;20(1):44–46. doi: 10.5455/aim.2012.20.44-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greer AL. Adoption of medical technology. The hospital's three decision systems. Int J Technol Assess Health Care. 1985;1(3):669–680. doi: 10.1017/s0266462300001562. [DOI] [PubMed] [Google Scholar]
- 10.Greer AL. The state of the art versus the state of the science. The diffusion of new medical technologies into practise. Int J Technol Assess Health Care. 1988;4(1):5–26. doi: 10.1017/s0266462300003202. [DOI] [PubMed] [Google Scholar]
- 11.Crow G. Diffusion of innovation: the leaders' role in creating the organizational context for evidence-based practise. Nurs Adm Q. 2006;30(3):236–242. doi: 10.1097/00006216-200607000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Kyratsis Y, Ahmad R, Holmes A. Technology adoption and implementation in organisations: comparative case studies of 12 English NHS Trusts. BMJ Open. 2012;2(2):e000872. doi: 10.1136/bmjopen-2012-000872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roback K, Gaddlin PO, Nelson N, et al. Adoption of medical devices: perspectives of professionals in Swedish neonatal intensive care. Technol Health Care. 2007;15(3):157–179. [PubMed] [Google Scholar]
- 14.Laupacis A, Feeny D, Detsky AS, et al. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992;146(4):473–481. [PMC free article] [PubMed] [Google Scholar]
- 15.Donaldson NE, Rutledge DN, Ashley J. Outcomes of adoption: measuring evidence uptake by individuals and organizations. Worldviews Evid Based Nurs. 2004;1(Suppl 1):S41–51. doi: 10.1111/j.1524-475X.2004.04048.x. [DOI] [PubMed] [Google Scholar]
- 16.Edmondson A, Bohmer R, Pisano G. Disrupted Routines: Team Learning and New Technology Implementation in Hospitals. Admin Sci Quarterly. 2001;46(4):685–716. [Google Scholar]
- 17.Patton MQ. Qualitative Research & Evaluation Methods. 3rd ed. Sage PUblications; Thousand Oaks, CA: 2002. [Google Scholar]
- 18.Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119(10):1442–1452. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 19.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lester S. An introduction to phenomenological research. Stan Lester Developments; Tauton, UK: 1999. [Google Scholar]
- 21.Creswell JW. Qualitative Inquiry & Research Design: Choosing Among Five Approaches. 2nd ed. Sage Publications; Thousand Oaks, CA: 2007. [Google Scholar]
- 22.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rogers EM. Diffusion of Inovations. Fifth edition ed. Free Press; New York, NY: 2003. [Google Scholar]
- 24.Collins BA, Hawks JW, Davis R. From theory to practise: identifying authentic opinion leaders to improve care. Manag Care. 2000;9(7):56–58, 61-52. [PubMed] [Google Scholar]
- 25.Dearing JW. Evolution of diffusion and dissemination theory. J Public Health Manag Pract. 2008;14(2):99–108. doi: 10.1097/01.PHH.0000311886.98627.b7. [DOI] [PubMed] [Google Scholar]
- 26.Scott SD, Osmond MH, O'Leary KA, et al. Barriers and supports to implementation of MDI/spacer use in nine Canadian pediatric emergency departments: a qualitative study. Implement Sci. 2009;4:65. doi: 10.1186/1748-5908-4-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carlbom DJ, Rubenfeld GD. Barriers to implementing protocol-based sepsis resuscitation in the emergency department--results of a national survey. Crit Care Med. 2007;35(11):2525–2532. doi: 10.1097/01.ccm.0000298122.49245.d7. [DOI] [PubMed] [Google Scholar]
- 28.Janssen MA, van Achterberg T, Adriaansen MJ, et al. Factors influencing the implementation of the guideline triage in emergency departments: a qualitative study. J Clin Nurs. 2012;21(3-4):437–447. doi: 10.1111/j.1365-2702.2011.03921.x. [DOI] [PubMed] [Google Scholar]
- 29.Olajos-Clow J, Szpiro K, Julien B, et al. Emergency department adult asthma care pathway: healthcare providers' perceived utility and barriers to implementation. Adv Emerg Nurs J. 2009;31(1):44–53. doi: 10.1097/TME.0b013e3181946f76. [DOI] [PubMed] [Google Scholar]
- 30.Cabana MD, Flores G. The role of clinical practise guidelines in enhancing quality and reducing racial/ethnic disparities in paediatrics. Paediatr Respir Rev. 2002;3(1):52–58. doi: 10.1053/prrv.2002.0182. [DOI] [PubMed] [Google Scholar]
- 31.McGee JB, Kanter SL. How we develop and sustain innovation in medical education technology: Keys to success. Med Teach. 2011;33(4):279–285. doi: 10.3109/0142159X.2011.540264. [DOI] [PubMed] [Google Scholar]
- 32.Olson KE, O'Brien MA, Rogers WA, et al. Diffusion of Technology: Frequency of Use for Younger and Older Adults. Ageing Int. 2011;36(1):123–145. doi: 10.1007/s12126-010-9077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Veer AJ, Fleuren MA, Bekkema N, et al. Successful implementation of new technologies in nursing care: a questionnaire survey of nurse-users. BMC Med Inform Decis Mak. 2011;11:67. doi: 10.1186/1472-6947-11-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jones D, Smith M. Implementing New Technology.. Proceedings of the Human Factors and Ergonomics Society 48th Annual Meeting; New Orleans, LA. 2004; Sage Publications; 2004. pp. 1601–1604. [Google Scholar]
- 35.Rycroft-Malone J, Kitson A, Harvey G, et al. Ingredients for change: revisiting a conceptual framework. Qual Saf Health Care. 2002;11(2):174–180. doi: 10.1136/qhc.11.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Masse LC, Naiman D, Naylor PJ. From policy to practise: implementation of physical activity and food policies in schools. Int J Behav Nutr Phys Act. 2013;10:71. doi: 10.1186/1479-5868-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kumar S, Aldrich K. Overcoming barriers to electronic medical record (EMR) implementation in the US healthcare system: A comparative study. Health Informatics J. 2010;16(4):306–318. doi: 10.1177/1460458210380523. [DOI] [PubMed] [Google Scholar]
- 38.Doolan DF, Bates DW. Computerized physician order entry systems in hospitals: mandates and incentives. Health Aff (Millwood) 2002;21(4):180–188. doi: 10.1377/hlthaff.21.4.180. [DOI] [PubMed] [Google Scholar]
- 39.Studnicki J, Remmel R, Campbell R, et al. The impact of legislatively imposed practise guidelines on cesarean section rates: the Florida experience. Am J Med Qual. 1997;12(1):62–68. doi: 10.1177/0885713X9701200111. [DOI] [PubMed] [Google Scholar]
- 40.Bierstock SR. A great idea turning bad. EHR mandates would feel better if they came with tort reform. Med Econ. 2009;86(16):34. [PubMed] [Google Scholar]
- 41.Harvey G, Kitson A. Achieving improvement through quality: an evaluation of key factors in the implementation process. J Adv Nurs. 1996;24(1):185–195. doi: 10.1046/j.1365-2648.1996.15825.x. [DOI] [PubMed] [Google Scholar]
- 42.Weinert CR, Mann HJ. The science of implementation: changing the practise of critical care. Curr Opin Crit Care. 2008;14(4):460–465. doi: 10.1097/MCC.0b013e3283079eb5. [DOI] [PubMed] [Google Scholar]
- 43.Lukas CV, Mohr DC, Meterko M. Team effectiveness and organizational context in the implementation of a clinical innovation. Qual Manag Health Care. 2009;18(1):25–39. doi: 10.1097/01.QMH.0000344591.56133.90. [DOI] [PubMed] [Google Scholar]
- 44.Scott S, Hartling L, Grimshaw J, et al. Improving outcomes for ill and injured children in emergency departments: protocol for a program in pediatric emergency medicine and knowledge translation science. Implement Sci. 2009;4:60. doi: 10.1186/1748-5908-4-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sinuff T, Cook DJ, Giacomini M. How qualitative research can contribute to research in the intensive care unit. J Crit Care. 2007;22(2):104–111. doi: 10.1016/j.jcrc.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 46.Diner BM, Carpenter CR, O'Connell T, et al. Graduate medical education and knowledge translation: role models, information pipelines, and practise change thresholds. Acad Emerg Med. 2007;14(11):1008–1014. doi: 10.1197/j.aem.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 47.Holleman G, Poot E, Mintjes-de Groot J, et al. The relevance of team characteristics and team directed strategies in the implementation of nursing innovations: a literature review. Int J Nurs Stud. 2009;46(9):1256–1264. doi: 10.1016/j.ijnurstu.2009.01.005. [DOI] [PubMed] [Google Scholar]


