Abstract
Background/Aims
Hypokalemia and hyperkalemia are often noted in chronic kidney disease (CKD) patients but their impact on mortality and end stage renal disease (ESRD) is less well understood. We aimed to study the associations between potassium disorders, and mortality and progression to ESRD in a CKD population.
Methods
Using our Electronic Health Record-based CKD registry, 36,359 patients with eGFR < 60 ml/min/1.73m2 and potassium levels measured from January 1, 2005 to September 15, 2009 were identified. We examined factors associated with hypokalemia (<3.5 mmol/l) and hyperkalemia (>5.0 mmol/l) using logistic regression models and associations between serum potassium levels (both as continuous and categorical variables) and all-cause mortality or ESRD using Cox-proportional hazards models.
Results
Serum potassium <3.5 mmol/l was noted among 3% and >5.0 mmol/l among 11% of the study population. In the multivariable logistic regression analysis, lower eGFR, diabetes and use of ACE inhibitors or Angiotensin-Receptor Blockers were associated with higher odds of having hyperkalemia. Heart failure and African American race were associated with higher odds of hypokalemia. After adjustment for covariates including kidney function, serum potassium <4.0 mmol/l and >5.0 mmol/l were significantly associated with increased mortality risk but there was no increased risk for progression to ESRD. Time-dependent repeated measures analysis confirmed these findings. When potassium was examined as a continuous variable, there was a U-shaped association between serum potassium levels and mortality.
Conclusion
In patients with stage 3–4 CKD, serum potassium level <4.0 mmol/l and >5.0 mmol/l are associated with higher mortality but not with ESRD.
Keywords: Potassium, mortality, ESRD, chronic kidney disease
Background
The kidneys play a crucial role in potassium homeostasis and the importance of their contribution in the maintenance of potassium balance is reflected by the high rates of potassium disorders in patients with decreased kidney function (1, 2). Indeed, individuals with chronic kidney disease (CKD) and those with end-stage renal disease (ESRD) can experience both hyperkalemia and hypokalemia; the former typically occurs by virtue of their low kidney function or as a consequence of drugs such as Angiotensin Converting Enzyme inhibitors (ACEIs) or Angiotensin-Receptor Blockers (ARBs) while the latter is typically a consequence diuretic administration (3).
Among dialysis patients, hyperkalemia has been associated with higher mortality due to its arrhythmogenic effects (4, 5). Hypokalemia has also been linked to higher mortality in dialysis patients, not only because of the electrophysiological effects of potassium, but also because hypokalemia often reflects a poor underlying nutritional status (6). In CKD patients not on dialysis, however, the impact of potassium disorders on outcomes is unclear. Recent evidence suggests that the relationship between serum potassium and mortality follows a U-shaped curve, wherein both low and high serum potassium are associated with an increase in mortality (7, 8). However, the data is heterogeneous with a variable follow-up ranging from 1 day to 4 years and variable number of potassium values per patient (9). In addition, low serum potassium has been postulated to be a risk factor for the progression of CKD, as it had been shown to induce kidney damage via modulation of renal inflammation and impaired angiogenesis (10–12). To our knowledge, the association between serum potassium and ESRD has not been studied in detail. Therefore, we examined the associations between serum potassium and all-cause mortality and ESRD in a cohort of stage 3 and stage 4 CKD patients following in our health care system.
Methods
We conducted an analysis using our preexisting Electronic Health Record (EHR)-based CKD registry. The development and validation of our EHR-based CKD registry at Cleveland Clinic have been described in detail elsewhere (13).
Study Population
Patients who met the following criteria from January 1, 2005 to September 15, 2009, were included in the study population: (1) had at least one face-to-face outpatient encounter with a Cleveland Clinic health care provider, (2) had two or more estimated GFR (eGFR) values <60 ml/min per 1.73 m2 more than 90 days apart, and (3) had a potassium measured on the date of the second eGFR <60 ml/min per 1.73m2. Patients aged <18 years old, who entered the registry after 9/15/2009 and those who were diagnosed with ESRD needing dialysis or renal transplant before the date of second eGFR <60 ml/min/1.73 m2 were excluded.
Definitions and Outcome Measures
Renal Function
We applied the CKD-EPI equation to patients in our health system who had two outpatient serum creatinine levels between January 1, 2005, and September 15, 2009, to calculate eGFR (14). All creatinine measurements were performed by the modified kinetic Jaffe reaction, using a Hitachi D 2400 Modular Chemistry Analyzer (Roche Diagnostics, Indianapolis, IN) in our laboratory. CKD was defined according to current guidelines as follows: stage 3 CKD (eGFR 30–59 ml/min per 1.73 m2) and stage 4 CKD (eGFR 15– 29 ml/min per 1.73 m2). We further categorized stage 3 into CKD stage 3a (eGFR 45–59 ml/min per 1.73 m2) and stage 3b (eGFR 30–44 ml/min per 1.73 m2).
Serum Potassium
Only outpatient serum potassium laboratory measures obtained with a same reference range were included in this analysis. Serum potassium levels measured on the day of CKD confirmation (second eGFR <60 ml/min per 1.73 m2 at least 90 days after the first eGFR), as described, were used for the analysis in which single potassium measured was considered. For our time-dependent repeated measures analysis, we included the baseline potassium as well as the first potassium with appropriate reference range measured each month during the study follow-up. We used carry-forward values to fill in data for months with no potassium measurement.
Comorbid Conditions and Laboratory Parameters
Demographic details were extracted from the EHR. Diabetes mellitus, hypertension, coronary artery disease, and other comorbid conditions were defined using pre-specified criteria and validated (13). Serum potassium levels and other relevant outpatient laboratory details were obtained from our electronic laboratory records.
Outcomes
The primary outcomes of interest, all-cause mortality and ESRD were ascertained from our EHR and linkage of our CKD registry with the Social Security Death Index and United States Renal Data Services (USRDS). Patients were followed from their date of inclusion in the registry (date of second qualifying eGFR) until September 15, 2009.
Statistical Analyses
CKD patients with measured outpatient serum potassium values at the time of second eGFR <60 ml/min per 1.73 m2 were further classified into three groups: <3.5 mmol/l, 3.5–3.9 mmol/l, 4.0–4.9 mmol/l, 5.0–5.5 mmol/l and >5.5 mmol/l based on clinical relevance and previous reports. Associations of the baseline characteristics for these groups were assessed using Chi-square and ANOVA tests for categorical and continuous variables respectively.
Two separate logistic regression analyses were conducted to examine the association of low (<3.5 mmol/l) or high (>5.0 mmol/l) serum potassium levels with potential covariates. For each of these models, the reference group was all patients with normal serum potassium levels based on our laboratory reference values (3.5–5 mmol/l). Covariates were based on information known prior to second eGFR<60 and chosen a priori based on factors previously shown or thought to be related to both serum potassium, ESRD and mortality. These include age, gender, race, body mass index (BMI), eGFR, diabetes, hypertension, malignancy, coronary artery disease, heart failure, chronic obstructive pulmonary disease (COPD) and/or asthma, use of ACE/ARB, and use of Beta Blockers.
To evaluate whether survival and ESRD among persons with CKD was associated with serum potassium levels, we used Kaplan-Meier plots and log-rank tests with date of second eGFR <60 ml/min/1.73 m2 as the time of origin. Progression to ESRD and pre-ESRD death are competing events; therefore we fitted cumulative incidence functions that adjust for competing risks and compared these results to the traditional cause specific analysis. In addition, a separate analysis that included all deaths (both before and after ESRD) was also conducted. We used Cox proportional hazards models to assess the association between serum potassium and mortality and ESRD while adjusting for other covariates mentioned above, as well as cerebrovascular disease, peripheral vascular disease, potassium sparing diuretics, non-potassium sparing diuretics, potassium supplementation, serum bicarbonate, log glucose and albumin. To incorporate serum potassium results obtained after inception we fitted a Cox proportional hazards model with time-dependent repeated measures of potassium while adjusting for all variables mentioned before. We used splines to relax linearity assumptions for continuous variables included in the models. We also examined the relationship between continuous baseline serum potassium and each outcome using restricted cubic splines.
We tested 2-way interactions between baseline serum potassium and the following covariates: age, gender, race, diabetes and eGFR in the adjusted Cox proportional hazards model. 0.3% of patients had missing serum glucose and/or bicarbonate data and 13% of patients had missing albumin. We used mean value imputation to include all patients in the cox model. To evaluate the effect of the imputation we also fit a model with time-dependent serum potassium with complete case data. We did not adjust for proteinuria in our main models because we only had data in 49% of the sample. However, we performed a sensitivity analysis fitting cox models with time-dependent serum potassium as described above and adjusting for proteinuria in a sensitivity analysis.
All data analyses were conducted using Unix SAS version 9.2 (SAS Institute, Cary, NC) and R 3.0.1 (The R Foundation for Statistical Computing, Vienna, Austria). The cmprsk package was used for competing risk analysis. The CKD registry and this study were approved by the Cleveland Clinic Institutional Review Board.
Results
Patient characteristics
There were 42,912 patients with stage 3 and 4 CKD from our CKD registry, and of those, 36,359 (85%) had serum potassium levels measured on the date of second eGFR <60 ml/min per 1.73 m2 with reference ranges 3.5–5 mmol/l and constituted the study population (Supplemental Figure 1). Patients who had had measurements with different assays (n=4,725, 11%) were excluded. Mean age of the study population was 72 ± 11.9 years with 55% being females and 13% African Americans. Demographic variables and comorbid conditions were significantly different among patients with various ranges of serum potassium levels (Table 1). Serum potassium <3.5mmol/l was noted among 3% and >5.0 mmol/l was observed among 11% of the study population.
Table 1.
Characteristics of study population based on serum potassium levels
| Variable~ | Total (N=36359) | <3.5 (N=1106) | 3.5–3.9 (N=5392) | 4–4.9 (N=24717) | 5–5.4 (N=3931) | >5.5 (N=1213) |
|---|---|---|---|---|---|---|
| Age | 72.3±11.9 | 68.7±13.4 | 72.0±11.9 | 72.7±11.7 | 71.9±12.1 | 70.4±12.9 |
| Male gender | 45.1 | 33.5 | 37.1 | 45.8 | 52.7 | 53.2 |
| African American | 13.2 | 26.3 | 18.1 | 11.6 | 11.2 | 19.3 |
| eGFR | 47.0±10.4 | 46.2±11.1 | 48.3±9.8 | 47.6±10.0 | 43.8±11.4 | 39.9±12.2 |
| CKD stage | ||||||
| Stage 3a (45–59) | 64.6 | 63.3 | 69.6 | 66.8 | 52.0 | 38.8 |
| Stage 3b (30–44) | 26.9 | 26.4 | 24.4 | 25.9 | 33.6 | 36.8 |
| Stage 4 (15–29) | 8.5 | 10.3 | 6.0 | 7.3 | 14.4 | 24.4 |
| BMI* kg/m2 | 29.2±6.4 | 29.4±7.0 | 29.3±6.5 | 29.2±6.3 | 29.0±6.4 | 29.5±7.5 |
| BMI group | ||||||
| <18.5 kg/m2 | 1.3 | 1.4 | 1.3 | 1.2 | 1.7 | 2.3 |
| 18.5–24.9 kg/m2 | 23.4 | 26.6 | 23.4 | 23.1 | 23.9 | 25.0 |
| 25–29.9 kg/m2 | 34.8 | 29.6 | 33.3 | 35.4 | 35.9 | 31.6 |
| 30+ kg/m2 | 36.2 | 38.2 | 37.1 | 36.2 | 34.3 | 36.0 |
| Missing | 4.3 | 4.3 | 4.9 | 4.1 | 4.1 | 5.1 |
| Smoking status | ||||||
| No | 76.2 | 68.1 | 73.7 | 77.2 | 76.4 | 73.0 |
| Yes | 6.7 | 8.1 | 6.9 | 6.4 | 7.3 | 8.6 |
| Missing | 17.1 | 23.8 | 19.3 | 16.4 | 16.3 | 18.5 |
| COPD | 38.6 | 9.3 | 9.1 | 8.4 | 8.5 | 8.7 |
| Diabetes | 21.9 | 16.3 | 15.9 | 21.7 | 29.5 | 34.2 |
| Hypertension | 84.3 | 76.9 | 81.9 | 84.8 | 86.9 | 83.8 |
| Coronary artery disease | 21.5 | 14.1 | 16.9 | 21.8 | 27.3 | 24.1 |
| Congestive heart failure | 8.2 | 9.6 | 7.3 | 7.9 | 9.6 | 11.2 |
| Cerebrovascular disease | 9.0 | 6.1 | 7.6 | 9.2 | 10.3 | 10.6 |
| Peripheral vascular disease | 2.7 | 2.1 | 1.9 | 2.7 | 3.6 | 4.1 |
| Malignancy | 24.4 | 24.7 | 24.2 | 24.4 | 24.2 | 24.8 |
| Use of ACEI/ARBs | 62.1 | 50.6 | 55.1 | 62.2 | 71.2 | 73.0 |
| Use of Beta Blockers | 54.7 | 49.6 | 50.8 | 54.5 | 61.0 | 59.9 |
| Use of Statins | 55.6 | 47.0 | 49.5 | 56.6 | 60.4 | 56.8 |
| Diuretic use | 65.9 | 75.9 | 75.1 | 63.8 | 63.1 | 67.4 |
| K supplement | 13.3 | 30.8 | 19.5 | 11.9 | 10.1 | 10.2 |
| Serum Sodium mmol/l* | 139.4±3.2 | 138.9±4.2 | 139.6±3.2 | 139.5±3.0 | 139.0±3.5 | 137.9±4.4 |
| Serum bicarbonate mmol/l* | 26.0±3.3 | 27.5±4.2 | 26.8±3.3 | 26.1±3.1 | 25.0±3.4 | 23.6±4.1 |
| Serum albumin g/dl* | 4.1±0.46 | 3.9±0.61 | 4.0±0.50 | 4.1±0.44 | 4.1±0.47 | 4.0±0.54 |
| Serum glucose mg/dl* | 100.0[89.0,120.0] | 106.0[91.0,129.0] | 101.0[89.0,120.0] | 99.0[88.0,117.0] | 101.0[89.0,126.0] | 103.0[88.0,137.0] |
All variables presented as % unless otherwise specified.
Data not available for all subjects.
Missing values: BMI = 1562, Serum Sodium mmol/l = 106, Serum CO2 mmol/l = 110, Glucose mg/dl = 105, albumin 4,751. Values presented as Mean ± SD, Median [P25, P75], or N (column %). All variables statistically significant across groups except continuous BMI, COPD/asthma, and malignancy
Factors associated with low and high serum potassium levels
Low serum potassium levels (<3.5 mmol/l)
In the multivariable analysis, the following variables were associated with higher odds of having low potassium levels compared to normal: African American race, lower eGFR, malignancy, and heart failure (Table 2). Conversely, the following variables were associated with having lower odds of having low serum potassium levels: older age, male gender, being overweight, diabetes, hypertension and use of ACE/ARB (Table 2).
Table 2.
Associations of low (K <3.5 mmol/l) and high serum potassium levels (K >5 mmol/l) in non-dialysis dependent CKD
| Effect | Hypokalemia OR (95% CI)* | Hyperkalemia (OR (95% CI)* |
|---|---|---|
| Age (per 10 years incremental increase) | 0.80 (0.76, 0.84) | 0.90 (0.87, 0.92) |
| Male sex | 0.65 (0.57, 0.74) | 1.37 (1.28, 1.47) |
| African American race | 2.34 (2.03, 2.69) | 0.92 (0.83, 1.02) |
| eGFR (per 5 ml/min decrease) | 1.06 (1.03, 1.09) | 1.25 (1.23, 1.27) |
| BMI group (Ref: 18.5–24.9 kg/m2) | ||
| <18.5 kg/m2 | 0.74 (0.43, 1.25) | 1.60 (1.23, 2.08) |
| 18.5–24.9 kg/m2 | Ref | Ref |
| 25–29.9 kg/m2 | 0.80 (0.68, 0.94) | 0.87 (0.80, 0.96) |
| ≥30 kg/m2 | 0.87 (0.74, 1.02) | 0.77 (0.70, 0.85) |
| Missing | 0.86 (0.63, 1.18) | 0.97 (0.81, 1.16) |
| Diabetes | 0.77 (0.65, 0.92) | 1.53 (1.41, 1.66) |
| Hypertension | 0.75 (0.64, 0.88) | 1.03 (0.93, 1.15) |
| Malignancy | 1.17 (1.01, 1.35) | 1.12 (1.03, 1.21) |
| Coronary artery disease | 0.84 (0.70, 1.02) | 1.09 (1.00, 1.19) |
| Congestive heart failure | 1.50 (1.20, 1.87) | 0.95 (0.84, 1.07) |
| COPD | 1.13 (0.91, 1.39) | 1.02 (0.90, 1.16) |
| Use of ACEI/ARBs | 0.71 (0.62, 0.82) | 1.40 (1.29, 1.52) |
| Use of Beta Blockers | 1.04 (0.91, 1.19) | 1.06 (0.98, 1.14) |
High serum potassium levels (>5.0 mmol/l)
In the multivariable analysis, the following variables were associated with higher odds of having high potassium levels compared to normal: male gender, lower eGFR, BMI <18.5 kg/m2, diabetes, malignancy, and use of ACE/ARB (Table 2). The following variables were associated with having lower odds of having high serum potassium levels: higher age and higher BMI (Table 2).
Serum potassium levels, ESRD and all-cause mortality
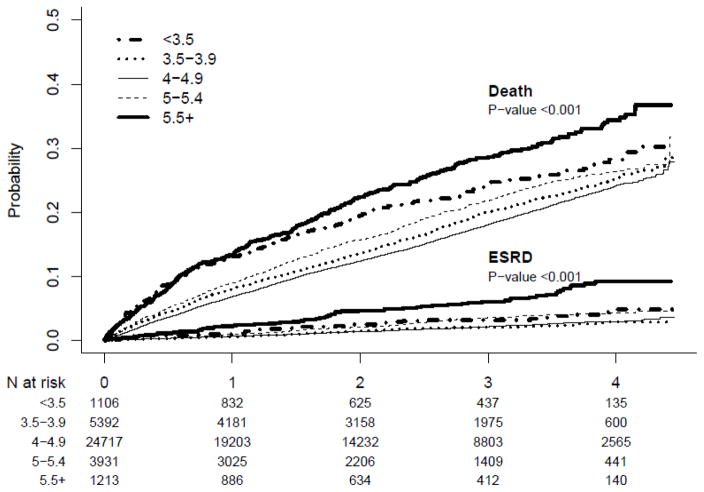
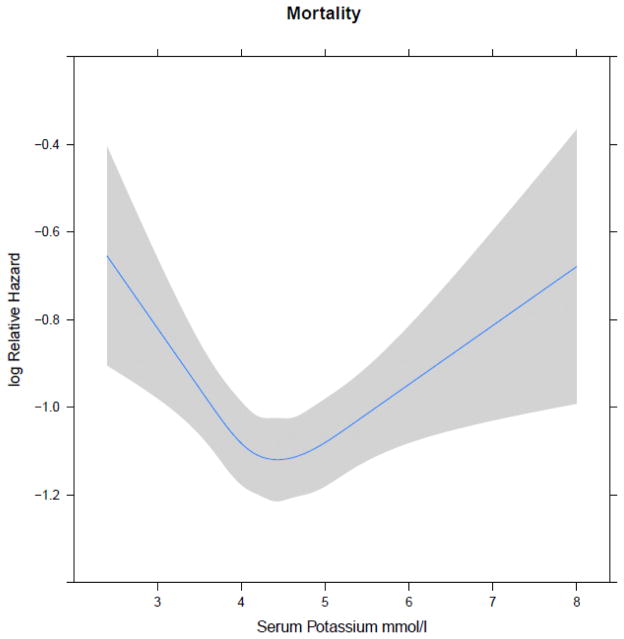
Among our study population, 6,114 of them died before reaching ESRD and 772 reached ESRD during an average follow-up of 2.3 years. A total of 6,379 patients died overall. Both the Kaplan-Meier and competing risk analyses showed a significant difference in overall mortality and ESRD among those with different potassium levels (p<0.001, Figure 1) and the results were similar in both analytical approaches. In the multivariate model (time-dependent repeated measures analysis) adjusting for demographics, comorbid conditions, medications use, lower levels of serum potassium (<3.5 and 3.5–3.9 mmol/l) were associated with higher risk for mortality. Similar higher risk for mortality was noted for those with higher levels of serum potassium (5.0 –5.4 and >5.5 mmol/l) (Table 3). No such associations between potassium levels and ESRD were noted (Table 3). In a model in which only baseline serum potassium was considered as the explanatory variable, serum potassium levels >5.5 mmol/l was associated with higher risk for death (Supplemental table 1). There was a U-shaped association between serum potassium levels and mortality when serum potassium was examined as a continuous variable (Figure 2).
Figure 1.
Cumulative incidence curve for death and ESRD for various categories of serum potassium (Graph shows that the unadjusted risk for mortality and ESRD differ among patients with different serum potassium levels)
Table 3.
Associations between serum potassium levels and outcomes (ESRD and death) in non-dialysis dependent CKD
| Overall Mortality HR (95%CI) | ESRD HR (95%CI) | |
|---|---|---|
| <3.5 mmol/l | 1.95 (1.74, 2.18) | 0.97 (0.67, 1.40) |
| 3.5–3.9 mmol/l | 1.16 (1.09, 1.25) | 1.39 (1.13, 1.70) |
| 4–4.9 mmol/l | Reference | Reference |
| 5–5.4 mmol/l | 1.12 (1.03, 1.21) | 1.17 (0.96, 1.42) |
| ≥5.5 mmol/l | 1.65 (1.48, 1.84) | 1.20 (0.91, 1.58) |
Models adjusted for age, gender, race, diabetes, hypertension, malignancy, Congestive heart failure, coronary artery disease, COPD/asthma, BMI group, history of ACE/ARB, potassium sparing diuretics, not potassium sparing diuretics, beta blockers, eGFR, potassium supplementation, cerebrovascular disease, peripheral vascular disease, serum bicarbonate, log glucose and albumin. Mean value imputation was used for serum bicarbonate, glucose and albumin
First potassium per patient per month was used in the analysis. Missing data is filled as follows: potassium value is carried forward until a new potassium value is observed. All subjects and all follow up are included regardless of the amount of time elapsed since last potassium measurement. Median time from last potassium measured to death/censor is 5.4 months.
Figure 2.
Relationship between serum potassium (as a continuous measure) and all-cause mortality (The graph shows a U-shaped relationship between continuous potassium and mortality. Splines were used to allow for non-linear relationship. Knots were placed at potassium values of 3.6, 4.1, 4.4, 4.7 and 5.3).
Effect modification by age and CKD stage
We found significant 2-way interactions between serum potassium and age and eGFR on mortality, which indicated that the increased mortality hazard associated with abnormal levels of serum potassium was different at different ages (p=0.04) and eGFR stages (p<0.001). Age appears to modify the association with younger patients showing stronger association and seems to either attenuate or lose of statistical significance in elderly population (Supplemental table 2). The interaction with CKD stage suggested that serum potassium is associated with increased mortality among patients with stage 3a but not in other stages of CKD (data not shown).
Sensitivity analyses
In a sensitivity analysis in which we included patients who had proteinuria data (n=17,790), similar results were noted (data not shown). Results from the model including only patients with complete data (complete case analyses) were qualitatively similar to those in the model using mean value imputation and a class level for missing BMI groups.
Discussion
In this large cohort of patients with stage 3 and 4 CKD, the prevalence of hypokalemia (K <3.5 mmol/L) and hyperkalemia (K >5.0 mmol/L) were 3% and 11% respectively. Hyperkalemia was more frequently observed in patients with lower eGFR, treated with ACEI/ARB and those with conditions known to cause cellular shifts such as diabetes. On the other hand, hypokalemia was more often seen in African Americans and in patients taking diuretics. We observed a U-shaped association between serum potassium and death with both lower and higher levels of potassium being associated with increased risk of death. However, neither low nor high serum potassium levels were associated with progression to ESRD.
Hypokalemia and hyperkalemia are frequently observed in patients with CKD. As the eGFR falls, the renal excretion of potassium is reduced, and the prevalence of hyperkalemia increases from 2% in patients with eGFR > 60 ml/min/1.73m2 to 42% in patients with eGFR <20 ml/min/1.73 m2(15, 16). Other factors that have been linked to hyperkalemia include cellular shifts from underlying acidosis or diabetes and treatment with RAAS blockers such as ACEI or ARB (17–20). Hypokalemia on the other hand, is often seen in the setting of diuretic use and has been proposed as a marker of poor nutritional status (21). Our findings were concordant with the previous studies: hyperkalemia was more frequently observed in patients with lower GFR, treated with ACEI/ARB and those with diabetes. These same factors were associated with lesser risk for hypokalemia. On the other hand, diuretics were associated with higher odds of hypokalemia and lower odds of hyperkalemia. Black race was also associated with higher odds of hypokalemia. Previous reports have shown that African Americans have lower mean serum potassium concentration than whites in non-CKD population and the risk for unprovoked hypokalemia was five times that of Whites (22–25). Our findings extend this to African Americans with CKD and suggest the need to monitor them closely for development of hypokalemia.
Hypokalemia has been previously linked to increased mortality in patients with heart failure and acute myocardial infarction (26, 27). In a propensity-matched analysis, Bowling et al., reported an association between low serum potassium (defined as <4 mmol/l) and mortality in those with CHF and CKD (28). In a CKD population with mean eGFR of 25.4 ml/min/1.73 m2, an association between low serum potassium and mortality was reported. Our findings extend these observations to those without heart failure and to those with stage 3 CKD. Low serum potassium levels affect the myocardial resting membrane potential which can lead to ventricular arrhythmias and sudden cardiac death (29). Low potassium levels can also be a reflection of a poor nutritional status, which in turn portends poor prognosis (30) but in the repeated measures analysis, the association between hypokalemia (both in the 3.5–3.9 mmol/l and <3.5 mmol/l) and mortality remains despite adjusting for serum albumin.
In our study population, serum potassium >5.0 mmol/l is also associated with increased mortality in non-dialysis-dependent CKD patients, a finding that is typically attributed to the arrhythmogenic effects of potassium. In a secondary analysis of the Renal Research Institute (RRI) study CKD cohort, an increased risk of the composite of death or cardiovascular events requiring hospitalization was observed but did not show an increase in overall mortality (8). The differences between our study and the RRI study could be attributed to the reference ranges used (4–5.5 mmol/l in RRI vs. 4.0–4.9 mmol/l in our study). However, another study included hospitalized CKD patients and demonstrated higher risk for death within 1 day among those with hyperkalemia (31). Our study shows a clear association between serum potassium and mortality with hypokalemia <4.0 mmol/L and hyperkalemia ≥5.0 mmol/L (Table 3).
However, when looking at the interaction between age groups and potassium, we found a statistically significant association between serum potassium of 3.5–3.9 mmol/L and mortality for patients aged <80 years old but not in those aged >80 (Supplemental Table 2). A potential explanation could relate to the high morbidity load of patients aged above 80 that would put them at risk of death regardless of their serum potassium. Baseline kidney function seem to modify the associations between serum potassium and outcomes as patients with hypo/hyperkalemia and stage 3a CKD (eGFR 45–59 ml/min/1.73m2) were more likely to die than those with stage 3b and stage 4 CKD (eGFR < 45 ml/min/1.73m2). Such findings could be attributed to the fact that higher occurrence of chronic hyperkalemia in CKD patients might be better tolerated than acute hyperkalemia. This in turn might lead to a reduced sensitivity to cardiac complications (32). Whether such phenomenon exists for hypokalemia warrants further studies.
It has been suggested that potassium disorders could lead to progression of renal disease. Hypokalemia in particular could contribute to interstitial renal scarring and experimental studies suggest that chronic hypokalemia can lead to renal fibrosis via modulation of renal inflammation and local activation of the RAAS (11, 33, 34). Current clinical evidence provide conflicting findings as some studies suggest that hypokalemia was associated with progression to ESRD, while others did not observe such association after adjustment for nutritional indices (serum albumin) (8, 35). Hayes et al noted that hypokalemia was associated with renal progression but the association with hard renal outcome, such as reaching ESRD was unclear (36). Table 3 shows that there could be a higher risk for ESRD in those with serum potassium 3.5–3.9 mmol/l but the overall p-value for the model wasn’t significant suggesting that no associations exist between hypokalemia and ESRD. Despite the large sample size and inclusion of relevant confounders, we didn’t observe an association between hypokalemia and kidney disease progression.
Strengths of this analysis include a large diverse patient population with stage 3 and 4 CKD, availability of several confounding variables and the use of time-dependent repeated measures analyses. However, retrospective analyses are prone to residual confounding. While we included several variables that could affect serum potassium levels and are related to mortality (diabetes, serum bicarbonate, medications etc.), we lacked details about nutritional data. Further, our patients have been followed in a health care system and hence these data might not be applicable to the community-dwelling adults with CKD
In summary, hypokalemia and hyperkalemia are often noted in those with CKD. Several clinical and demographic factors are associated with potassium disorders. Both serum potassium levels <4.0 mmol/l and >5.0 mmol/l are associated with all-cause mortality but not with ESRD in those with stage 3 and stage 4 CKD. These associations are modified by the stage of kidney disease and age and further studies are needed to understand the potential mechanisms that explain these findings.
Supplementary Material
Acknowledgments
The authors wish to thank Welf Saupe, Vicky Konig and John Sharp of Cleveland Clinic who helped in data extraction during the development of the registry.
Grant support:
SDN: R01DK101500; JVN: DK094112 and SEJ: 1K23DK091363. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The creation of the CCF CKD registry was funded by an unrestricted grant from Amgen, Inc to the Department of Nephrology and Hypertension Research and Education Fund. Parts of this manuscript were presented as a poster at the annual National Kidney Foundation Meeting held in Dallas, TX in March 2015.
Footnotes
Disclosures
The authors have no relevant financial interest in the study.
References
- 1.Stanton BA. Renal potassium transport: morphological and functional adaptations. Am J Physiol. 1989 Nov;257(5 Pt 2):R989–97. doi: 10.1152/ajpregu.1989.257.5.R989. [DOI] [PubMed] [Google Scholar]
- 2.Gonick HC, Kleeman CR, Rubini ME, Maxwell MH. Functional impairment in chronic renal disease. 3. Studies of potassium excretion. Am J Med Sci. 1971 May;261(5):281–90. doi: 10.1097/00000441-197105000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Palmer BF. Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. N Engl J Med. 2004 Aug 5;351(6):585–92. doi: 10.1056/NEJMra035279. [DOI] [PubMed] [Google Scholar]
- 4.Genovesi S, Valsecchi MG, Rossi E, Pogliani D, Acquistapace I, De Cristofaro V, et al. Sudden death and associated factors in a historical cohort of chronic haemodialysis patients. Nephrol Dial Transplant. 2009 Aug;24(8):2529–36. doi: 10.1093/ndt/gfp104. [DOI] [PubMed] [Google Scholar]
- 5.Unruh ML, Evans IV, Fink NE, Powe NR, Meyer KB Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) Study. Skipped treatments, markers of nutritional nonadherence, and survival among incident hemodialysis patients. Am J Kidney Dis. 2005 Dec;46(6):1107–16. doi: 10.1053/j.ajkd.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Lowrie EG, Lew NL. Death risk in hemodialysis patients: the predictive value of commonly measured variables and an evaluation of death rate differences between facilities. Am J Kidney Dis. 1990 May;15(5):458–82. doi: 10.1016/s0272-6386(12)70364-5. [DOI] [PubMed] [Google Scholar]
- 7.Hayes J, Kalantar-Zadeh K, Lu JL, Turban S, Anderson JE, Kovesdy CP. Association of hypo- and hyperkalemia with disease progression and mortality in males with chronic kidney disease: the role of race. Nephron Clin Pract. 2012;120(1):c8–16. doi: 10.1159/000329511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korgaonkar S, Tilea A, Gillespie BW, Kiser M, Eisele G, Finkelstein F, et al. Serum potassium and outcomes in CKD: insights from the RRI-CKD cohort study. Clin J Am Soc Nephrol. 2010 May;5(5):762–9. doi: 10.2215/CJN.05850809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sinha AD, Agarwal R. Chronic renal disease progression: treatment strategies and potassium intake. Semin Nephrol. 2013 May;33(3):290–9. doi: 10.1016/j.semnephrol.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 10.Weir MR, Fink JC. Salt intake and progression of chronic kidney disease: an overlooked modifiable exposure? A commentary. Am J Kidney Dis. 2005 Jan;45(1):176–88. doi: 10.1053/j.ajkd.2004.08.041. [DOI] [PubMed] [Google Scholar]
- 11.Wang W, Soltero L, Zhang P, Huang XR, Lan HY, Adrogue HJ. Renal inflammation is modulated by potassium in chronic kidney disease: possible role of Smad7. Am J Physiol Renal Physiol. 2007 Oct;293(4):F1123–30. doi: 10.1152/ajprenal.00104.2007. [DOI] [PubMed] [Google Scholar]
- 12.Reungjui S, Roncal CA, Sato W, Glushakova OY, Croker BP, Suga S, et al. Hypokalemic nephropathy is associated with impaired angiogenesis. J Am Soc Nephrol. 2008 Jan;19(1):125–34. doi: 10.1681/ASN.2007030261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Navaneethan SD, Jolly SE, Schold JD, Arrigain S, Saupe W, Sharp J, et al. Development and validation of an electronic health record-based chronic kidney disease registry. Clin J Am Soc Nephrol. 2011 Jan;6(1):40–9. doi: 10.2215/CJN.04230510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009 May 5;150(9):604–12. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moranne O, Froissart M, Rossert J, Gauci C, Boffa JJ, Haymann JP, et al. Timing of onset of CKD-related metabolic complications. J Am Soc Nephrol. 2009 Jan;20(1):164–71. doi: 10.1681/ASN.2008020159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perez GO, Pelleya R, Oster JR, Kem DC, Vaamonde CA. Blunted kaliuresis after an acute potassium load in patients with chronic renal failure. Kidney Int. 1983 Nov;24(5):656–62. doi: 10.1038/ki.1983.208. [DOI] [PubMed] [Google Scholar]
- 17.Kraft MD, Btaiche IF, Sacks GS, Kudsk KA. Treatment of electrolyte disorders in adult patients in the intensive care unit. Am J Health Syst Pharm. 2005 Aug 15;62(16):1663–82. doi: 10.2146/ajhp040300. [DOI] [PubMed] [Google Scholar]
- 18.Williams ME. Endocrine crises. Hyperkalemia. Crit Care Clin. 1991 Jan;7(1):155–74. [PubMed] [Google Scholar]
- 19.Seliger SL, Zhan M, Hsu VD, Walker LD, Fink JC. Chronic kidney disease adversely influences patient safety. J Am Soc Nephrol. 2008 Dec;19(12):2414–9. doi: 10.1681/ASN.2008010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reardon LC, Macpherson DS. Hyperkalemia in outpatients using angiotensin-converting enzyme inhibitors. How much should we worry? Arch Intern Med. 1998 Jan 12;158(1):26–32. doi: 10.1001/archinte.158.1.26. [DOI] [PubMed] [Google Scholar]
- 21.Tannen RL. Diuretic-induced hypokalemia. Kidney Int. 1985 Dec;28(6):988–1000. doi: 10.1038/ki.1985.229. [DOI] [PubMed] [Google Scholar]
- 22.Berenson GS, Voors AW, Dalferes ER, Jr, Webber LS, Shuler SE. Creatinine clearance, electrolytes, and plasma renin activity related to the blood pressure of white and black children--the Bogalusa Heart Study. J Lab Clin Med. 1979 Apr;93(4):535–48. [PubMed] [Google Scholar]
- 23.Lasker N, Hopp L, Grossman S, Bamforth R, Aviv A. Race and sex differences in erythrocyte Na+, K+, and Na+-K+-adenosine triphosphatase. J Clin Invest. 1985 Jun;75(6):1813–20. doi: 10.1172/JCI111894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gallen IW, Rosa RM, Esparaz DY, Young JB, Robertson GL, Batlle D, et al. On the mechanism of the effects of potassium restriction on blood pressure and renal sodium retention. Am J Kidney Dis. 1998 Jan;31(1):19–27. doi: 10.1053/ajkd.1998.v31.pm9428447. [DOI] [PubMed] [Google Scholar]
- 25.Voors AW, Dalferes ER, Jr, Frank GC, Aristimuno GG, Berenson GS. Relation between ingested potassium and sodium balance in young Blacks and whites. Am J Clin Nutr. 1983 Apr;37(4):583–94. doi: 10.1093/ajcn/37.4.583. [DOI] [PubMed] [Google Scholar]
- 26.Ahmed A, Zannad F, Love TE, Tallaj J, Gheorghiade M, Ekundayo OJ, et al. A propensity-matched study of the association of low serum potassium levels and mortality in chronic heart failure. Eur Heart J. 2007 Jun;28(11):1334–43. doi: 10.1093/eurheartj/ehm091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hunt SA American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) J Am Coll Cardiol. 2005 Sep 20;46(6):e1–82. doi: 10.1016/j.jacc.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 28.Bowling CB, Pitt B, Ahmed MI, Aban IB, Sanders PW, Mujib M, et al. Hypokalemia and outcomes in patients with chronic heart failure and chronic kidney disease: findings from propensity-matched studies. Circ Heart Fail. 2010 Mar;3(2):253–60. doi: 10.1161/CIRCHEARTFAILURE.109.899526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schulman M, Narins RG. Hypokalemia and cardiovascular disease. Am J Cardiol. 1990 Mar 6;65(10):4E, 9E. doi: 10.1016/0002-9149(90)90244-u. discussion 22E–23E. [DOI] [PubMed] [Google Scholar]
- 30.Erlinger TP, Tarver-Carr ME, Powe NR, Appel LJ, Coresh J, Eberhardt MS, et al. Leukocytosis, hypoalbuminemia, and the risk for chronic kidney disease in US adults. Am J Kidney Dis. 2003 Aug;42(2):256–63. doi: 10.1016/s0272-6386(03)00650-4. [DOI] [PubMed] [Google Scholar]
- 31.Einhorn LM, Zhan M, Hsu VD, Walker LD, Moen MF, Seliger SL, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009 Jun 22;169(12):1156–62. doi: 10.1001/archinternmed.2009.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Surawicz B, Chlebus H, Mazzoleni A. Hemodynamic and electrocardiographic effects of hyperpotassemia. Differences in response to slow and rapid increases in concentration of plasma K. Am Heart J. 1967 May;73(5):647–64. doi: 10.1016/0002-8703(67)90174-3. [DOI] [PubMed] [Google Scholar]
- 33.Elger M, Bankir L, Kriz W. Morphometric analysis of kidney hypertrophy in rats after chronic potassium depletion. Am J Physiol. 1992 Apr;262(4 Pt 2):F656–67. doi: 10.1152/ajprenal.1992.262.4.F656. [DOI] [PubMed] [Google Scholar]
- 34.Ray PE, Suga S, Liu XH, Huang X, Johnson RJ. Chronic potassium depletion induces renal injury, salt sensitivity, and hypertension in young rats. Kidney Int. 2001 May;59(5):1850–8. doi: 10.1046/j.1523-1755.2001.0590051850.x. [DOI] [PubMed] [Google Scholar]
- 35.Drawz PE, Goswami P, Azem R, Babineau DC, Rahman M. A simple tool to predict end-stage renal disease within 1 year in elderly adults with advanced chronic kidney disease. J Am Geriatr Soc. 2013 May;61(5):762–8. doi: 10.1111/jgs.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hayes J, Kalantar-Zadeh K, Lu JL, Turban S, Anderson JE, Kovesdy CP. Association of hypo- and hyperkalemia with disease progression and mortality in males with chronic kidney disease: the role of race. Nephron Clin Pract. 2012;120(1):c8–16. doi: 10.1159/000329511. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.