Abstract
AIM: To review current applications of the laparoscopic surgery while highlighting the standard procedures across different fields.
METHODS: A comprehensive search was undertaken using the PubMed Advanced Search Builder. A total of 321 articles were found in this search. The following criteria had to be met for the publication to be selected: Review article, randomized controlled trials, or meta-analyses discussing the subject of laparoscopic surgery. In addition, publications were hand-searched in the Cochrane database and the high-impact journals. A total of 82 of the findings were included according to matching the inclusion criteria. Overall, 403 full-text articles were reviewed. Of these, 218 were excluded due to not matching the inclusion criteria.
RESULTS: A total of 185 relevant articles were identified matching the search criteria for an overview of the current literature on the laparoscopic surgery. Articles covered the period from the first laparoscopic application through its tremendous advancement over the last several years. Overall, the biggest advantage of the procedure has been minimizing trauma to the abdominal wall compared with open surgery. In the case of cholecystectomy, fundoplication, and adrenalectomy, the procedure has become the gold standard without being proven as a superior technique over the open surgery in randomized controlled trials. Faster recovery, reduced hospital stay, and a quicker return to normal activities are the most evident advantages of the laparoscopic surgery. Positive outcomes, efficiency, a lower rate of wound infections, and reduction in the perioperative morbidity of minimally invasive procedures have been shown in most indications.
CONCLUSION: Improvements in surgical training and developments in instruments, imaging, and surgical techniques have greatly increased safety and feasibility of the laparoscopic surgical procedures.
Keywords: Laparoscopic surgery, Endoscopic surgery, Pancreatic surgery, Rectal resection, Gastrectomy, Gastric cancer, Colon resection, Appendectomy, Esophagectomy, Cholecystectomy
Core tip: This review investigates different applications of the laparoscopic approach on the basis of the current literature and summarizes studies concerning laparoscopic surgery in the different medical fields.
INTRODUCTION
Laparoscopic surgery has existed since the development of diagnostic laparoscopy in the 1960s. The pioneers of laparoscopic surgery Semm K[1] and Muehe E[1] changed it from a diagnostic to a surgical procedure at the beginning of the 1980s, and it has since become a frequently applied technique for a wide field of indications. The procedure has become the gold standard for many organ systems, with some of the most common being reproductive (particularly gynecological) and digestive (as for cholecystectomy). Significant improvements in surgical training, as well as developments of instruments, imaging, and surgical techniques, have made laparoscopic surgery safe and feasible across different medical fields.
This review summarizes studies on the laparoscopic surgery across different fields and highlights the state of the art, standard procedures in laparoscopic surgery.
MATERIALS AND METHODS
A comprehensive search was undertaken using the PubMed Advanced Search Builder. The exact search strings are listed in Tables 1 and 2. In addition, publications were hand-searched in the Cochrane database and in the high-impact journals such as Ann Surg, Lancet, BMJ, Brit J Surg, World J Gastroenterol, Surg Endosc, World J Surg, Am J Gastroenterol, Hernia, Am J Surg, Langenbecks Arch Surg, Arch Surg, Chirurg, J Am Coll Surg, and Colorectal Dis. Publications had to meet the following criteria to be selected: review articles, randomized controlled trials, or meta-analyses discussing the subject of laparoscopic surgery (Figure 1). A total of 403 articles were identified and downloaded for full-text review. Of these, 218 articles were excluded for not matching the inclusion criteria and 185 articles were determined to match the search criteria and included in the analysis.
Table 1.
Search strategy using publication within the past 5 years
| And | And | And | And | Results | Selected | |
| Laparoscopic surgery | Pancreatic surgery | Whipple | Meta-analysis | Analysis | 1 | 1 |
| Laparoscopic surgery | Rectal resection | Meta-analysis | 37 | 13 | ||
| Laparoscopic surgery | Gastrectomy | Gastric cancer | Meta-analysis | 65 | 20 | |
| Laparoscopic surgery | Liver resection | Liver surgery | Meta-analysis | 30 | 11 | |
| Laparoscopic surgery | Colon resection | Meta-analysis | 16 | 6 | ||
| Laparoscopic appendectomy | Open appendectomy | Meta-analysis | 26 | 13 | ||
| Laparoscopic surgery | Esophagectomy | Meta-analysis | 9 | 3 |
Table 2.
Search strategy using unrestricted publication dates
| And | And | And | Results | Selected | |
| Laparoscopic surgery | Open cholecystectomy | Meta-analysis | 61 | 15 | |
| Laparoscopic surgery | Endoscopic surgery | Groin hernia | Meta-analysis | 15 | 6 |
| Laparoscopic surgery | Endoscopic surgery | Incisional hernia | Meta-analysis | 19 | 6 |
| Laparoscopic surgery | Fundoplication | Meta-analysis | 42 | 9 |
Figure 1.
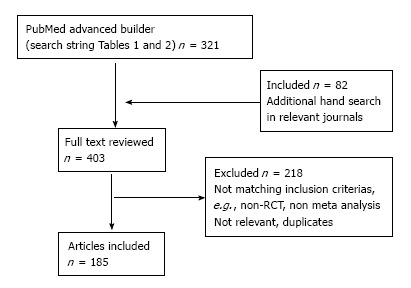
Selection of articles for the review.
The systematic review was conducted in compliance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines[2]. The study was registered on the PROSPERO international prospective register of systematic reviews (Registration Number: CRD42015019334).
RESULTS
Appendectomy
The systematic reviews and meta-analysis that compared the clinical outcome of laparoscopic vs open appendectomy clearly showed an advantage of the laparoscopic procedure[3]. Laparoscopic appendectomy has been proven to be a safe and feasible procedure in the treatment of acute appendicitis and even complicated appendicitis[4,5]. Supporters of the laparoscopic appendectomy maintain that in addition to an improved diagnostic accuracy, the procedure lowers the number of wound infections, results in less pain, faster recovery, and an earlier return to work[6]. However, there seems to be an increase in the operating time for the laparoscopic vs open surgery[7]. Earlier reviews reported an increase in incidences of intra-abdominal abscess in the laparoscopic group[8]; later reviews, however, did not find any significant difference between the laparoscopic and open surgery groups[6]. The authors explained the discrepancy in the data as a result of an adapted learning curve, better instruments and imaging quality, and of course more experienced surgeons[6].
Regarding the complication rates of laparoscopic vs open appendectomy, there were no significant differences in the overall postoperative complications, pulmonary complications, or postoperative ileus[3]. Considering the postoperative ileus situation after a laparoscopic appendectomy, a significant reduction in the short-term bowel obstruction in pediatric patients and patients with perforated appendicitis were described.
Regarding the long-term bowel obstruction or bowel obstruction requiring surgery, there was a significantly better outcome in the laparoscopic appendectomy group[9]. Patients who underwent the laparoscopic procedure for their appendectomy had shorter hospital stays and were able to “return to normal activity” and “return to work” faster than those who underwent open surgery[3]. The initial higher charges and operating costs in the laparoscopic group were compensated through reduced costs required outside the hospital stay[10].
In the obese patients, the outcome parameters, wound infection rate and overall postoperative complication rate were significantly decreased compared to the open appendectomy group. The operation time did increase, most likely due to technical challenges associated with patients who have a body mass index > 30 kg/m2. Despite this, the advantages of the laparoscopic approach outweigh the disadvantages for the treatment of appendectomy in obese patients[11].
In pregnant patients, there is a higher risk of fetal loss (although with little evidence) and a slightly increased rate of preterm labor, which was not significant and was without clinical importance[12].
Newer techniques of reduced ports surgery and single-incision surgery as a less invasive alternative are also performed as a procedure for laparoscopic appendectomy.
The reviews comparing single-incision vs conventional laparoscopic appendectomy show a significantly longer operation time with an outcome similar to a conventional laparoscopic procedure with no difference in wound infection rate, conversion to open surgery, reoperation, intra-abdominal collection of fluid, or overall complications[13,14]. Single-incision appendectomy is considered a safe and feasible procedure with comparable clinical outcomes when undertaken by experienced surgeons[15,16]. Results related to better cosmetics and an earlier return to work should be considered with caution due to the small number of studies reporting these two items, along with the short follow-ups used for evaluation of cosmetic results[17]. Critics of the approach have stated that there is no benefit in a single-incision access for appendectomy since clinical outcomes were related to increased operation time, higher frequency of technical failure, and potentially higher costs[18].
Cholecystectomy
Patients who underwent cholecystectomy via laparoscopic procedure had no significant difference in morbidity and mortality compared to those who underwent open surgery. In fact, they had faster recovery and shorter hospital stay[19]. Although mini-laparotomy had a similar overall outcome, the authors regard the minimalized open technique as a viable and safe option for healthcare providers without financial resources for laparoscopic equipment and without appropriate, trained surgeons[20]. Later studies showed no difference between laparoscopic and minimally open and conventional open surgery in terms of morbidity and mortality[21].
Laparoscopic cholecystectomy is proven as a safe and feasible technique; concerning cardiac and respiratory complications, it shows superiority over open surgery in elderly patients[22].
Patients with child A or B stadium of liver cirrhosis who underwent laparoscopic cholecystectomy had a similar or even better outcome than those who underwent open surgery. As a result, these patients experienced a lower incidence of postoperative complications[23], such as blood loss and bacterial contamination of ascites - an important cause of in-hospital morbidity and mortality[23]. The postoperative incidence of hepatic insufficiency was not different. These findings have to be regarded with caution, however, because some of the studies had small patient groups with heterogeneous patient populations and criteria[24].
The routine on-table use of intraoperative cholangiography shows no advantage in preventing injuries of the common bile duct or retained stones[25]. There is a significantly longer surgery time with the recommendation not to use routine on-table cholangiography when there are no clinical, radiological or biochemical signs of common bile duct stones[26]. In the management of suspected common bile duct stones, there is a slight advantage concerning complications after sphincterotomy in patients, where the endoscopic sphincterotomy is performed intraoperatively rather than preoperatively[27].
With laparoscopic cholecystectomy, the goal is to minimize trauma to the abdominal wall as much as possible by using the upcoming techniques of reduced port[28-30] or single-port surgery[31] or hybrid NOTES techniques. These techniques have yet to prove their feasibility, safety, and possible superiority over the established 4-port technique of laparoscopic cholecystectomy. In the case of single-incision techniques, the findings varied depending on the number of cases included in the studies. Some of the earlier studies that had been performed when single-incision surgery was newly introduced often lacked evidence and were thus biased.
Some of the studies showed better postoperative pain scores after single-incision procedure vs laparoscopic procedure[32,33], while others showed no difference[34,35]. Because there was no significant difference in mortality, morbidity, short-term surgical outcome, length of hospital stay, or return to normal activity, many authors consider single-incision cholecystectomy safe and feasible, with a better outcome for patients’ cosmetic satisfaction. Others do not recommend single-incision techniques because there is no apparent advantage over conventional laparoscopic cholecystectomy, which has longer operation times and requires additional ports[36]. Hybrid NOTES did not differ in overall complications, surgery-related complications, or postoperative pain, but did have a significantly better outcome in “return to normal
activity”[37].
Laparoscopic cholecystectomy is accepted as the gold standard, although studies have shown that mini-laparotomy is similar in outcome, with decreased surgery time and lower cost[19,21]. Single-incision techniques and hybrid NOTES must prove their advantage or similarity in the same way that laparoscopic cholecystectomy has had to do.
Esophageal surgery
Minimally invasive surgery for esophageal cancer is a technically challenging procedure, and the great variability in surgical techniques makes it difficult to interpret the findings and outcomes reported in the current literature. Many studies have a small number of patients, and no randomized controlled trials are available to verify the data[38].
Patients with esophageal cancer who underwent laparoscopy experienced longer surgery time, less blood loss, shorter hospital stay, and reduced overall morbidity[39,40].
One of the difficulties in comparing results across different studies was a lack of definitions regarding postoperative complications or operative techniques. Many studies did not perform or describe a radical lymphadenectomy, and lymph node harvest was lower than the recommended minimum number[41]. Other studies have found a similar lymph node harvest[42] or even more lymph nodes in laparoscopic treatment compared with open surgery[43]. The reported minor complications associated with laparoscopy were similar to open surgery, but the major complications were significantly lower in the laparoscopic group. The lower number of harvested lymph nodes showed a similar percentage of positive lymph nodes, and the lymph node harvest did not impact the survival rate[44], even in the case of the long-term results[45]. A reported adjustment in the surgical techniques (the “Ivor Lewis approach”) led to better short-term and long-term outcomes for patients undergoing minimally invasive surgery with an acceptable lymph node harvest and a similar oncological outcome to open surgery[46,47].
Burdall et al[48] found significant independent parameters that had an impact on outcome in overall survival. These included the use of neoadjuvant chemotherapy, tumor size (T3 or T4), positivity of lymph nodes, R1-resection, and the surgical approach. Overall, patients who underwent laparoscopic treatment had a significantly better overall survival.
Reflux surgery
The laparoscopic approach has become the gold standard for surgical management of gastroesophageal reflux disease (GERD). Laparoscopic surgery in the treatment of GERD led to reduced hospital stay, faster recovery, faster return to normal activity, and a significant reduction of perioperative morbidity compared with open surgery[49,50]. Laparoscopy has been shown to more effectively treat symptoms, such as reduction of heartburn and regurgitation, and patients reported higher quality of life than achieved with other medical treatments such as proton-pump inhibitor drug alone[51].
The different surgical techniques in the surgical management of GERD are still under discussion. The functional outcome appears similar whether the short gastric vessels are divided or not; therefore, this step in the reflux surgery procedure seems unnecessary and may reduce the operation time if avoided[52-54]. Posterior surgical techniques - the Nissen 360° and Toupet 270° procedures - gave patients a satisfactory control of reflux symptoms. Dysphagia symptoms were more prevalent after the Nissen procedure, while Toupet operations had a higher rate of gas-related symptoms, such as inability to belch and bloating[55]. The Toupet’s procedure seems to have superior level 1a evidence than the Nissen procedure. However, these findings should be taken with caution since the study had a Jadad score of 2 with a corresponding possibility of bias[55]. Another evidence-based appraisal for these posterior methods in reflux surgery showed adequate symptom relief after both procedures with a slightly reduced rate of adverse results in the Toupet group[56].
The anterior approach in the treatment of GERD often leads to a longer esophagus acid exposure time, persistent heartburn symptoms and a higher rate of reoperation in the short-term outcomes compared with the posterior approach. However, these symptoms are counterbalanced by the less severe dysphagia symptoms. For the long-term outcomes, persistence of heartburn and higher use of antacids prevail, with dysphagia scores and gas-related symptoms being similar to those in the posterior group. Hence, there is level 1a support for the usage of posterior techniques in reflux surgery[57].
Robotic surgery used in surgical treatment of GERD is a feasible alternative to laparoscopic surgery. The approach has similar results in terms of symptom relief and surgical outcome. However, lack of obvious advantages with respect to operating time and length of hospital stay and cost do not support the expansion of robotic surgery to other applications in clinics[58].
Gastric surgery
Laparoscopic gastric surgery is a demanding procedure. Results of the surgery depend on the stage of the gastric tumor (early vs advanced), whether a partial or total gastrectomy was performed, and presence of gastrointestinal stromal tumors (GIST)[59]. Laparoscopic resections have an overall better short-term outcome with less blood loss, shorter hospital stay, faster recovery of bowel movement with shorter time to first flatus, and fewer serious perioperative complications. However, there was an overall longer time for surgery[60]. Wound complications and surgical site infections were less significant in the laparoscopic group. For severe postoperative complications, such as anastomotic leakage, stenosis, bleeding and postoperative ileus, there was no difference from open surgery[61].
Clearance of harvested lymph nodes is an important factor influencing long-term survival in gastric cancer. Laparoscopic distal gastric resection for early gastric cancer shows fewer or a similar amount of harvested lymph nodes compared with open surgery[60,62,63]. Viñuela et al[64] had significantly more lymph nodes harvested in the open surgery group, and the proportion of patients with < 15 lymph nodes was similar to that in the laparoscopic group. The authors were of the opinion that adequate pathological lymph node staging was not compromised by the laparoscopic technique.
Further improvements in the laparoscopic technique show no difference between D2-lymphadenectomy performed for advanced gastric cancer compared to open surgery[65,66]. The surgical approach is not the only parameter that determines the types of or frequency of complications, as well as an acceptable long-term outcome. Other factors such as patient’s age, comorbidities (e.g., chronic liver disease, chronic renal failure) and additional organ resection have a significant effect on complications and outcome[67].
In advanced gastric cancer, the total laparoscopic gastrectomy consistently showed the advantages of laparoscopic surgery, having a better short-term outcome than open surgery. Incidence of the short-term complications appears to be correlated with intraoperative blood loss; hence, many studies directed their attention to this parameter. The results in all studies were consistently in favor of the laparoscopic surgery[68].
Concerning the long-term follow-up, the results of laparoscopic surgery were suggested to be similar to open procedures[69]. Current clinical evidence showed that laparoscopic gastric surgery is not inferior to open techniques, even in the treatment of advanced gastric cancer, if the surgeon is experienced[70]. The laparoscopic gastric resection had acceptable results concerning oncological safety[71]. These findings were confirmed in gastric stromal tumors. Laparoscopic surgery was superior to open techniques regarding short-term postoperative outcome without compromising oncological safety and long-term oncological outcome[72]. Furthermore, these long-term results depended mainly on the tumor itself rather than the performed surgical technique[73].
The results of robotic gastric surgery are comparable to laparoscopic surgery. The robotic gastric surgery could be favorably effective considering the increased number of harvested lymph nodes and D2-lymphadenectomy in patients with high body mass index[74]. Data on the long-term outcome and survival are rare, so randomized clinical trials are required[75].
Colorectal surgery
Laparoscopic colorectal surgery is well established as a safe procedure and must be differentiated between the surgical treatment of the benign and malignant disease. The review of current literature shows an ongoing learning curve and an improvement in the management of postoperative care, such as developing fast-track concepts and pathways in “enhanced recovery after surgery” (ERAS). This combination of the surgical procedures (minimally invasive access) reducing major morbidities and standardized postoperative treatment concepts led to a satisfying outcome for patients undergoing colorectal surgery[76]. Colorectal cancer patients who underwent laparoscopic surgery within a multimodal rehabilitation protocol experienced the shortest hospital stay and the lowest morbidity[77].
The general benefits for patients undergoing laparoscopic surgery are the minimal trauma of access, reduced pain, accelerated postoperative return of bowel function, faster return to activity, and better cosmesis. Evidence for potential benefits such as reduced adhesions and a lower rate of incisional hernias was difficult to find[78].
For the ulcerative colitis surgery, the results showed a reduced morbidity in colectomy with a lower mortality in the laparoscopic group compared to open surgery[79].
Surgical treatment of Crohn’s disease showed a trend towards lower rate of wound infections, with a lower rate of reoperation in non-disease related complications in the laparoscopic group[80]. In regard to the perioperative morbidity and convalescence, there is evidence that laparoscopic surgery is favored over open surgery for the treatment of Crohn’s disease. The data on the lower incidence of small bowel obstruction and Crohn’s recurrence following a minimally invasive surgery was of poor quality[81].
A laparoscopic surgical approach to diverticular disease was associated with longer operation time and reduced postoperative pain. In the elective cases, the reported quality of life score and reduced major morbidity rates were superior to open surgery[82-84]. The decreased incidence of wound infection, the lower need for blood transfusion, and the lower ileus rates led to acceptance of laparoscopic surgery in treatment of elective cases of recurrent diverticulitis[85]. Although laparoscopy minimized the short-term complication rate, a meta-analysis of randomized clinical trials found 42% morbidity in the elective cases, a worrisome finding[86].
The use of hand-assisted devices led to a decrease of conversion rates without difference in the duration of surgery or complication rates. However, all these studies had methodical limitations, along with the additional cost associated with these devices[87]. These findings were less certain in the case of emergency surgery. In generalized peritonitis due to perforated diverticulitis, the approach to drain without resection reduced the incidence of Hartmann’s procedure without increasing morbidity and mortality. This finding may lead to a shift in the management of acute perforated diverticulitis in the future[88].
Natural orifice specimen extraction after colon or sigmoid resection is feasible and seems to have an advantage in minimizing trauma to the abdominal wall by avoiding a small incision for specimen extraction. Current literature, however, shows that this technique is not standardized, and no pooled analysis or meta-analysis is practicable, so evidence in the literature is weak[89].
Colon cancer
For colon cancer, the laparoscopic approach is regarded safe and feasible without compromising the oncological outcome. The short-term outcome benefits were lower blood loss, earlier recovery of bowel movement, earlier resumption of oral intake, and reduced hospital stay, as well as lower overall morbidity. The lymph node harvest and results of oncological outcome were similar to open surgery. Thus, laparoscopic surgery was considered superior to open surgery in the short-term outcome of colon cancer[90].
Expert opinion in the literature shows a growing acceptance of laparoscopic surgery for treatment of colorectal cancer, which is further supported by the large randomized clinical trials[91]. Evaluation of the long-term outcomes for non-metastatic colon cancer shows no difference in the occurrence of port site metastasis/wound recurrence, cancer-related mortality, tumor recurrence, or overall mortality[92]. Considering the anatomical circumstances and the oncological outcome, complete mesocolic excision is also recommended in the minimally invasive surgery[93].
For the right hemicolectomy, in regard to the benign and malignant disease, the intraoperative and postoperative results were favorable for the laparoscopic group. There was no difference between the laparoscopic treatment and open surgery in regard to the short-term oncological outcome, including lymph node harvest and length of specimen, and the long-term oncological outcome[94].
In transverse colon tumors, the evidence is not as clear as in other types of colorectal cancer. The benefits of the laparoscopic approach have been demonstrated; however, the data need to be interpreted with caution due to the heterogeneity in the included studies[95].
For long-term survival following laparoscopic colectomy, there was no difference in the overall survival between the laparoscopic group and open surgery. Large randomized controlled trials (excluding transverse colon cancer) demonstrated that laparoscopic surgery was not inferior to open surgery in the long-term oncological outcomes[96]. There was no significant difference in overall mortality, total recurrence rate, or 5-year disease-free and overall survival[97].
Conversion to open surgery seems to have a worse oncological long-term outcome than completion with laparoscopic surgery or starting with an open procedure from the outset. Factors for conversion include higher body mass index, male sex, T3-T4 tumor size, or positive lymph nodal disease[98].
Robotic surgery has short-term outcomes similar to laparoscopic surgery. For blood loss, conversion rate, and time to recover bowel function, there were significant findings in favor of robotic surgery compared with laparoscopy[99].
Rectal surgery
The current data is insufficient to favor a certain technique over another for treatment of rectal prolapse. Laparoscopic rectopexy had fewer postoperative complications and a shorter hospital stay compared with open surgery. The different rectopexy fixation methods did not differ in their outcomes[100]. Compared with a perineal approach (Delorme procedure), the laparoscopic group had higher overall morbidity[101].
Rectal cancer
Rectal cancer laparoscopic surgery has the benefit of minimally invasive access. In the laparoscopic group, blood loss, time to first bowel movement, intake of oral fluids and wound infection were significantly lower after the laparoscopic approach. There were no differences between the laparoscopic approach and the open surgery in terms of complications such as ureter injury, urinary retention, ileus, anastomotic leakage, or an incisional hernia. Oncological outcomes in the short-term and long-term results, such as length of specimen, circumferential resection margin, regional recurrence, port/wound metastasis and distant metastasis, also showed no significant difference[102]. Three-year, 5-year and 10-year disease-free and overall survival was similar between the two treatments[103].
For early rectal cancer, preoperative staging determines the surgical approach to the rectum. In tumors with good prognostic features and a limited risk of relapse, which can safely be removed while preserving the rectum, the endoscopic mucosal resection or a transanal microsurgery can be performed. If local excision is pathologically difficult or risky, a complete total mesorectal excision (TME) must be done. The laparoscopic approach showed a better short-term outcome with a similar oncological outcome[104].
Contrary to the findings for colon cancer, the clinical outcome was not worse when a laparoscopic procedure was converted to open surgery in rectal cancer. The conversion had no impact on unplanned hospital readmission or redo surgery, nor on 3-year disease-free survival and local recurrence compared with a laparoscopic procedure[105].
Minimally invasive TME can also be performed safely and efficiently after neoadjuvant radiochemotherapy, with a rate similar to open surgery for postoperative complications and a comparable rate of positive circumference resection margin[106].
Considering postoperative bladder and sexual function in patients undergoing rectal surgery for cancer, there is no difference between the laparoscopic and open surgery group for men in the postoperative ejaculatory and erectile function or bladder function. No difference in the sexual or bladder function between open and laparoscopic surgery was found in women either. Therefore, none of the techniques are superior to the other. Since there is limited data available for these results, they must be viewed with caution[107].
The oncological outcome in laparoscopic surgery was controversial when laparoscopic TME was first introduced. However, the latest results that focus on equivalent oncological outcome prove this topic. The involvement of a circumferential resection margin is equivalent to open TME. Harvest of lymph nodes in the open surgery group was described as slightly higher without having an impact on oncological outcome. In subgroup analysis, there was no difference in R0-resection, distal margin clearance, integrity of the mesorectal fascia, or in local recurrence after 5 years[108,109].
Laparoscopic rectal surgery is a challenging procedure for experienced surgeons. For trainees being supervised by an experienced surgeon, there are similar rates of anastomotic leakage with no difference in the conversion, R0-resection, local recurrence and 30-d mortality compared with experienced surgeons. Furthermore, there were no differences in the cancer-specific survival between the experienced group and the supervised trainees. Therefore, the procedure can be performed by supervised trainees with an adequate learning curve[110].
An upcoming technique is a transanal approach for performing the TME in combination with a laparoscopic approach. In the current literature, the reported TME quality with intact mesorectal fascia is satisfactorily complete, and the number of harvested lymph nodes was ≥ 12, so the oncological safety parameters seem to be adequate[111].
Robotic procedures in the rectal surgery show the known merits of robotic surgery with a favorable perioperative outcome considering the conversion rate. There were no significant differences with laparoscopic surgery in terms of surgery length, blood loss, recovery of bowel movement, hospital stay, short-term complications and details on the pathological performance such as harvested lymph nodes, resection margin, and circumferential resection margin. These results must be viewed with caution, however, because most of the studies had small sample size or a low level of evidence[112-114]. More high-quality studies are necessary to show the benefit of robotic over laparoscopic surgery and to justify its costs[115]. The long-term benefits of robotic surgery in colon and rectal cancers are still unknown[116].
Liver surgery
Laparoscopic resection of the liver is performed mainly when treating metastasis of colorectal carcinoma or primary hepatocellular carcinoma. Other indications such as cyst resection are rare. The minimally invasive approach is widely applied to patients with limited disease, such as those with solitary findings of 3-4 metastases in the liver. Findings in the liver segments II-IV are better suited for a laparoscopic approach than those in segments VII, VIII and IVa, which are difficult to reach. Detailed preoperative imaging and an intraoperative ultrasound are helpful[117].
Laparoscopic liver resection has advantages for short-term outcomes such as lower blood loss with a lower rate of transfusion, shorter postoperative hospital stay, and lower rates of positive resection margin and perioperative complications. Patient selection may have influenced some of the observed outcomes[118].
Left lateral resection is described as safe and feasible, and due to lower complication rates and the known advantages of minimally invasive access, some authors claim that it should be used as a standard technique for left resection. At this time, however, there is a lack of randomized controlled trials to support such a statement[119].
Laparoscopic resection with positive short-term results and improved surgical outcome[120] do not compromise oncological outcome or 5-year disease-free and overall survival compared to patients with similar results from open surgery[121,122].
There were fewer postoperative complications in the laparoscopic group concerning short-term outcomes of hepatocellular carcinoma resection, positive resection margin rate, and tumor recurrence, with no significant difference between laparoscopic and open surgery. In short-term results, no tumor recurrence in the site of resection margin and no peritoneal dissemination or trocar site metastasis were found in the laparoscopic group[123].
The incidence of postoperative ascites and liver failure in the laparoscopic surgery group was lower, benefiting patients with severe liver disease and especially for those with hepatocellular carcinoma[124]. For laparoscopic surgery in the treatment of liver cirrhosis, the advantages for the short-term and long-term outcomes persist[125]. Although laparoscopic liver resection is described as a safe and feasible alternative to open surgery, with favorable outcomes, there is a need for future randomized controlled trials[126] as the current studies do not provide enough support[127].
The laparoscopic approach for radiofrequency ablation is used for hepatocellular carcinoma. Intraoperative laparoscopic ultrasound led to an oncological upstaging in up to 32% in a small case series[128]. In the laparoscopic resection of liver metastases for colorectal carcinoma, these findings do not show any true benefit for the patient, so here, laparoscopy as a diagnostic method appears more as a useful instrument when a peritoneal disease is suspected[129].
Blood loss with a significant reduction of transfusion and the overall complication rate were lower in the laparoscopic group. No difference in the long-term oncological results in 1-, 3- and 5-year survival was found compared with open surgery[130,131]. Some analyses even showed a lower incidence of R1 resection in the laparoscopic group[132].
Resection of liver metastasis can be performed synchronously with colectomy, with a favorable outcome of the short-time results, but there was no difference in the long-term results in regard to the survival or recurrence. The authors consider synchronous resection of liver metastasis to be an option for selected cases, but the included studies lacked standardized inclusion criteria, so the results must be interpreted carefully[133].
In fenestration of congenital hepatic cysts, a favorable short-term outcome of the laparoscopic approach is described without a difference in postoperative complications or cyst recurrence rates, so the minimally invasive surgery is favored in these cases[134].
In living donor liver transplantation, the laparoscopic approach is seen as comparable to the open approach for liver procurement in terms of donor safety. Lower blood loss was shown in the laparoscopic group[135].
Surgery of the adrenal glands
Minimally invasive surgery of the adrenal glands has become the gold standard in resection of benign and malignant disease. Potential laparoscopic techniques are the lateral transperitoneal approach and the posterior retroperitoneal approach. Regarding outcome of these approaches, compared to each other, the posterior retroperitoneal seems to be a comparable[136] or superior[137] approach based on the operation time, blood loss, pain score, hospital stay, and time to return to normal activity[138]. The conversion rate and surgical complication rate are similar[139]. Both techniques have replaced open access to the adrenal gland in tumors ≤ 8 cm. For the retroperitoneal approach, the findings support a faster convalescence compared with the lateral transperitoneal approach. Since the difference is not significant the authors could not make a recommendation for either approach[140].
Minimally invasive adrenalectomy is the mainstay of operative options for adrenal tumors. Despite lack of evidence for the technique in the randomized controlled trials, it has gained acceptance in the surgical world. Adrenalectomy is performed in hormone-active tumors, lesions > 4 cm, and benign disease with untypical imaging[141].
Studies have shown that the laparoscopic approach can be an acceptable option for the primary neoplasm or adrenal metastasis with no evidence of local invasion[142]. If there is any doubt before the operation that the tumor cannot be removed with an intact capsule, open surgery must be considered[143].
Surgical therapy of primary aldosteronism (Conn’s
disease), compared with medical treatment, leads to a significantly better decrease in blood pressure, with no difference in the cardiovascular complications in qualitative analyses with heterogeneous protocols. Despite the absence of randomized controlled trials, there is support for unilateral resection of unilateral disease[144].
For subclinical Cushing’s disease, unilateral laparoscopic adrenalectomy can resolve the hypercortisolism with low morbidity and can provide significant benefit to blood pressure, glucometabolic control and obesity vs a conservative medical treatment. However, these findings lack evidence are from studies that include data that is too low quality for a systematic review, so the authors could not give a definitive recommendation[145].
In the treatment of refractory Cushing’s disease, bilateral adrenalectomy plays a crucial role in cases where transsphenoidal surgery of ACTH-producing tumors does not lead to normalization of hypercortisolism. In these cases, laparoscopic bilateral resection is safe and effective[146].
The single-incision technique showed similar benefits to the conventional laparoscopic approach. The studies found no difference in blood loss, length of hospital stay, or time to oral intake, with similar outcomes in cosmetic satisfaction, rate of complication, rate of conversion to open surgery, and need for transfusion[147]; longer duration of surgery, lower pain perception, and slightly faster recovery were also reported[148].
Robotic surgery is used in the retroperitoneal posterior and transabdominal lateral approach. A significantly lower blood loss was found in the robotic group compared with the group who underwent laparoscopic surgery, with no difference in the short-term surgical outcomes or complications[149]. With longer surgery and selection of patients, the widespread robotic techniques will be difficult[150] even with lower conversion rate for large tumors compared with laparoscopic surgery[151]. Training and costs associated with the technique are the major drawbacks of robotic surgery in the treatment of adrenal glands[152].
Pancreatic surgery
Laparoscopic surgery of the pancreas is a challenging procedure for experienced surgeons. Most of the studies had a small sample size, and patients were highly selected. Laparoscopic left-side resection of pathologies of the distal pancreas or laparoscopic enucleation for benign lesions has been reported as safe and feasible, with morbidity comparable to open surgery[153]. Left-side resection is the most common laparoscopic procedure in pancreas surgery because it is technically easier to perform. The duration of surgery, surgical morbidity, rate of R1-resection and rate of major complications like pancreatic fistula are similar to the open surgery group; hospital stay and blood loss were reduced[154]. Long-term outcomes of the left resection are equivalent[155] even for malignant findings[156].
For laparoscopic necrosectomy, therapeutic drainage is the best option for conservative management. The literature findings were difficult to compare because of differences in the techniques used, as well as in timings of the interventions[154].
Laparoscopic pancreaticoduodenectomy is performed as a laparoscopic-assisted or total laparoscopic procedure[157]. The outcomes were comparable to open surgery in overall morbidity and surgical-related complications; oncological criteria were fulfilled in terms of number of harvested lymph nodes and resection margin. Due to a lack of randomized controlled trials and the small sample sizes of highly selected patients[158], there was a selection bias so the results should be viewed with caution[154].
Robotic surgery was reported only in the case reports or cohort series, making it difficult to compare. Trials were heterogeneous so data could not be analyzed. In the selected patients, results were comparable to laparoscopic surgery[159] with a trend to improve spleen preservation[160].
Surgery of the spleen
Laparoscopic surgery has become standard for splenectomy in elective cases. The laparoscopic approach showed a reduced morbidity, especially in the pulmonary complications after surgery and wound infection compared with open surgery[161].
In large spleens, a hand-assisted device showed an advantage to open surgery in terms of reduced pain and reduced length of hospital stay, with a surgical outcome similar to laparoscopic surgery. Furthermore, compared with laparoscopic splenectomy, the hand-assisted surgery of the spleen had a lower conversion rate to open surgery[162].
Information on the alternative methods of access like NOTES or single-incision laparoscopic splenectomy is rare. These methods are feasible, however, there is a high risk of bias in the early case reports regarding the alternative approaches in highly selected patients[163]. Only single cases on robotic surgery for splenectomy have been reported[164].
Laparoscopic hernia surgery
Groin hernia: Operative and perioperative management of hernia repair represent a wide field of surgical research. Of the tissue repair techniques, the Shouldice procedure is the only technique with recurrence rates that are lower than other open non-mesh techniques. Mesh repair is evidently superior to tissue reconstruction[165]. The Lichtenstein’s procedure is the gold standard in open hernia mesh repair, and has minimal recurrence and morbidity.
There are two minimally invasive surgeries available for a groin hernia: A transabdominal preperitoneal repair (TAPP) and a totally extraperitoneal hernia repair (TEP). While the mesh is placed in the same position, the approach through the abdominal cavity (TAPP) or in front of the peritoneum (TEP) is different. Both techniques are described as effective treatments of a groin hernia but with a slight increase in perioperative morbidity in comparison to open mesh techniques[165].
Comparing the two techniques, TEP is associated with a slightly faster postoperative recovery; the TAPP technique has a significantly higher incidence of operative morbidity. For incidence of recurrence, long-term neuralgia, duration of surgery, and length of hospital stay, both laparoscopic approaches seem to be similar[166].
Comparison of the minimally invasive approach with the open mesh repair (Lichtenstein) in unilateral hernias, the TAPP technique had a similar recurrence rate and was associated with greater perioperative morbidity. The TEP technique had a slightly increased recurrence rate and a comparable incidence of perioperative complications. The minimally invasive techniques had a significantly reduced risk of chronic groin pain and groin stiffness[167]. In recurrent hernia repair, neither of the laparoscopic procedures were considered superior to open surgery in terms of recurrence and chronic pain[168].
Use of lightweight mesh in hernia repair reduced the risk of chronic groin pain[169] with no effect on recurrence[170] and showed a reduced risk of stiffness and groin body sensation[169,171].
The type of mesh fixation method in laparoscopic hernia repair led to different outcomes. Fibrin glue showed a reduced risk of chronic groin pain and a higher patient satisfaction[172] without impact on recurrence rate[173]. Use of staplers/tacks had a higher incidence of postoperative and groin pain[174].
In the TEP procedure, mesh fixation was not necessary. In cases where mesh fixation was not used, there was no difference in recurrence, incidence of seroma, or postoperative or chronic pain[175].
In the guidelines for endoscopic hernia repair, the EAES Consensus (European Association of Endoscopic Surgeons), and the International Endohernia Society recommend technical points for a tailored approach to specific hernias on the basis of evidence[176-178].
Incisional hernia: Laparoscopic surgery for repair of an incisional hernia shows no difference in recurrence or length of hospital stay compared with open surgery. There were significantly fewer wound infections and complications requiring mesh removal[179]. Risk of bowel injury increased, while postoperative pain score showed no significant difference. Long-term results were not available from the current data[180].
A comparison of the data was difficult. There were many studies, reviews and meta-analyses regarding ventral hernia and incisional hernia, although the origin of these hernias was different. Furthermore, the optimal mesh was not found and neither was the optimal mesh fixation[181], which is why long-term results with a high level of evidence are not available[182].
The results on incisional hernia were highly biased due to methodical limitations. It was hard to distinguish whether patient-related factors or technique-related factors, such as type of mesh and fixation, influenced the outcome[183]. Compared with open surgery, there was a longer duration of operation with no difference in the short-term adverse events[184]. The incidence of wound infection was significantly decreased[185]. There was no difference in the overall recurrence. There was a lack of randomized controlled trials with a standardized technique to demonstrate one technique’s superiority over the other[186].
DISCUSSION
Laparoscopic surgery has continuously developed over the past years, advancing from an invasive diagnostic tool to an efficient instrument for surgical treatment of benign and malignant disease. Ongoing training, experience, and development in imaging and laparoscopic instruments have facilitated extension of the applications of laparoscopic surgery.
The overall advantage of minimizing trauma to the abdominal wall has been reproducible in many of the laparoscopic procedures compared with open surgery. Faster convalescence, reduced hospital stay, and faster return to normal activity are the most evident advantages of laparoscopic surgery. The outcome, efficiency, decreased incidence of wound infections, and reduced perioperative morbidity of minimally invasive procedures have been shown across different applications, e.g., cholecystectomy, fundoplication, and adrenalectomy. Despite the lack of randomized controlled trials to support laparoscopic applications, these procedures are accepted as the gold standard for surgical intervention. The laparoscopic surgeries are longer than the open ones. However, the duration has decreased over the years through experience and the learning curve. There has been no evidence that open surgery is superior to laparoscopic surgery in terms of oncological short- and long-term outcomes.
Interpretation of the data in meta-analyses or reviews was at times difficult. Different laparoscopic techniques were mixed up under one indication, e.g., in incisional hernia repair. The use of different mesh and types of fixation led to heterogeneity in the compared studies. The possibility of bias as a methodical limitation was high.
Demonstrating the superiority of laparoscopy over other techniques, such as single-incision surgery, NOTES, and robotic surgery was difficult. Cost and effort were the major drawbacks in distribution of these techniques, particularly for the robotic surgery.
Randomized controlled trials in some fields of laparoscopic surgery could not be performed. There is a lack of sufficient evidence, because, for example, sample size calculation to achieve a certain power is too high to conduct such a study in daily surgical routine. There is a need for randomized controlled studies and standardization because many results were interpreted from case reports or cohort series, and were difficult to compare. This is especially needed in technically demanding procedures like laparoscopic gastric, pancreatic and esophagus surgeries.
COMMENTS
Background
Laparoscopic surgery is a technique with a widespread field of applications. In some medical fields, the laparoscopic approach is a standard, e.g., cholecystectomy. Due to the continuous surgical training and the ongoing development of instruments, imaging systems and surgical techniques, highly complex laparoscopic procedures are possible, such as laparoscopic gastrectomy. The primary aim of this review is to show a variety of different laparoscopic surgeries and to assess their benefits and outcomes in benign and malignant diseases.
Research frontiers
This review is a clinical evaluation of laparoscopic surgery and its role in the surgical treatment of benign and malignant disease of different organ systems. Since the first laparoscopic appendectomy and the first laparoscopic cholecystectomy, there has been an overwhelming development of the technique. Therefore, this review shows a complete summary of the most frequent procedures used for digestive diseases and performed with a minimally invasive approach.
Innovations and breakthroughs
No other surgical technique has gone through such advances as laparoscopic surgery over the years, including approaches such as robotic or single-port surgery. This review summarizes the current literature (review articles, meta-analyses, and randomized trials) to give an overview of the laparoscopic procedures.
Applications
Laparoscopic surgery has become a state of the art technique in many fields of surgical treatment, providing better clinical outcomes than open surgery without compromising the oncological results.
Peer-review
The authors have performed a good study. The manuscript is interesting.
Footnotes
P- Reviewer: Chen GS, Ciccone MM, Neri V S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
Conflict-of-interest statement: All the authors declare no conflict of interest.
Data sharing statement: No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: May 8, 2015
First decision: June 18, 2015
Article in press: November 25, 2015
References
- 1.Reynolds W. The first laparoscopic cholecystectomy. JSLS. 2001;5:89–94. [PMC free article] [PubMed] [Google Scholar]
- 2.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg. 2012;16:1929–1939. doi: 10.1007/s11605-012-1972-9. [DOI] [PubMed] [Google Scholar]
- 4.Thomson JE, Kruger D, Jann-Kruger C, Kiss A, Omoshoro-Jones JA, Luvhengo T, Brand M. Laparoscopic versus open surgery for complicated appendicitis: a randomized controlled trial to prove safety. Surg Endosc. 2015;29:2027–2032. doi: 10.1007/s00464-014-3906-y. [DOI] [PubMed] [Google Scholar]
- 5.Markides G, Subar D, Riyad K. Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg. 2010;34:2026–2040. doi: 10.1007/s00268-010-0669-z. [DOI] [PubMed] [Google Scholar]
- 6.Li X, Zhang J, Sang L, Zhang W, Chu Z, Li X, Liu Y. Laparoscopic versus conventional appendectomy--a meta-analysis of randomized controlled trials. BMC Gastroenterol. 2010;10:129. doi: 10.1186/1471-230X-10-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wei B, Qi CL, Chen TF, Zheng ZH, Huang JL, Hu BG, Wei HB. Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc. 2011;25:1199–1208. doi: 10.1007/s00464-010-1344-z. [DOI] [PubMed] [Google Scholar]
- 8.Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg. 1998;186:545–553. doi: 10.1016/s1072-7515(98)00080-5. [DOI] [PubMed] [Google Scholar]
- 9.Markar SR, Penna M, Harris A. Laparoscopic approach to appendectomy reduces the incidence of short- and long-term post-operative bowel obstruction: systematic review and pooled analysis. J Gastrointest Surg. 2014;18:1683–1692. doi: 10.1007/s11605-014-2572-7. [DOI] [PubMed] [Google Scholar]
- 10.Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2004;(4):CD001546. doi: 10.1002/14651858.CD001546.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Woodham BL, Cox MR, Eslick GD. Evidence to support the use of laparoscopic over open appendicectomy for obese individuals: a meta-analysis. Surg Endosc. 2012;26:2566–2570. doi: 10.1007/s00464-012-2233-4. [DOI] [PubMed] [Google Scholar]
- 12.Wilasrusmee C, Sukrat B, McEvoy M, Attia J, Thakkinstian A. Systematic review and meta-analysis of safety of laparoscopic versus open appendicectomy for suspected appendicitis in pregnancy. Br J Surg. 2012;99:1470–1478. doi: 10.1002/bjs.8889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Antoniou SA, Koch OO, Antoniou GA, Lasithiotakis K, Chalkiadakis GE, Pointner R, Granderath FA. Meta-analysis of randomized trials on single-incision laparoscopic versus conventional laparoscopic appendectomy. Am J Surg. 2014;207:613–622. doi: 10.1016/j.amjsurg.2013.07.045. [DOI] [PubMed] [Google Scholar]
- 14.Li P, Chen ZH, Li QG, Qiao T, Tian YY, Wang DR. Safety and efficacy of single-incision laparoscopic surgery for appendectomies: a meta-analysis. World J Gastroenterol. 2013;19:4072–4082. doi: 10.3748/wjg.v19.i25.4072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Markar SR, Karthikesalingam A, Di Franco F, Harris AM. Systematic review and meta-analysis of single-incision versus conventional multiport appendicectomy. Br J Surg. 2013;100:1709–1718. doi: 10.1002/bjs.9296. [DOI] [PubMed] [Google Scholar]
- 16.Xu AM, Huang L, Li TJ. Single-incision versus three-port laparoscopic appendectomy for acute appendicitis: systematic review and meta-analysis of randomized controlled trials. Surg Endosc. 2015;29:822–843. doi: 10.1007/s00464-014-3735-z. [DOI] [PubMed] [Google Scholar]
- 17.Clerveus M, Morandeira-Rivas A, Moreno-Sanz C, Herrero-Bogajo ML, Picazo-Yeste JS, Tadeo-Ruiz G. Systematic review and meta-analysis of randomized controlled trials comparing single incision versus conventional laparoscopic appendectomy. World J Surg. 2014;38:1937–1946. doi: 10.1007/s00268-014-2535-x. [DOI] [PubMed] [Google Scholar]
- 18.Qiu J, Yuan H, Chen S, He Z, Wu H. Single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy: evidence from randomized controlled trials and nonrandomized comparative studies. Surg Laparosc Endosc Percutan Tech. 2014;24:12–21. doi: 10.1097/SLE.0b013e3182937da4. [DOI] [PubMed] [Google Scholar]
- 19.Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006;(4):CD006231. doi: 10.1002/14651858.CD006231. [DOI] [PubMed] [Google Scholar]
- 20.Purkayastha S, Tilney HS, Georgiou P, Athanasiou T, Tekkis PP, Darzi AW. Laparoscopic cholecystectomy versus mini-laparotomy cholecystectomy: a meta-analysis of randomised control trials. Surg Endosc. 2007;21:1294–1300. doi: 10.1007/s00464-007-9210-3. [DOI] [PubMed] [Google Scholar]
- 21.Keus F, Gooszen HG, van Laarhoven CJ. Open, small-incision, or laparoscopic cholecystectomy for patients with symptomatic cholecystolithiasis. An overview of Cochrane Hepato-Biliary Group reviews. Cochrane Database Syst Rev. 2010;(1):CD008318. doi: 10.1002/14651858.CD008318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Meta-analysis of laparoscopic vs open cholecystectomy in elderly patients. World J Gastroenterol. 2014;20:17626–17634. doi: 10.3748/wjg.v20.i46.17626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Goede B, Klitsie PJ, Hagen SM, van Kempen BJ, Spronk S, Metselaar HJ, Lange JF, Kazemier G. Meta-analysis of laparoscopic versus open cholecystectomy for patients with liver cirrhosis and symptomatic cholecystolithiasis. Br J Surg. 2013;100:209–216. doi: 10.1002/bjs.8911. [DOI] [PubMed] [Google Scholar]
- 24.Laurence JM, Tran PD, Richardson AJ, Pleass HC, Lam VW. Laparoscopic or open cholecystectomy in cirrhosis: a systematic review of outcomes and meta-analysis of randomized trials. HPB (Oxford) 2012;14:153–161. doi: 10.1111/j.1477-2574.2011.00425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ford JA, Soop M, Du J, Loveday BP, Rodgers M. Systematic review of intraoperative cholangiography in cholecystectomy. Br J Surg. 2012;99:160–167. doi: 10.1002/bjs.7809. [DOI] [PubMed] [Google Scholar]
- 26.Sajid MS, Leaver C, Haider Z, Worthington T, Karanjia N, Singh KK. Routine on-table cholangiography during cholecystectomy: a systematic review. Ann R Coll Surg Engl. 2012;94:375–380. doi: 10.1308/003588412X13373405385331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gurusamy K, Sahay SJ, Burroughs AK, Davidson BR. Systematic review and meta-analysis of intraoperative versus preoperative endoscopic sphincterotomy in patients with gallbladder and suspected common bile duct stones. Br J Surg. 2011;98:908–916. doi: 10.1002/bjs.7460. [DOI] [PubMed] [Google Scholar]
- 28.Sun S, Yang K, Gao M, He X, Tian J, Ma B. Three-port versus four-port laparoscopic cholecystectomy: meta-analysis of randomized clinical trials. World J Surg. 2009;33:1904–1908. doi: 10.1007/s00268-009-0108-1. [DOI] [PubMed] [Google Scholar]
- 29.Sajid MS, Khan MA, Ray K, Cheek E, Baig MK. Needlescopic versus laparoscopic cholecystectomy: a meta-analysis. ANZ J Surg. 2009;79:437–442. doi: 10.1111/j.1445-2197.2009.04945.x. [DOI] [PubMed] [Google Scholar]
- 30.Li L, Tian J, Tian H, Sun R, Wang Q, Yang K. The efficacy and safety of different kinds of laparoscopic cholecystectomy: a network meta analysis of 43 randomized controlled trials. PLoS One. 2014;9:e90313. doi: 10.1371/journal.pone.0090313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pisanu A, Reccia I, Porceddu G, Uccheddu A. Meta-analysis of prospective randomized studies comparing single-incision laparoscopic cholecystectomy (SILC) and conventional multiport laparoscopic cholecystectomy (CMLC) J Gastrointest Surg. 2012;16:1790–1801. doi: 10.1007/s11605-012-1956-9. [DOI] [PubMed] [Google Scholar]
- 32.Geng L, Sun C, Bai J. Single incision versus conventional laparoscopic cholecystectomy outcomes: a meta-analysis of randomized controlled trials. PLoS One. 2013;8:e76530. doi: 10.1371/journal.pone.0076530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arezzo A, Scozzari G, Famiglietti F, Passera R, Morino M. Is single-incision laparoscopic cholecystectomy safe? Results of a systematic review and meta-analysis. Surg Endosc. 2013;27:2293–2304. doi: 10.1007/s00464-012-2763-9. [DOI] [PubMed] [Google Scholar]
- 34.Qiu J, Yuan H, Chen S, He Z, Han P, Wu H. Single-port versus conventional multiport laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials and nonrandomized studies. J Laparoendosc Adv Surg Tech A. 2013;23:815–831. doi: 10.1089/lap.2013.0040. [DOI] [PubMed] [Google Scholar]
- 35.Zehetner J, Pelipad D, Darehzereshki A, Mason RJ, Lipham JC, Katkhouda N. Single-access laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a systematic review and meta-analysis of randomized controlled trials. Surg Laparosc Endosc Percutan Tech. 2013;23:235–243. doi: 10.1097/SLE.0b013e31828b8b4e. [DOI] [PubMed] [Google Scholar]
- 36.Sajid MS, Ladwa N, Kalra L, Hutson KK, Singh KK, Sayegh M. Single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: meta-analysis and systematic review of randomized controlled trials. World J Surg. 2012;36:2644–2653. doi: 10.1007/s00268-012-1719-5. [DOI] [PubMed] [Google Scholar]
- 37.Sodergren MH, Markar S, Pucher PH, Badran IA, Jiao LR, Darzi A. Safety of transvaginal hybrid NOTES cholecystectomy: a systematic review and meta-analysis. Surg Endosc. 2015;29:2077–2090. doi: 10.1007/s00464-014-3915-x. [DOI] [PubMed] [Google Scholar]
- 38.Herbella FA, Patti MG. Minimally invasive esophagectomy. World J Gastroenterol. 2010;16:3811–3815. doi: 10.3748/wjg.v16.i30.3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Butler N, Collins S, Memon B, Memon MA. Minimally invasive oesophagectomy: current status and future direction. Surg Endosc. 2011;25:2071–2083. doi: 10.1007/s00464-010-1511-2. [DOI] [PubMed] [Google Scholar]
- 40.Watanabe M, Baba Y, Nagai Y, Baba H. Minimally invasive esophagectomy for esophageal cancer: an updated review. Surg Today. 2013;43:237–244. doi: 10.1007/s00595-012-0300-z. [DOI] [PubMed] [Google Scholar]
- 41.Hanna GB, Arya S, Markar SR. Variation in the standard of minimally invasive esophagectomy for cancer--systematic review. Semin Thorac Cardiovasc Surg. 2012;24:176–187. doi: 10.1053/j.semtcvs.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 42.Safranek PM, Cubitt J, Booth MI, Dehn TC. Review of open and minimal access approaches to oesophagectomy for cancer. Br J Surg. 2010;97:1845–1853. doi: 10.1002/bjs.7231. [DOI] [PubMed] [Google Scholar]
- 43.Dantoc MM, Cox MR, Eslick GD. Does minimally invasive esophagectomy (MIE) provide for comparable oncologic outcomes to open techniques? A systematic review. J Gastrointest Surg. 2012;16:486–494. doi: 10.1007/s11605-011-1792-3. [DOI] [PubMed] [Google Scholar]
- 44.Cash JC, Zehetner J, Hedayati B, Bildzukewicz NA, Katkhouda N, Mason RJ, Lipham JC. Outcomes following laparoscopic transhiatal esophagectomy for esophageal cancer. Surg Endosc. 2014;28:492–499. doi: 10.1007/s00464-013-3230-y. [DOI] [PubMed] [Google Scholar]
- 45.Dantoc M, Cox MR, Eslick GD. Evidence to support the use of minimally invasive esophagectomy for esophageal cancer: a meta-analysis. Arch Surg. 2012;147:768–776. doi: 10.1001/archsurg.2012.1326. [DOI] [PubMed] [Google Scholar]
- 46.Zhang J, Wang R, Liu S, Luketich JD, Chen S, Chen H, Schuchert MJ. Refinement of minimally invasive esophagectomy techniques after 15 years of experience. J Gastrointest Surg. 2012;16:1768–1774. doi: 10.1007/s11605-012-1950-2. [DOI] [PubMed] [Google Scholar]
- 47.Luketich JD, Pennathur A, Awais O, Levy RM, Keeley S, Shende M, Christie NA, Weksler B, Landreneau RJ, Abbas G, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg. 2012;256:95–103. doi: 10.1097/SLA.0b013e3182590603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Burdall OC, Boddy AP, Fullick J, Blazeby J, Krysztopik R, Streets C, Hollowood A, Barham CP, Titcomb D. A comparative study of survival after minimally invasive and open oesophagectomy. Surg Endosc. 2015;29:431–437. doi: 10.1007/s00464-014-3694-4. [DOI] [PubMed] [Google Scholar]
- 49.Peters MJ, Mukhtar A, Yunus RM, Khan S, Pappalardo J, Memon B, Memon MA. Meta-analysis of randomized clinical trials comparing open and laparoscopic anti-reflux surgery. Am J Gastroenterol. 2009;104:1548–1561; quiz 1547, 1562. doi: 10.1038/ajg.2009.176. [DOI] [PubMed] [Google Scholar]
- 50.Memon MA, Subramanya MS, Hossain MB, Yunus RM, Khan S, Memon B. Laparoscopic anterior versus posterior fundoplication for gastro-esophageal reflux disease: a meta-analysis and systematic review. World J Surg. 2015;39:981–996. doi: 10.1007/s00268-014-2889-0. [DOI] [PubMed] [Google Scholar]
- 51.Rickenbacher N, Kötter T, Kochen MM, Scherer M, Blozik E. Fundoplication versus medical management of gastroesophageal reflux disease: systematic review and meta-analysis. Surg Endosc. 2014;28:143–155. doi: 10.1007/s00464-013-3140-z. [DOI] [PubMed] [Google Scholar]
- 52.Khatri K, Sajid MS, Brodrick R, Baig MK, Sayegh M, Singh KK. Laparoscopic Nissen fundoplication with or without short gastric vessel division: a meta-analysis. Surg Endosc. 2012;26:970–978. doi: 10.1007/s00464-011-1979-4. [DOI] [PubMed] [Google Scholar]
- 53.Markar SR, Karthikesalingam AP, Wagner OJ, Jackson D, Hewes JC, Vyas S, Hashemi M. Systematic review and meta-analysis of laparoscopic Nissen fundoplication with or without division of the short gastric vessels. Br J Surg. 2011;98:1056–1062. doi: 10.1002/bjs.7519. [DOI] [PubMed] [Google Scholar]
- 54.Engström C, Jamieson GG, Devitt PG, Watson DI. Meta-analysis of two randomized controlled trials to identify long-term symptoms after division of the short gastric vessels during Nissen fundoplication. Br J Surg. 2011;98:1063–1067. doi: 10.1002/bjs.7563. [DOI] [PubMed] [Google Scholar]
- 55.Broeders JA, Mauritz FA, Ahmed Ali U, Draaisma WA, Ruurda JP, Gooszen HG, Smout AJ, Broeders IA, Hazebroek EJ. Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Br J Surg. 2010;97:1318–1330. doi: 10.1002/bjs.7174. [DOI] [PubMed] [Google Scholar]
- 56.Shan CX, Zhang W, Zheng XM, Jiang DZ, Liu S, Qiu M. Evidence-based appraisal in laparoscopic Nissen and Toupet fundoplications for gastroesophageal reflux disease. World J Gastroenterol. 2010;16:3063–3071. doi: 10.3748/wjg.v16.i24.3063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Broeders JA, Roks DJ, Ahmed Ali U, Draaisma WA, Smout AJ, Hazebroek EJ. Laparoscopic anterior versus posterior fundoplication for gastroesophageal reflux disease: systematic review and meta-analysis of randomized clinical trials. Ann Surg. 2011;254:39–47. doi: 10.1097/SLA.0b013e31821d4ba0. [DOI] [PubMed] [Google Scholar]
- 58.Mi J, Kang Y, Chen X, Wang B, Wang Z. Whether robot-assisted laparoscopic fundoplication is better for gastroesophageal reflux disease in adults: a systematic review and meta-analysis. Surg Endosc. 2010;24:1803–1814. doi: 10.1007/s00464-009-0873-9. [DOI] [PubMed] [Google Scholar]
- 59.Parisi A, Nguyen NT, Reim D, Zhang S, Jiang ZW, Brower ST, Azagra JS, Facy O, Alimoglu O, Jackson PG, et al. Current status of minimally invasive surgery for gastric cancer: A literature review to highlight studies limits. Int J Surg. 2015;17:34–40. doi: 10.1016/j.ijsu.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 60.Zhang CD, Chen SC, Feng ZF, Zhao ZM, Wang JN, Dai DQ. Laparoscopic versus open gastrectomy for early gastric cancer in Asia: a meta-analysis. Surg Laparosc Endosc Percutan Tech. 2013;23:365–377. doi: 10.1097/SLE.0b013e31828e3e6e. [DOI] [PubMed] [Google Scholar]
- 61.Inokuchi M, Sugita H, Otsuki S, Sato Y, Nakagawa M, Kojima K. Laparoscopic distal gastrectomy reduced surgical site infection as compared with open distal gastrectomy for gastric cancer in a meta-analysis of both randomized controlled and case-controlled studies. Int J Surg. 2015;15:61–67. doi: 10.1016/j.ijsu.2015.01.030. [DOI] [PubMed] [Google Scholar]
- 62.Sun J, Li J, Wang J, Pan T, Zhou J, Fu X, Zhang S. Meta-analysis of randomized controlled trials on laparoscopic gastrectomy vs. open gastrectomy for distal gastric cancer. Hepatogastroenterology. 2012;59:1699–1705. doi: 10.5754/hge12259. [DOI] [PubMed] [Google Scholar]
- 63.Zeng YK, Yang ZL, Peng JS, Lin HS, Cai L. Laparoscopy-assisted versus open distal gastrectomy for early gastric cancer: evidence from randomized and nonrandomized clinical trials. Ann Surg. 2012;256:39–52. doi: 10.1097/SLA.0b013e3182583e2e. [DOI] [PubMed] [Google Scholar]
- 64.Viñuela EF, Gonen M, Brennan MF, Coit DG, Strong VE. Laparoscopic versus open distal gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized studies. Ann Surg. 2012;255:446–456. doi: 10.1097/SLA.0b013e31824682f4. [DOI] [PubMed] [Google Scholar]
- 65.Lu C, Zhou S, Peng Z, Chen L. Quality of D2 lymphadenectomy for advanced gastric cancer: is laparoscopic-assisted distal gastrectomy as effective as open distal gastrectomy? Surg Endosc. 2015;29:1537–1544. doi: 10.1007/s00464-014-3838-6. [DOI] [PubMed] [Google Scholar]
- 66.Ding J, Liao GQ, Liu HL, Liu S, Tang J. Meta-analysis of laparoscopy-assisted distal gastrectomy with D2 lymph node dissection for gastric cancer. J Surg Oncol. 2012;105:297–303. doi: 10.1002/jso.22098. [DOI] [PubMed] [Google Scholar]
- 67.Oh SY, Kwon S, Lee KG, Suh YS, Choe HN, Kong SH, Lee HJ, Kim WH, Yang HK. Outcomes of minimally invasive surgery for early gastric cancer are comparable with those for open surgery: analysis of 1,013 minimally invasive surgeries at a single institution. Surg Endosc. 2014;28:789–795. doi: 10.1007/s00464-013-3256-1. [DOI] [PubMed] [Google Scholar]
- 68.Kunisaki C, Makino H, Takagawa R, Kimura J, Ota M, Ichikawa Y, Kosaka T, Akiyama H, Endo I. A systematic review of laparoscopic total gastrectomy for gastric cancer. Gastric Cancer. 2015;18:218–226. doi: 10.1007/s10120-015-0474-3. [DOI] [PubMed] [Google Scholar]
- 69.Lee HJ, Yang HK. Laparoscopic gastrectomy for gastric cancer. Dig Surg. 2013;30:132–141. doi: 10.1159/000350884. [DOI] [PubMed] [Google Scholar]
- 70.Choi YY, Bae JM, An JY, Hyung WJ, Noh SH. Laparoscopic gastrectomy for advanced gastric cancer: are the long-term results comparable with conventional open gastrectomy? A systematic review and meta-analysis. J Surg Oncol. 2013;108:550–556. doi: 10.1002/jso.23438. [DOI] [PubMed] [Google Scholar]
- 71.Chen XZ, Wen L, Rui YY, Liu CX, Zhao QC, Zhou ZG, Hu JK. Long-term survival outcomes of laparoscopic versus open gastrectomy for gastric cancer: a systematic review and meta-analysis. Medicine (Baltimore) 2015;94:e454. doi: 10.1097/MD.0000000000000454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Koh YX, Chok AY, Zheng HL, Tan CS, Chow PK, Wong WK, Goh BK. A systematic review and meta-analysis comparing laparoscopic versus open gastric resections for gastrointestinal stromal tumors of the stomach. Ann Surg Oncol. 2013;20:3549–3560. doi: 10.1245/s10434-013-3051-1. [DOI] [PubMed] [Google Scholar]
- 73.Zheng L, Ding W, Zhou D, Lu L, Yao L. Laparoscopic versus open resection for gastric gastrointestinal stromal tumors: a meta-analysis. Am Surg. 2014;80:48–56. [PubMed] [Google Scholar]
- 74.Lee J, Kim Y-M, Woo Y, Obama K, Noh SH, Hyung WJ. Robotic distal subtotal gastrectomy with D2 lymphadenectomy for gastric cancer patients with high body mass index: comparison with conventional laparoscopic distal subtotal gastrectomy with D2 lymphadenectomy. Surg Endosc. 2015:Jan 29; Epub ahead of print. doi: 10.1007/s00464-015-4069-1. [DOI] [PubMed] [Google Scholar]
- 75.Xiong B, Ma L, Zhang C. Robotic versus laparoscopic gastrectomy for gastric cancer: a meta-analysis of short outcomes. Surg Oncol. 2012;21:274–280. doi: 10.1016/j.suronc.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 76.Spanjersberg WR, van Sambeeck JDP, Bremers A, Rosman C, van Laarhoven CJHM. Systematic review and meta-analysis for laparoscopic versus open colon surgery with or without an ERAS programme. Surg Endosc. 2015:Mar 24; Epub ahead of print. doi: 10.1007/s00464-015-4148-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Esteban F, Cerdan FJ, Garcia-Alonso M, Sanz-Lopez R, Arroyo A, Ramirez JM, Moreno C, Morales R, Navarro A, Fuentes M. A multicentre comparison of a fast track or conventional postoperative protocol following laparoscopic or open elective surgery for colorectal cancer surgery. Colorectal Dis. 2014;16:134–140. doi: 10.1111/codi.12472. [DOI] [PubMed] [Google Scholar]
- 78.Jones OM, Lindsey I, Cunningham C. Laparoscopic colorectal surgery. BMJ. 2011;343:d8029. doi: 10.1136/bmj.d8029. [DOI] [PubMed] [Google Scholar]
- 79.Tan JJ, Tjandra JJ. Laparoscopic surgery for ulcerative colitis - a meta-analysis. Colorectal Dis. 2006;8:626–636. doi: 10.1111/j.1463-1318.2006.00971.x. [DOI] [PubMed] [Google Scholar]
- 80.Dasari BV, McKay D, Gardiner K. Laparoscopic versus Open surgery for small bowel Crohn’s disease. Cochrane Database Syst Rev. 2011;(1):CD006956. doi: 10.1002/14651858.CD006956.pub2. [DOI] [PubMed] [Google Scholar]
- 81.Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Is laparoscopic ileocecal resection a safe option for Crohn’s disease? Best evidence topic. Int J Surg. 2014;12:22–25. doi: 10.1016/j.ijsu.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 82.Gervaz P, Inan I, Perneger T, Schiffer E, Morel P. A prospective, randomized, single-blind comparison of laparoscopic versus open sigmoid colectomy for diverticulitis. Ann Surg. 2010;252:3–8. doi: 10.1097/SLA.0b013e3181dbb5a5. [DOI] [PubMed] [Google Scholar]
- 83.Klarenbeek BR, Veenhof AA, Bergamaschi R, van der Peet DL, van den Broek WT, de Lange ES, Bemelman WA, Heres P, Lacy AM, Engel AF, et al. Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma Trial. Ann Surg. 2009;249:39–44. doi: 10.1097/SLA.0b013e31818e416a. [DOI] [PubMed] [Google Scholar]
- 84.Jones OM, Stevenson AR, Clark D, Stitz RW, Lumley JW. Laparoscopic resection for diverticular disease: follow-up of 500 consecutive patients. Ann Surg. 2008;248:1092–1097. doi: 10.1097/SLA.0b013e3181884923. [DOI] [PubMed] [Google Scholar]
- 85.Siddiqui MR, Sajid MS, Qureshi S, Cheek E, Baig MK. Elective laparoscopic sigmoid resection for diverticular disease has fewer complications than conventional surgery: a meta-analysis. Am J Surg. 2010;200:144–161. doi: 10.1016/j.amjsurg.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 86.Cirocchi R, Farinella E, Trastulli S, Sciannameo F, Audisio RA. Elective sigmoid colectomy for diverticular disease. Laparoscopic vs open surgery: A systematic review. Color Dis. 2012;14:671–683. doi: 10.1111/j.1463-1318.2011.02666.x. [DOI] [PubMed] [Google Scholar]
- 87.Moloo H, Haggar F, Coyle D, Hutton B, Duhaime S, Mamazza J, Poulin EC, Boushey RP, Grimshaw J. Hand assisted laparoscopic surgery versus conventional laparoscopy for colorectal surgery. Cochrane Database Syst Rev. 2010;(10):CD006585. doi: 10.1002/14651858.CD006585.pub2. [DOI] [PubMed] [Google Scholar]
- 88.Myers E, Hurley M, O’Sullivan GC, Kavanagh D, Wilson I, Winter DC. Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg. 2008;95:97–101. doi: 10.1002/bjs.6024. [DOI] [PubMed] [Google Scholar]
- 89.Wolthuis AM, Penninckx F, D’Hoore A. Laparoscopic sigmoid resection with transrectal specimen extraction has a good short-term outcome. Surg Endosc. 2011;25:2034–2038. doi: 10.1007/s00464-010-1472-5. [DOI] [PubMed] [Google Scholar]
- 90.Lorenzon L, La Torre M, Ziparo V, Montebelli F, Mercantini P, Balducci G, Ferri M. Evidence based medicine and surgical approaches for colon cancer: evidences, benefits and limitations of the laparoscopic vs open resection. World J Gastroenterol. 2014;20:3680–3692. doi: 10.3748/wjg.v20.i13.3680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Martel G, Crawford A, Barkun JS, Boushey RP, Ramsay CR, Fergusson DA. Expert opinion on laparoscopic surgery for colorectal cancer parallels evidence from a cumulative meta-analysis of randomized controlled trials. PLoS One. 2012;7:e35292. doi: 10.1371/journal.pone.0035292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kuhry E, Schwenk W, Gaupset R, Romild U, Bonjer J. Long-term outcome of laparoscopic surgery for colorectal cancer: a cochrane systematic review of randomised controlled trials. Cancer Treat Rev. 2008;34:498–504. doi: 10.1016/j.ctrv.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 93.Søndenaa K, Quirke P, Hohenberger W, Sugihara K, Kobayashi H, Kessler H, Brown G, Tudyka V, D’Hoore A, Kennedy RH, et al. The rationale behind complete mesocolic excision (CME) and a central vascular ligation for colon cancer in open and laparoscopic surgery: proceedings of a consensus conference. Int J Colorectal Dis. 2014;29:419–428. doi: 10.1007/s00384-013-1818-2. [DOI] [PubMed] [Google Scholar]
- 94.Rondelli F, Trastulli S, Avenia N, Schillaci G, Cirocchi R, Gullà N, Mariani E, Bistoni G, Noya G. Is laparoscopic right colectomy more effective than open resection? A meta-analysis of randomized and nonrandomized studies. Colorectal Dis. 2012;14:e447–e469. doi: 10.1111/j.1463-1318.2012.03054.x. [DOI] [PubMed] [Google Scholar]
- 95.Chand M, Siddiqui MR, Rasheed S, Brown G, Tekkis P, Parvaiz A, Qureshi T. A systematic review and meta-analysis evaluating the role of laparoscopic surgical resection of transverse colon tumours. Surg Endosc. 2014;28:3263–3272. doi: 10.1007/s00464-014-3634-3. [DOI] [PubMed] [Google Scholar]
- 96.Theophilus M, Platell C, Spilsbury K. Long-term survival following laparoscopic and open colectomy for colon cancer: a meta-analysis of randomized controlled trials. Colorectal Dis. 2014;16:O75–O81. doi: 10.1111/codi.12483. [DOI] [PubMed] [Google Scholar]
- 97.Di B, Li Y, Wei K, Xiao X, Shi J, Zhang Y, Yang X, Gao P, Zhang K, Yuan Y, et al. Laparoscopic versus open surgery for colon cancer: a meta-analysis of 5-year follow-up outcomes. Surg Oncol. 2013;22:e39–e43. doi: 10.1016/j.suronc.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 98.Clancy C, O’Leary DP, Burke JP, Redmond HP, Coffey JC, Kerin MJ, Myers E. A meta-analysis to determine the oncological implications of conversion in laparoscopic colorectal cancer surgery. Colorectal Dis. 2015;17:482–490. doi: 10.1111/codi.12875. [DOI] [PubMed] [Google Scholar]
- 99.Liao G, Zhao Z, Lin S, Li R, Yuan Y, Du S, Chen J, Deng H. Robotic-assisted versus laparoscopic colorectal surgery: a meta-analysis of four randomized controlled trials. World J Surg Oncol. 2014;12:122. doi: 10.1186/1477-7819-12-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tou S, Brown SR, Malik AI, Nelson RL. Surgery for complete rectal prolapse in adults. Cochrane Database Syst Rev. 2008;(4):CD001758. doi: 10.1002/14651858.CD001758.pub2. [DOI] [PubMed] [Google Scholar]
- 101.Young MT, Jafari MD, Phelan MJ, Stamos MJ, Mills S, Pigazzi A, Carmichael JC. Surgical treatments for rectal prolapse: how does a perineal approach compare in the laparoscopic era? Surg Endosc. 2015;29:607–613. doi: 10.1007/s00464-014-3707-3. [DOI] [PubMed] [Google Scholar]
- 102.Zhao J, Chen N, Zheng J, He S, Sun X. Laparoscopic versus open surgery for rectal cancer: Results of a systematic review and meta-analysis on clinical efficacy. Mol Clin Oncol. 2014;2:1097–1102. doi: 10.3892/mco.2014.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhang FW, Zhou ZY, Wang HL, Zhang JX, Di BS, Huang WH, Yang KH. Laparoscopic versus open surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. Asian Pac J Cancer Prev. 2014;15:9985–9996. doi: 10.7314/apjcp.2014.15.22.9985. [DOI] [PubMed] [Google Scholar]
- 104.Morino M, Risio M, Bach S, Beets-Tan R, Bujko K, Panis Y, Quirke P, Rembacken B, Rullier E, Saito Y, et al. Early rectal cancer: the European Association for Endoscopic Surgery (EAES) clinical consensus conference. Surg Endosc. 2015;29:755–773. doi: 10.1007/s00464-015-4067-3. [DOI] [PubMed] [Google Scholar]
- 105.Keller DS, Khorgami Z, Swendseid B, Champagne BJ, Reynolds HL, Stein SL, Delaney CP. Laparoscopic and converted approaches to rectal cancer resection have superior long-term outcomes: a comparative study by operative approach. Surg Endosc. 2014;28:1940–1948. doi: 10.1007/s00464-014-3419-8. [DOI] [PubMed] [Google Scholar]
- 106.Chen H, Zhao L, An S, Wu J, Zou Z, Liu H, Li G. Laparoscopic versus open surgery following neoadjuvant chemoradiotherapy for rectal cancer: a systematic review and meta-analysis. J Gastrointest Surg. 2014;18:617–626. doi: 10.1007/s11605-014-2452-1. [DOI] [PubMed] [Google Scholar]
- 107.Lim RS, Yang TX, Chua TC. Postoperative bladder and sexual function in patients undergoing surgery for rectal cancer: a systematic review and meta-analysis of laparoscopic versus open resection of rectal cancer. Tech Coloproctol. 2014;18:993–1002. doi: 10.1007/s10151-014-1189-x. [DOI] [PubMed] [Google Scholar]
- 108.Arezzo A, Passera R, Salvai A, Arolfo S, Allaix ME, Schwarzer G, Morino M. Laparoscopy for rectal cancer is oncologically adequate: a systematic review and meta-analysis of the literature. Surg Endosc. 2015;29:334–348. doi: 10.1007/s00464-014-3686-4. [DOI] [PubMed] [Google Scholar]
- 109.Breukink S, Pierie J, Wiggers T. Laparoscopic versus open total mesorectal excision for rectal cancer. Cochrane Database Syst Rev. 2006;(4):CD005200. doi: 10.1002/14651858.CD005200.pub2. [DOI] [PubMed] [Google Scholar]
- 110.Kelly M, Bhangu A, Singh P, Fitzgerald JE, Tekkis PP. Systematic review and meta-analysis of trainee- versus expert surgeon-performed colorectal resection. Br J Surg. 2014;101:750–759. doi: 10.1002/bjs.9472. [DOI] [PubMed] [Google Scholar]
- 111.Araujo SE, Crawshaw B, Mendes CR, Delaney CP. Transanal total mesorectal excision: a systematic review of the experimental and clinical evidence. Tech Coloproctol. 2015;19:69–82. doi: 10.1007/s10151-014-1233-x. [DOI] [PubMed] [Google Scholar]
- 112.Lin S, Jiang HG, Chen ZH, Zhou SY, Liu XS, Yu JR. Meta-analysis of robotic and laparoscopic surgery for treatment of rectal cancer. World J Gastroenterol. 2011;17:5214–5220. doi: 10.3748/wjg.v17.i47.5214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Trastulli S, Farinella E, Cirocchi R, Cavaliere D, Avenia N, Sciannameo F, Gullà N, Noya G, Boselli C. Robotic resection compared with laparoscopic rectal resection for cancer: systematic review and meta-analysis of short-term outcome. Colorectal Dis. 2012;14:e134–e156. doi: 10.1111/j.1463-1318.2011.02907.x. [DOI] [PubMed] [Google Scholar]
- 114.Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Robot-assisted laparoscopic surgery of the colon and rectum. Surg Endosc. 2012;26:1–11. doi: 10.1007/s00464-011-1867-y. [DOI] [PubMed] [Google Scholar]
- 115.Mak TW, Lee JF, Futaba K, Hon SS, Ngo DK, Ng SS. Robotic surgery for rectal cancer: A systematic review of current practice. World J Gastrointest Oncol. 2014;6:184–193. doi: 10.4251/wjgo.v6.i6.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Baek SK, Carmichael JC, Pigazzi A. Robotic surgery: colon and rectum. Cancer J. 2013;19:140–146. doi: 10.1097/PPO.0b013e31828ba0fd. [DOI] [PubMed] [Google Scholar]
- 117.Winslow E, Hawkins WG. Laparoscopic resection of the liver for cancer. Surg Oncol Clin N Am. 2013;22:75–89, vi. doi: 10.1016/j.soc.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 118.Fancellu A, Rosman AS, Sanna V, Nigri GR, Zorcolo L, Pisano M, Melis M. Meta-analysis of trials comparing minimally-invasive and open liver resections for hepatocellular carcinoma. J Surg Res. 2011;171:e33–e45. doi: 10.1016/j.jss.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 119.Rao A, Rao G, Ahmed I. Laparoscopic left lateral liver resection should be a standard operation. Surg Endosc. 2011;25:1603–1610. doi: 10.1007/s00464-010-1459-2. [DOI] [PubMed] [Google Scholar]
- 120.Rao A, Rao G, Ahmed I. Laparoscopic or open liver resection? Let systematic review decide it. Am J Surg. 2012;204:222–231. doi: 10.1016/j.amjsurg.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 121.Zhou Y, Xiao Y, Wu L, Li B, Li H. Laparoscopic liver resection as a safe and efficacious alternative to open resection for colorectal liver metastasis: a meta-analysis. BMC Surg. 2013;13:44. doi: 10.1186/1471-2482-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Yin Z, Fan X, Ye H, Yin D, Wang J. Short- and long-term outcomes after laparoscopic and open hepatectomy for hepatocellular carcinoma: a global systematic review and meta-analysis. Ann Surg Oncol. 2013;20:1203–1215. doi: 10.1245/s10434-012-2705-8. [DOI] [PubMed] [Google Scholar]
- 123.Li N, Wu YR, Wu B, Lu MQ. Surgical and oncologic outcomes following laparoscopic versus open liver resection for hepatocellular carcinoma: A meta-analysis. Hepatol Res. 2012;42:51–59. doi: 10.1111/j.1872-034X.2011.00890.x. [DOI] [PubMed] [Google Scholar]
- 124.Morise Z, Ciria R, Cherqui D, Chen KH, Belli G, Wakabayashi G. Can we expand the indications for laparoscopic liver resection? A systematic review and meta-analysis of laparoscopic liver resection for patients with hepatocellular carcinoma and chronic liver disease. J Hepatobiliary Pancreat Sci. 2015;22:342–352. doi: 10.1002/jhbp.215. [DOI] [PubMed] [Google Scholar]
- 125.Twaij A, Pucher PH, Sodergren MH, Gall T, Darzi A, Jiao LR. Laparoscopic vs open approach to resection of hepatocellular carcinoma in patients with known cirrhosis: systematic review and meta-analysis. World J Gastroenterol. 2014;20:8274–8281. doi: 10.3748/wjg.v20.i25.8274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Xiong JJ, Altaf K, Javed MA, Huang W, Mukherjee R, Mai G, Sutton R, Liu XB, Hu WM. Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. World J Gastroenterol. 2012;18:6657–6668. doi: 10.3748/wjg.v18.i45.6657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mizuguchi T, Kawamoto M, Meguro M, Shibata T, Nakamura Y, Kimura Y, Furuhata T, Sonoda T, Hirata K. Laparoscopic hepatectomy: a systematic review, meta-analysis, and power analysis. Surg Today. 2011;41:39–47. doi: 10.1007/s00595-010-4337-6. [DOI] [PubMed] [Google Scholar]
- 128.Herbold T, Wahba R, Bangard C, Demir M, Drebber U, Stippel DL. The laparoscopic approach for radiofrequency ablation of hepatocellular carcinoma--indication, technique and results. Langenbecks Arch Surg. 2013;398:47–53. doi: 10.1007/s00423-012-1018-5. [DOI] [PubMed] [Google Scholar]
- 129.Hariharan D, Constantinides V, Kocher HM, Tekkis PP. The role of laparoscopy and laparoscopic ultrasound in the preoperative staging of patients with resectable colorectal liver metastases: a meta-analysis. Am J Surg. 2012;204:84–92. doi: 10.1016/j.amjsurg.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 130.Schiffman SC, Kim KH, Tsung A, Marsh JW, Geller DA. Laparoscopic versus open liver resection for metastatic colorectal cancer: a metaanalysis of 610 patients. Surgery. 2015;157:211–222. doi: 10.1016/j.surg.2014.08.036. [DOI] [PubMed] [Google Scholar]
- 131.Parks KR, Kuo YH, Davis JM, O’ Brien B, Hagopian EJ. Laparoscopic versus open liver resection: a meta-analysis of long-term outcome. HPB (Oxford) 2014;16:109–118. doi: 10.1111/hpb.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Luo LX, Yu ZY, Bai YN. Laparoscopic hepatectomy for liver metastases from colorectal cancer: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2014;24:213–222. doi: 10.1089/lap.2013.0399. [DOI] [PubMed] [Google Scholar]
- 133.Wei M, He Y, Wang J, Chen N, Zhou Z, Wang Z. Laparoscopic versus open hepatectomy with or without synchronous colectomy for colorectal liver metastasis: a meta-analysis. PLoS One. 2014;9:e87461. doi: 10.1371/journal.pone.0087461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Qiu JG, Wu H, Jiang H, Huang JW, Pankaj P, Xu YL, Wang JZ, Zeng Y. Laparoscopic fenestration vs open fenestration in patients with congenital hepatic cysts: a meta-analysis. World J Gastroenterol. 2011;17:3359–3365. doi: 10.3748/wjg.v17.i28.3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Bekheit M, Khafagy P-A, Bucur P, Katri K, Elgendi A, Abdel-salam WN, Vibert E, El-kayal E. Donor safety in live donor laparoscopic liver procurement: systematic review and meta-analysis. Surg Endosc. 2015:Jan 1; Epub ahead of print. doi: 10.1007/s00464-014-4045-1. [DOI] [PubMed] [Google Scholar]
- 136.Nigri G, Rosman AS, Petrucciani N, Fancellu A, Pisano M, Zorcolo L, Ramacciato G, Melis M. Meta-analysis of trials comparing laparoscopic transperitoneal and retroperitoneal adrenalectomy. Surgery. 2013;153:111–119. doi: 10.1016/j.surg.2012.05.042. [DOI] [PubMed] [Google Scholar]
- 137.Constantinides VA, Christakis I, Touska P, Palazzo FF. Systematic review and meta-analysis of retroperitoneoscopic versus laparoscopic adrenalectomy. Br J Surg. 2012;99:1639–1648. doi: 10.1002/bjs.8921. [DOI] [PubMed] [Google Scholar]
- 138.Chen W, Li F, Chen D, Zhu Y, He C, Du Y, Tan W. Retroperitoneal versus transperitoneal laparoscopic adrenalectomy in adrenal tumor: a meta-analysis. Surg Laparosc Endosc Percutan Tech. 2013;23:121–127. doi: 10.1097/SLE.0b013e3182827b57. [DOI] [PubMed] [Google Scholar]
- 139.Chai YJ, Kwon H, Yu HW, Kim SJ, Choi JY, Lee KE, Youn YK. Systematic Review of Surgical Approaches for Adrenal Tumors: Lateral Transperitoneal versus Posterior Retroperitoneal and Laparoscopic versus Robotic Adrenalectomy. Int J Endocrinol. 2014;2014:918346. doi: 10.1155/2014/918346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Walz MK. [Minimally invasive adrenal gland surgery] Chirurg. 1998;69:613–620. doi: 10.1007/s001040050464. [DOI] [PubMed] [Google Scholar]
- 141.Bittner JG, Brunt LM. Evaluation and management of adrenal incidentaloma. J Surg Oncol. 2012;106:557–564. doi: 10.1002/jso.23161. [DOI] [PubMed] [Google Scholar]
- 142.Creamer J, Matthews BD. Laparoscopic adrenalectomy for cancer. Surg Oncol Clin N Am. 2013;22:111–124, vi-vii. doi: 10.1016/j.soc.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 143.Bickenbach KA, Strong VE. Laparoscopic transabdominal lateral adrenalectomy. J Surg Oncol. 2012;106:611–618. doi: 10.1002/jso.23250. [DOI] [PubMed] [Google Scholar]
- 144.Muth A, Ragnarsson O, Johannsson G, Wängberg B. Systematic review of surgery and outcomes in patients with primary aldosteronism. Br J Surg. 2015;102:307–317. doi: 10.1002/bjs.9744. [DOI] [PubMed] [Google Scholar]
- 145.Iacobone M, Citton M, Scarpa M, Viel G, Boscaro M, Nitti D. Systematic review of surgical treatment of subclinical Cushing’s syndrome. Br J Surg. 2015;102:318–330. doi: 10.1002/bjs.9742. [DOI] [PubMed] [Google Scholar]
- 146.Wong A, Eloy JA, Liu JK. The role of bilateral adrenalectomy in the treatment of refractory Cushing’s disease. Neurosurg Focus. 2015;38:E9. doi: 10.3171/2014.10.FOCUS14684. [DOI] [PubMed] [Google Scholar]
- 147.Wang L, Wu Z, Li M, Cai C, Liu B, Yang Q, Sun Y. Laparoendoscopic single-site adrenalectomy versus conventional laparoscopic surgery: a systematic review and meta-analysis of observational studies. J Endourol. 2013;27:743–750. doi: 10.1089/end.2012.0599. [DOI] [PubMed] [Google Scholar]
- 148.Hu Q, Gou Y, Sun C, Xu K, Xia G, Ding Q. A systematic review and meta-analysis of current evidence comparing laparoendoscopic single-site adrenalectomy and conventional laparoscopic adrenalectomy. J Endourol. 2013;27:676–683. doi: 10.1089/end.2012.0687. [DOI] [PubMed] [Google Scholar]
- 149.Brandao LF, Autorino R, Laydner H, Haber GP, Ouzaid I, De Sio M, Perdonà S, Stein RJ, Porpiglia F, Kaouk JH. Robotic versus laparoscopic adrenalectomy: a systematic review and meta-analysis. Eur Urol. 2014;65:1154–1161. doi: 10.1016/j.eururo.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 150.Tang K, Li H, Xia D, Yu G, Guo X, Guan W, Xu H, Ye Z. Robot-assisted versus laparoscopic adrenalectomy: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A. 2015;25:187–195. doi: 10.1089/lap.2014.0431. [DOI] [PubMed] [Google Scholar]
- 151.Agcaoglu O, Aliyev S, Karabulut K, Mitchell J, Siperstein A, Berber E. Robotic versus laparoscopic resection of large adrenal tumors. Ann Surg Oncol. 2012;19:2288–2294. doi: 10.1245/s10434-012-2296-4. [DOI] [PubMed] [Google Scholar]
- 152.Moinzadeh A, Gill IS. Robotic adrenalectomy. Urol Clin North Am. 2004;31:753–756. doi: 10.1016/j.ucl.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 153.Giger U, Michel JM, Wiesli P, Schmid C, Krähenbühl L. Laparoscopic surgery for benign lesions of the pancreas. J Laparoendosc Adv Surg Tech A. 2006;16:452–457. doi: 10.1089/lap.2006.16.452. [DOI] [PubMed] [Google Scholar]
- 154.Subar D, Gobardhan PD, Gayet B. Laparoscopic pancreatic surgery: An overview of the literature and experiences of a single center. Best Pract Res Clin Gastroenterol. 2014;28:123–132. doi: 10.1016/j.bpg.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 155.Kooby DA, Gillespie T, Bentrem D, Nakeeb A, Schmidt MC, Merchant NB, Parikh AA, Martin RC, Scoggins CR, Ahmad S, et al. Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann Surg. 2008;248:438–446. doi: 10.1097/SLA.0b013e318185a990. [DOI] [PubMed] [Google Scholar]
- 156.Kooby DA, Hawkins WG, Schmidt CM, Weber SM, Bentrem DJ, Gillespie TW, Sellers JB, Merchant NB, Scoggins CR, Martin RC, et al. A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg. 2010;210:779–785, 786-787. doi: 10.1016/j.jamcollsurg.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 157.Gagner M, Palermo M. Laparoscopic Whipple procedure: review of the literature. J Hepatobiliary Pancreat Surg. 2009;16:726–730. doi: 10.1007/s00534-009-0142-2. [DOI] [PubMed] [Google Scholar]
- 158.Gumbs AA, Rodriguez Rivera AM, Milone L, Hoffman JP. Laparoscopic pancreatoduodenectomy: a review of 285 published cases. Ann Surg Oncol. 2011;18:1335–1341. doi: 10.1245/s10434-010-1503-4. [DOI] [PubMed] [Google Scholar]
- 159.Lai EC, Tang CN. Current status of robot-assisted laparoscopic pancreaticoduodenectomy and distal pancreatectomy: a comprehensive review. Asian J Endosc Surg. 2013;6:158–164. doi: 10.1111/ases.12040. [DOI] [PubMed] [Google Scholar]
- 160.Cirocchi R, Partelli S, Trastulli S, Coratti A, Parisi A, Falconi M. A systematic review on robotic pancreaticoduodenectomy. Surg Oncol. 2013;22:238–246. doi: 10.1016/j.suronc.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 161.Feldman LS. Laparoscopic splenectomy: standardized approach. World J Surg. 2011;35:1487–1495. doi: 10.1007/s00268-011-1059-x. [DOI] [PubMed] [Google Scholar]
- 162.Qian D, He Z, Hua J, Gong J, Lin S, Song Z. Hand-assisted versus conventional laparoscopic splenectomy: a systematic review and meta-analysis. ANZ J Surg. 2014;84:915–920. doi: 10.1111/ans.12597. [DOI] [PubMed] [Google Scholar]
- 163.Makino T, Zhou J, Pankaj P, Peng B. Comparative treatment and literature review for laparoscopic splenectomy alone versus preoperative splenic artery embolization splenectomy. Surg Endosc. 2012;26:2758–2766. doi: 10.1007/s00464-012-2270-z. [DOI] [PubMed] [Google Scholar]
- 164.Wu Z, Reza M, Mayol JA, Blasco JA, Guerra M, Andradas E, Plana MN. Efficacy of the Da Vinci surgical system in abdominal surgery compared with that of laparoscopy: a systematic review and meta-analysis. Ann Surg. 2010;252:254–262. doi: 10.1097/SLA.0b013e3181e6239e. [DOI] [PubMed] [Google Scholar]
- 165.Antoniou SA, Pointner R, Granderath FA. Current treatment concepts for groin hernia. Langenbecks Arch Surg. 2014;399:553–558. doi: 10.1007/s00423-014-1212-8. [DOI] [PubMed] [Google Scholar]
- 166.Antoniou SA, Antoniou GA, Bartsch DK, Fendrich V, Koch OO, Pointner R, Granderath FA. Transabdominal preperitoneal versus totally extraperitoneal repair of inguinal hernia: a meta-analysis of randomized studies. Am J Surg. 2013;206:245–252.e1. doi: 10.1016/j.amjsurg.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 167.O’Reilly EA, Burke JP, O’Connell PR. A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg. 2012;255:846–853. doi: 10.1097/SLA.0b013e31824e96cf. [DOI] [PubMed] [Google Scholar]
- 168.Karthikesalingam A, Markar SR, Holt PJ, Praseedom RK. Meta-analysis of randomized controlled trials comparing laparoscopic with open mesh repair of recurrent inguinal hernia. Br J Surg. 2010;97:4–11. doi: 10.1002/bjs.6902. [DOI] [PubMed] [Google Scholar]
- 169.Sajid MS, Kalra L, Parampalli U, Sains PS, Baig MK. A systematic review and meta-analysis evaluating the effectiveness of lightweight mesh against heavyweight mesh in influencing the incidence of chronic groin pain following laparoscopic inguinal hernia repair. Am J Surg. 2013;205:726–736. doi: 10.1016/j.amjsurg.2012.07.046. [DOI] [PubMed] [Google Scholar]
- 170.Currie A, Andrew H, Tonsi A, Hurley PR, Taribagil S. Lightweight versus heavyweight mesh in laparoscopic inguinal hernia repair: a meta-analysis. Surg Endosc. 2012;26:2126–2133. doi: 10.1007/s00464-012-2179-6. [DOI] [PubMed] [Google Scholar]
- 171.Sajid MS, Leaver C, Baig MK, Sains P. Systematic review and meta-analysis of the use of lightweight versus heavyweight mesh in open inguinal hernia repair. Br J Surg. 2012;99:29–37. doi: 10.1002/bjs.7718. [DOI] [PubMed] [Google Scholar]
- 172.Berney CR, Yeo AE. Mesh fixation with fibrin sealant during endoscopic totally extraperitoneal inguinal hernia approach: a review of 640 repairs. Hernia. 2013;17:709–717. doi: 10.1007/s10029-012-1034-y. [DOI] [PubMed] [Google Scholar]
- 173.Sajid MS, Ladwa N, Kalra L, McFall M, Baig MK, Sains P. A meta-analysis examining the use of tacker mesh fixation versus glue mesh fixation in laparoscopic inguinal hernia repair. Am J Surg. 2013;206:103–111. doi: 10.1016/j.amjsurg.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 174.Kaul A, Hutfless S, Le H, Hamed SA, Tymitz K, Nguyen H, Marohn MR. Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc. 2012;26:1269–1278. doi: 10.1007/s00464-011-2025-2. [DOI] [PubMed] [Google Scholar]
- 175.Teng YJ, Pan SM, Liu YL, Yang KH, Zhang YC, Tian JH, Han JX. A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc. 2011;25:2849–2858. doi: 10.1007/s00464-011-1668-3. [DOI] [PubMed] [Google Scholar]
- 176.Poelman MM, van den Heuvel B, Deelder JD, Abis GS, Beudeker N, Bittner RR, Campanelli G, van Dam D, Dwars BJ, Eker HH, et al. EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc. 2013;27:3505–3519. doi: 10.1007/s00464-013-3001-9. [DOI] [PubMed] [Google Scholar]
- 177.Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)] Surg Endosc. 2011;25:2773–2843. doi: 10.1007/s00464-011-1799-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Bittner R, Montgomery MA, Arregui E, Bansal V, Bingener J, Bisgaard T, Buhck H, Dudai M, Ferzli GS, Fitzgibbons RJ, et al. Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society) Surg Endosc. 2015;29:289–321. doi: 10.1007/s00464-014-3917-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Forbes SS, Eskicioglu C, McLeod RS, Okrainec A. Meta-analysis of randomized controlled trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg. 2009;96:851–858. doi: 10.1002/bjs.6668. [DOI] [PubMed] [Google Scholar]
- 180.Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M. Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev. 2011;(3):CD007781. doi: 10.1002/14651858.CD007781.pub2. [DOI] [PubMed] [Google Scholar]
- 181.Sajid MS, Bokhari SA, Mallick AS, Cheek E, Baig MK. Laparoscopic versus open repair of incisional/ventral hernia: a meta-analysis. Am J Surg. 2009;197:64–72. doi: 10.1016/j.amjsurg.2007.12.051. [DOI] [PubMed] [Google Scholar]
- 182.Kapischke M, Schulz T, Schipper T, Tensfeldt J, Caliebe A. Open versus laparoscopic incisional hernia repair: something different from a meta-analysis. Surg Endosc. 2008;22:2251–2260. doi: 10.1007/s00464-008-9773-7. [DOI] [PubMed] [Google Scholar]
- 183.Müller-Riemenschneider F, Roll S, Friedrich M, Zieren J, Reinhold T, von der Schulenburg JM, Greiner W, Willich SN. Medical effectiveness and safety of conventional compared to laparoscopic incisional hernia repair: a systematic review. Surg Endosc. 2007;21:2127–2136. doi: 10.1007/s00464-007-9513-4. [DOI] [PubMed] [Google Scholar]
- 184.Sains PS, Tilney HS, Purkayastha S, Darzi AW, Athanasiou T, Tekkis PP, Heriot AG. Outcomes following laparoscopic versus open repair of incisional hernia. World J Surg. 2006;30:2056–2064. doi: 10.1007/s00268-006-0026-4. [DOI] [PubMed] [Google Scholar]
- 185.Zhang Y, Zhou H, Chai Y, Cao C, Jin K, Hu Z. Laparoscopic versus open incisional and ventral hernia repair: a systematic review and meta-analysis. World J Surg. 2014;38:2233–2240. doi: 10.1007/s00268-014-2578-z. [DOI] [PubMed] [Google Scholar]
- 186.Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, Memon MA. Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia. 2015;19:449–463. doi: 10.1007/s10029-015-1351-z. [DOI] [PubMed] [Google Scholar]


