Abstract
Developmental dysplasia of the hip (DDH) describes the spectrum of structural abnormalities that involve the growing hip. Early diagnosis and treatment is critical to provide the best possible functional outcome. Persistence of hip dysplasia into adolescence and adulthood may result in abnormal gait, decreased strength and increased rate of degenerative hip and knee joint disease. Despite efforts to recognize and treat all cases of DDH soon after birth, diagnosis is delayed in some children, and outcomes deteriorate with increasing delay of presentation. Different screening programs for DDH were implicated. The suspicion is raised based on a physical examination soon after birth. Radiography and ultrasonography are used to confirm the diagnosis. The role of other imaging modalities, such as magnetic resonance imaging, is still undetermined; however, extensive research is underway on this subject. Treatment depends on the age of the patient and the reducibility of the hip joint. At an early age and up to 6 mo, the main treatment is an abduction brace like the Pavlik harness. If this fails, closed reduction and spica casting is usually done. After the age of 18 mo, treatment usually consists of open reduction and hip reconstruction surgery. Various treatment protocols have been proposed. We summarize the current practice for detection and treatment of DDH, emphasizing updates in screening and treatment during the last two decades.
Keywords: Developmental dysplasia, Newborn, Infant, Children, Hip, Developmental dysplasia of the hip
Core tip: Developmental dysplasia of the hip (DDH) is a common and important topic in pediatric orthopedics. Early diagnosis and treatment are critical. Screening for this condition is of utmost importance. The treatment depends on the age at presentation and the amount of dysplasia of the hip. We summarize the current practice for detection and treatment of DDH, emphasizing updates in screening and treatment during the last two decades.
INTRODUCTION
The term developmental dysplasia of the hip (DDH) describes the whole range of deformities involving the growing hip including frank dislocation, subluxation and instability, and dysplasia of the femoral head and acetabulum. This term replaced the previously accepted “congenital dysplasia of the hip”, which did not describe the developmental aspect of the disorder[1-3].
In a dislocated hip there is no articular contact between the femoral head and the acetabulum. A dislocated hip may be irreducible or reducible. In a subluxated hip, the femoral head is partially displaced from its normal position, but some degree of contact with the acetabulum still remains. The hip is called dislocatable, when application of posteriorly directed force on the hip positioned in adduction, leads to complete displacement of the femoral head from the margins of the acetabulum. Similarly, the hip is called subluxable, if just gliding of the femoral head is noticed. Acetabular dysplasia describes the abnormality in the development of the acetabulum, including an alteration in size, shape and organization[1,4].
Dislocations are divided into two subtypes: Dislocation that occurs in an otherwise healthy infant is called typical and it may occur pre- or post-natally. Dislocation that is associated with neuromuscular disorders is called teratologic and it occurs prenatally[1,3,5].
The normal development of the child’s hip relies on congruent stability of the femoral head within the acetabulum. The hip joint will not develop properly if it stays unstable and anatomically abnormal by walking age[1,6].
Early diagnosis and treatment is critical to provide the best possible functional outcome. Different screening programs have been devised to recognize DDH as soon as possible. Despite efforts to recognize and treat all cases of DDH soon after birth, the diagnosis is delayed in some children. Treatment of DDH changes with the age at presentation. At a later age, treatment involves more extensive surgery with more complications with a worse functional outcome.
INCIDENCE AND RISK FACTORS
The incidence of a dislocated hip at birth is 1:1000-5:1000, the incidence of subluxation and dysplasia is 10:1000; when implementing universal ultrasonographic screening, the reported incidence is 25:1000-50:1000[1,5,7]. The incidence is higher in cultures that still practice swaddling with the lower extremities fully extended and wrapped together. Studies in Native Americans showed, following a change from traditional swaddling to “safe swaddling”, a decrease in the prevalence of dysplasia from 6 times the United States average to the same prevalence as the rest of United States population[6]. Similar experience was documented in Japan and Turkey[8,9]. It has been shown that keeping the legs in a naturally flexed and abducted position without restricting hip motion lessens the risk of DDH[6,10-15]. In “safe swaddling” the infant hips should be positioned in slight flexion; additional free movement in the direction of hip flexion and abduction may have some benefit[13].
Risk factors include female sex (80% of the affected children) probably due to increased ligamentous laxity as a result of the circulating maternal hormone relaxin. The left side is involved in 60% of the children, the right side in 20% and 20% have bilateral involvement. The left side is more commonly involved, perhaps due to the left occiput anterior positioning of most non-breech newborns where the hip is adducted against the mother’s spine with limited space for abduction[1,5].
The breech position is probably the most important single risk factor, whether delivered vaginally or by cesarean section[6,16,17]. Other risk factors include first born children, postural deformities, oligohydramnios and a positive family history[1,18]. Latest evidence suggests that prematurity is not a risk factor for DDH[19].
NATURAL HISTORY
Neonates with mild dysplasia and mild instability noted in the first few weeks of life may have a benign course, with up to 88% resolving by 8 wk of age[6,20]. Those with instability and frank dislocation often have progressive dysplasia. Spontaneous resolution without intervention is unlikely in children over the age of 6 mo[4].
The modifications in the hip joint reflect contracture of the soft tissue and changes in normal growth of the femoral head and acetabulum. Persistent subluxation or dislocation leads to progressive dysplasia of the femoral head and the acetabulum. The labrum may be inverted and serve as mechanical block for concentric reduction of the hip. Other structures that may block reduction are the limbus, which is formed as a pathologic response of the acetabulum to abnormal pressure around the hip; the ligamentum teres, which lengthens and hypertrophies; the pulvinar, a fibro-fatty tissue found in the depth of the acetabulum; the transverse acetabular ligament which contracts; and the capsule that becomes constricted by contracted iliopsoas tendon[1].
Although acetabular changes in DDH are well recognized, little is known about the morphologic changes of the femoral head. A recent study showed that the femoral head in walking children with DDH is often ‘‘less round’’, although the degree of asphericity is extremely variable and not related to the age of the patient. These differences in femoral head sphericity may explain differences in outcome following the same surgical procedure. Further studies are warranted on this matter[21]. It was also shown that hips with different acetabular coverage have distinct proximal femoral shapes[22].
Persistence of hip dysplasia into adolescence and adulthood may result in abnormal gait, decreased strength, limb-length discrepancy with a flexion/adduction deformity of the hip, increased rate of degenerative hip joint disease, postural scoliosis, back pain and ipsilateral genu valgum with consequent arthritis of the knee[23-26]. Patients with unilateral dislocations have a worse prognosis than those with bilateral dislocations because they have problems of limb-length discrepancy, asymmetrical motion and strength, gait disturbance and knee disorders. Patients with chronic subluxation experience symptoms earlier than those with true dislocation[4].
Outcomes after intervention for DDH deteriorate with increasing delay of presentation. A tipping point is reached, probably around the age of eight years, after which complications from treatment may lead to an outcome no better than the untreated clinical course[23,27,28]. The clinical outcome of bilateral DDH treated surgically is worse compared to unilateral cases mainly due to asymmetrical outcome[29].
Avascular necrosis (AVN) of the femoral head is the most feared complication in children with DDH. AVN is iatrogenic and not part of the natural history of the condition. It is potentially devastating and often untreatable[23]. It is commonly accepted that consequences of AVN are more devastating when it occurs at a younger age. The proposed explanation is that the cartilaginous femoral head without an ossific nucleus is more susceptible to ischemia than a more developed femoral head where an ossific nucleus is already present[1,30,31]. However a systematic review of the medical literature did not show any conclusive evidence to support this. The authors conclude that they did not find that the presence of the ossific nucleus had a significant effect on the development of osteonecrosis of any grade after hip reduction in infants with DDH[32].
Surprisingly, a recent study that examined functional outcomes in children with AVN secondary to treatment of DDH at a mean age of 14 years showed that, although there was some limitation in hip function, it was not associated with marked physical disability[33].
SCREENING FOR DDH
Screening is important because the condition is easily treated when caught early, but difficult to treat when detected late and can lead to long-term disability. The physical examination is still the most important means of detection[7,34,35]. In a decision analysis model, the lowest probability of developing degenerative disease of the hip by age 60 was by doing a thorough physical examination of the hip in all newborns[36]. Radiography and sonography are used to confirm the suspicion of DDH. Periodic physical examination should be performed on all children until walking age[5,6]. Despite our better understanding of the pathology and all current methods of screening, many young adults with dysplasia who require hip arthroplasty are not detected at birth[37]. In the future, genetic profiling may improve matters[38].
Physical examination[1,5]
DDH is an evolving process, therefore the physical examination changes as the child grows older. Normal physical examination findings during the immediate postnatal period do not preclude a subsequent diagnosis of DDH[4,39].
All newborn infants should be examined by a physician in the nursery. A general examination should be done to look for associated conditions with an increased prevalence of DDH. Assessment of the hip joint starts with observation for asymmetry - asymmetrical gluteal or thigh skin folds, limb length discrepancy (evaluated by placing the child in a supine position with the hips and knees flexed - unequal knee heights might be noticed - Galeazzi sign), and restricted hip abduction. The Ortolani test in which the dislocated femoral head is reduced into the acetabulum is the most important clinical test to detect dysplasia[40]. The Barlow test in which the examiner dislocates an unstable hip from the acetabulum is also commonly used. Each hip should be examined independently with the other side held in maximum abduction in order to lock the pelvis. Occasionally, soft tissue clicks might be felt during the movement of the hip. In the absence of any other abnormal findings they are considered benign[41].
By the age of 3 mo, the Barlow and Ortolani tests become negative and the limitation of abduction (and asymmetry of abduction) becomes the most reliable sign associated with DDH. A recent study demonstrated that unilateral limitation of hip abduction after eight weeks of age is strongly associated with DDH. The authors recommended that this sign should be actively sought, and if present, should be further evaluated by a formal ultrasound or radiographs. The presence of bilateral limitation of hip adduction was not an accurate sign for DDH[42].
An ambulating child might have a Trendelenburg gait. In children with bilateral dislocation, the diagnosis is more challenging; however, the Trendelenburg sign, waddling gait, and symmetrical but decreased hip abduction might be noticed[4]. Although commonly accepted that DDH can be a cause of walking delay in children, a recent controlled study suggested that even though the median time to the age of independent walking was 1 mo less in healthy controls compared with that of children with late presentation of DDH, this was clinically insignificant as they all walked within the expected time[43].
Imaging
Radiographs of the hips and pelvis have traditionally been used in all children with suspected DDH. However, instability and displacement may be unnoticeable on a simple radiograph during the first few months of life. The ossification center of the femoral head appears by the age of 4-6 mo. At this stage radiographs become more reliable[5]. Real-time ultrasonography has been established as an accurate method for imaging of the hip during the first few months of life[44-50]. In patients treated for DDH, a delay in appearance of the femoral head ossification center is commonly seen, even up to 1 year after hip reduction. This allows continued utilization of ultrasonographic imaging for follow-up[1].
Computed tomography (CT) is useful for assessment of quality of reduction after closed or open reduction and fixation in a spica cast[51]. It is also useful in the treatment of adolescents and young adults, defining the dysplasia and allowing for better selection of the appropriate procedures, including pelvic and/or femoral osteotomies[52]. Although ionizing radiation exposure from a limited CT is low, magnetic resonance imaging (MRI) has been effectively used completely avoiding radiation exposure (Figure 1). However, the use of MRI has been challenging as there is an extensive diversity of sequences described in the literature and the time needed to perform the study may be as long as 30 min, requiring sedation. A recent retrospective study assessed different MRI imaging protocols. The authors found that axial and coronal T2 FSE provided excellent contrast between the femoral ossification center, surrounding cartilage, and the acetabulum in less than 3 min per sequence and provided the potential for a total examination time of less than 15 min[53]. Another group performed a retrospective analysis of contrast-enhanced MRI as a possible predictor of AVN after closed reduction in DDH. They found that a global decreased enhancement was associated with a significantly higher risk of developing AVN[54]. Another recent publication supported these findings[55]. MRI is also useful in the assessment of labral abnormalities. Isolated labral tears are best treated with arthroscopic techniques[52].
Figure 1.
Magnetic resonance imaging of a two-year-old girl with developmental dysplasia of the hip.
Arthrography displays the cartilaginous anatomy of the femoral head and the acetabulum. Therefore it is commonly used as an intraoperative dynamic test to assess the quality of reduction and the stability of the hip joint. It has a central role in the decision making between closed and open reduction[1].
Ultrasonography
Ultrasonographic techniques pioneered by Graf include static and dynamic evaluation of the hip joint. This allows assessment of the static anatomy of the hip and the stability of the femoral head in the acetabular socket[56]. However, ultrasound screening should not be performed before 3-4 wk of age in infants with clinical signs or risk factors for DDH because of the normal physiologic laxity that resolves spontaneously by 6 wk of age[56-58].
Screening of all newborns with ultrasonography led to a high rate of reexaminations and resulted in a large number of hips needlessly treated[59,60]. However, it was reported that the majority of patients in the United States with symptomatic dysplasia of the acetabulum at skeletal maturity do not meet the criteria for selective ultrasound screening[61]. Recently, a large randomized controlled study comparing universal or selective ultrasound screening with well performed physical examination showed higher treatment rates, a slight reduction in late diagnosis of dysplasia which was not significant, and increased treatment rates which were not associated with AVN[62]. A Cochrane review of screening programs for DDH in newborns found that studies that compared the addition of ultrasonography to clinical examination reported that, when ultrasonography was performed on all infants, the rate of treatment increased with no significant change in the rate of late detected dysplasia or surgery. Targeted ultrasonography to infants at high risk of hip dysplasia did not significantly increase the rate of treatment but also did not significantly decrease the rate of late detected dysplasia or surgery[63].
Consequently, ultrasonography is the preferred technique for clarifying physical findings, evaluating a high-risk infant, and monitoring DDH as it is followed and treated. Universal ultrasonography screening of newborn infants is not recommended[5,64-67]. It was shown that mildly dysplastic but stable hips recognized by ultrasonography soon after birth, usually resolve without treatment. Therefore, an active sonographic surveillance strategy is sufficient[68].
Several ultrasonography techniques have been developed to evaluate the relationship between the acetabulum and the femoral head of an infant. The most common ones are the Graf, Harcke, Terjesen and Suzuki methods. The Graf method is composed of a quantitative classification system, while the Harcke and Suzuki methods have qualitative definitions, and the Terjesen method contains both quantitative and qualitative descriptions[69]. Studies that compared the reliability and sensitivity of the Terjesen and Graf methods, reached different conclusions[70,71]. A study that compared the Graf, Suzuki and Harcke methods, a correlation was found between the three methods in normal and dislocated hips; however, Graf type IIa and IIb hips were frequently regarded as normal when evaluated by the other two methods[72]. There is no conclusive evidence to prefer one method over the other. However an effective ultrasonographic method should include simple, precise, quantitative and consistent definitions for a proper examination and diagnosis, and Graf’s method meets all these requirements[69].
Radiography
An AP radiograph of the pelvis is obtained in newborns and infants when other conditions, such as congenital short femur, are suspected. Plain radiography becomes useful for DDH when the femoral head ossification center appears at the age of 4-6 mo. A single AP pelvic view is usually sufficient. If subluxation or dislocation is noted, a frog view should be done to assess reducibility. There is still a debate whether minor radiographic variability in young infants constitutes actual disease[6,73].
Some orientation lines and angles are useful in the assessment of the AP pelvic radiograph of the infant. The femoral head is supposed to be in the lower medial quadrant created by the Hilgenreiner’s and Perkins’ lines. Shenton’s line should be continuous without breaks. The acetabular index becomes lower with age and, if too high, may be a sign of dysplasia[74,75]. The center-edge angle may be calculated when the femoral ossification center appears, which reflects both acetabular coverage and femoral head displacement. In children younger than 3 years, the femoral head ossification center is irregular or incomplete, and thus difficult to measure. For that reason, it should be used in children older than 3-5 years[1] (Figure 2).
Figure 2.
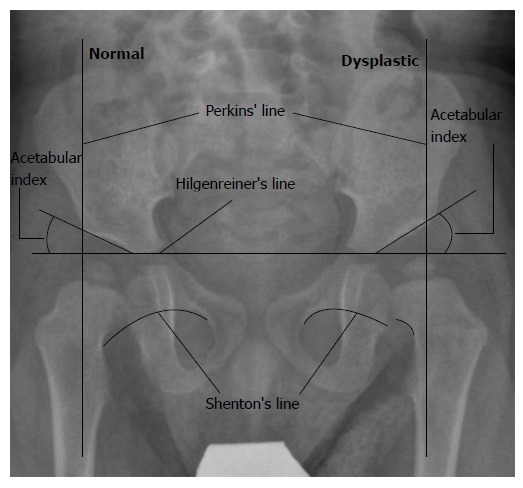
One-year-old girl with developmental dysplasia of the hip on the left side.
TREATMENT
The goal of treatment is to acquire and sustain a stable, concentrically reduced hip joint at an earliest possible age with minimal complications[4,30]. There is well-established correlation between residual dysplasia and age of reduction. Ideally, patients should be identified and treated in infancy. Failing this, treatment should be instituted as soon as possible, preferably before 4 years of age[4,74,76]. The goals of treatment in older children with persistent acetabular dysplasia are to delay or prevent the development of osteoarthritis and to obviate the need for arthroplasty at a relatively young age[74].
Subluxation of the hip joint noted near birth can be observed for 3 wk without any treatment, as it is commonly corrects spontaneously. The use of triple diapers is not recommended, as it has not shown better results compared to no treatment. After 3 wk, if there is still evidence of subluxation on physical and ultrasonographic examinations, initiation of treatment is recommended. When complete displacement of the hip joint is noted at birth, initiation of treatment without an observation period is recommended[1,5]. A recent Cochrane review showed that in infants who were identified clinically to have unstable but not dislocated hips, or were identified on ultrasounography to have mild hip dysplasia, postponing treatment by 2 to 8 wk reduces the need for treatment without a significant increase in late diagnosed dysplasia or surgery[63].
The Pavlik harness
This is the most commonly used device today to treat hip instability in infants[77]. Alternatives include the Craig splint and the Von Rosen splint. Although there are few comparative studies, all the three braces are superior to no treatment. The Craig and the Von Rosen splints might be slightly superior to the Pavlik harness[78], but the Pavlik harness remains the standard treatment for the majority of children younger than 6 mo as it is the most thoroughly examined, and found to be safe and highly effective, with success rates greater than 90%[79-83]. The function of the frontal leg straps is to flex the hips, and the rear leg straps to prevent adduction of the hips (extreme abduction of the hips should be avoided as this is related to AVN). The indication for its use is a reducible hip in an infant who is not yet trying to stand. Close follow-up is required, usually at weekly intervals. If the reduction of the hip joint is unsuccessful after 3 wk, other treatment modalities should be considered[1]. Continuation of the harness with the dislocated hip may potentiate acetabular dysplasia, which may increase the difficulty of subsequent closed reduction (“Pavlik harness disease”)[84,85]. Higher rates of AVN have also been reported[86-91].
A recent study examined the influence of different risk factors (age, gender, side, family history, breech presentation, first-born girl, oligohydramnios, swaddling, and the severity of hip dysplasia defined by ultrasonography) on the success rate of treatment with the Pavlik harness. Age was the only patient-related variable influencing the success rate of treatment. The authors concluded that Pavlik harness treatment is less effective in children at and over the age of 4 mo at the time the harness is first applied, as well as in hips with complete dislocations and hips with severely deficient acetabular bony roofs[92]. Another study examined the relationship between ultrasonographic findings and failure of treatment with Pavlik harness. Two static ultrasonographic findings linked with treatment outcome were described. A femoral head positioned below the labrum was strongly associated with success, whereas a femoral head located substantially superior and lateral to the labrum was associated with failure[93,94]. Bilateral DDH was not found to be a risk factor for Pavlik harness failure[95].
Femoral nerve palsy is a rare but clinically significant complication of Pavlik harness treatment. It usually appears on the involved side, around the end of first week of treatment, and resolves between several days and 2 wk. This complication was shown to be strongly predictive of failure of treatment, with correlation between the number of days until return of femoral nerve function and the probability of successful treatment with the Pavlik harness (prompt resolution was predictive of treatment success)[96].
A recent study from Switzerland reported results of treatment of infants 0-6 mo of age with an abduction brace instead of a Pavlik harness with results that are comparable to the reported results of treatment with a Pavlik harness. The use of an abduction brace is easier for the patients and the physician. However, this was a retrospective study with a small number of patients, and more research is needed to draw any firm conclusions[97].
The use of the Pavlik harness after the age of 6 mo is not recommended by most authors[92]. However, a recent retrospective study of the outcome of late-diagnosed DDH in infants who were treated with Pavlik harness beginning treatment at the age of 6-24 mo, showed encouraging results in the treatment of hip dislocation type Graf 3. Neither of the Graf 4 hips were successfully reduced[98]. Another study reported a successful treatment with Pavlik harness, in children aged 5 to 13 mo of age. The rate of successful reduction was higher with less severe dislocations[99]. Both of these studies used periods of treatment that were longer than the commonly accepted 3 wk. It is expected that the management of an older child with the Pavlik harness might be complicated because of parental compliance[100]. Additional study examined the results of modified Hoffmann-Daimler method of treatment, for children aged 6 to 44 mo of age with good results[101].
If the dysplastic hip treated by Pavlik harness is successfully reduced and free of contracture but still unstable, it should be treated with a fixed abduction orthosis[80,102,103]. Different abduction braces were reported to be successful, including Plastazote and Ilfeld abduction orthoses[104-106]. A part-time use of an abduction brace orthosis between the age of 6 to 12 mo is an effective intervention to improve residual acetabular dysplasia. The optimal duration of abduction bracing is still unclear[107].
Closed reduction and fixation with spica cast
Closed reduction of the hip joint performed under general anesthesia is indicated in patients who failed to achieve stable reduction with the Pavlik harness. It may also be considered as primary treatment for patients with poor social situation or an unreliable family. Better results were achieved when reduction was performed before the age of 6 mo[1,30]. The use of traction before attempted closed reduction is controversial. Although once very popular[108], there is now a trend toward decreasing the use of traction. Dynamic arthrography with fluoroscopy is useful to assess the quality of reduction, the extent of coverage of the femoral head and the optimal position for immobilization[4].
The “safe zone” is the range between maximal passive abduction of the hip and the angle of abduction where the femoral head becomes unstable. Adductor tenotomy (performed either open or percutaneously) can widen the safe zone by decreasing adduction contracture, thereby increasing abduction. Immobilization should not be done in a position of extreme hip abduction, as this is associated with AVN. After closed reduction, a spica cast is applied with the use of a greater trochanter mold, maintenance of 90-100 degrees of hip flexion and controlled abduction. Reduction is confirmed using a limited CT or MRI study[109,110]. A spica cast is utilized for 3 mo without changing, and then an abduction orthosis is used. Assessment of hip maturation is accomplished with serial radiographs. The majority of patients who had successful closed reduction after the age of 18 mo required an additional open procedure[4,111].
Gradual reduction using long-term traction techniques has been described as a mean of closed reduction. The reported reduction rates were high, with a low rate of AVN; however, many of these patients had residual acetabular dysplasia and required future acetabular osteotomy as a secondary procedure. These techniques require long traction periods and prolonged hospitalization, which may be difficult both for the children and the family[112-116].
Open reduction and hip reconstruction
Typically, open reduction is considered for children older than 18 mo. However, open reduction is indicated for all children who failed to achieve a stable concentric reduction of the hip joint by closed techniques.
Open reduction can be performed through different approaches. The inability to perform a pelvic osteotomy or capsulorrhaphy via the medial approach limits its use to patients less than 18 mo. Several modifications to this approach have been proposed. These medial approaches require minimal dissection, avoid splitting of the iliac apophysis, and allow direct access to the medial structures. However, they potentially endanger the blood supply to the femoral head and some authors noted an association between the medial approach and osteonecrosis[117-119]. Although not substantiated[120,121], this decreased the popularity of this approach. Newer, medial minimally invasive approaches for open reduction, such as the use of arthroscopy to release the psoas and to remove the ligamentum teres and the pulvinar are under development[122,123]. A modified posteromedial approach to the hip joint has been described as a limited surgical technique for patients up to 18 mo of age. The adductor longus and iliopsoas tendons are sectioned through the posteromedial incision. If concentric reduction is not achieved, hip arthrotomy is performed. Good results were reported with this new technique[124-126].
The modified Smith-Petersen anterolateral approach is very useful because it allows for a concomitant pelvic osteotomy, capsulorrhaphy and usually a shorter period in a spica. Therefore, it is usually the procedure of choice in children older than 18 mo[4,23,127].
Redislocation following open reduction is an important problem with a variable incidence. Frequently, the failure of a primary open reduction is due to errors in surgical technique, like insufficient release of the anteromedial capsule and the inferior articular structures. A common finding in a re-dislocated hip following open reduction is an intact transverse acetabular ligament which was not fully released at the initial procedure. The presence of a stump of the ligamentum teres causing redislocation has also been found. This stresses the importance of complete removal of all obstacles to reduction including the need for complete release of the transverse acetabular ligament[4,128-130]. Risk factors for failed open reduction were not thoroughly evaluated. A recent retrospective match-controlled study examined those risk factors which were: right side (or bilateral) involvement, greater pubic width, and decreased abduction in the spica cast. In several cases, dysplasia of the femoral head or an insufficiently corrected femoral version were thought to be the reason for the failure of the primary surgery[131].
Procedures are being developed in the effort to reduce the rate of redislocation. The transfer and tenodesis of the ligamentum teres has been described with good results. This procedure is done through a medial approach[132,133]. Another technique is the use of a percutaneous Kirschner wire (K-wire) to stabilize the hip after successful reduction. The result of this technique that can be performed with the common anterolateral approach is very encouraging. A reduced rate of redislocation was reported without an increase in complications such as AVN, premature closure of triradiate cartilage and septic arthritis[134,135].
Following open reduction a spica cast is used for 6 wk with immobilization in 30 degrees of abduction, flexion and internal rotation. After cast removal, physiotherapy is recommended[4].
Femoral osteotomy can facilitate reduction and decrease the rate of osteonecrosis by relieving tension in the hip joint. It allows the surgeon to perform shortening and to correct excessive femoral anteversion. Femoral shortening should be used whenever excessive force is needed for hip reduction. The amount of shortening is determined by the amount of overlap between the femoral segments after osteotomy with the hip reduced[4]. In a recent study open reduction without simultaneous femoral osteotomy strongly predicted the need for a secondary procedure, and the authors concluded there should be a low threshold to performing femoral osteotomy during a primary open reduction[136]. Although generally accepted that DDH is associated with increased femoral anteversion, some studies did not show a difference in anteversion compared with normal hips[137,138] while others did[139]. Therefore, the indications for femoral derotational osteotomy remain unclear. Earlier studies reported a common use of derotational osteotomy[140,141]; however, recent literature does not support this practice[142,143]. It should be noted that all these studies utilized a different system to measure femoral anteversion. A recent study showed that femoral anteversion is inconsistent in children with DDH and should be evaluated on a case-by-case basis to establish the necessity of derotational femoral osteotomy[144].
Pelvic osteotomy is indicated for persistence of acetabular dysplasia, when there is insufficiency in acetabular coverage. The need for an acetabular procedure at the time of open reduction in a 1.5-3-year-old child with acetabular dysplasia is controversial. One approach is to delay the acetabular procedure until the remodeling response of the acetabulum following open reduction is assessed. However, in recent years, there has been a tendency to include an acetabular procedure (single innominate osteotomy - Salter[145,146]) at the time of primary treatment to maximize the potential for the development of a normal acetabulum[74,147,148]. A recent study compared acetabular development after femoral varus derotational osteotomy and an innominate osteotomy, in patients 15 mo to 4 years of age. The authors concluded that acetabular remodeling after open hip reduction and innominate osteotomy was more effective for reversing acetabular dysplasia and maintaining hip stability than open reduction combined with a femoral varus derotation osteotomy[149]. A long term follow-up after patients who had been treated with innominate osteotomy showed a 54% rate of survival of the hip at 45 years[150].
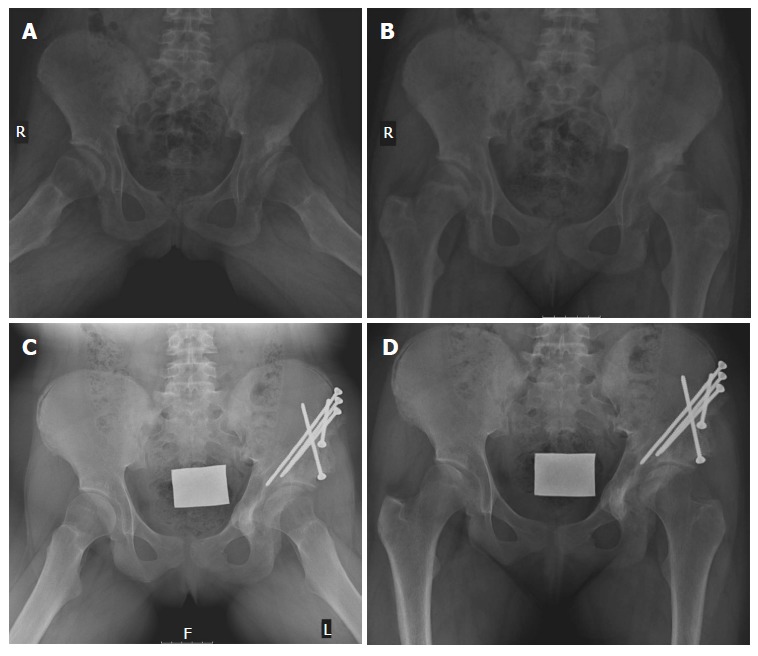
In the child older than 3 years, acetabular osteotomy is performed routinely because of the unpredictable remodeling potential of the acetabulum beyond this age. Femoral derotational osteotomy is also usually needed. For an acetabular procedure, either a Salter or Pemberton osteotomy may be performed (Figure 3). The primary indication for Salter osteotomy is a deficiency in anterolateral femoral head coverage in a concentrically reduced hip, while a shallow acetabulum is a relative contraindication. Placement of bone graft and internal fixation is needed. Best results were reported in patients aged 1.5-4 years. Pemberton osteotomy is an incomplete osteotomy that hinges through the triradiate cartilage (Figure 4). As this is an incomplete osteotomy, it is inherently stable and no internal fixation is required. A spica cast is used for 8 wk. This procedure is appropriate for patients older than 1.5 years and until skeletal maturity[74].
Figure 3.
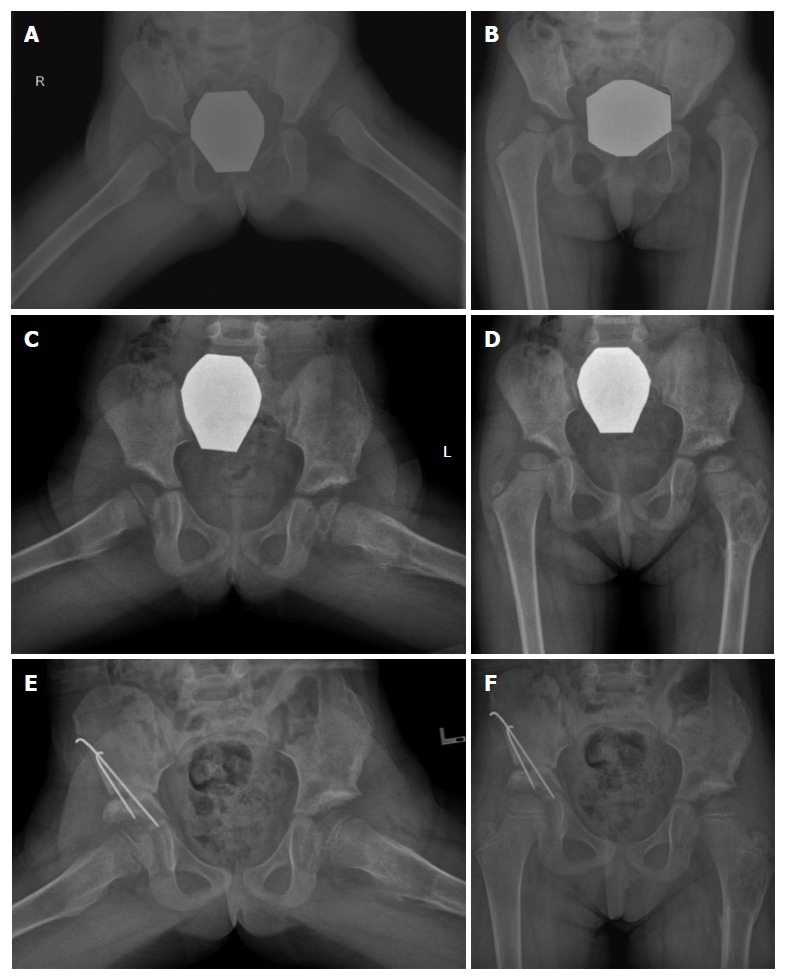
Hip reconstruction. A, B: Female patient, diagnosed with bilateral developmental dysplasia of the hip at the age of 2.5 years; C, D: On presentation left hip reconstruction, that included open reduction, Salter osteotomy and femoral derotational osteotomy with shortening, was performed. Post-operative X-rays after removal of the internal fixation devices are shown; E, F: Due to persistent mild hip dysplasia on the right side, a Salter osteotomy was performed at the age of 4 years.
Figure 4.
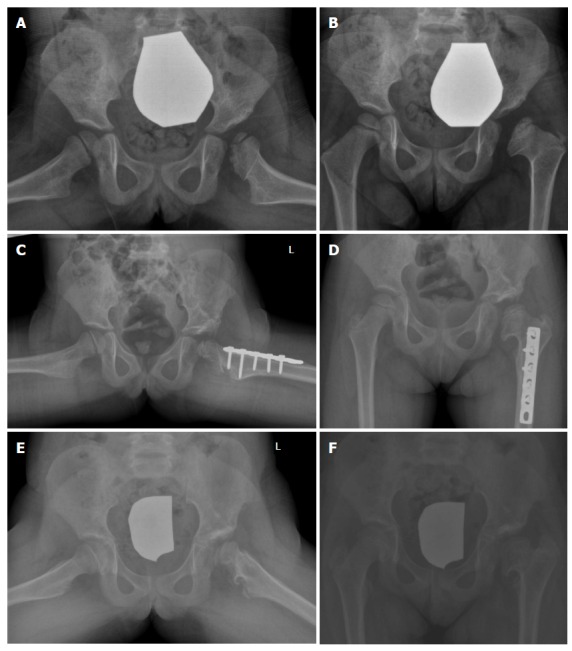
Acetabuloplasty. A female patient was diagnosed with DDH of the left hip at the age of 6 mo using sonography. She was treated with a spica cast. AVN of the left femoral head was seen on follow-up radiographs at the age of 3 years (A,B); C, D: Acetabuloplasty of the left hip with femoral derotational osteotomy was performed at the age of 5 years; E, F: Follow-up X-rays at the age of 8 years. DDH: Developmental dysplasia of the hip; AVN: Avascular necrosis.
A combination of Salter and Pemberton osteotomies, called the Pembersal procedure, was also reported. The main complication of this procedure is iatrogenic damage to the triradiate cartilage. The reported results of this operation are satisfactory; however, whether this procedure provides any advantages remains unclear[151,152].
In the older child or adolescent, if the triradiate cartilage remains open, the triple innominate osteotomy is the procedure of choice. After triradiate cartilage closure, Ganz periacetabular osteotomy, triple innominate osteotomy or a salvage osteotomy (such as Chiari or shelf procedure) should be considered. In triple innominate osteotomy described by Steel[153], concentric hip reduction is a prerequisite. It allows significant mobility of the acetabular fragment and its displacement medially, moving the hip center medially and improving gait mechanics. Placement of a bone graft and internal fixation are required[154]. A modified triple osteotomy was proposed with better preliminary results[155,156]. An endoscopic method of performing triple innominate osteotomy has also been developed; although technically demanding, preliminary studies demonstrate good results with reduced surgical morbidity[157]. Ganz periacetabular osteotomy is indicated only after skeletal maturity as it crosses the triradiate cartilage (Figure 5). This procedure is very stable and immediate crutch weight-bearing is allowed. However the procedure is difficult to learn[74]. Long-term results of the correction of acetabular dysplasia with periacetabular osteotomies have been published. The end point of these studies was conversion to arthroplasty. The preoperative grade of arthritis was a consistent risk factor for failure. There are now consistent data demonstrating the efficacy of pelvic osteotomy for the treatment of symptomatic acetabular dysplasia[158-161].
Figure 5.
Female patient with developmental dysplasia of the hip that was diagnosed in early adolescence. A, B: X-rays at the time of diagnosis of DDH at the age of 13 years; C, D: X-rays taken two years after Ganz osteotomy on the left side. DDH: Developmental dysplasia of the hip.
Salvage procedures are indicated when congruent reduction between the femoral head and the acetabulum cannot be obtained. These procedures increase the weight bearing surface and rely on capsular metaplasia to provide an articulating surface. Usually concomitant femoral varus or valgus osteotomy is performed. A Chiari procedure can be performed on a patient older than 8 years if there is satisfactory range of motion, maintenance of cartilage space and minimal osteoarthritis, with good results[162,163]. Shelf procedures are performed to increase the extra-articular buttress, thereby increasing the load-bearing area of the hip. They are indicated when congruent reduction is impossible, when there is no severe osteoarthritis and when augmentation is needed after other osteotomies. The slotted-shelf procedure is recommended over the other types because of the greater resultant stability[74,164].
FOLLOW-UP
Most orthopedic surgeons agree that children with a history of DDH should be followed until skeletal maturity[1,6]. However, some studies raise doubt regarding the necessity of radiographic monitoring[165-167], while others stress its significance[17,48,168]. The incidence of residual acetabular dysplasia after successful treatment with Pavlik harness cannot be disregarded[79,169,170]. Concern has been raised about the late effects of radiation due to the long life expectancy of the patients[171,172]. A recent retrospective study established the incidence of radiographic acetabular dysplasia in children with previous DDH normalization to be 17% and 33% around the ages 6 and 12 mo, respectively. Based on this data, the authors concluded that infants who normalize after treatment with Pavlik harness or spontaneously can benefit from a single-view AP radiograph of the pelvis at the age 6 and 12 mo. Follow-up at these particular ages can allow early intervention. The need for long-term radiographic follow-up after 12 mo of age cannot be inferred from this study[173]. A group from the United Kingdom reported a 4% recurrent dysplasia that required intervention after treatment of DDH to ultrasonographic normality. They recommended long-term follow-up of dysplastic hips with an early pelvic X-ray at around 6 mo[174]. Another study evaluated children with unilateral hip dysplasia for a contralateral hip dysplasia that was not apparent with thorough and recurring evaluations early in childhood. The authors showed that mild dysplasia of the hip can develop as the child grows older[175]. This emphasizes the significance of thorough and recurring clinical and radiographic examinations.
CONCLUSION
The main changes in the field of DDH during the last 20 years are summarized in Figure 6.
Figure 6.
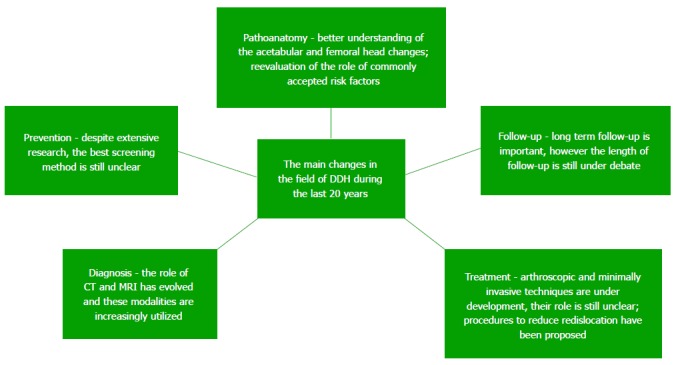
Summary of the main changes in the field of developmental dysplasia of the hip during the last 20 years. MRI: Magnetic resonance imaging; DDH: Developmental dysplasia of the hip; CT: Computed tomography.
The normal development of the child’s hip relies on congruent stability of the femoral head within the acetabulum. Early diagnosis and treatment of DDH is critical to provide the best possible functional outcome. The acetabular changes in DDH are well recognized. Recently we also gained understanding into the changes of the femoral head. The traditional risk factors for DDH were questioned and new ones were explored, and consequently we have a better understanding of the factors that are associated with this condition. The best example is probably the change that was made in some cultures, from traditional swaddling, with the lower extremities fully extended and wrapped together, to safe swaddling, with the infant hips positioned in slight flexion, leading to reduced incidence of DDH. In the future, genetic research may give us better understanding on the molecular mechanisms that lead to this condition. There is still much clinical research to be done in order to convert all of our knowledge into clinical practice.
As early diagnosis and treatment is critical in order to achieve best functional outcome, there is much interest in the search for the best screening program. Despite best efforts many young adults with dysplasia are not detected at birth. Although ultrasonography is the technique of choice for visualization of acetabular changes in children up to 4 mo of age, its role in the screening of DDH in newborns is still controversial. The recommended length of follow-up for at risk infants is also undefined. We recommend performing ultrasonographic screening to all newborns with risk factors at 4 to 6 wk of age, followed by ultrasonographic monitoring until age one year. We also recommend radiographic follow-up of all children treated because of dysplasia of the hip until at least 3 years of age.
Imaging and its role in the screening, follow-up and treatment of DDH is rapidly evolving. The role of ultrasonography was established as the best imaging modality for screening and follow up of infants suspected for DDH up to the age when the proximal ossific nucleus appears. Radiographs are used in order to rule out other conditions and for evaluation and follow up of older patients. CT is increasingly used especially for evaluation of dysplasia in older patients. Protocols using less radiation are developed. MRI is gaining popularity due to the fact that no radiation is involved and as it has the ability to show better soft tissue anatomy than any other imaging modality. Shorter imaging protocols were developed. Contrast enhanced MRI might also be of use in the future to assess perfusion of the femoral head after reduction and fixation.
Much research has been done in order to compare different treatment protocols and surgical procedures. The Pavlik harness still remains the main treatment for the younger infant. Patients that failed to achieve stable fixation with the Pavlik harness need closed reduction and spica casting. The introduction of the “safe zone” concept has reduced the AVN rates associated with this treatment.
Patients who fail after closed treatment need an open reduction. Patients older than 18 mo of age usually require hip reconstruction during open reduction. A vast amount of research has been performed comparing different surgical approaches and different procedures in the search for the best treatment protocol based on deformity and patient age. New procedures are being proposed and developed, such as minimally invasive and arthroscopic surgery. Some common features that led to failure of primary surgery were identified and the role of femoral shortening and derotational femoral osteotomy has been assessed. Despite substantial research, high quality comparative studies are lacking and the treatment of an older child with DDH is mainly based on the clinical experience of the treating surgeon.
Footnotes
Conflict-of-interest statement: None of the authors has any conflict of interest.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: July 1, 2015
First decision: August 4, 2015
Article in press: October 13, 2015
P- Reviewer: Malik H, Pamidi N S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
References
- 1.Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg. 2000;8:232–242. doi: 10.5435/00124635-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Klisic PJ. Congenital dislocation of the hip--a misleading term: brief report. J Bone Joint Surg Br. 1989;71:136. doi: 10.1302/0301-620X.71B1.2914985. [DOI] [PubMed] [Google Scholar]
- 3.Aronsson DD, Goldberg MJ, Kling TF, Roy DR. Developmental dysplasia of the hip. Pediatrics. 1994;94:201–208. [PubMed] [Google Scholar]
- 4.Vitale MG, Skaggs DL. Developmental dysplasia of the hip from six months to four years of age. J Am Acad Orthop Surg. 2001;9:401–411. doi: 10.5435/00124635-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics. Clinical practice guideline: early detection of developmental dysplasia of the hip. Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip. American Academy of Pediatrics. Pediatrics. 2000;105:896–905. doi: 10.1542/peds.105.4.896. [DOI] [PubMed] [Google Scholar]
- 6.Schwend RM, Shaw BA, Segal LS. Evaluation and treatment of developmental hip dysplasia in the newborn and infant. Pediatr Clin North Am. 2014;61:1095–1107. doi: 10.1016/j.pcl.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Bialik V, Bialik GM, Blazer S, Sujov P, Wiener F, Berant M. Developmental dysplasia of the hip: a new approach to incidence. Pediatrics. 1999;103:93–99. doi: 10.1542/peds.103.1.93. [DOI] [PubMed] [Google Scholar]
- 8.Yamamuro T, Ishida K. Recent advances in the prevention, early diagnosis, and treatment of congenital dislocation of the hip in Japan. Clin Orthop Relat Res. 1984;184:34–40. [PubMed] [Google Scholar]
- 9.Kutlu A, Memik R, Mutlu M, Kutlu R, Arslan A. Congenital dislocation of the hip and its relation to swaddling used in Turkey. J Pediatr Orthop. 1992;12:598–602. [PubMed] [Google Scholar]
- 10.van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, Kuis W, Schulpen TW, L’Hoir MP. Swaddling: a systematic review. Pediatrics. 2007;120:e1097–e1106. doi: 10.1542/peds.2006-2083. [DOI] [PubMed] [Google Scholar]
- 11.Mahan ST, Kasser JR. Does swaddling influence developmental dysplasia of the hip? Pediatrics. 2008;121:177–178. doi: 10.1542/peds.2007-1618. [DOI] [PubMed] [Google Scholar]
- 12.Wang E, Liu T, Li J, Edmonds EW, Zhao Q, Zhang L, Zhao X, Wang K. Does swaddling influence developmental dysplasia of the hip?: An experimental study of the traditional straight-leg swaddling model in neonatal rats. J Bone Joint Surg Am. 2012;94:1071–1077. doi: 10.2106/JBJS.K.00720. [DOI] [PubMed] [Google Scholar]
- 13.International Hip Dysplasia Institute. [Online resources] Available from: http: // hipdysplasia.org.
- 14.American Academy of Orthopaedic Surgeons. [Online resources] Available from: http: //orthoinfo.aaos.org/main.cfm.
- 15.Pediatric Orthopaedic Society of North America. [Online resources] Available from: http: //posna.org/
- 16.Bache CE, Clegg J, Herron M. Risk factors for developmental dysplasia of the hip: ultrasonographic findings in the neonatal period. J Pediatr Orthop B. 2002;11:212–218. doi: 10.1097/00009957-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Imrie M, Scott V, Stearns P, Bastrom T, Mubarak SJ. Is ultrasound screening for DDH in babies born breech sufficient? J Child Orthop. 2010;4:3–8. doi: 10.1007/s11832-009-0217-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stevenson DA, Mineau G, Kerber RA, Viskochil DH, Schaefer C, Roach JW. Familial predisposition to developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:463–466. doi: 10.1097/BPO.0b013e3181aa586b. [DOI] [PubMed] [Google Scholar]
- 19.Orak MM, Onay T, Gümüştaş SA, Gürsoy T, Muratlí HH. Is prematurity a risk factor for developmental dysplasia of the hip? : a prospective study. Bone Joint J. 2015;97-B:716–720. doi: 10.1302/0301-620X.97B5.34010. [DOI] [PubMed] [Google Scholar]
- 20.Barlow TG. Early diagnosis and treatment of congenital dislocation of the hip. J Bone Joint Surg Br. 1962;44:292–301. [Google Scholar]
- 21.Sankar WN, Neubuerger CO, Moseley CF. Femoral head sphericity in untreated developmental dislocation of the hip. J Pediatr Orthop. 2010;30:558–561. doi: 10.1097/BPO.0b013e3181e4f53e. [DOI] [PubMed] [Google Scholar]
- 22.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790. doi: 10.1007/s11999-008-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas SR. A review of long-term outcomes for late presenting developmental hip dysplasia. Bone Joint J. 2015;97-B:729–733. doi: 10.1302/0301-620X.97B6.35395. [DOI] [PubMed] [Google Scholar]
- 24.Wedge JH, Wasylenko MJ. The natural history of congenital disease of the hip. J Bone Joint Surg Br. 1979;61-B:334–338. doi: 10.1302/0301-620X.61B3.158025. [DOI] [PubMed] [Google Scholar]
- 25.Wedge JH, Wasylenko MJ. The natural history of congenital dislocation of the hip: a critical review. Clin Orthop Relat Res. 1978;137:154–162. [PubMed] [Google Scholar]
- 26.Lai KA, Lin CJ, Su FC. Gait analysis of adult patients with complete congenital dislocation of the hip. J Formos Med Assoc. 1997;96:740–744. [PubMed] [Google Scholar]
- 27.Vallamshetla VR, Mughal E, O’Hara JN. Congenital dislocation of the hip. A re-appraisal of the upper age limit for treatment. J Bone Joint Surg Br. 2006;88:1076–1081. doi: 10.1302/0301-620X.88B8.17592. [DOI] [PubMed] [Google Scholar]
- 28.Ryan MG, Johnson LO, Quanbeck DS, Minkowitz B. One-stage treatment of congenital dislocation of the hip in children three to ten years old. Functional and radiographic results. J Bone Joint Surg Am. 1998;80:336–344. doi: 10.2106/00004623-199803000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Wang TM, Wu KW, Shih SF, Huang SC, Kuo KN. Outcomes of open reduction for developmental dysplasia of the hip: does bilateral dysplasia have a poorer outcome? J Bone Joint Surg Am. 2013;95:1081–1086. doi: 10.2106/JBJS.K.01324. [DOI] [PubMed] [Google Scholar]
- 30.Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am. 1994;76:1777–1792. doi: 10.2106/00004623-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Luhmann SJ, Schoenecker PL, Anderson AM, Bassett GS. The prognostic importance of the ossific nucleus in the treatment of congenital dysplasia of the hip. J Bone Joint Surg Am. 1998;80:1719–1727. doi: 10.2106/00004623-199812000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Roposch A, Stöhr KK, Dobson M. The effect of the femoral head ossific nucleus in the treatment of developmental dysplasia of the hip. A meta-analysis. J Bone Joint Surg Am. 2009;91:911–918. doi: 10.2106/JBJS.H.00096. [DOI] [PubMed] [Google Scholar]
- 33.Roposch A, Liu LQ, Offiah AC, Wedge JH. Functional outcomes in children with osteonecrosis secondary to treatment of developmental dysplasia of the hip. J Bone Joint Surg Am. 2011;93:e145. doi: 10.2106/JBJS.J.01623. [DOI] [PubMed] [Google Scholar]
- 34.Patel H. Preventive health care, 2001 update: screening and management of developmental dysplasia of the hip in newborns. CMAJ. 2001;164:1669–1677. [PMC free article] [PubMed] [Google Scholar]
- 35.Shipman SA, Helfand M, Moyer VA, Yawn BP. Screening for developmental dysplasia of the hip: a systematic literature review for the US Preventive Services Task Force. Pediatrics. 2006;117:e557–e576. doi: 10.1542/peds.2005-1597. [DOI] [PubMed] [Google Scholar]
- 36.Mahan ST, Katz JN, Kim YJ. To screen or not to screen? A decision analysis of the utility of screening for developmental dysplasia of the hip. J Bone Joint Surg Am. 2009;91:1705–1719. doi: 10.2106/JBJS.H.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Engesaeter IØ, Lie SA, Lehmann TG, Furnes O, Vollset SE, Engesaeter LB. Neonatal hip instability and risk of total hip replacement in young adulthood: follow-up of 2,218,596 newborns from the Medical Birth Registry of Norway in the Norwegian Arthroplasty Register. Acta Orthop. 2008;79:321–326. doi: 10.1080/17453670710015201. [DOI] [PubMed] [Google Scholar]
- 38.Dai J, Shi D, Zhu P, Qin J, Ni H, Xu Y, Yao C, Zhu L, Zhu H, Zhao B, et al. Association of a single nucleotide polymorphism in growth differentiate factor 5 with congenital dysplasia of the hip: a case-control study. Arthritis Res Ther. 2008;10:R126. doi: 10.1186/ar2540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenberg N, Bialik V, Norman D, Blazer S. The importance of combined clinical and sonographic examination of instability of the neonatal hip. Int Orthop. 1998;22:185–188. doi: 10.1007/s002640050238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lipton GE, Guille JT, Altiok H, Bowen JR, Harcke HT. A reappraisal of the Ortolani examination in children with developmental dysplasia of the hip. J Pediatr Orthop. 2007;27:27–31. doi: 10.1097/BPO.0b013e31802b70e5. [DOI] [PubMed] [Google Scholar]
- 41.Bond CD, Hennrikus WL, DellaMaggiore ED. Prospective evaluation of newborn soft-tissue hip “clicks” with ultrasound. J Pediatr Orthop. 1997;17:199–201. doi: 10.1097/00004694-199703000-00011. [DOI] [PubMed] [Google Scholar]
- 42.Choudry Q, Goyal R, Paton RW. Is limitation of hip abduction a useful clinical sign in the diagnosis of developmental dysplasia of the hip? Arch Dis Child. 2013;98:862–866. doi: 10.1136/archdischild-2012-303121. [DOI] [PubMed] [Google Scholar]
- 43.Kamath SU, Bennet GC. Does developmental dysplasia of the hip cause a delay in walking? J Pediatr Orthop. 2004;24:265. doi: 10.1097/00004694-200405000-00005. [DOI] [PubMed] [Google Scholar]
- 44.De Pellegrin M. Ultrasound screening for congenital dislocation of the hip. Results and correlations between clinical and ultrasound findings. Ital J Orthop Traumatol. 1991;17:547–553. [PubMed] [Google Scholar]
- 45.Bialik V, Wiener F, Benderly A. Ultrasonography and screening in developmental displacement of the hip. J Pediatr Orthop B. 1992;1:51–54. [Google Scholar]
- 46.Castelein RM, Sauter AJ. Ultrasound screening for congenital dysplasia of the hip in newborns: its value. J Pediatr Orthop. 1988;8:666–670. doi: 10.1097/01241398-198811000-00007. [DOI] [PubMed] [Google Scholar]
- 47.Clarke NM, Harcke HT, McHugh P, Lee MS, Borns PF, MacEwen GD. Real-time ultrasound in the diagnosis of congenital dislocation and dysplasia of the hip. J Bone Joint Surg Br. 1985;67:406–412. doi: 10.1302/0301-620X.67B3.3889008. [DOI] [PubMed] [Google Scholar]
- 48.Garvey M, Donoghue VB, Gorman WA, O’Brien N, Murphy JF. Radiographic screening at four months of infants at risk for congenital hip dislocation. J Bone Joint Surg Br. 1992;74:704–707. doi: 10.1302/0301-620X.74B5.1527117. [DOI] [PubMed] [Google Scholar]
- 49.Terjesen T. Ultrasound as the primary imaging method in the diagnosis of hip dysplasia in children aged < 2 years. J Pediatr Orthop B. 1996;5:123–128. doi: 10.1097/01202412-199605020-00013. [DOI] [PubMed] [Google Scholar]
- 50.Vedantam R, Bell MJ. Dynamic ultrasound assessment for monitoring of treatment of congenital dislocation of the hip. J Pediatr Orthop. 1995;15:725–728. doi: 10.1097/01241398-199511000-00002. [DOI] [PubMed] [Google Scholar]
- 51.Stanton RP, Capecci R. Computed tomography for early evaluation of developmental dysplasia of the hip. J Pediatr Orthop. 1992;12:727–730. doi: 10.1097/01241398-199211000-00005. [DOI] [PubMed] [Google Scholar]
- 52.Grissom L, Harcke HT, Thacker M. Imaging in the surgical management of developmental dislocation of the hip. Clin Orthop Relat Res. 2008;466:791–801. doi: 10.1007/s11999-008-0161-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gould SW, Grissom LE, Niedzielski A, Kecskemethy HH, Bowen JR, Harcke HT. Protocol for MRI of the hips after spica cast placement. J Pediatr Orthop. 2012;32:504–509. doi: 10.1097/BPO.0b013e31825a23e4. [DOI] [PubMed] [Google Scholar]
- 54.Tiderius C, Jaramillo D, Connolly S, Griffey M, Rodriguez DP, Kasser JR, Millis MB, Zurakowski D, Kim YJ. Post-closed reduction perfusion magnetic resonance imaging as a predictor of avascular necrosis in developmental hip dysplasia: a preliminary report. J Pediatr Orthop. 2009;29:14–20. doi: 10.1097/BPO.0b013e3181926c40. [DOI] [PubMed] [Google Scholar]
- 55.Gornitzky AL, Georgiadis AG, Seeley MA, Horn BD, Sankar WN. Does Perfusion MRI After Closed Reduction of Developmental Dysplasia of the Hip Reduce the Incidence of Avascular Necrosis? Clin Orthop Relat Res. 2015:Epub ahead of print. doi: 10.1007/s11999-015-4387-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.American Institute of Ultrasound in Medicine; American College of Radiology. AIUM practice guideline for the performance of an ultrasound examination for detection and assessment of developmental dysplasia of the hip. J Ultrasound Med. 2009;28:114–119. doi: 10.7863/jum.2009.28.1.114. [DOI] [PubMed] [Google Scholar]
- 57.Marks DS, Clegg J, al-Chalabi AN. Routine ultrasound screening for neonatal hip instability. Can it abolish late-presenting congenital dislocation of the hip? J Bone Joint Surg Br. 1994;76:534–538. [PubMed] [Google Scholar]
- 58.Castelein RM, Sauter AJ, de Vlieger M, van Linge B. Natural history of ultrasound hip abnormalities in clinically normal newborns. J Pediatr Orthop. 1992;12:423–427. doi: 10.1097/01241398-199207000-00001. [DOI] [PubMed] [Google Scholar]
- 59.Rosendahl K, Markestad T, Lie RT. Ultrasound screening for developmental dysplasia of the hip in the neonate: the effect on treatment rate and prevalence of late cases. Pediatrics. 1994;94:47–52. [PubMed] [Google Scholar]
- 60.Bialik V, Bialik GM, Wiener F. Prevention of overtreatment of neonatal hip dysplasia by the use of ultrasonography. J Pediatr Orthop B. 1998;7:39–42. doi: 10.1097/01202412-199801000-00007. [DOI] [PubMed] [Google Scholar]
- 61.Sink EL, Ricciardi BF, Torre KD, Price CT. Selective ultrasound screening is inadequate to identify patients who present with symptomatic adult acetabular dysplasia. J Child Orthop. 2014;8:451–455. doi: 10.1007/s11832-014-0620-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Laborie LB, Engesæter IØ, Lehmann TG, Eastwood DM, Engesæter LB, Rosendahl K. Screening strategies for hip dysplasia: long-term outcome of a randomized controlled trial. Pediatrics. 2013;132:492–501. doi: 10.1542/peds.2013-0911. [DOI] [PubMed] [Google Scholar]
- 63.Shorter D, Hong T, Osborn DA. Cochrane Review: Screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health. 2013;8:11–54. doi: 10.1002/ebch.1891. [DOI] [PubMed] [Google Scholar]
- 64.Elbourne D, Dezateux C, Arthur R, Clarke NM, Gray A, King A, Quinn A, Gardner F, Russell G. Ultrasonography in the diagnosis and management of developmental hip dysplasia (UK Hip Trial): clinical and economic results of a multicentre randomised controlled trial. Lancet. 2002;360:2009–2017. doi: 10.1016/s0140-6736(02)12024-1. [DOI] [PubMed] [Google Scholar]
- 65.Mulpuri K, Song KM. AAOS Clinical Practice Guideline: Detection and Nonoperative Management of Pediatric Developmental Dysplasia of the Hip in Infants up to Six Months of Age. J Am Acad Orthop Surg. 2015;23:206–207. doi: 10.5435/JAAOS-D-15-00008. [DOI] [PubMed] [Google Scholar]
- 66.Vane AG, Gwynne Jones DP, Dunbar JD, Theis JC. The diagnosis and management of neonatal hip instability: results of a clinical and targeted ultrasound screening program. J Pediatr Orthop. 2005;25:292–295. doi: 10.1097/01.bpo.0000152944.02864.d4. [DOI] [PubMed] [Google Scholar]
- 67.Paton RW, Hinduja K, Thomas CD. The significance of at-risk factors in ultrasound surveillance of developmental dysplasia of the hip. A ten-year prospective study. J Bone Joint Surg Br. 2005;87:1264–1266. doi: 10.1302/0301-620X.87B9.16565. [DOI] [PubMed] [Google Scholar]
- 68.Rosendahl K, Dezateux C, Fosse KR, Aase H, Aukland SM, Reigstad H, Alsaker T, Moster D, Lie RT, Markestad T. Immediate treatment versus sonographic surveillance for mild hip dysplasia in newborns. Pediatrics. 2010;125:e9–16. doi: 10.1542/peds.2009-0357. [DOI] [PubMed] [Google Scholar]
- 69.Omeroğlu H. Use of ultrasonography in developmental dysplasia of the hip. J Child Orthop. 2014;8:105–113. doi: 10.1007/s11832-014-0561-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Falliner A, Schwinzer D, Hahne HJ, Hedderich J, Hassenpflug J. Comparing ultrasound measurements of neonatal hips using the methods of Graf and Terjesen. J Bone Joint Surg Br. 2006;88:104–106. doi: 10.1302/0301-620X.88B1.16419. [DOI] [PubMed] [Google Scholar]
- 71.Czubak J, Kotwicki T, Ponitek T, Skrzypek H. Ultrasound measurements of the newborn hip. Comparison of two methods in 657 newborns. Acta Orthop Scand. 1998;69:21–24. doi: 10.3109/17453679809002349. [DOI] [PubMed] [Google Scholar]
- 72.Diaz A, Cuervo M, Epeldegui T. Simultaneous ultrasound studies of developmental dysplasia of the hip using the Graf, Harcke, and Suzuki approaches. J Pediatr Orthop B. 1994;3:185–189. [Google Scholar]
- 73.Mladenov K, Dora C, Wicart P, Seringe R. Natural history of hips with borderline acetabular index and acetabular dysplasia in infants. J Pediatr Orthop. 2002;22:607–612. [PubMed] [Google Scholar]
- 74.Gillingham BL, Sanchez AA, Wenger DR. Pelvic osteotomies for the treatment of hip dysplasia in children and young adults. J Am Acad Orthop Surg. 1999;7:325–337. doi: 10.5435/00124635-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 75.Scoles PV, Boyd A, Jones PK. Roentgenographic parameters of the normal infant hip. J Pediatr Orthop. 1987;7:656–663. [PubMed] [Google Scholar]
- 76.Holman J, Carroll KL, Murray KA, Macleod LM, Roach JW. Long-term follow-up of open reduction surgery for developmental dislocation of the hip. J Pediatr Orthop. 2012;32:121–124. doi: 10.1097/BPO.0b013e3182471aad. [DOI] [PubMed] [Google Scholar]
- 77.Mubarak SJ, Bialik V. Pavlik: the man and his method. J Pediatr Orthop. 2003;23:342–346. [PubMed] [Google Scholar]
- 78.Wilkinson AG, Sherlock DA, Murray GD. The efficacy of the Pavlik harness, the Craig splint and the von Rosen splint in the management of neonatal dysplasia of the hip. A comparative study. J Bone Joint Surg Br. 2002;84:716–719. doi: 10.1302/0301-620x.84b5.12571. [DOI] [PubMed] [Google Scholar]
- 79.Cashman JP, Round J, Taylor G, Clarke NM. The natural history of developmental dysplasia of the hip after early supervised treatment in the Pavlik harness. A prospective, longitudinal follow-up. J Bone Joint Surg Br. 2002;84:418–425. doi: 10.1302/0301-620x.84b3.12230. [DOI] [PubMed] [Google Scholar]
- 80.Fabry G. Clinical practice: the hip from birth to adolescence. Eur J Pediatr. 2010;169:143–148. doi: 10.1007/s00431-009-1025-x. [DOI] [PubMed] [Google Scholar]
- 81.Kokavec M, Makai F, Olos M, Bialik V. Pavlik’s method: a retrospective study. Arch Orthop Trauma Surg. 2006;126:73–76. doi: 10.1007/s00402-005-0086-1. [DOI] [PubMed] [Google Scholar]
- 82.Peled E, Bialik V, Katzman A, Eidelman M, Norman D. Treatment of Graf’s ultrasound class III and IV hips using Pavlik’s method. Clin Orthop Relat Res. 2008;466:825–829. doi: 10.1007/s11999-008-0119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Grill F, Bensahel H, Canadell J, Dungl P, Matasovic T, Vizkelety T. The Pavlik harness in the treatment of congenital dislocating hip: report on a multicenter study of the European Paediatric Orthopaedic Society. J Pediatr Orthop. 1988;8:1–8. doi: 10.1097/01241398-198801000-00001. [DOI] [PubMed] [Google Scholar]
- 84.Jones GT, Schoenecker PL, Dias LS. Developmental hip dysplasia potentiated by inappropriate use of the Pavlik harness. J Pediatr Orthop. 1992;12:722–726. doi: 10.1097/01241398-199211000-00004. [DOI] [PubMed] [Google Scholar]
- 85.Kitoh H, Kawasumi M, Ishiguro N. Predictive factors for unsuccessful treatment of developmental dysplasia of the hip by the Pavlik harness. J Pediatr Orthop. 2009;29:552–557. doi: 10.1097/BPO.0b013e3181b2f200. [DOI] [PubMed] [Google Scholar]
- 86.Senaran H, Bowen JR, Harcke HT. Avascular necrosis rate in early reduction after failed Pavlik harness treatment of developmental dysplasia of the hip. J Pediatr Orthop. 2007;27:192–197. doi: 10.1097/01.bpb.0000248567.49089.f0. [DOI] [PubMed] [Google Scholar]
- 87.Suzuki S, Yamamuro T. Avascular necrosis in patients treated with the Pavlik harness for congenital dislocation of the hip. J Bone Joint Surg Am. 1990;72:1048–1055. [PubMed] [Google Scholar]
- 88.Inoue T, Naito M, Nomiyama H. Treatment of developmental dysplasia of the hip with the Pavlik harness: factors for predicting unsuccessful reduction. J Pediatr Orthop B. 2001;10:186–191. [PubMed] [Google Scholar]
- 89.Fujioka F, Terayama K, Sugimoto N, Tanikawa H. Long-term results of congenital dislocation of the hip treated with the Pavlik harness. J Pediatr Orthop. 1995;15:747–752. doi: 10.1097/01241398-199511000-00006. [DOI] [PubMed] [Google Scholar]
- 90.Segal LS, Boal DK, Borthwick L, Clark MW, Localio AR, Schwentker EP. Avascular necrosis after treatment of DDH: the protective influence of the ossific nucleus. J Pediatr Orthop. 1999;19:177–184. doi: 10.1097/00004694-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 91.Tiruveedhula M, Reading IC, Clarke NM. Failed Pavlik harness treatment for DDH as a risk factor for avascular necrosis. J Pediatr Orthop. 2015;35:140–143. doi: 10.1097/BPO.0000000000000236. [DOI] [PubMed] [Google Scholar]
- 92.Ömeroğlu H, Köse N, Akceylan A. Success of Pavlik Harness Treatment Decreases in Patients ≥ 4 Months and in Ultrasonographically Dislocated Hips in Developmental Dysplasia of the Hip. Clin Orthop Relat Res. 2015:Epub ahead of print. doi: 10.1007/s11999-015-4388-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zaltz I, Hosalkar H, Wenger D. What’s new in pediatric orthopaedic surgery. J Bone Joint Surg Am. 2012;94:375–381. doi: 10.2106/JBJS.K.01370. [DOI] [PubMed] [Google Scholar]
- 94.White KK, Sucato DJ, Agrawal S, Browne R. Ultrasonographic findings in hips with a positive Ortolani sign and their relationship to Pavlik harness failure. J Bone Joint Surg Am. 2010;92:113–120. doi: 10.2106/JBJS.H.01880. [DOI] [PubMed] [Google Scholar]
- 95.Borowski A, Thawrani D, Grissom L, Littleton AG, Thacker MM. Bilaterally dislocated hips treated with the Pavlik harness are not at a higher risk for failure. J Pediatr Orthop. 2009;29:661–665. doi: 10.1097/BPO.0b013e3181b528f8. [DOI] [PubMed] [Google Scholar]
- 96.Murnaghan ML, Browne RH, Sucato DJ, Birch J. Femoral nerve palsy in Pavlik harness treatment for developmental dysplasia of the hip. J Bone Joint Surg Am. 2011;93:493–499. doi: 10.2106/JBJS.J.01210. [DOI] [PubMed] [Google Scholar]
- 97.Wahlen R, Zambelli PY. Treatment of the Developmental Dysplasia of the Hip with an Abduction Brace in Children up to 6 Months Old. Adv Orthop. 2015;2015:103580. doi: 10.1155/2015/103580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pollet V, Pruijs H, Sakkers R, Castelein R. Results of Pavlik harness treatment in children with dislocated hips between the age of six and twenty-four months. J Pediatr Orthop. 2010;30:437–442. doi: 10.1097/BPO.0b013e3181df85ab. [DOI] [PubMed] [Google Scholar]
- 99.van de Sande MA, Melisie F. Successful Pavlik treatment in late-diagnosed developmental dysplasia of the hip. Int Orthop. 2012;36:1661–1668. doi: 10.1007/s00264-012-1587-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hosalkar HS, Pandya NK, Wenger DR. What’s new in pediatric orthopaedics. J Bone Joint Surg Am. 2013;95:377–383. doi: 10.2106/JBJS.L.01375. [DOI] [PubMed] [Google Scholar]
- 101.Papadimitriou NG, Papadimitriou A, Christophorides JE, Beslikas TA, Panagopoulos PK. Late-presenting developmental dysplasia of the hip treated with the modified Hoffmann-Daimler functional method. J Bone Joint Surg Am. 2007;89:1258–1268. doi: 10.2106/JBJS.E.01414. [DOI] [PubMed] [Google Scholar]
- 102.Hedequist D, Kasser J, Emans J. Use of an abduction brace for developmental dysplasia of the hip after failure of Pavlik harness use. J Pediatr Orthop. 2002;23:175–177. [PubMed] [Google Scholar]
- 103.Noordin S, Umer M, Hafeez K, Nawaz H. Developmental dysplasia of the hip. Orthop Rev (Pavia) 2010;2:e19. doi: 10.4081/or.2010.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Swaroop VT, Mubarak SJ. Difficult-to-treat Ortolani-positive hip: improved success with new treatment protocol. J Pediatr Orthop. 2009;29:224–230. doi: 10.1097/BPO.0b013e31819bcecf. [DOI] [PubMed] [Google Scholar]
- 105.Eberle CF. Plastazote abduction orthosis in the management of neonatal hip instability. J Pediatr Orthop. 2003;23:607–616. doi: 10.1097/00004694-200309000-00007. [DOI] [PubMed] [Google Scholar]
- 106.Sankar WN, Nduaguba A, Flynn JM. Ilfeld abduction orthosis is an effective second-line treatment after failure of Pavlik harness for infants with developmental dysplasia of the hip. J Bone Joint Surg Am. 2015;97:292–297. doi: 10.2106/JBJS.N.00707. [DOI] [PubMed] [Google Scholar]
- 107.Gans I, Flynn JM, Sankar WN. Abduction bracing for residual acetabular dysplasia in infantile DDH. J Pediatr Orthop. 2013;33:714–718. doi: 10.1097/BPO.0b013e31829d5704. [DOI] [PubMed] [Google Scholar]
- 108.Fish DN, Herzenberg JE, Hensinger RN. Current practice in use of prereduction traction for congenital dislocation of the hip. J Pediatr Orthop. 1991;11:149–153. doi: 10.1097/01241398-199103000-00002. [DOI] [PubMed] [Google Scholar]
- 109.Smith BG, Kasser JR, Hey LA, Jaramillo D, Millis MB. Postreduction computed tomography in developmental dislocation of the hip: part I: analysis of measurement reliability. J Pediatr Orthop. 1997;17:626–630. doi: 10.1097/00004694-199709000-00010. [DOI] [PubMed] [Google Scholar]
- 110.Smith BG, Millis MB, Hey LA, Jaramillo D, Kasser JR. Postreduction computed tomography in developmental dislocation of the hip: part II: predictive value for outcome. J Pediatr Orthop. 1997;17:631–636. doi: 10.1097/00004694-199709000-00011. [DOI] [PubMed] [Google Scholar]
- 111.Schoenecker PL, Dollard PA, Sheridan JJ, Strecker WB. Closed reduction of developmental dislocation of the hip in children older than 18 months. J Pediatr Orthop. 1995;15:763–767. doi: 10.1097/01241398-199511000-00008. [DOI] [PubMed] [Google Scholar]
- 112.Rampal V, Sabourin M, Erdeneshoo E, Koureas G, Seringe R, Wicart P. Closed reduction with traction for developmental dysplasia of the hip in children aged between one and five years. J Bone Joint Surg Br. 2008;90:858–863. doi: 10.1302/0301-620X.90B7.20041. [DOI] [PubMed] [Google Scholar]
- 113.Kaneko H, Kitoh H, Mishima K, Matsushita M, Ishiguro N. Long-term outcome of gradual reduction using overhead traction for developmental dysplasia of the hip over 6 months of age. J Pediatr Orthop. 2013;33:628–634. doi: 10.1097/BPO.0b013e31829b2d8b. [DOI] [PubMed] [Google Scholar]
- 114.Fukiage K, Futami T, Ogi Y, Harada Y, Shimozono F, Kashiwagi N, Takase T, Suzuki S. Ultrasound-guided gradual reduction using flexion and abduction continuous traction for developmental dysplasia of the hip: a new method of treatment. Bone Joint J. 2015;97-B:405–411. doi: 10.1302/0301-620X.97B3.34287. [DOI] [PubMed] [Google Scholar]
- 115.Terjesen T, Horn J, Gunderson RB. Fifty-year follow-up of late-detected hip dislocation: clinical and radiographic outcomes for seventy-one patients treated with traction to obtain gradual closed reduction. J Bone Joint Surg Am. 2014;96:e28. doi: 10.2106/JBJS.M.00397. [DOI] [PubMed] [Google Scholar]
- 116.Zionts LE, MacEwen GD. Treatment of congenital dislocation of the hip in children between the ages of one and three years. J Bone Joint Surg Am. 1986;68:829–846. [PubMed] [Google Scholar]
- 117.Millis MB, Zaltz I. Current perspectives on the pediatric hip: selected topics in hip dysplasia, Perthes disease, and chondrolysis: synopsis of the hip subspecialty session at the POSNA Annual Meeting, May 1, 2013, Toronto. J Pediatr Orthop. 2014;34 Suppl 1:S36–S43. doi: 10.1097/BPO.0000000000000286. [DOI] [PubMed] [Google Scholar]
- 118.Sosna A, Rejholec M. Ludloff’s open reduction of the hip: long-term results. J Pediatr Orthop. 1992;12:603–606. [PubMed] [Google Scholar]
- 119.Koizumi W, Moriya H, Tsuchiya K, Takeuchi T, Kamegaya M, Akita T. Ludloff’s medial approach for open reduction of congenital dislocation of the hip. A 20-year follow-up. J Bone Joint Surg Br. 1996;78:924–929. doi: 10.1302/0301-620x78b6.6885. [DOI] [PubMed] [Google Scholar]
- 120.Morcuende JA, Meyer MD, Dolan LA, Weinstein SL. Long-term outcome after open reduction through an anteromedial approach for congenital dislocation of the hip. J Bone Joint Surg Am. 1997;79:810–817. doi: 10.2106/00004623-199706000-00002. [DOI] [PubMed] [Google Scholar]
- 121.Ucar DH, Isiklar ZU, Stanitski CL, Kandemir U, Tumer Y. Open reduction through a medial approach in developmental dislocation of the hip: a follow-up study to skeletal maturity. J Pediatr Orthop. 2004;24:493–500. [PubMed] [Google Scholar]
- 122.Bulut O, Oztürk H, Tezeren G, Bulut S. Arthroscopic-assisted surgical treatment for developmental dislocation of the hip. Arthroscopy. 2005;21:574–579. doi: 10.1016/j.arthro.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 123.Oztürk H, Oztemür Z, Bulut O, Tezeren G, Bulut S. Arthroscopic-assisted surgical treatment for developmental dislocation of the hip before the age of 18 months. Arch Orthop Trauma Surg. 2013;133:1289–1294. doi: 10.1007/s00402-013-1781-y. [DOI] [PubMed] [Google Scholar]
- 124.Biçimoğlu A, Ağuş H, Omeroğlu H, Tümer Y. Posteromedial limited surgery in developmental dysplasia of the hip. Clin Orthop Relat Res. 2008;466:847–855. doi: 10.1007/s11999-008-0127-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Weinstein SL, Mubarak SJ, Wenger DR. Developmental hip dysplasia and dislocation: Part II. Instr Course Lect. 2004;53:531–542. [PubMed] [Google Scholar]
- 126.Gardner RO, Bradley CS, Howard A, Narayanan UG, Wedge JH, Kelley SP. The incidence of avascular necrosis and the radiographic outcome following medial open reduction in children with developmental dysplasia of the hip: a systematic review. Bone Joint J. 2014;96-B:279–286. doi: 10.1302/0301-620X.96B2.32361. [DOI] [PubMed] [Google Scholar]
- 127.Tarassoli P, Gargan MF, Atherton WG, Thomas SR. The medial approach for the treatment of children with developmental dysplasia of the hip. Bone Joint J. 2014;96-B:406–413. doi: 10.1302/0301-620X.96B3.32616. [DOI] [PubMed] [Google Scholar]
- 128.Kershaw CJ, Ware HE, Pattinson R, Fixsen JA. Revision of failed open reduction of congenital dislocation of the hip. J Bone Joint Surg Br. 1993;75:744–749. doi: 10.1302/0301-620X.75B5.8376431. [DOI] [PubMed] [Google Scholar]
- 129.McCluskey WP, Bassett GS, Mora-Garcia G, MacEwen GD. Treatment of failed open reduction for congenital dislocation of the hip. J Pediatr Orthop. 1989;9:633–639. doi: 10.1097/01241398-198911000-00001. [DOI] [PubMed] [Google Scholar]
- 130.Chmielewski J, Albiñana J. Failures of open reduction in developmental dislocation of the hip. J Pediatr Orthop B. 2002;11:284–289. [PubMed] [Google Scholar]
- 131.Sankar WN, Young CR, Lin AG, Crow SA, Baldwin KD, Moseley CF. Risk factors for failure after open reduction for DDH: a matched cohort analysis. J Pediatr Orthop. 2011;31:232–239. doi: 10.1097/BPO.0b013e31820c9b31. [DOI] [PubMed] [Google Scholar]
- 132.Wenger DR, Mubarak SJ, Henderson PC, Miyanji F. Ligamentum teres maintenance and transfer as a stabilizer in open reduction for pediatric hip dislocation: surgical technique and early clinical results. J Child Orthop. 2008;2:177–185. doi: 10.1007/s11832-008-0103-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bache CE, Graham HK, Dickens DR, Donnan L, Johnson MB, Nattrass G, O’Sullivan M, Torode IP. Ligamentum teres tenodesis in medial approach open reduction for developmental dislocation of the hip. J Pediatr Orthop. 2008;28:607–613. doi: 10.1097/BPO.0b013e318184202c. [DOI] [PubMed] [Google Scholar]
- 134.Alsiddiky AM, Bakarman KA, Alzain KO, Aljassir FF, Al-Ahaideb AS, Kremli MK, Zamzam MM, Mervyn Letts R. The early detection and management of unstable concentric closed reduction of DDH with percutaneous K-wire fixation in infants 6 to 12 months of age. J Pediatr Orthop. 2012;32:64–69. doi: 10.1097/BPO.0b013e318236b1fc. [DOI] [PubMed] [Google Scholar]
- 135.Castañeda P, Tejerina P, Nualart L, Cassis N. The safety and efficacy of a transarticular pin for maintaining reduction in patients with developmental dislocation of the hip undergoing an open reduction. J Pediatr Orthop. 2015;35:358–362. doi: 10.1097/BPO.0000000000000284. [DOI] [PubMed] [Google Scholar]
- 136.Gholve PA, Flynn JM, Garner MR, Millis MB, Kim YJ. Predictors for secondary procedures in walking DDH. J Pediatr Orthop. 2012;32:282–289. doi: 10.1097/BPO.0b013e31824b21a6. [DOI] [PubMed] [Google Scholar]
- 137.Sarban S, Ozturk A, Tabur H, Isikan UE. Anteversion of the acetabulum and femoral neck in early walking age patients with developmental dysplasia of the hip. J Pediatr Orthop B. 2005;14:410–414. doi: 10.1097/01202412-200511000-00003. [DOI] [PubMed] [Google Scholar]
- 138.Edelson JG, Hirsch M, Weinberg H, Attar D, Barmeir E. Congenital dislocation of the hip and computerised axial tomography. J Bone Joint Surg Br. 1984;66:472–478. doi: 10.1302/0301-620X.66B4.6746676. [DOI] [PubMed] [Google Scholar]
- 139.Sugano N, Noble PC, Kamaric E, Salama JK, Ochi T, Tullos HS. The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br. 1998;80:711–719. doi: 10.1302/0301-620x.80b4.8319. [DOI] [PubMed] [Google Scholar]
- 140.Berkeley ME, Dickson JH, Cain TE, Donovan MM. Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg Am. 1984;66:412–420. [PubMed] [Google Scholar]
- 141.Wenger DR, Lee CS, Kolman B. Derotational femoral shortening for developmental dislocation of the hip: special indications and results in the child younger than 2 years. J Pediatr Orthop. 1995;15:768–779. doi: 10.1097/01241398-199511000-00009. [DOI] [PubMed] [Google Scholar]
- 142.Weinstein SL. Developmental Hip Dysplasia and Dislocation. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 143.Herring JA. Developmental Dysplasia of the Hip. Philadelphia: WB Saunders; 2002. [Google Scholar]
- 144.Sankar WN, Neubuerger CO, Moseley CF. Femoral anteversion in developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:885–888. doi: 10.1097/BPO.0b013e3181c1e961. [DOI] [PubMed] [Google Scholar]
- 145.Salter RB. Innominate osteotomy in the treatment of congenital hip dislocation and subluxation of the hip. J Bone Joint Surg Br. 1961;43:518–539. [PubMed] [Google Scholar]
- 146.Kitoh H, Kaneko H, Ishiguro N. Radiographic analysis of movements of the acetabulum and the femoral head after Salter innominate osteotomy. J Pediatr Orthop. 2009;29:879–884. doi: 10.1097/BPO.0b013e3181c1e314. [DOI] [PubMed] [Google Scholar]
- 147.DelBello DA, Nattrass GR, Moseley CF, Watts HG. Acetabular development after open reduction in developmental dysplasia of the hip: The role of concurrent innominate osteotomy. Orthop Trans. 1995;19:298. [Google Scholar]
- 148.Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Joint Surg Br. 2004;86:876–886. doi: 10.1302/0301-620x.86b6.14441. [DOI] [PubMed] [Google Scholar]
- 149.Spence G, Hocking R, Wedge JH, Roposch A. Effect of innominate and femoral varus derotation osteotomy on acetabular development in developmental dysplasia of the hip. J Bone Joint Surg Am. 2009;91:2622–2636. doi: 10.2106/JBJS.H.01392. [DOI] [PubMed] [Google Scholar]
- 150.Thomas SR, Wedge JH, Salter RB. Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. J Bone Joint Surg Am. 2007;89:2341–2350. doi: 10.2106/JBJS.F.00857. [DOI] [PubMed] [Google Scholar]
- 151.Perlik PC, Westin GW, Marafioti RL. A combination pelvic osteotomy for acetabular dysplasia in children. J Bone Joint Surg Am. 1985;67:842–850. [PubMed] [Google Scholar]
- 152.Bursali A, Tonbul M. How are outcomes affected by combining the Pemberton and Salter osteotomies? Clin Orthop Relat Res. 2008;466:837–846. doi: 10.1007/s11999-008-0153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Steel HH. Triple osteotomy of the innominate bone. J Bone Joint Surg Am. 1973;55:343–350. [PubMed] [Google Scholar]
- 154.Faciszewski T, Coleman SS, Biddulph G. Triple innominate osteotomy for acetabular dysplasia. J Pediatr Orthop. 1993;13:426–430. doi: 10.1097/01241398-199307000-00002. [DOI] [PubMed] [Google Scholar]
- 155.Li YC, Wu KW, Huang SC, Wang TM, Kuo KN. Modified triple innominate osteotomy for acetabular dysplasia: for better femoral head medialization and coverage. J Pediatr Orthop B. 2012;21:193–199. doi: 10.1097/BPB.0b013e32834f4377. [DOI] [PubMed] [Google Scholar]
- 156.Lipton GE, Bowen JR. A new modified technique of triple osteotomy of the innominate bone for acetabular dysplasia. Clin Orthop Relat Res. 2005;434:78–85. doi: 10.1097/01.blo.0000163484.93211.94. [DOI] [PubMed] [Google Scholar]
- 157.Wall EJ, Kolata R, Roy DR, Mehlman CT, Crawford AH. Endoscopic pelvic osteotomy for the treatment of hip dysplasia. J Am Acad Orthop Surg. 2001;9:150–156. doi: 10.5435/00124635-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 158.Kim YJ, Noonan KJ. What’s new in pediatric orthopaedics. J Bone Joint Surg Am. 2010;92:1575–1582. doi: 10.2106/JBJS.J.00267. [DOI] [PubMed] [Google Scholar]
- 159.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 160.Troelsen A, Elmengaard B, Søballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179. doi: 10.2106/JBJS.H.00994. [DOI] [PubMed] [Google Scholar]
- 161.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Windhager R, Pongracz N, Schönecker W, Kotz R. Chiari osteotomy for congenital dislocation and subluxation of the hip. Results after 20 to 34 years follow-up. J Bone Joint Surg Br. 1991;73:890–895. doi: 10.1302/0301-620X.73B6.1955430. [DOI] [PubMed] [Google Scholar]
- 163.Kotz R, Chiari C, Hofstaetter JG, Lunzer A, Peloschek P. Long-term experience with Chiari’s osteotomy. Clin Orthop Relat Res. 2009;467:2215–2220. doi: 10.1007/s11999-009-0910-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Staheli LT, Chew DE. Slotted acetabular augmentation in childhood and adolescence. J Pediatr Orthop. 1992;12:569–580. [PubMed] [Google Scholar]
- 165.Jellicoe P, Aitken A, Wright K. Ultrasound screening in developmental hip dysplasia: do all scanned hips need to be followed up? J Pediatr Orthop B. 2007;16:192–195. doi: 10.1097/BPB.0b013e328014058d. [DOI] [PubMed] [Google Scholar]
- 166.Arumilli BR, Koneru P, Garg NK, Davies R, Saville S, Sampath J, Bruce C. Is secondary radiological follow-up of infants with a family history of developmental dysplasia of the hip necessary? J Bone Joint Surg Br. 2006;88:1224–1227. doi: 10.1302/0301-620X.88B9.17330. [DOI] [PubMed] [Google Scholar]
- 167.Osarumwense D, Popple D, Kershaw IF, Kershaw CJ, Furlong AJ. What follow-up is required for children with a family history of developmental dysplasia of the hip? J Pediatr Orthop B. 2007;16:399–402. doi: 10.1097/BPB.0b013e3282f05944. [DOI] [PubMed] [Google Scholar]
- 168.Modaressi K, Erschbamer M, Exner GU. Dysplasia of the hip in adolescent patients successfully treated for developmental dysplasia of the hip. J Child Orthop. 2011;5:261–266. doi: 10.1007/s11832-011-0356-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Dornacher D, Cakir B, Reichel H, Nelitz M. Early radiological outcome of ultrasound monitoring in infants with developmental dysplasia of the hips. J Pediatr Orthop B. 2010;19:27–31. doi: 10.1097/BPB.0b013e328330335e. [DOI] [PubMed] [Google Scholar]
- 170.Alexiev VA, Harcke HT, Kumar SJ. Residual dysplasia after successful Pavlik harness treatment: early ultrasound predictors. J Pediatr Orthop. 2006;26:16–23. doi: 10.1097/01.bpo.0000187995.02140.c7. [DOI] [PubMed] [Google Scholar]
- 171.Bone CM, Hsieh GH. The risk of carcinogenesis from radiographs to pediatric orthopaedic patients. J Pediatr Orthop. 2000;20:251–254. [PubMed] [Google Scholar]
- 172.Rajaraman P, Simpson J, Neta G, Berrington de Gonzalez A, Ansell P, Linet MS, Ron E, Roman E. Early life exposure to diagnostic radiation and ultrasound scans and risk of childhood cancer: case-control study. BMJ. 2011;342:d472. doi: 10.1136/bmj.d472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Sarkissian EJ, Sankar WN, Zhu X, Wu CH, Flynn JM. Radiographic Follow-up of DDH in Infants: Are X-rays Necessary After a Normalized Ultrasound? J Pediatr Orthop. 2015;35:551–555. doi: 10.1097/BPO.0000000000000326. [DOI] [PubMed] [Google Scholar]
- 174.David M, Robb C, Jawanda S, Bache C, Bradish C. Late recurrence of developmental dysplasia of the hip following Pavlik harness treatment until normal ultrasound appearance. J Orthop. 2015;12:81–85. doi: 10.1016/j.jor.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Song FS, McCarthy JJ, MacEwen GD, Fuchs KE, Dulka SE. The incidence of occult dysplasia of the contralateral hip in children with unilateral hip dysplasia. J Pediatr Orthop. 2008;28:173–176. doi: 10.1097/BPO.0b013e318164ee2d. [DOI] [PubMed] [Google Scholar]


