Abstract
The efficacy of hybrid assistive limb (HAL) rehabilitation in the acute phase of stroke remains unclear. The purpose of this study was to evaluate the outcomes of patients with acute intracranial hemorrhage (ICH) who were treated with or without HAL rehabilitation. Among 270 patients with acute ICH from 2009 to 2014, 91 patients with supratentorial ICH were included in this retrospective study. Of these, 14 patients (HAL group) received HAL rehabilitation at approximately 1 week after ICH occurrence, while the remaining 77 patients received usual rehabilitation without HAL (N-HAL group). We obtained various patient data from the hospitals where the patients were moved to for further rehabilitation. Statistical comparisons were performed for the characteristics of the ICH patients, and outcomes between the HAL and N-HAL groups. There were no differences in outcomes between the HAL and N-HAL groups. However, patients with right ICH in the HAL group exhibited a significant association with a functional independence measure (FIM) score of ≥ 110 compared with patients in the N-HAL group (HAL group: 81.8%, N-HAL group: 43.9%, P = 0.04). In patients with right ICH, HAL rehabilitation was associated with improved outcomes as evaluated by the FIM score. Thus, HAL rehabilitation may improve outcomes of acute ICH in appropriately selected patients.
Keywords: acute stroke, intracerebral hemorrhage, hybrid assistive limb, rehabilitation, outcome, functional independence measure
Introduction
A wearable-type robot hybrid assistive limb (HAL) has been developed to provide physical support for patients in their daily activities and for heavy work. The HAL is a robot suit that can assist voluntary control of knee and hip joint motion by detecting very subtle bioelectric signals from muscles.1) This walking-aid system enables the user to perform movements smoothly such as standing up, sitting down, and going up and down stairs.2) HAL technologies have also advanced to provide assistance for rehabilitation in various diseases. For example, HAL was recently reported to be beneficial in patients with chronic phase stroke or spinal cord injury.3–5)
We previously reported the tolerability and safety of HAL for patients with acute stroke.6) However, the efficacy of HAL rehabilitation for patients with stroke in the acute phase remains unclear. Thus, in the present study we compared the outcomes of patients with acute intracranial hemorrhage (ICH) who were treated with and without HAL rehabilitation.
Materials and Methods
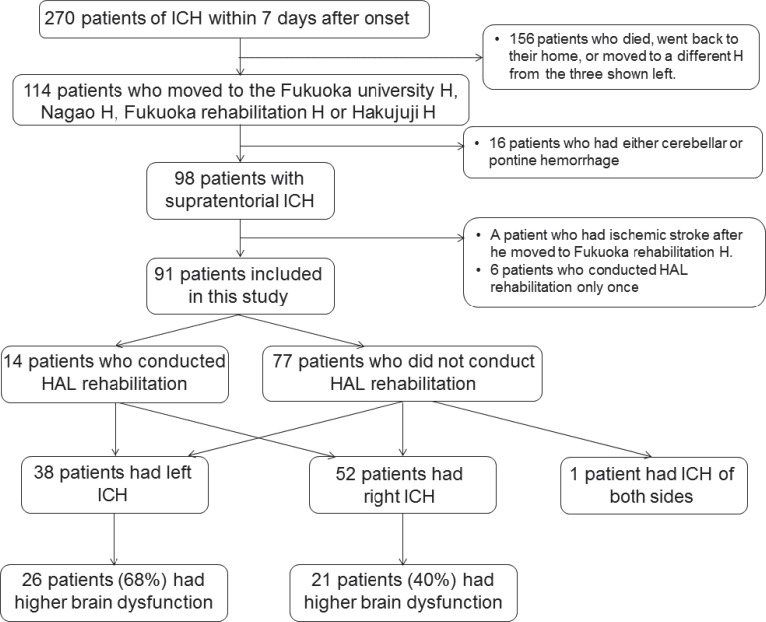
We registered a total of 270 patients with acute ICH in the neurosurgical department of Fukuoka University Hospital from January 2009 to February 2014 (Fig. 1). Of these, we included patients with supratentorial ICH who moved to Nagao Hospital, Fukuoka Rehabilitation Hospital, or Hakujuji Hospital for further rehabilitation, all of which are neighboring hospitals that specialize in rehabilitation. One patient was excluded from this study as he had an ischemic stroke shortly after he was moved. HAL rehabilitation was started for patients at approximately 1 week after the occurrence of ICH. The HAL rehabilitation protocol was the same as we previously reported.6) In brief, patients were included if they satisfied the following criteria: hemorrhagic stroke with either hemiplegia or ataxia, Glasgow Coma Scale (GCS) over 9, and systolic blood pressure of 100–160 mmHg. This study was approved by the ethics committees of Fukuoka University Hospital, Nagao Hospital, Fukuoka Rehabilitation Hospital, and Hakujuji Hospital. Written informed consent was obtained from all patients.
Fig. 1.
Flowchart of patient selection. H: hospital, HAL: hybrid assistive limb, ICH: intracerebral hemorrhage.
The HAL robot suit is an exoskeleton with a frame and robotic actuators that attach to the patient's legs. Joint movement is supported by electric motors. To support voluntary movement of the patients, HAL detects minimal bioelectrical signals that emerge from extensor and flexor muscles of the hip and knee via electromyography electrodes. The voluntary robotic system was used in the present study, which was enabled by a cable connection between the exoskeleton and the patient. On the first day of HAL rehabilitation, every patient wore a double-leg model HAL, while the choice of a single or double model HAL on the second day and thereafter was dependent on each patient. Vital signs were carefully monitored to prevent adverse accidents such as fall or orthostatic hypotension. During HAL rehabilitation, telescopic motion of the lower legs, standing and sitting, and walking were performed, although the exact type and amount of training varied from patient to patient. Six patients were excluded from this study as they received HAL rehabilitation only once.
After the patients moved to any of the three hospitals, they continued rehabilitation. We attempted to obtain patient information from the three hospitals regarding the date and condition at discharge. Data on activities of daily living collected included the Brunnstrom stage of hand, arm, and leg, the Barthel index (BI), and the functional independence measure (FIM).
Descriptive analyses of demographic and characteristics data were performed using frequency distribution for categorical data and median for continuous variables. Differences between patients with HAL rehabilitation in their acute phase (HAL group) and those without (N-HAL group) were assessed by the Mann–Whitney U test (for continuous variables), while Fisher's exact test was used for the categorical variables. For outcome analyses, all patients were divided into two groups depending on whether their FIM was ≥ 110, while the threshold of BI was 85. For sub-analyses, patients were categorized into ICH in the right or left hemisphere. One patient was excluded from the sub-analyses as he had ICH in both cerebral hemispheres. P values < 0.05 were considered statistically significant. Data were analyzed using SPSS for Windows version 22.0 (SPSS; IBM Co., Armonk, New York, USA).
Results
Of the 91 patients included in our study, 14 patients received HAL rehabilitation, while 77 patients did not (Fig. 1). As patients at Fukuoka Rehabilitation Hospital and Hakujuji Hospital could perform or continue HAL rehabilitation, 11 out of the 14 patients with HAL rehabilitation in our hospital continued HAL at the hospital to which they were transferred (Table 1). All the patients who did not receive HAL rehabilitation in our hospital did not receive HAL in the chronic recovery phase.
Table 1.
Summary of patients who performed hybrid assistive limb rehabilitation in our hospital
| Age (years) | Sex | Character of ICH | Side | Amount of hemorrhage (mL) | Operation | Number of HAL treatments | The hospital where they moved | Continuation of HAL rehabilitation in the next hospital | Total hospital stay (days) |
|---|---|---|---|---|---|---|---|---|---|
| 57 | F | Thalamus | R | 19.98 | N | 3 | NH | NC | 48 |
| 64 | M | Thalamus | L | 19.76 | Y | 4 | NH | NC | 231 |
| 49 | F | Lobar | R | 22.59 | Y | 3 | HH | C | 209 |
| 70 | M | Ventricular | R | 4.58 | Y | 3 | HH | C | 207 |
| 69 | F | Putamen | L | 47.74 | Y | 6 | HH | C | 231 |
| 63 | F | Thalamus | R | 1.46 | N | 6 | HH | C | 165 |
| 69 | F | Putamen | R | 9.49 | N | 6 | FH | C | 138 |
| 56 | F | Lobar | R | 21.0 | Y | 6 | FH | C | 220 |
| 77 | M | Putamen | L | 19.7 | Y | 3 | FH | NC | 215 |
| 66 | F | Thalamus | R | 7.78 | N | 4 | FH | C | 71 |
| 69 | F | Putamen | R | 74.4 | Y | 3 | FH | C | 217 |
| 69 | F | Putamen | R | 35.28 | N | 3 | FH | C | 73 |
| 64 | M | Thalamus | R | 4.45 | N | 3 | FH | C | 108 |
| 54 | M | Mixed | R | 72.58 | Y | 5 | FH | C | 101 |
C: continued, F: female, FH: Fukuoka Rehabilitation Hospital, HAL: hybrid assistive limb, HH: Hakujuji Hospital, ICH: intracerebral hemorrhage, M: male, N: no, NC: not continued, NH: Nagao Hospital, Y: yes.
When patients were grouped into HAL and N-HAL groups, there was a trend for more severe National Institutes of Health Stroke Scale (NIHSS) score at admission in the HAL group compared with patients in the N-HAL group (Table 2). Similarly, the total hospital stay tended to be longer in the HAL group. The outcome scales were not different between the two groups.
Table 2.
Comparison of features and outcomes between hybrid assistive limb (HAL) and N-HAL groups
| HAL group (N = 14) | N-HAL group (N = 77) | P value | |
|---|---|---|---|
| Age | 65 (57–69) | 64 (57–75) | 0.865 |
| Sex (male) | 5 (35.7%) | 43 (55.8%) | 0.245 |
| NIHSS | 15 (9–30) | 11 (4–20) | 0.098 |
| GCS | 14 (11–15) | 14 (9–15) | 0.829 |
| Amount of hematoma (mL) | 19.87 (6.98–38.39) | 15.64 (5.84–33.74) | 0.708 |
| Site of hematoma | 0.731 | ||
| subcortical | 2 (14.2%) | 23 (29.9%) | |
| putamen | 4 (28.6%) | 21 (27.2%) | |
| thalamus | 5 (35.7%) | 18 (23.3%) | |
| mixed | 2 (14.2%) | 9 (11.7%) | |
| other | 1 (7.1%) | 6 (7.8%) | |
| Presence of ventricular hematoma | 4 (28.6%) | 24 (31.2%) | 1 |
| side of hematoma | 0.272 | ||
| right | 11 (78.6%) | 41 (53.2%) | |
| left | 3 (21.4%) | 35 (45.5%) | |
| both | 0 (0%) | 1 (1.3%) | |
| operation | 8 (57.1%) | 43 (55.8%) | 1 |
| Hospital stay of ours (days) | 21 (17–30) | 13 (9–19) | 0.001 |
| BI ≥ 85 | 7 (50%) | 40 (51.9%) | 1 |
| FIM ≥ 110 | 9 (64.3%) | 31 (40.3%) | 0.143 |
| Br. stage of upper extremities | 5 (3–6) | 4 (2–6) | 0.778 |
| Br. stage of hand function | 5 (3–6) | 4 (2–6) | 0.827 |
| Br. stage of lower extremities | 5 (3–6) | 5 (3–6) | 0.971 |
| Home discharge from a neighboring hospital | 11 (78.6%) | 44 (57.1%) | 0.152 |
| Hospital stay of a neighboring hospital (days) | 163 (66–196) | 110 (50–164) | 0.164 |
| Total hospital stay from ours to a neighboring one | 186 (94–218) | 123 (62–182) | 0.081 |
BI: Barthel index, Br: Brunnstrom, FIM: functional independence measure, GCS: Glasgow Coma Scale, HAL: hybrid assistive limb, NIHSS: National Institutes of Health Stroke Scale.
For the sub analysis in which patients were separated according to the side of ICH, the rate of FIM ≥ 110 was significantly higher in the HAL group than the N-HAL group in patients with right ICH (Table 3, P = 0.04 ). There were no differences in the total length of hospital stay, although the length of stay at our hospital was significantly longer in the right ICH HAL group. By contrast, there were no differences in outcomes for HAL treatment in patients with left ICH.
Table 3.
Comparison of features and outcomes of patients with right intracranial hemorrhage between hybrid assistive limb (HAL) and N-HAL groups
| HAL group (N = 11) | N-HAL group (N = 41) | P value | |
|---|---|---|---|
| Age | 64 (56–69) | 64 (56–77) | 0.56 |
| Sex (male) | 3 (27.3%) | 22 (53.7%) | 0.177 |
| NIHSS | 14 (8–28) | 11 (5–16) | 0.269 |
| GCS | 14 (12–15) | 14 (10–15) | 0.549 |
| Amount of hematoma (mL) | 19.98 (4.58–35.28) | 15.64 (6.18–33.5) | 0.902 |
| Site of hematoma | 0.932 | ||
| subcortical | 2 (18.2%) | 13 (31.7%) | |
| putamen | 3 (27.3%) | 9 (22.0%) | |
| thalamus | 4 (36.4%) | 12 (29.3%) | |
| mixed | 1 (9.1%) | 3 (7.3%) | |
| other | 1 (9.1%) | 4 (9.8%) | |
| Presence of ventricular hematoma | 2 (18.2%) | 15 (36.6%) | 0.304 |
| Operation | 5 (45.5%) | 24 (58.5%) | 0.507 |
| Hospital stay of ours (days) | 22 (16–30) | 13 (9–18) | 0.003 |
| BI ≥ 85 | 7 (63.6%) | 20 (48.8%) | 0.503 |
| FIM ≥ 110 | 9 (81.8%) | 18 (43.9%) | 0.04 |
| Br. stage of upper extremities | 6 (4–6) | 4 (2–6) | 0.165 |
| Br. stage of hand function | 5 (4–6) | 4 (2–6) | 0.2 |
| Br. stage of lower extremities | 6 (4–6) | 4 (3–6) | 0.221 |
| Home discharge from a neighboring hospital | 9 (81.8%) | 25 (61.0%) | 0.291 |
| Hospital stay of a neighboring hospital | 119 (58–179) | 113 (61–180) | 0.937 |
| Total hospital stay from ours to a neighboring one | 138 (73–209) | 132 (73–197) | 0.762 |
BI: Barthel index, Br: Brunnstrom, FIM: functional independence measure, GCS: Glasgow Coma Scale, HAL: hybrid assistive limb, NIHSS: National Institutes of Health Stroke Scale.
I. Case 1: right side ICH
A 54-year-old man who was transferred to our emergency ward was diagnosed to have right mixed type of hemorrhage of 73 mL. Initially, he suffered from consciousness disturbance, conjugate deviation, unilateral spatial neglect, and left hemiparesis, and his NIHSS score at admission was 17. Because neurological deterioration was not seen after endoscopic hematoma evacuation and control of blood pressure, HAL rehabilitation was initiated on day 10. Totally, he conducted HAL rehabilitation 5 times in our hospital. After moving to a convalescence stage at hospital, he continued with HAL rehabilitation on top of standard rehabilitation, and his HAL rehabilitation reached 9 times. His neurological symptoms were improved and he left hospital on day 101. At discharge, his FIM score was 116.
II. Case 2: left side ICH
A 64-year-old man who had consciousness disturbance, aphasia, dysarthria, and right hemiparesis was hospitalized in our emergency ward. Left thalamic hemorrhage (total amount: 20 mL) with ventricular hemorrhage was diagnosed. His NIHSS score at admission was 15. After endoscopic hematoma evacuation and ventricular drainage, HAL rehabilitation was started on day 7. Although he conducted HAL rehabilitation 4 times in our hospital, he was unable to do it sufficiently because of his weariness. After moving to a convalescence stage at hospital, he stopped HAL rehabilitation. Finally, he left hospital on day 231. At discharge, his FIM score was 72.
Discussion
The aim of the present study was to determine the effect of HAL rehabilitation in the acute phase of ICH on patient outcomes. Our key finding was that HAL rehabilitation could improve functional recovery in patients with right hemisphere ICH compared with those with left hemisphere ICH.
There is an increasing evidence that early onset, intensive, repetitive, task-specific training may accelerate functional restitution after stroke and improve final motor outcomes,7) although most motor rehabilitation trials have been performed in the chronic stage post stroke.8) Although HAL rehabilitation is effective in sub-acute stroke patients when rehabilitation was delayed until 7 weeks after stroke onset,4) the efficacy in patients with acute stroke is unknown. Therefore, we evaluated the efficacy of HAL rehabilitation started in the acute phase on function in patients with ICH.
The main finding of the present study was that acute-phase HAL treatment was beneficial in patients with right hemisphere ICH. Although the causes of the better effect in the right side ICH are unknown, there were more patients with right ICH who received HAL rehabilitation in our study. Patients with left hemisphere ICH may also have more difficulties performing HAL rehabilitation, likely because of language dysfunction. Aphasic patients are often unable to understand their therapist's instructions on performing manual tasks of neurorehabilitation treatments for both paretic and aphasic symptoms.9) In these cases, encouraging the treatment of aphasia is needed in order to improve communication, for example by means of gesture training. Indeed, in our experience, language dysfunction due to left hemisphere damage can often affect patient's comprehension of the HAL rehabilitation instructions, even by using gesture. Thus, it would be difficult for patients with aphasia to receive a complete beneficial effect of HAL rehabilitation. Some idea would be necessary to perform HAL rehabilitation effectively in patients who had both hemiparesis and aphasia.
On the other hand, it remains unclear whether HAL rehabilitation may positively affect the outcomes of ischemic stroke patients. It was reported that ICH led to better functional outcome after stroke severity, basal disability, age, and sex; and onset admission intervals were matched between ICH and cerebral infarct.10) They said that the difference in outcome was caused by the mechanism of neurological deficits, wherein ICHs were partly caused by brain compression while the death of brain cells was the reason in cerebral infarct.10) Since the ways of recovering neurological deficits are different between ICH and ischemic stroke,11) the effect of HAL rehabilitation might be different between them, further studies are required.
We propose four possible effects of HAL rehabilitation on the acute phase of stroke, as follows: (1) reducing the burden of assistance from physical therapists, (2) promoting patients to apply their weight load onto the paralyzed leg by providing a sense of ease when assisted by HAL, (3) showing patients their gravity position with the gravity sensor, and (4) measuring the strength of the bioelectric signals in the muscles. Visualizing the position of gravity and semi-quantifying the bioelectric signals are important functions not provided by conventional rehabilitation, which likely contribute to the efficacy of HAL rehabilitation in patients with acute stroke.
There are several limitations of this study. First, this was a retrospective design. Second, the number of patients who performed HAL rehabilitation was small. Thus, a system that allows patients with acute stroke to perform HAL rehabilitation should be established. Third, many patients were excluded as they moved to different hospitals from those used in our study. Furthermore, some patients continued HAL rehabilitation after moving to subsequent hospitals. As beneficial effects of HAL rehabilitation in the subacute or chronic phase have been reported,4,5) it is unknown whether the improvement in outcomes in the present study originated from acute or chronic HAL rehabilitation. Randomized controlled trials are required to confirm the effect of HAL in acute stroke patients.
In conclusion, in this retrospective study we found no evidence that HAL rehabilitation was effective in patients with acute hemorrhagic stroke. However, in patients with right ICH, HAL rehabilitation was significantly associated with good outcome evaluated by FIM score, suggesting that HAL rehabilitation may improve function in selected patients with acute ICH.
Acknowledgments
The authors thank Dr. Fumitada Hattori at Nagao Hospital, Dr. Nobuyuki Irie at Fukuoka Rehabilitation Hospital, and Dr. Shuji Hayashi at Hakujuji Hospital, for their assistance and valuable comments. They also thank Ms. Asuka Ikezaki for her technical assistance. This study was partly supported by the Clinical Research Institute in Japan.
References
- 1). Kasaoka K, Sankai Y: Predictive control estimating operator's intention for stepping-up motion by exoskeleton type power assist system HAL. Proceedings 2001 IEEE/RSJ International Conference on Intelligent Robots and Systems. Maui, Hawaii, USA; Oct. 29–Nov. 3, 2001. [Google Scholar]
- 2). Lee S, Sankai Y: Power assist control for leg with HAL-3 based on virtual torque 347 and impedance adjustment. Proceedings of the IEEE International Conference on 348 Systems, Man and Cybernetics 4: 6, 2002. [Google Scholar]
- 3). Aach M, Cruciger O, Sczesny-Kaiser M, Höffken O, Meindl RCh, Tegenthoff M, Schwenkreis P, Sankai Y, Schildhauer TA: Voluntary driven exoskeleton as a new tool for rehabilitation in chronic spinal cord injury: a pilot study. Spine J 14: 2847– 2853, 2014. [DOI] [PubMed] [Google Scholar]
- 4). Kawamoto H, Kamibayashi K, Nakata Y, Yamawaki K, Ariyasu R, Sankai Y, Sakane M, Eguchi K, Ochiai N: Pilot study of locomotion improvement using hybrid assistive limb in chronic stroke patients. BMC Neurol 13: 141, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Nilsson A, Vreede KS, Häglund V, Kawamoto H, Sankai Y, Borg J: Gait training early after stroke with a new exoskeleton—the hybrid assistive limb: a study of safety and feasibility. J Neuroeng Rehabil 11: 92, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Ueba T, Hamada O, Ogata T, Inoue T, Shiota E, Sankai Y: Feasibility and safety of acute phase rehabilitation after stroke using the hybrid assistive limb robot suit. Neurol Med Chir (Tokyo) 53: 287– 290, 2013. [DOI] [PubMed] [Google Scholar]
- 7). Kwakkel G, van Peppen R, Wagenaar RC, Wood Dauphinee S, Richards C, Ashburn A, Miller K, Lincoln N, Partridge C, Wellwood I, Langhorne P: Effects of augmented exercise therapy time after stroke: a meta-analysis. Stroke 35: 2529– 2539, 2004. [DOI] [PubMed] [Google Scholar]
- 8). Stinear C, Ackerley S, Byblow W: Rehabilitation is initiated early after stroke, but most motor rehabilitation trials are not: a systematic review. Stroke 44: 2039– 2045, 2013. [DOI] [PubMed] [Google Scholar]
- 9). Ertelt D, Binkofski F: Action observation as a tool for neurorehabilitation to moderate motor deficits and aphasia following stroke. Neural Regen Res 7: 2063– 2074, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). Paolucci S, Antonucci G, Grasso MG, Bragoni M, Coiro P, De Angelis D, Fusco FR, Morelli D, Venturiero V, Troisi E, Pratesi L: Functional outcome of ischemic and hemorrhagic stroke patients after inpatient rehabilitation: a matched comparison. Stroke 34: 2861– 2865, 2003. [DOI] [PubMed] [Google Scholar]
- 11). Chae J, Zorowitz RD, Johnston MV: Functional outcome of hemorrhagic and nonhemorrhagic stroke patients after in-patient rehabilitation. Am J Phys Med Rehabil 75: 177– 182, 1996. [DOI] [PubMed] [Google Scholar]