Abstract
Background:
Pharmacist interventions have been shown to have an impact on reducing readmission rates, however further research is necessary to target resources to high-risk populations and determine the most effective bundle of interventions.
Objective:
To evaluate the effect of a pharmacist-bundled intervention on 30-day readmission rates for high-risk patients with pneumonia.
Methods:
A pilot study with a historical control conducted at a community, teaching-affiliated medical center. Up to 65 selected subjects were included if they had pneumonia and any of the following high-risk criteria: admission within 6 months, at least 5 scheduled home medications, chronic obstructive pulmonary disease (COPD), or heart failure. A retrospective chart review was conducted to compile the historical control group that received usual care between June and November 2013. Patients admitted from December 2013 through March 2014 were reviewed to receive a bundled intervention. The primary outcome was 30-day readmission rates. Risk factors and reasons for readmission, pharmacist clinical interventions, and the time interval between discharge and readmission were also evaluated.
Results:
A trend toward a reduced 30-day readmission rate was observed in the intervention group (n = 43) compared to those who received usual care (n = 65) (27.9% vs 40.0%; relative risk [RR], 0.6977; 95% CI, 0.3965–1.2278; P = .2119). The most commonly identified high-risk inclusion criteria were having at least 5 scheduled home medications and COPD. The time interval between discharge and readmission did not considerably differ between groups (10.8 vs 10.6 days).
Conclusions:
The pharmacist-bundled intervention was associated with a reduced 30-day readmission rate for high-risk patients with pneumonia.
Keywords: discharge planning, hospital readmissions, medication reconciliationv, pharmacistv, risk, factors
Reducing readmission rates has been a persistent priority for many policymakers as a means to improve the quality of health care and reduce costs. Nearly 1 in 6 Medicare patients discharged from the hospital is rehospitalized within 30 days, and Medicare expenditures for potentially preventable rehospitalizations are estimated to be as high as $17 billion a year.1–3 These data encouraged hospital accountability, with a focus on readmissions, to become an important element of health care reform. Subsequently, the Patient Protection and Affordable Care Act (ACA) of 2010 introduced the Hospital Readmissions Reduction Program. This program requires Centers for Medicare & Medicaid Services (CMS) to reduce payments to inpatient prospective payment systems (IPPS) with excessive readmissions effective for discharges on October 1, 2012. The penalties currently apply to 3 conditions, including acute myocardial infarction, heart failure, and pneumonia. Penalties for the fiscal year (FY) 2013 were reported to total $280 million. In addition, CMS has finalized the expansion of applicable conditions to include chronic obstructive pulmonary disease (COPD) and elective total hip arthroplasty and total knee arthroplasty in FY 2015, with other third-party payers likely implementing similar penalties in the future.4 Therefore, reducing hospital readmissions by providing the utmost quality of health care possible is now becoming a priority for institutions as well.
Several studies have been published describing efforts to assess patients at risk for readmission and interventions to reduce readmissions.5 Within this body of literature, adverse medication events and nonadherence have been found to be main contributors to readmission rates and the health care system’s financial burden.6–9 One in every 5 people discharged experience an adverse event, with greater than twothirds being medication-related and a majority of these considered preventable.6 Nonadherence, contributing to treatment failures and lost resources, is estimated to cost $150 billion every year.10 Coleman and colleagues found that patients with medication discrepancies after discharge had greater than double the 30-day readmission rate compared to patients without medication discrepancies, 14.3% and 6.1%, respectively.11 Another concern is the deficiency of patient understanding of medications and treatment plans at discharge, with one study identifying fewer than half of patients able to list their diagnoses, the names and purposes of their medications, or the major side effects.12
Due to the impact of medication-related issues, pharmacist involvement throughout the hospitalization and discharge process has been recognized as a vital component of efforts to reduce readmissions. Several programs, such as Project RED,13 STARR,14 and Care Transitions Program,15 have demonstrated some success in reducing readmissions with the utilization of a pharmacist. However, these programs require extensive resources and are not specifically designed to target high-risk patients. Another initiative, Project BOOST, developed a tool to identify high-risk patients, although the program implementation is still resource intensive.16
Although numerous studies have established the valuable influence of pharmacist participation during the hospitalization and transitions of care, data are conflicting regarding reduced readmission rates.13,15,17–21 Additionally, the variability of interventions described in the literature has lead to heterogeneous comparisons. Although no single intervention has been shown to reliably reduce readmissions, providing a bundled intervention (ie, medication reconciliation, counseling, and follow-up phone call) and targeting high-risk patient populations have been shown to have the most benefit.5 Likewise, no particular set of high-risk criteria has been widely established, but patients with multiple medications, specific comorbidities, and a history of recent hospitalization have all been associated with increased readmission rates.5,11,20,21 A recent systematic review of the literature indicated that further research is necessary to target resources to a high-risk patient population and determine the most effective bundle of interventions to reduce readmissions.5 This pilot study aimed to evaluate the effect of a pharmacistspecific bundled intervention on 30-day readmission rates for high-risk patients with pneumonia.
Methods
Study Design
A pilot study with a historical control was conducted at DCH Regional Medical Center, a community, not-for-profit, teaching-affiliated medical center in Tuscaloosa, Alabama. Pneumonia was chosen as the target condition for this study, because it was associated with the highest 30-day readmission rates at DCH Regional Medical Center. The institution’s home health department conducts postdischarge follow-up phone calls for patients without a home health referral for specific diagnoses, including heart failure and pneumonia. Other than the postdischarge phone calls and standard nursing education, there are no additional institutional standardized efforts dedicated to patients with pneumonia. This study was approved by the institutional review boards of the health system and university.
Subjects
Patients 19 years of age or older admitted with a working diagnosis of pneumonia were identified for potential inclusion in the study if they had any of the following high-risk criteria: previous admission within 6 months, greater than or equal to 5 scheduled home medications, COPD, or heart failure. These criteria were risk factors associated with increased readmission rates identified both in the literature and at our institution.5,11,20–22 Patients were excluded if admitted from or discharged to a skilled nursing facility or other hospital, admitted to an intensive care unit (ICU), non-English speaking, without telephone access, pregnant, receiving hospice services, or diagnosed with dementia or any psychological or physical disorder that would prevent them from participating in patient education. Medicaid patients were excluded due to a contract Alabama CMS has with a private nonprofit care management organization that provides similar pharmacy consultation services. A retrospective chart review was completed to compile the historical control that received usual care between June and November 2013. Usual care may have included medication reconciliation performed by nursing, antibiotic therapy via the physician’s discretion, nurse education, and a home health followup phone call.
Pharmacist Intervention
Patients admitted from December 2013 through March 2014 with a working diagnosis of pneumonia were included on a computer-generated work list. A nurse or unit secretary entered the working diagnosis based on information available in the medical record, therefore the pharmacist confirmed pneumonia as an active diagnosis during the screening process. The work list was reviewed Monday through Friday, excluding holidays and days the pharmacist was not present. Patients were further evaluated for inclusion with data obtained from the medical record, software programs (ie, MIDAS), and patient interviews when necessary. Patients admitted and discharged before the pharmacist had an opportunity to begin the intervention were excluded from the intervention group.
Patients were followed prospectively through their admission and the pharmacist conducted a bundled intervention including medication reconciliation, therapeutic recommendations, patient discharge counseling, and a postdischarge follow-up phone call. Each medication list was scanned for drug interactions, pertinent allergies, and duplications, and these were appropriately addressed with the medical team as clinically indicated. Therapeutic recommendations were made regarding, but not limited to, drug selection, dosages, and monitoring for optimized treatment of pneumonia. An effort was made to confirm that a cost-effective option was prescribed for each patient. Once the attending physician indicated discharge plans, each patient and/or family member received counseling on antibiotic therapy and any new changes in therapy pertinent to the home medication list. Each patient received a postdischarge follow-up phone call within 48 to 96 hours after discharge to address medication adherence, adverse drug events (ADEs), or medication questions. If the patient was unable to be contacted after 3 attempts, he or she was considered lost to follow-up and any available data were included in the final analysis. Patients in the intervention group were followed for 30 days to assess for readmission for any reason. The 30-day readmission rate of the historical control was compared to the 30-day readmission rate of the intervention group to evaluate the effect of a pharmacist’s involvement. The primary investigator, who was completing a postgraduate year 1 (PGY1) residency at the time, conducted all prospective interventions.
Data Collection
Patient characteristics and clinical data pertaining to the admission and treatment for pneumonia were obtained from the medical records. For the retrospective analysis, dates and reasons for readmissions within 30 days of discharge as well as home health follow-up phone calls and referrals were collected. For the prospective analysis, errors identified during medication reconciliation were categorized as medication omissions, medication additions, incorrect dose and/or frequency, duplicate therapy, and nonadherence. If applicable, reasons for not filling antibiotic prescriptions, missed doses, and ADEs were collected during the follow-up phone call. Home health follow-up phone call attempts, filled antibiotic prescriptions, and reasons for readmission were also collected from the electronic medical record and by contacting community pharmacies as necessary.
Study Outcomes
The primary outcome was readmission for any reason within 30 days of discharge. Secondary outcomes included risk factors and reasons for readmission, documented pharmacist clinical interventions, and the time interval between discharge and readmission.
Statistical Analysis
Patient characteristics and secondary outcomes were analyzed using descriptive statistics. To accommodate resource and time constraints while still implementing the intervention and generating pilot data, an a priori decision was made to utilize convenience sampling and enroll up to 65 patients in both the retrospective and prospective analyses. This sample size was calculated based on the anticipated target population during the intervention period. A relative risk (RR) was calculated using a 95% confidence interval and an a priori level of significance was set at .05 for the primary outcome. Primary outcome data were analyzed using MedCalc Software for Windows (MedCalc Software Version 13.2.2; Ostend, Belgium).
Results
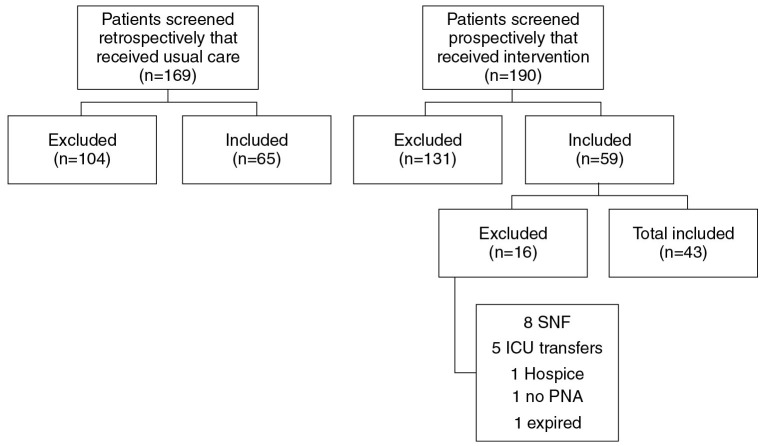
Sixty-five patients were included in the historical control and 43 in the intervention group (Figure 1). Baseline characteristics were fairly well balanced in regard to age, gender, and the average number of risk factors present per patient (Table 1). However, there were a greater percentage of patients in the control group previously admitted within 6 months compared to the intervention group.
Figure 1.
Patient selection. ICU = intensive care unit; PNA = pneumonia; SNF = skilled nursing facility.
Table 1. Patient characteristics.
| Characteristic |
Historical control (n = 65) |
Pharmacist intervention (n = 43) |
| Mean age, years (range; SD) | 69 (24–89; 13.1) | 69 (49–100; 11.0) |
| Male | 34 (52) | 24 (56) |
| Risk factors, mean per patient (range; SD) | 2.3 (1–4; 1.0) | 2.0 (1–4; 0.9) |
| Admitted within 6 months | 40 (62) | 14 (33) |
| Months since admission, mean (range; SD) | 2.1 (1–5; 1.3) | 2.8 (1–6; 1.4) |
| ≥5 scheduled home medications | 58 (89) | 37 (86) |
| COPD | 28 (43) | 23 (53) |
| Heart failure | 21 (32) | 12 (28) |
| Health insurance | ||
| Medicare | 51 (78) | 38 (88) |
| BCBS | 39 (60) | 20 (47) |
| Self-pay | 6 (9) | 4 (9) |
| Other | 19 (29) | 6 (14) |
Note: All data are given as n (%) unless specified otherwise, and all percentages were rounded to the nearest whole number. BCBS = Blue Cross and Blue Shield; COPD = chronic obstructive pulmonary disease.
Study outcomes regarding readmissions are displayed in Table 2. A trend toward a reduced 30-day readmission rate was observed for the intervention group compared to the historical control that received usual care (27.9% vs 40.0%; RR, 0.6977; 95% CI, 0.3965–1.2278; P = .2119). There was not a considerable change in time to readmission between the groups (10.8 vs 10.6 days). The majority of reasons for readmission in the historical control were treatment failure or recurrence of pneumonia or another condition requiring hospitalization, which mainly consisted of COPD and heart failure exacerbations. A decreased percentage of treatment failure and recurrence of pneumonia, as well as documented nonadherence, was observed in the intervention group. The one ADE that was documented as contributing to readmission in the prospective group was Clostridium difficile–associated diarrhea (CDAD).
Table 2. Readmission outcomes in high-risk patients with pneumonia.
| Outcome |
Historical control (n = 65) |
Pharmacist intervention (n = 43) |
RR (95% CI)a |
| Readmission within 30 days | 26 (40) | 12 (28) | 0.6977 (0.3965–1.2278)b |
| Mean time from discharge to readmission, days (range; SD) | 10.6 (2–27; 7.6) | 10.8 (2–28; 8.2) | |
| Reasons for readmission | (n = 29) | (n = 14) | |
| Treatment failure | 12 (41) | 2 (14) | |
| Nonadherence | 4 (14) | 0 (0) | |
| Adverse drug event | 1 (4) | 1 (7) | |
| Other | 12 (41) | 11 (79) | |
Note: All data are given as n (%) unless specified otherwise, and all percentages were rounded to the nearest whole number.
Comparison using relative risk (RR).
P = .2119 (level of significance, P = .05).
There were 103 (2.4 per patient) errors identified during medication reconciliation, with the majority of errors relating to an incorrect dose or frequency or a medication being omitted from the home medication list (Table 3). All errors were identified following the medication reconciliation completed by nursing. There were 38 recommendations made regarding antibiotic therapy, which were all accepted by the provider. Changing the route of administration (ie, intravenous to oral) was the most common intervention followed by optimizing therapy. Optimizing therapy included making renal dose adjustments and recommending alternative regimens, particularly if a patient’s inpatient antibiotic regimen was similar to an outpatient regimen he or she had failed or if he or she had risk factors for a health care–associated infection. For the dischargecounseling component of the intervention, 91% of patients were discharged on antibiotics, and a majority of them (85%) were successfully counseled before discharge. Several patients also received counseling on their chronic medications if they were not aware of or misunderstood changes in their medications.
Table 3. Medication errors identified and pharmacist interventions.
| Intervention (n = 186) | n (%) |
| Medication reconciliation (n = 103) | |
| Incorrect dose or frequency | 49 (48) |
| Medication omitted | 33 (32) |
| Medication added | 14 (14) |
| Duplicate therapy | 4 (4) |
| Counseled on nonadherence | 3 (3) |
| Errors per patienta, mean | 2.4 |
| Therapeutic recommendations (n = 38) | |
| Route change | 29 (76) |
| Optimize therapy | 7 (18) |
| De-escalate therapy | 2 (5) |
| Discharge counseling (n = 45) | |
| Counseled on antibioticsb | 33 (73) |
| Counseled on chronic medication changes | 12 (27) |
Note: All data are given as n (%) unless specified otherwise, and all percentages were rounded to the nearest whole number.
n = 43 patients.
n = 39 patients were prescribed discharge antibiotics.
Only 49% of patients in the historical control and 47% in the intervention group had documentation of either a phone call attempt or referral by the institution’s home health department (Table 4). Consequently, over half of the patients in both groups were missed by the current system’s attempt to follow-up, whereas an attempt was made to call all of the patients in the intervention group and 91% of patients were successfully contacted. A total of 4 (9%) patients in the intervention group were not reached due to a phone number disconnection or no answer after 3 attempts. Per patient report and using insurance claims and pharmacy data, the initial prescription fill rate was 85%, and this rate increased to 92% after the pharmacist was able to reinforce adherence during the phone call. There was one patient who did not fill the prescription even after the phone call and was readmitted. Most of the ADEs identified were gastrointestinal in nature, thus the pharmacist reinforced the instructions to the patients to take the antibiotic therapy with food if applicable, stay hydrated, and finish the treatment course.
Table 4. Results from postdischarge interventions.
| Intervention |
Historical control (n = 65) |
Pharmacist intervention (n = 43) |
| Home health referrala | 26 (40) | 15 (35) |
| Home health follow-up phone call | 6 (9) | 5 (12) |
| Pharmacist follow-up phone call | —b | 39 (91) |
| No answer or number disconnected | — | 4 (9) |
| Antibiotic prescription initially filled (n = 39) | — | 33 (85) |
| Antibiotic prescription filled after pharmacist phone call (n = 39) | — | 36 (92) |
| Reason for not filling prescription (n = 6)c | ||
| No transportation | — | 2 (33) |
| No time yet | — | 1 (17) |
| Other/unknown | — | 3 (50) |
| Missed dosec | — | 3 (7) |
| Adverse drug event | — | 7 (16) |
| Gastrointestinal | — | 6 (86) |
| Other | — | 1 (14) |
Note: All data are given as n (%), and all percentages were rounded to the nearest whole number.
Patients who received a home health referral were excluded from the home health agency’s follow-up phone call list.
Not applicable.
Patients were counseled on nonadherence.
Discussion
This single-center pilot study highlights the impact pharmacists can have on transitions of care and readmission rates through interventions such as medication reconciliation, therapeutic recommendations, discharge education, and follow-up. Due to the nature and design of pilot studies, this study was not adequately powered to detect a significant reduction in readmission rates. However, the 30-day readmission rate was reduced from 40.0% in the usual care group to 27.9% in the intervention group. Therefore, it would be beneficial to further investigate this bundled intervention in a population identified to be at high risk for readmission in an adequately powered study.
The readmission rate observed for the usual care group is consistent with other high-risk populations in the literature.21,23–26 The literature pertaining to pharmacist interventions and their impact on readmission rates is more diverse, with inconsistent results in terms of significantly reducing readmissions. The majority of reasons for readmission in the retrospective usual care group were for treatment failure or recurrence of pneumonia (41%) and other conditions requiring hospitalization (41%). Only 14% of the documented reasons for readmission in the prospective intervention group were for treatment failure or recurrence of pneumonia and 79% were referring to another condition requiring hospitalization. This substantial shift may be reflective of pharmacist involvement and patients having a better understanding of medications and treatment plans.
Significant results have been observed with bundled interventions, although most of these programs require substantial resource investment.13–16 Significant results with an isolated intervention have only been observed in a high-risk population, inferring that this population will experience the greatest benefit with limited resources.5 While it is imperative to recognize the limitations of the existing literature, there have been some encouraging methods to reduce readmissions and improve transitions of care that warrant further investigation.5 It is crucial to identify cost-effective methods that utilize current resources to improve the quality of care and decrease health care expenditures.
Further analysis of standardized risk-stratification tools would be extremely valuable in targeting resources and funds to specific populations, as well as providing institutions with evidence-based approaches and implementation strategies. This study used inclusion criteria incorporating risk factors identified from previous reports (ie, multiple medications, comorbidities, and recent prior hospitalizations) in addition to those specifically recognized at our institution (ie, COPD and heart failure patients) to distinguish patients at higher risk for readmission.5,11,20–22 These criteria allowed for the utilization of available resources in a patient population in which we expect to see the greatest impact.5 Another strength of this study was its focus on one condition, which optimized the use of restricted resources while still providing guidance on the feasibility of implementing similar pharmacy services.
The design of the bundled intervention was also considered a strength, because it provided a continuity of care throughout each patient’s treatment. Multiple interactions and interventions at different times throughout care helped establish a relationship and a good rapport with the patient and other health care providers, which may have contributed to higher rates of adherence and follow-up phone call responses. For example, the initial prescription fill rate in the intervention group was found to be 85%, which is higher than the national average of 80%; it increased to 92% after the phone call component of the intervention.27 This finding may reflect the importance of persistence and accountability in transitions of care. In addition to obtaining a thorough and accurate medication history during medication reconciliation, there were also numerous instances during the process when patients disclosed medication nonadherence. This was another opportunity for the pharmacist to reinforce and explain the value of the medication and provide encouragement to become adherent.
Therapeutic recommendations provided an opportunity to introduce important aspects to the treatment assessment and plan such as recent antibiotic exposure and present risk factors for health care–associated pneumonia. Providing discharge counseling for antibiotic therapy also afforded the time to address chronic medication changes and answer any questions the patient had, which may have contributed to a successful transition home. There were several undocumented interventions during this time when unforeseen intercessions were made, such as addressing communication errors between physicians and patients, identifying incorrect or inappropriate dosing or regimens on written prescriptions, and fulfilling patient requests such as calling discharge antibiotic prescriptions into the pharmacy. Although some patients were discharged before counseling could be completed due to schedule constraints, an attempt was made to complete counseling via telephone. Furthermore, the follow-up phone call timeline (ie, 48 to 96 hours after discharge) offered the patients sufficient time to fill the prescription and for the pharmacist to address any side effects observed or concerns they had. Lastly, having one pharmacist perform all of the interventions helped limit confounders and standardize the process, although there was still risk for variability between patients.
There are also several limitations to discuss. First, this was a nonrandomized pilot study with a small sample size that can only provide insight into the feasibility of implementing a similar program or study.28 Due to the lack of access, only readmissions to our health system were captured, and therefore the readmission rates may be underestimated if patients were readmitted to another institution. Nonetheless, our health system serves 11 counties in West Alabama, which reduces the probability that this was a significant limitation. The primary investigator was completing a PGY1 residency at the time of this study, whereas similar interventions in the literature were carried out by at least one full-time equivalent pharmacist.18,21,23,29 This aspect may have limited the findings and collaboration with multiple disciplines epresentative of true transitional care, such as case management, social work, primary care providers, and community pharmacies. The historical control group had a greater percentage of patients with a prior hospitalization within 6 months, suggesting a potential greater baseline risk in this group. However, seasonal variation associated with hospitalizations may have contributed to this finding rather than significant differences in risk for readmission at baseline, because the groups were assessed during different periods of the year. Finally, the generalizability of this study may be somewhat restricted, because it was designed specifically for our institution.
This pilot study has provided several additional insights into future investigations. First, it has been observed that most patients screened had at least 5 medications (86% and 89%) and may not necessarily be at the highest risk for readmission. An increased number of scheduled medications (ie, 10 medications) or certain high-risk medications, such as anticoagulants and insulin, have been associated with a higher risk of readmission.21 To increase the selectivity of the highrisk population, it may be beneficial to target either an increased number or specific category of medications in future studies. This study, along with several other similar designs, excluded patients admitted to an ICU or focused on certain medical wards due to available resources.18,21,23 However, a majority of these patients would potentially be classified as high-risk for readmission given their critical illness and therefore may benefit from such an intervention. Similarly, we also excluded patients who were discharged to a skilled nursing facility, which included patients going to short-term rehabilitation, and they may have also benefited from the intervention. Lastly, the patients in this study received the institution’s computer-generated medication list, yet evidence shows the importance of appropriate literacy levels and physical appearance of a medication list for patient understanding.24
Health care reform has created several challenges, but it has also provided opportunities to improve the quality of care delivered to patients. To meet new health care measures, hospitals will need to expand operations outside their walls and create smoother transitions to the community, which the findings from this project highlight. There is more emphasis on reducing readmissions today than ever before, and participation from all providers of patient care will be needed to overcome this challenge. With medicationrelated events having a significant role in readmission statistics, pharmacist involvement is essential. By utilizing medication management expertise and concentrating on national quality indicators, pharmacists have a unique opportunity to demonstrate the value they provide to patients, providers, and organizations. Successful implementation of such services will help pharmacists define their worth in relatable terms to other health care providers and hospital administration. Improving the overall quality of care patients receive involves specialized efforts beyond the 30 days following discharge. Emphasizing one specific measure, such as 30-day readmission rates, may discount other important aspects of care and portrays a systemwide approach characteristic of reactive medicine versus preventative medicine. Providing safe and effective health care requires the combined efforts of the patients and their caregivers, medical institutions, and primary providers in every specialty.30
Conclusion
The results from this pilot study reveal that a pharmacist-specific bundled intervention, including medication reconciliation, therapeutic recommendations, patient discharge counseling, and a follow-up phone call, was associated with a reduced 30-day readmission rate for high-risk patients with pneumonia. With over 200 total interventions documented, there are numerous potential opportunities for increased pharmacist involvement in care. Allowing a pharmacist to dedicate time and effort to a highrisk patient population could demonstrate the value to maintain and expand services to other populations in the future, reduce health care costs, and ultimately benefit patient care.
Acknowledgments
The authors declare no conflicts of interest. The authors would like to thank Tom Wyatt, PhD, CPHQ, for his contributions to the study design and statistical analysis.
References
- 1.A path to bundled payment around a rehospitalization. In: Report to the Congress: Reforming the Delivery System. Washington, DC: Medicare Payment Advisory Commission; 2005:83–103. [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA, et al. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 3.Dartmouth Atlas Project (Goodman DC, Fisher ES, Chang CH, et al. ). Dartmouth Institute for Health Policy and Clinical Practice. The Revolving Door: A Report on U.S. Hospital Readmissions. Princeton: Robert Wood Johnson Foundation; 2013. [Google Scholar]
- 4.Centers for Medicare and Medicaid Services. Readmissions reduction program. August 2014. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html Accessed September17, 2014.
- 5.Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: A systematic review. Ann Intern Med. 2011;155:520–528. [DOI] [PubMed] [Google Scholar]
- 6.Forster AJ, Murff HJ, Peterson JF, et al. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20(4):317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davies EC, Green CF, Mottram DR, et al. Emergency re-admissions to hospital due to adverse drug reactions within 1 year of the index admission. Br J Clin Pharmacol. 2010;70(5):749–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Budnitz DS, Lovegrove MC, Shehab N, et al. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365:2002–2012. [DOI] [PubMed] [Google Scholar]
- 9.Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: An analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25(5):441–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erickson J. The cost of medication noncompliance. J Am Assoc Preferred Provider Organ. 1993:3(2):33–34, 38–40. [PubMed] [Google Scholar]
- 11.Coleman EA, Smith JD, Raha D, et al. Posthospital medication discrepancies: Prevalence and contributing factors. Arch Intern Med. 2005;165:1842–1847. [DOI] [PubMed] [Google Scholar]
- 12.Makaryus AN, Friedman EA. Patients understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991–994. [DOI] [PubMed] [Google Scholar]
- 13.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann Intern Med. 2009;150(3):178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boutwell A, Jencks S, Nielsen GA, Rutherford P. State Action on Avoidable Rehospitalizations (STAAR) Initiative: Applying Early Evidence and Experience in Front-Line Process Improvements to Develop a State-Based Strategy. Cambridge, MA: Institute for Healthcare Improvement; 2009. [Google Scholar]
- 15.Coleman EA, Parry C, Chalmers S, Min SJ. The Care Transitions Intervention results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828. [DOI] [PubMed] [Google Scholar]
- 16.Society of Hospital Medicine. Project Better Outcomes for Older adults through Safe Transitions (BOOST). 2008. http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm Accessed August5, 2013.
- 17.Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166(5):565–571. [DOI] [PubMed] [Google Scholar]
- 18.Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: A randomized controlled trial. Arch Intern Med. 2009;169(9):894–900. [DOI] [PubMed] [Google Scholar]
- 19.Vinks TH, Egberts TC, de Lange TM, de Koning FH. Pharmacist-based medication review reduces potential drug related problems in the elderly: The SMOG controlled trial. Drugs Aging. 2009;26(2):123–133. [DOI] [PubMed] [Google Scholar]
- 20.Walker PC, Bernstein SJ, Jones JN, et al. Impact of a pharmacist-facilitated hospital discharge program: A quasiexperimental study. Arch Intern Med. 2009;169:2003–2010. [DOI] [PubMed] [Google Scholar]
- 21.Pal A, Babbot S, Wilkinson ST, et al. Can the targeted use of a discharge pharmacist significantly decrease 30-day readmissions? Hosp Pharm. 2013;48(5):380–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greenwald JL, Jack BW. Preventing the preventable. Prof Case Manag. 2009:14(3):135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4:211–218. [DOI] [PubMed] [Google Scholar]
- 24.Root R, Phelps P, Brummel A, et al. Implementing a pharmacist-led medication management pilot to improve care transitions. Innov Pharm. 2012;3(2):article 75. [Google Scholar]
- 25.Kirkham HS, Clark BL, Paynter J, et al. The effect of a collaborative pharmacist–hospital care transition program on the likelihood of 30-day readmission. Am J Health Syst Pharm. 2014;71:739–745. [DOI] [PubMed] [Google Scholar]
- 26.Stewart S, Pearson S, Horowitz JD. Effects of a homebased intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med. 1998;158:1067–1072. [DOI] [PubMed] [Google Scholar]
- 27.Langer Research Associates. Medication adherence in America: A national report card. National Community Pharmacists Association. June 2013. http://www.ncpanet.org/pdf/reportcard/AdherenceReportCard_Full.pdf Accessed March 2, 2014.
- 28.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gattis WA, Hasselblad V, Whellan DJ, et al. Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team. Arch Intern Med. 1999;159:1939–1945. [DOI] [PubMed] [Google Scholar]
- 30.Institute for Safe Medication Practices (ISMP). Reduce readmissions with pharmacy programs that focus on transitions from the hospital to the community. ISMP Medication Safety Alert. November 201). http://www.medscape.com/viewarticle/778965_1 Accessed July15, 2013.