Abstract
Background
Maintaining robust perfusion is an important physiologic parameter in wound healing. The effect of different closure techniques on wound perfusion after total knee arthroplasty (TKA) has not been established previously and may have implications for wound healing.
Questions/purposes
We asked whether a running subcuticular, vertical mattress, or skin staple closure technique enables the most robust wound perfusion after TKA as measured by laser-assisted indocyanine green angiography (LA-ICGA) in patients without specific risk factors for wound healing complications.
Methods
Forty-five patients undergoing primary TKA without comorbidities known to impact wound healing and perfusion were prospectively randomized to receive superficial skin closure with one of the following techniques: (1) running subcuticular (3-0 monofilament); (2) vertical mattress (2-0 nylon); or (3) skin staples. Twenty procedures were performed by RTT, 15 by RJS, and 10 by FHS. All surgeons used an anterior skin incision over the medial third of the patella in combination with a median parapatellar arthrotomy. Perfusion was assessed with a LA-ICGA device and software system immediately after closure to quantify fluorescence. Twenty-seven points were assessed immediately after closure in the operating room in each patient (nine along the incision and nine pairs medial and lateral to the incision). Mean incision perfusion was determined from the nine points along the incision with higher values indicating greater blood flow. Mean perfusion impairment was determined by calculating the difference between the nine pairs of surrounding skin and the nine points along the incision with smaller values indicating less perfusion impairment. These parameters were compared with analysis of variance (ANOVA) and subsequent pairwise comparisons with an unadjusted analysis as well as a multivariate analysis that adjusted for age, sex, and body mass index. Patients were followed for a mean of 7 months after surgery (range, 3–12 months) for possible incision-related complications. No patents were lost to followup.
Results
Running subcuticular closure demonstrated the best overall perfusion. Mean incision perfusion in fluorescent units with SD was as follows: running subcuticular, 64 (16); vertical mattress, 32 (18); and staples, 19 (7) (ANOVA p < 0.001). The running subcuticular closure demonstrated the least impairment of perfusion among the closures compared. Mean perfusion impairment was as follows: running subcuticular, 21 (12); vertical mattress, 37 (24); and staples, 69 (27) (ANOVA p < 0.001). All Tukey-adjusted pairwise comparisons from both metrics likewise favored the subcuticular closure (p < 0.001) both before and after adjusting for age, sex, and body mass index. One patient in the vertical mattress cohort experienced a surgical site infection; no other wound-related complications were observed in this study.
Conclusions
The method of closure can influence skin and soft tissue perfusion after TKA. Running subcuticular closure enables the most physiologic robust blood flow, which may improve wound healing. However, the clinical importance of these findings remains uncertain, because patients in this study were selected because they lacked risk factors for wound healing complications. Studies with this modality in specific patient populations at higher risk for wound complications will be necessary to quantify the clinical advantage of using running subcuticular closure.
Level of Evidence
Level I, therapeutic study.
Introduction
Multiple studies have compared different closure techniques in TKA [2, 3, 6, 15–18]. The majority of these studies have involved running subcuticular closure versus staple closure and focused on factors such as cost, performance time, patient satisfaction, and wound complications. Results have varied based on the characteristics studied and to date there is no consensus on a superior wound closure technique for TKA. The number of TKAs performed each year is on the rise, and a greater percentage of these patients have comorbidities that can impair wound healing such as diabetes, a history of smoking, previous surgery about the knee, chronic infection, peripheral arterial disease, and anticoagulant or corticosteroid use [7–9, 14]. These comorbidities in conjunction with relatively thin skin anterior to the knee makes wound complications an issue of growing concern [19, 20].
Maintaining robust perfusion at the incision site is one of the most important physiologic parameters in wound healing [1, 5, 14]. Therefore, the closure technique should theoretically have an impact on prevention of wound complications through differential promotion of perfusion. To date, no study has adequately determined which closure technique enables the most robust perfusion in TKA. One investigation attempted to describe differences in blood content and wound oxygenation between staple and running subcuticular closure in TKA with the use of tissue spectrophotography [3]. This technology has limitations because it only obtains a static view of blood in soft tissue and is influenced more by blood pooling than perfusion status.
Laser-assisted indocyanine green angiography (LA-ICGA) is a technology that has been used in a variety of specialties but most prominently in plastic surgery over the past decade [4, 10, 11, 13, 22]. Through the intravenous administration of the plasma protein-bound indocyanine green (ICG) dye, an external camera can detect the specific frequency of the dye and thus track perfusion to skin and soft tissues in real time. The dynamic view of blood flow made possible by this technology has recently been shown to improve management of wound closure in complex knee reconstruction [21]. This device is also capable of quantifying perfusion, which provides an opportunity for a novel approach to define which closure technique affords the most robust perfusion in TKA.
We therefore asked whether a running subcuticular, vertical mattress, or skin staple closure technique enables the most robust wound perfusion after TKA as measured by LA-ICGA in patients without specific risk factors for wound healing complications.
Patients and Methods
This prospective, randomized clinical trial was initiated in August 2013 after obtaining institutional review board approval and registering the study with www.clinicaltrials.gov (NCT01924403). Recruitment and patient evaluation took place at one center among three surgeons (RTT, RJS, FHS) from August 2013 to May 2014 with a minimum clinical followup of 3 months (mean, 7 months; range 3–12 months).
Patients presenting for a presurgical TKA consultation were approached by a study coordinator for potential enrollment the day before their procedure. They were informed that participation would entail randomization of their wound closure to a running subcuticular, vertical mattress, or staple technique with subsequent intraoperative LA-ICGA imaging. Inclusion criteria were patients aged ≥ 18 years undergoing primary TKA. Exclusion criteria were previous surgery about the knee and therefore a previous incision, a history of smoking within 1 year, diabetes mellitus (Type I and II), peripheral arterial disease, long-term corticosteroid use (≥ 1 month; intranasal and inhaled excluded), long-term anticoagulation use (≥ 1 month; low-dose aspirin excluded), infection (HIV, syphilis, hepatitis), and iodine allergy (contraindication to LA-ICGA). With the exception of iodine allergy, all exclusion criteria were chosen with the intent of removing factors that could impede blood flow and wound healing and therefore confound results. These criteria allowed for stringent experimental isolation of closure type as the primary variable impacting wound perfusion. It was decided a priori to enroll 45 eligible patients with an equal number randomly allocated to each treatment arm for a total of 15 patients per intervention. A power analysis was not performed before the initiation of this study as a result of lack of available data to effectively estimate sample size. Therefore, the sample size was determined based on feasibility of enrollment and budgetary constraints and with the understanding that this would serve as an initial investigation to help determine effect size for future studies.
A strategy of random allocation permuted-block randomization was used to ensure that 1:1:1 allocation (15 patients per treatment arm) was achieved for the desired enrollment of 45 patients and for treatment arm allocation among the three participating surgeons. Twenty procedures were performed by RTT, 15 by RJS, and 10 by FHS. Fifteen minutes before the initiation of wound closure, a concealed envelope was opened by the study coordinator and the closure type was called into the operating room. However, it was not possible for either the patient or the surgeon to remain blinded after the operation as a result of the obvious visible differences of each closure method. Quantitative imaging of wound perfusion was performed immediately after closure in the operating room.
All surgeons used an anterior skin incision over the medial third of the patella in combination with a median parapatellar arthrotomy. The length of these incisions was determined based on patient size and extended as necessary to provide adequate access for the procedure. Each closure was performed identically to the extent possible in three layers as follows. All patients received closure of the arthrotomy and deep fascia with 0-Vicryl (Ethicon, Cincinnati, OH, USA) applied in a simple interrupted fashion. Furthermore, each patient received closure of the subcutaneous layer with 2-0 Monocryl (Ethicon) also applied in a simple interrupted fashion. The superficial skin wound closure differed based on treatment assignment. One group received 3-0 Monocryl (Ethicon) applied with a running subcuticular technique. The second group received superficial closure with 2-0 nylon suture (Ethicon) applied with a vertical mattress technique. The final group received superficial closure with PROXIMATE fixed-head skin staples (Ethicon).
Postoperative care protocols and instructions were identical for all patients per institutional norms regardless of closure type. The 2-0 nylon sutures or staples were removed at approximately the 2-week clinical followup appointment as indicated. The incision site was checked for any complications at all followup appointments through a minimum of 3 months after surgery. Patients were also encouraged to contact the surgical team if they had any concerns about their wound or general rehabilitation course per institutional protocol.
LA-ICGA Imaging System
The SPY Elite® fluorescent imaging system (Lifecell Corporation, Branchburg, NJ, USA) used in this clinical trial to assess perfusion of soft tissues in the orthopaedic setting has been previously described [21]. Briefly, the LA-ICGA system uses an imaging head with a charge-coupled device camera and a laser light source, functioning at a 40 mW/cm2 power density (Fig. 1) [21].
Fig. 1.

This photograph displays the LA-ICGA system used in this investigation to quantitatively measure wound perfusion in real time. With kind permission from Springer Science + Business Media:[21]
The LA-ICGA camera recognizes a peak waveform in the range from 800 to 810 nm, thus excluding nonspecific signal. Indeed, ICG emits this exact frequency in blood after intravenous administration. To obtain accurate measurements, all dressings are removed from the skin before imaging and the camera is sterilely draped. The anesthesiologist pushes a 5-cc bolus of dye followed by a 10-cc saline flush. After this step, the operating room lights must be immediately shut off to reduce background signal to the camera [12]. ICG takes approximately 15 seconds to reach the knee after infusion in the antecubital fossa. On perfusion initiation, a scaled black and white real-time 120-second video is produced with darker areas representing lower perfusion and brighter zones indicating higher perfusion [21].
Incision Fluorescence Measurement
Typically, the intensity of fluorescence rapidly increases for approximately 15 to 20 seconds during the arterial phase of perfusion and then slowly decreases over the course of an additional 20 to 30 seconds to a plateau where the arterial and venous phases of perfusion have reached equilibrium. This fluorescence plateau is maintained for approximately 45 seconds until the signal begins to slowly fade secondary to decay of the ICG. The LA-ICGA fluorescence software graphs this waveform to facilitate identification of views at specific time points. In recognition of this waveform, data were collected at two time points. The first was at the point of maximum fluorescence during the arterial phase (normally between 15 and 20 seconds into recording), which we defined as “peak perfusion.” The second set of data points was always collected 70 seconds into the video recording. Discussions with Lifecell representatives and a plastic surgeon at our institution with extensive experience with the LA-ICGA system (SRJ) affirmed that the 70-second time point has the highest probability of capturing the plateau phase of fluorescence where the arterial and venous phases of perfusion are in equilibrium (data not shown). We defined this point as “baseline perfusion” and at 70 seconds into the video recording, all 45 of our cases were in the plateau phase. Baseline perfusion was our primary outcome measure and peak perfusion was our secondary outcome measure.
The LA-ICGA system used in this investigation is capable of quantifying the brightness of up to 27 points simultaneously on a scale from 0 to 255 fluorescent units [12]. At peak perfusion, nine points were collected along the incision, each 1 cm apart. In addition, nine pairs of points were collected 1 cm medial and lateral to the nine points along the incision for a total of 27 points. These same 27 points were collected at baseline perfusion (Fig. 2). The fluorescence data points were always collected by the lead study coordinator (CCW) and confirmed for accuracy by another study team member (MTH).
Fig. 2A–L.
This compilation demonstrates the images obtained by the LA-ICGA system at peak perfusion and baseline perfusion in three study patients. Lighter areas are receiving more blood flow than darker zones, thus qualitatively demonstrating that running subcuticular enables the greatest perfusion, vertical mattress is intermediate, and staples provide the poorest outcome. Also shown are the 27 points that were quantified with nine points along the incision and nine pairs that were 1 cm medial and lateral to the incision. (A) A running subcuticular closure at peak perfusion. (B) A running subcuticular closure at peak perfusion with quantitation. (C) A vertical mattress closure at peak perfusion. (D) A vertical mattress closure at peak perfusion with quantitation. (E) A staple closure at peak perfusion. (F) A staple closure at peak perfusion with quantitation. (G) A running subcuticular closure at baseline perfusion. (H) A running subcuticular closure at baseline perfusion with quantitation. (I) A vertical mattress closure at baseline perfusion. (J) A vertical mattress closure at baseline perfusion with quantitation. (K) A staple closure at baseline perfusion. (L) A staple closure at baseline perfusion with quantitation.
Outcome Measures
For both baseline perfusion and peak perfusion, two coprimary metrics were quantified. The first outcome was the mean incision perfusion, defined as the mean of the nine fluorescent points along the incision. This metric is aimed at quantifying absolute perfusion to the incision; thus, higher values indicate more robust perfusion. The second outcome was the mean perfusion impairment, defined as the difference between the average of the nine medial and lateral pairs of surrounding skin and the nine points along the incision. This metric is aimed at quantifying perfusion to the incision relative to undisturbed surrounding skin, thus controlling for global differences in perfusion to the knee between patients. For mean perfusion impairment, smaller values indicate less perfusion impairment and thus more robust blood flow secondary to the wound closure. Pairwise comparisons were made for mean incision perfusion at both baseline perfusion and peak perfusion. The metric reported is the difference in mean incision perfusion with 95% confidence intervals (CIs) and p values. Pairwise comparisons were also made for mean perfusion impairment at both baseline perfusion and peak perfusion. The metric reported is the difference in mean perfusion impairment with 95% CI and p values.
The analysis focused on comparing the three wound closure techniques (running subcuticular, vertical mattress, and staple, as noted previously) with respect to the coprimary outcomes (mean incision perfusion and mean perfusion impairment at baseline perfusion, as described previously); separate analyses were performed for mean incision perfusion and mean perfusion impairment. This analytic strategy was also carried out for the cosecondary outcomes of mean incision perfusion and mean perfusion impairment at peak perfusion. The analysis was conducted using one-way analysis of variance (ANOVA) with either mean incision perfusion or mean perfusion impairment as the dependent variable and closure technique (three levels) as the independent variable. When the global F-test from the ANOVA was statistically significant, further analysis was undertaken by performing pairwise comparisons among the three wound closure techniques using the Tukey method for multiple comparisons to control the overall Type I error rate. For both the ANOVA tests and Tukey-adjusted pairwise comparisons, a p value < 0.05 was considered significant. Additional multivariate regression models were generated that included age, sex, and body mass index (BMI) as adjusting covariates. All analyses were conducted using SAS Version 9.2 (SAS Institute, Inc, Cary, NC, USA) and R Version 3.0.1 (R Development Core Team, Boston, MA, USA; 2011).
Demographics and Description of Study Population
The baseline demographic characteristics of age, gender, and BMI were well balanced among the three treatment arms, supporting the effectiveness of the randomization process (Table 1). None of the patients had any of the wound healing comorbidities outlined in the exclusion criteria; however, 17 of the 45 patients had a remote history of smoking (> 1 year before surgery) (Table 1). Only one patient experienced a wound complication, which was a superficial site infection (SSI) from the vertical mattress cohort (Table 1).
Table 1.
Summary of patient demographics*
| Patient cohort | Age (years) | Sex | Body mass index (kg/m2) | Wound healing comorbidities | Wound complications |
|---|---|---|---|---|---|
| Overall patient cohort (n = 45) | 70 (42–88) | 30 women, 15 men | 33 (23–60) | 0 (17) | 1 (SSI) |
| Running subcuticular (n = 15) | 71 (53–88) | 12 women, 3 men | 33 (25–50) | 0 (7) | 0 |
| Vertical mattress (n = 15) | 70 (56–86) | 8 women, 7 men | 31 (23–42) | 0 (6) | 1 (SSI) |
| Skin staple (N = 15) | 69 (42–85) | 10 women, 5 men | 36 (23–60) | 0 (4) | 0 |
* Wound healing comorbidities included previous surgery about the knee, diabetes mellitus, history of smoking within the previous year, peripheral arterial disease, chronic or recent infection, long-term or recent anticoagulation (aspirin excluded), long-term or recent steroid use (intranasal and inhaled excluded); numbers for age and body mass index are reported as means with ranges; sex and wound complications are reported as total counts; wound healing comorbidities are reported as total counts with number of former smokers in parentheses; SSI = superficial site infection.
Eighty-five patients presenting for primary TKA between August 2013 and May 2014 were prescreened for eligibility by chart review of the medical record. Fifty-five of these patients met all eligibility criteria and were approached for potential consent. Nine patients refused to participate leaving 46 patients who were enrolled. One patient was excluded on the day of surgery because of a metal allergy precluding them from receiving staples should they have been randomized to that closure.
Patients were followed clinically for the development of any wound complications as part of routine care. Minimum followup was 3 months after surgery and mean followup was 7 months (range, 3–12 months). There was no loss to followup in this study.
Results
Running subcuticular closure afforded the most robust baseline perfusion, vertical mattress closure was intermediate, and staple closure yielded the poorest blood flow (Table 2). The ANOVA global test for significance and all Tukey-adjusted pairwise comparisons supported these relationships with and without multivariate adjustment for age, sex, and BMI (p < 0.001; Table 2). For mean incision perfusion, larger values indicate greater blood flow to the incision. Baseline mean incision perfusion in fluorescent units with SD was as follows: running subcuticular, 64 (16); vertical mattress, 32 (18); and staple, 19 (7). For mean perfusion impairment, smaller values indicate greater blood flow to the incision. Baseline mean perfusion impairment in fluorescent units with SD was as follows: running subcuticular, 21 (12); vertical mattress, 37 (24); and staple, 69 (27) (Table 2).
Table 2.
Baseline perfusion by wound closure technique
| Outcome | Group | Number | Mean (SD*) | p value† | Pairwise comparisons‡ |
|---|---|---|---|---|---|
| MIP | Staple | 15 | 19 (7) | Running subcuticular versus staple (DMIP = 45.0; 95% CI, 32.1–57.9; p < 0.001) | |
| Vertical mattress | 15 | 32 (18) | < 0.001 | Running subcuticular versus vertical mattress (DMIP = 32.0; 95% CI, 19.1–45.0; p < 0.001) | |
| Running subcuticular | 15 | 64 (16) | Vertical mattress versus staple (DMIP = 13.0; 95% CI, 0.0–25.9; p = 0.05) | ||
| Staple | 15 | 19 (4)§ | Running subcuticular versus staple (DMIP = 41.1; 95% CI, 28.2–54.0; p < 0.001) | ||
| Vertical mattress | 15 | 29 (4)§ | < 0.001 | Running subcuticular versus vertical mattress (DMIP = 31.0; 95% CI, 18.6–43.5; p < 0.001) | |
| Running subcuticular | 15 | 60 (4)§ | Vertical mattress versus staple (DMIP = 10.1; 95% CI, 2.7–22.9; p = 0.15) | ||
| MPI | Staple | 15 | 69 (27) | Staple versus running subcuticular (DMPI = 48.0; 95% CI, 28.6–67.4; p < 0.001) | |
| Vertical mattress | 15 | 37 (24) | < 0.001 | Staple versus vertical mattress (DMPI = 31.7; 95% CI, 12.3–51.1; p < 0.001) | |
| Running subcuticular | 15 | 21 (12) | Vertical mattress versus running subcuticular (DMPI = 16.4; 95% CI, −3.1 to 35.8; p = 0.11) | ||
| Staple | 15 | 71 (6)§ | Staple versus running subcuticular (DMPI = 54.1; 95% CI, 34.3–73.9; p < 0.001) | ||
| Vertical mattress | 15 | 34 (6)§ | < 0.001 | Staple versus vertical mattress (DMPI = 36.5; 95% CI, 16.8–56.1; p < 0.001) | |
| Running subcuticular | 15 | 17 (6)§ | Vertical mattress versus running subcuticular (DMPI = 17.6; 95% CI, −1.5 to 36.7; p = 0.08) |
* Value listed for adjusted means is the SE; †analysis of variance p value; ‡individual pairwise comparisons with difference of means (either DMIP or DMPI), 95% CI for difference in means, and p values based on the Tukey method to guard against an increased Type I error probability resulting from multiple comparisons; §mean and SE adjusted for age, gender, and body mass index; MIP = mean incision perfusion; MPI = mean perfusion impairment; DMIP = difference in mean incision perfusion; DMPI = difference in mean perfusion impairment; CI = confidence interval.
Peak perfusion measurements likewise demonstrated running subcuticular closure afforded the most robust perfusion, vertical mattress closure was intermediate, and staple closure yielded the poorest blood flow (Table 3). The ANOVA global test for significance and all Tukey-adjusted pairwise comparisons supported these relationships with and without multivariate adjustment for age, gender, and BMI (p < 0.001; Table 3). Peak mean incision perfusion in fluorescent units with SD was as follows: running subcuticular, 78 (33); vertical mattress, 35 (20); and staple, 33 (12) (Table 3). Peak mean perfusion impairment in fluorescent units with SD was as follows: running subcuticular, 80 (29); vertical mattress, 83 (37); and staple, 123 (38) (Table 3).
Table 3.
Peak perfusion by wound closure technique
| Outcome | Group | Number | Mean (SD*) | p value† | Pairwise comparisons‡ |
|---|---|---|---|---|---|
| MIP | Staple | 15 | 33 (12) | Running subcuticular versus staple (DMIP = 45.2; 95% CI, 24.6–65.7; p < 0.001) | |
| Vertical mattress | 15 | 35 (20) | < 0.001 | Running subcuticular versus vertical mattress (DMIP = 42.5; 95% CI, 21.9–63.1; p < 0.001) | |
| Running subcuticular | 15 | 78 (33) | Vertical mattress versus staple (DMIP = 2.6; 95% CI, −18.0 to 23.2; p = 0.95) | ||
| Staple | 15 | 34 (6)§ | Running subcuticular versus staple (DMIP = 41.4; 95% CI, 19.3–63.6; p < 0.001) | ||
| Vertical mattress | 15 | 33 (6)§ | < 0.001 | Running subcuticular versus vertical mattress (DMIP = 42.0; 95% CI, 20.7–63.3; p < 0.001) | |
| Running subcuticular | 15 | 75 (6)§ | Staple versus vertical mattress (DMIP = 0.6; 95% CI, −21.3 to 22.6; p = 0.998) | ||
| MPI | Staple | 15 | 123 (38) | Staple versus running subcuticular (DMPI = 42.2; 95% CI, 11.2–73.2; p = 0.005) | |
| Vertical mattress | 15 | 83 (37) | 0.003 | Staple versus vertical mattress (DMPI = 39.8; 95% CI, 8.8–70.9; p = 0.009) | |
| Running subcuticular | 15 | 80 (29) | Vertical mattress versus running subcuticular (DMPI = 2.4; 95% CI, −28.6 to 33.4; p = 0.98) | ||
| Staple | 15 | 124 (10)§ | Staple versus running subcuticular (DMPI = 47.0; 95% CI, 13.6–80.5; p = 0.004) | ||
| Vertical mattress | 15 | 80 (10)§ | 0.002 | Staple versus vertical mattress (DMPI = 43.9; 95% CI, 10.7–77.1; p = 0.007) | |
| Running subcuticular | 15 | 77 (10)§ | Vertical mattress versus running subcuticular (DMPI = 3.1; 95% CI, −29.1 to 35.4; p = 0.97) |
* Value listed for adjusted means is the SE; †analysis of variance p value; ‡individual pairwise comparisons with difference of means (either DMIP or DMPI), 95% CI for difference in means, and p values based on the Tukey method to guard against an increased Type I error probability resulting from multiple comparisons; §mean and SE adjusted for age, gender, and body mass index; MIP = mean incision perfusion; MPI = mean perfusion impairment; DMIP = difference in mean incision perfusion; DMPI = difference in mean perfusion impairment; CI = confidence interval.
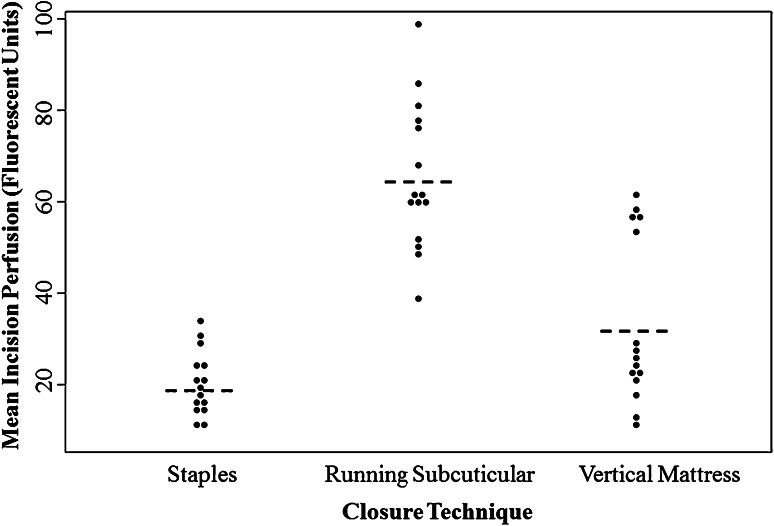
The consistency of incision perfusion differed by closure technique. The staple and running subcuticular closures followed a normal distribution; however, the vertical mattress closures were bimodal (Fig. 3). Ten of the vertical mattress closures had relatively low blood flow with a baseline mean incision perfusion of 20 (range, 9–27). The other five vertical mattress closures had relatively high blood flow with a baseline mean incision perfusion of 56 (range, 52–60) (Fig. 3).
Fig. 3.
This jit plot demonstrates mean incision perfusion at baseline by closure technique for all 45 patients in the study. Running subcuticular closure afforded the most robust perfusion, vertical mattress closure was intermediate, and staple closure resulted in the least blood flow to the incision site. Staple closure and running subcuticular closure followed a normal distribution; however, vertical mattress closure demonstrated a clear bimodal pattern. Five patients in this category obtained mean incision perfusion values similar to running subcuticular closure and the other 10 patients had mean incision perfusion values similar to staple closure. The horizontal bars represent the mean of the 15 patients for each respective closure technique.
With the numbers available and lack of baseline comorbidities in the cohort, there were no differences in clinically evident wound complications. One patient in the vertical mattress cohort experienced a surgical site infection; no other wound-related complications were observed in this study. There were also no significant differences in any of the reported quantitative outcomes after stratifying the results by surgeon.
Discussion
Many studies have previously compared wound closure techniques in TKA [2, 3, 6, 15–18]. Results have been highly variable and currently there is no consensus on a superior closure method. Physiologically, the most important modifiable factor in wound healing is maintenance of perfusion to the incision site [1, 5, 14, 19]. Therefore, it would be beneficial to know how the closure technique modifies this parameter. Recently, LA-ICGA has come into favor with plastic surgeons as a novel modality for defining skin and soft tissue perfusion that is dynamic, precise, and real time [4, 10, 11, 13, 22]. This technology has been described in one report to be advantageous in the management of wound closure for complex knee reconstructions, demonstrating the proof of concept for translatability to the current clinical question [21]. Although all previous studies to date have only used the qualitative functions of LA-ICGA, this system is also capable of quantifying blood flow, thus representing the best current technology for studying skin and soft tissue perfusion [12]. The aim of this randomized clinical trial was to quantitatively compare differences in perfusion among running subcuticular, vertical mattress, and staple closure in patients without specific risk factors for wound healing complications undergoing TKA as measured by a LA-ICGA device.
This study had a number of limitations. First, perfusion was only captured at the time of wound closure because analysis at later time points was too logistically cumbersome. Therefore, we cannot make conclusions about how perfusion may have been influenced by closure technique at later stages in the wound healing process or how it changes with knee flexion and extension. However, wound perfusion as it pertains to closure technique is driven by structural qualities that would not be expected to change substantially as the patient heals. Second, we could not comment on differences in the frequency of wound complications because only one patient from the vertical mattress cohort experienced a SSI. This study was not powered to detect differences in wound complications nor was that a primary aim. The choices for eligibility criteria allowed for the most robust experimental isolation of closure technique as the factor impacting perfusion status. Third, this study involves the first-time use of a technology, namely the quantitative function of an LA-ICGA device in orthopaedic surgery. Previous attempts at this type of investigation have been limited by feasibility, cost, poor quality of data, or static nature of perfusion assessment [3, 22]. The LA-ICGA used in this study overcame all of these challenges with a quantitative software interface that has been validated by the design engineers [12]. Fourth, we were not able to standardize all aspects of the surgical technique between surgeons or between patients. All surgeons did use an anterior skin incision over the medial third of the patella, median parapatellar arthrotomy, and three-layer closure as described earlier. Patient-specific factors necessitated individualized incision lengths and subfascial dissection to optimize the procedure. Nevertheless, no differences were observed in our quantitative outcomes after stratifying the results by surgeon. Finally, this randomized clinical trial was not powered a priori secondary to a lack of preliminary data or literature precedent for expected values of fluorescent units. Therefore, 45 patients were chosen for enrollment based on feasibility of completion for this preliminary study. Nevertheless, the results obtained were consistent and statistically significant in differentiating perfusion by closure technique. What remains unknown is the clinical importance of these results. However, given the paramount nature of perfusion status to adequate wound healing, it may be reasonable to consider that any difference in perfusion is clinically advantageous, perhaps more so in patients at risk of wound healing complications.
Many studies have compared different closure techniques in TKA [2, 3, 6, 15–18]. From the perspective of wound complications, one recent meta-analysis by Smith et al. showed that staple closure resulted in increased rates of infection after both hip and knee arthroplasty in comparison to running subcuticular [17]. Presumably, perfusion status is the most important factor in determining wound healing, yet the impact of closure technique on perfusion status has not been adequately studied [1, 5]. Graham et al. attempted to answer this question by performing a trial of 10 patients receiving staples after TKA versus 10 receiving running subcuticular closure; the status of wound healing comorbidities was undisclosed [3]. Using tissue spectrophotography, blood and oxygen content at the wound site was quantified preoperatively as well as at Days 3 and 7 postoperatively. This study found greater tissue blood content in running subcuticular closure when compared with staples spaced ≤ 6 mm apart, but found the greatest blood content in staples spaced > 6 mm apart [3]. These results are difficult to interpret because spectrophotography provides a static view of blood that is influenced more by blood pooling rather than by actual perfusion. By contrast, our study used a technology capable of precisely measuring dynamic blood flow in real time. Furthermore, we were able to demonstrate the perfusion status during both the arterial phase and during equilibrium between the arterial and venous phases of perfusion. The patient cohort was selected based on rigid criteria to exclude wound healing comorbidities in addition to randomization, which experimentally isolated closure technique as the primary factor influencing wound perfusion. The quantified metrics provided by the LA-ICGA technology make these results the most substantial to date in identifying perfusion characteristics of wound closure technique in TKA.
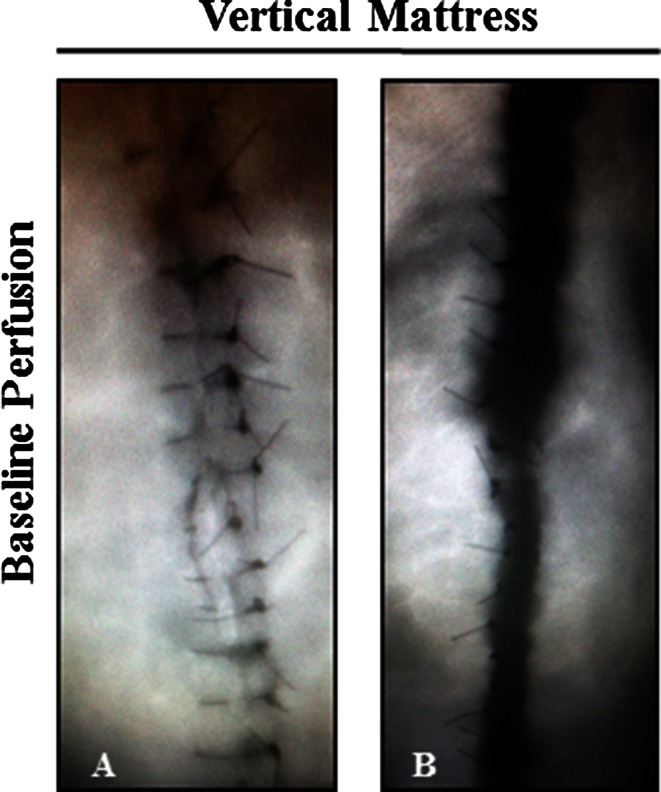
In this trial, running subcuticular and staple closure demonstrated consistent levels of perfusion. By contrast, vertical mattress closure showed a bimodal distribution of perfusion levels. We attribute these results to the operator dependency of each technique. Staple closure is the least dependent on technique, thus leading to the most reproducible, albeit poor outcome. Running subcuticular closure requires more skill but still provides a reproducible outcome because tension is applied parallel to the wound. Vertical mattress closure is the most operator-dependent technique because it relies on tension applied perpendicular to the incision. Perfusion was more variable from patient to patient and stitch to stitch in the vertical mattress closures, giving further credence to the influence of operator-dependent tension (Fig. 4). Vertical mattress closure has a place in many practices for complex reconstruction; however, results from this trial may caution surgeons to apply gentle tension for these closures.
Fig. 4A–B.
These images show examples of differential outcomes with vertical mattress closure. (A) This image shows a vertical mattress closure in a patient that resulted in high perfusion at baseline. (B) This image shows a vertical mattress closure in a different patient that resulted in low perfusion at baseline.
Most patients receiving primary TKA who have no particular risk factors for wound healing complications will likely go on to heal their incisions without incident regardless of closure technique. This clinical trial was not powered with the hundreds to thousands of patients that would be necessary to perform an outcomes and complications study with appropriate blocking for comorbidities. Instead, we chose to experimentally isolate closure method as a primary factor influencing perfusion and determined physiologic superiority of the running subcuticular technique. Because adequacy of blood flow is a primary biological determinant in wound healing, these results could hold importance for decreasing the incidence of wound complications in patients receiving TKA, especially revision cases and those with underlying wound healing comorbidities.
Many surgeons in our practice have subsequently changed their closure technique to running subcuticular. Those who have transitioned still consider vertical mattress an important option in select cases in which the wound is under high strain and needing structural reinforcement; however, only the minimum suture tension necessary is applied and LA-ICGA is often used at the end of these cases to document adequate perfusion and revise stitches as necessary. This study also provides additional support for the use of the LA-ICGA modality to examine skin perfusion in orthopaedic procedures about the knee with a higher potential of wound complications.
Acknowledgments
We thank Peter L. Bos PA-C, German A. Norambuena MD, and Lori J. McGowan PA-C, for their notable effort in patient enrollment; the entire orthopaedic surgery nursing team at Rochester Methodist Hospital for study coordination and creative troubleshooting; Kristin M. Fruth and Cathy D. Schleck for statistical support; and Karen M. Fasbender for assistance with manuscript preparation.
Footnotes
One of the authors (RJS) lists the following relevant financial activities outside of this work and/or any other relationships or activities that readers could perceive to have influenced, or that give the appearance of potentially influencing, this manuscript: Lifecell Corporation (Branchburg, NJ, USA) in an amount of less than USD 10,000 and Biomet Inc (Warsaw, IN, USA) in an amount of USD 10,000 to USD 100,000. One of the authors (MJT) lists the following relevant financial activities outside of this work and/or any other relationships or activities that readers could perceive to have influenced, or that give the appearance of potentially influencing, this manuscript: DJO Global (Vista, CA, USA) in an amount of less than USD 10,000. One of the authors (RTT) lists the following relevant financial activities outside of this work and/or any other relationships or activities that readers could perceive to have influenced, or that give the appearance of potentially influencing, this manuscript: DePuy Orthopaedics, Inc (Warsaw, IN, USA) in an amount of USD 10,000 to USD 100,000.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Dennis DA. Wound complications in total knee arthroplasty. Orthopedics. 1997;20:837–840. doi: 10.3928/0147-7447-19970901-26. [DOI] [PubMed] [Google Scholar]
- 2.Eggers MD, Fang L, Lionberger DR. A comparison of wound closure techniques for total knee arthroplasty. J Arthroplasty. 2011;26:1251–1258.e1251–1254. [DOI] [PubMed]
- 3.Graham DA, Jeffery JA, Bain D, Davies P, Bentley G. Staple vs. subcuticular vicryl skin closure in knee replacement surgery: a spectrophotographic assessment of wound characteristics. Knee. 2000;7:239–243. doi: 10.1016/S0968-0160(00)00055-7. [DOI] [PubMed] [Google Scholar]
- 4.Gurtner GC, Jones GE, Neligan PC, Newman MI, Phillips BT, Sacks JM, Zenn MR. Intraoperative laser angiography using the SPY system: review of the literature and recommendations for use. Ann Surg Innov Res. 2013;7:1. doi: 10.1186/1750-1164-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jonsson K, Jensen JA, Goodson WH, 3rd, Scheuenstuhl H, West J, Hopf HW, Hunt TK. Tissue oxygenation, anemia, and perfusion in relation to wound healing in surgical patients. Ann Surg. 1991;214:605–613. doi: 10.1097/00000658-199111000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan RJ, Fick D, Yao F, Tang K, Hurworth M, Nivbrant B, Wood D. A comparison of three methods of wound closure following arthroplasty: a prospective, randomised, controlled trial. J Bone Joint Surg Br. 2006;88:238–242. doi: 10.1302/0301-620X.88B2.16923. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 8.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res. 2010;468:52–56. doi: 10.1007/s11999-009-1013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lepow B, Perry D, Armstrong D. The use of SPY intra-operative angiography as a predictor of wound healing. Podiatry Management. 2011;8:141–148. [Google Scholar]
- 11.Losken A, Zenn MR, Hammel JA, Walsh MW, Carlson GW. Assessment of zonal perfusion using intraoperative angiography during abdominal flap breast reconstruction. Plast Reconstr Surg. 2012;129:618e–624e. doi: 10.1097/PRS.0b013e3182450b16. [DOI] [PubMed] [Google Scholar]
- 12.Novadaq. The SPY Elite (Intraoperative Perfusion Assessment System Operator’s Manual, November 2011013-50001-001, rev C). Richmond, British Columbia, Canada: Novadaq Technologies; 2008.
- 13.Pestana IA, Zenn MR. Correlation between abdominal perforator vessels identified with preoperative CT angiography and intraoperative fluorescent angiography in the microsurgical breast reconstruction patient. Ann Plast Surg. 2014;72:S144–S149. doi: 10.1097/SAP.0000000000000104. [DOI] [PubMed] [Google Scholar]
- 14.Poss R, Thornhill TS, Ewald FC, Thomas WH, Batte NJ, Sledge CB. Factors influencing the incidence and outcome of infection following total joint arthroplasty. Clin Orthop Relat Res. 1984;182:117–126. [PubMed] [Google Scholar]
- 15.Shantz JA, Vernon J, Leiter J, Morshed S, Stranges G. Sutures versus staples for wound closure in orthopaedic surgery: a randomized controlled trial. BMC Musculoskelet Disord. 2012;13:89. doi: 10.1186/1471-2474-13-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shetty AA, Kumar VS, Morgan-Hough C, Georgeu GA, James KD, Nicholl JE. Comparing wound complication rates following closure of hip wounds with metallic skin staples or subcuticular vicryl suture: a prospective randomised trial. J Orthop Surg (Hong Kong). 2004;12:191–193. doi: 10.1177/230949900401200210. [DOI] [PubMed] [Google Scholar]
- 17.Smith TO, Sexton D, Mann C, Donell S. Sutures versus staples for skin closure in orthopaedic surgery: meta-analysis. BMJ. 2010;340:c1199. doi: 10.1136/bmj.c1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stockley I, Elson RA. Skin closure using staples and nylon sutures: a comparison of results. Ann R Coll Surg Engl. 1987;69:76–78. [PMC free article] [PubMed] [Google Scholar]
- 19.Vince K, Chivas D, Droll KP. Wound complications after total knee arthroplasty. J Arthroplasty. 2007;22:39–44. doi: 10.1016/j.arth.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 20.Vince KG, Abdeen A. Wound problems in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:88–90. doi: 10.1097/01.blo.0000238821.71271.cc. [DOI] [PubMed] [Google Scholar]
- 21.Wyles CC, Taunton MJ, Jacobson SR, Tran NV, Sierra RJ, Trousdale RT. Intraoperative angiography provides objective assessment of skin perfusion in complex knee reconstruction. Clin Orthop Relat Res. 2015;473:82–89. doi: 10.1007/s11999-014-3612-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zenn MR. Fluorescent angiography. Clin Plast Surg. 2011;38:293–300. doi: 10.1016/j.cps.2011.03.009. [DOI] [PubMed] [Google Scholar]