Abstract
Objectives. To understand the current risk of HIV infection and transmission and further elucidate the underlying risk factors among men who have sex with men and women (MSMW) in China. Methods. Following PRISMA guidelines, we conducted a systematic review and meta-analysis of searching through Chinese and English available literature databases between January 2000 and June 2014 to identify articles. Results. Thirty-six articles (including 19,730 MSMW and 53,536 MSMO) met the selection criteria and the aggregated results found that MSMW have significantly higher HIV prevalence than MSMO (6.6% versus 5.4%, OR = 1.27, 95% CI = 1.01–1.58). A higher proportion of MSMW had commercial male partners in the past 6 months (18.3% versus 12.2%, OR = 1.56, 95% CI = 1.01–2.42). Additionally, substance use in the past 6 months was significantly more frequent among MSMW than MSMO (alcohol use: 27.1% versus 13.1%, OR = 2.53, 95% CI = 2.14–2.99; illicit drug use: 5.3% versus 2.5%, OR = 2.09, 95% CI = 1.48–2.95). Conclusion. A higher proportion of commercial sex and substance use among MSMW may be a potentially indicative factor for significantly higher HIV prevalence compared to MSMO. Targeted interventions should aim at increasing the frequency of HIV/STIs screening and preventing high risk commercial sex and substance use among MSMW to decrease their HIV transmission to the general population.
1. Introduction
Men who have sex with men (MSM) are considered as a group of high risk for HIV infection in many countries. According to The Joint United Nations Programme on HIV and AIDS (UNAIDS), the prevalence of HIV infection among MSM in capital cities from nearly 80 countries is on average 13 times higher than that of general populations in these countries [1]. This disparity is also prominent in China; a recent meta-analysis reported that almost 6.5% of MSM were living with HIV [2], which was more than 100 times higher than that in the general population (0.058%) [3]. The latest national report revealed that the proportion of newly diagnosed HIV cases due to male homosexual contact has increased from 12.2% in 2007 to 23.4% in 2014 [4, 5].
Homosexuality is still highly discriminated against in China, which partly results in bisexual behavior becoming one of the biggest obstacles in implementing HIV/AIDS prevention and control interventions among MSM [6, 7]. Additionally, marriage is a family obligation of Chinese traditional culture, which prompts over 80% of MSM eventually getting married to female to hide their real sexual identity and/or carry on family name [8, 9]. Only one in ten MSMW discloses homosexuality to their female partners [10, 11], and unprotected sexual behaviors with female sex partners were prevalent among MSMW [12], which may bridge HIV from the MSM population to the general population.
Previous studies have estimated peraction transmission probability of HIV during anal or vaginal sex among MSM [13, 14]. Clear understanding of the relative risk may help inform MSM of the potential risk which may in turn render them to avoid high risk sexual behaviors, especially among those who make condom use decisions based on penetrative sex type and role in anal sex (receptive or insertive anal sex) and self-reported HIV status of partner. However, until now little literature had vigorously compared the relative risk of HIV infection among MSMW, based on all available data in China.
Existing studies had contradictory findings on the relative risk of HIV infection comparing MSMW and MSMO in China. A recent published national cross-sectional survey of 47,231 MSM from 61 cities in China indicated that MSMW have a lower HIV prevalence than MSMO [15]. However, this conclusion is contradictory to a previous meta-analysis study, which found that MSMW in China have a significantly higher HIV prevalence than MSMO [16]. Until now, no new studies indicated whether or not Chinese MSMW really have higher risk of HIV infection than MSMO. An explicit assessment of the risk of HIV infection in MSMW populations is useful for understanding the dynamic of national HIV epidemic among MSM and developing targeted interventions. Additionally, many new researches on bisexual behavior of MSM have been published in recent years. As such, we also include the latest extensive literature in order to gain a more comprehensive and current understanding of national HIV epidemic among MSM in China. Besides, previous meta-analysis on bisexual behavior among MSM in China failed to explore the underlying differences in HIV-related behavioral risk factors between MSMW and MSMO, which are essential to contextualize behavioral interventions of high risk subpopulations among MSM in China. Therefore, we conducted this systematic review and meta-analysis to compare the disparities in HIV prevalence between MSMW and MSMO and examine behavioral factors underlying the disparities. Three research questions were addressed: (1) do MSMW in China have significantly higher HIV prevalence than MSMO; (2) what are the differences between risk behavioral factors of MSMW and MSMO in China; (3) do MSMW engage in more risk sexual behaviors in different proportions than MSMO that might help to explain the differences in the effect size for HIV prevalence?
2. Methods
2.1. Literature Search
This systematic review and meta-analysis adheres to the PRISMA guidelines [17, 18]; comprehensive literature search was conducted using the following databases for literature published between January 2000 and June 2014 to identify articles: PubMed, Web of Knowledge, Google Scholar, Chinese National Knowledge Infrastructure, VIP, and Wanfang Data. In addition, the reference lists of pertinent articles were examined for additional relevant studies. The combinations of search terms include “bisexual behavior,” “bisexual men,” “MSMW,” “men who have sex with men and women,” “BBM,” “behaviorally bisexual men,” “MSM,” “men who have sex with men,” “homosexual men,” “gay,” “MSMO,” “men who have sex with men only,” “HIV” and “risk behaviors,” “risk factor,” “unprotected sex,” and “condom use.”
2.2. Inclusion/Exclusion Criteria
Studies were included in the meta-analysis if they reported quantitative data on HIV prevalence and risky behaviors rate among both MSMW and MSMO. Studies were excluded if (1) they were duplicate reports; (2) they failed to report risky behaviors or HIV prevalence among both MSMW and MSMO; (3) HIV status was self-reported and not confirmed by test; (4) they did not mention the period of the recall window of risk behaviors; and (5) they were postintervention studies. For research data repeatedly be published in multiple articles, the most comprehensive article was included in the meta-analysis.
2.3. Quality Assessment
The quality of studies was assessed using the quality assessment checklist for observational studies (QATSO score), a validated quality assessment tool for HIV prevalence/risk behaviors among MSM [19]. Items were scored as 1, 0, and NA, which represents “yes,” “no,” and “not applicable,” respectively. The total score of each eligible study must have been above 33% (0% and 33%, 33% and 66%, and 67% and 100%, corresponded to “bad,” “satisfactory,” and “good quality,” resp.).
2.4. Data Extraction
Bisexuality was operationalized using a classification of MSMW or MSMO over any timeframe (behavior recall window) assessed by researchers. Data from eligible studies were extracted with the following information by two reviewers independently: (1) general information about each selected article was extracted (e.g., first author, publication year, study period, study location, method of recruitment, sampling method, and behavior recall window). (2) HIV infection: the prevalence of HIV infection. (3) Behavioral information: (1) condom use: unprotected anal intercourse (UAI) with males, unprotected receptive anal intercourse with males (URAI), and unprotected insertive anal intercourse (UIAI) with males and UAI with commercial male partner; (2) anal sex role: mainly insertive anal intercourse (IAI), mainly receptive anal intercourse (RAI), and both of the two roles; (3) male partner: multiple (≥2) male partners have casual male partners and have commercial male partner (include purchasing sex from male sex workers (money boys and MBs) or selling sex to males); (4) substance use: alcohol use and ever illicit drug use (including opiate, cocaine, amphetamine-type stimulants (ATS), cannabis, and hallucinogens [20]).
2.5. Statistical Analysis
To assess the differences in HIV infection and related risky behaviors between MSMW and MSMO, the random/fixed effect models were used to compute the pooled effect rates and odds ratios (OR) (i.e., prevalence and OR of HIV infection and proportion and OR of condom use, anal sex role, sex partners, and substance use) and relevant 95% confidence intervals (CI). Statistical heterogeneity was qualitatively tested using Cochran's Q statistic (p < 0.10 indicates significant heterogeneity) and quantified by the I 2 index (I 2 < 25%, low heterogeneity; I 2 = 25–50%, moderate heterogeneity; I 2 > 75%, high heterogeneity). If significant homogeneity was detected (I 2 < 75.0, p ≥ 0.10), fixed effect models were employed to calculate the pooled effect rates and ORs; otherwise random effects models were employed [21].
There were many factors that may have affected the homogeneity between studies, such as sample characteristics and methodological differences. Therefore, we performed subgroup analyses to explore the potential sources of between-study heterogeneity on (1) study region: Southwest China, East China, Northeast, North China, and multiple regions; (2) data collection period: prior to 2009, 2009 and later, and unidentified; (3) data collection method: interviewer-administered, self-administered, and unidentified.
A sensitivity analysis was conducted by omitting each study one at a time to assess the influence of each study on the overall estimate. To investigate publication bias, we utilized Egger's regression test and examined the symmetry of funnel plots for each comparative meta-analytic domain. All the statistical analyses were done using STATA V11.2.
3. Results
3.1. Study Selection
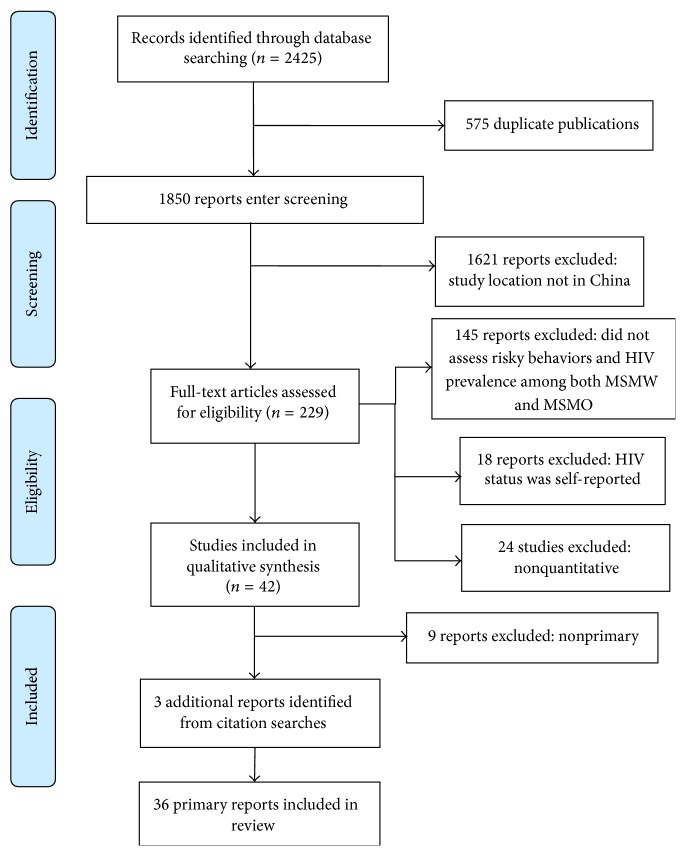
As shown in Figure 1, a total of 2425 relevant articles were identified, of which 42 articles entered further screening, and 36 articles (16 published in English and 20 in Chinese, including 19,730 MSMW and 53,536 MSMO) were finally included in our systematic review and meta-analysis (Figure 1) [15, 22–56]. The characteristics of these included studies are summarized in Table 1.
Figure 1.
Flow diagram of studies included in analysis.
Table 1.
Study characteristics of 36 samples included in meta-analysis.
| Author | Publication year | Location | Study periods | Setting | Sampling method | Survey method | Recall window (months) | QACO score (%) |
|---|---|---|---|---|---|---|---|---|
| Tang [55] | 2007 | Harbin | N/A# | Multiple recruiting methods | Snowball sampling | Interviewer-administered | 6 | 40 |
| Chen [51] | 2008 | Fuzhou | 2008 | MSM venue | Multiple sampling methods | Interviewer-administered | 6 | 60 |
| Ouyang et al. [50] | 2008 | Chongqing | 2006 | Multiple recruiting methods | Snowball sampling | Interviewer-administered | 6 | 33 |
| Bai and Feng [43] | 2010 | Liuzhou | 2008 | Multiple recruiting methods | N/A | Interviewer-administered | 6 | 75 |
| Han et al. [35] | 2012 | China | 2008 | N/A | N/A | N/A | 6 | 60 |
| She et al. [34] | 2012 | 4 cites | 2008 | N/A | Snowball sampling | Interviewer-administered | 6 | 60 |
| Li et al. [48] | 2009 | Chongqing | 2006 | MSM venue | Snowball sampling | Interviewer-administered | 6 | 40 |
| Zhang et al. [31] | 2012 | Wuhan | N/A | MSM venue | Stratified cluster sampling | Interviewer-administered | 6 | 80 |
| Ruan et al. [47] | 2009 | Jinan | 2008 | N/A | RDS## | Interviewer-administered | 6 | 60 |
| Chow et al. [29] | 2013 | Changsha,Tianjin | 2011 | MSM venue | Convenience sampling | Interviewer-administered | 6 | 75 |
| Cai et al. [24] | 2014 | Shenzhen | 2010 | Community-based | RDS | CASI∗ | 6 | 80 |
| Liao et al. [41] | 2011 | 4 cities in Shandong Province | 2008-2009 | Multiple recruiting methods | Multiple sampling methods | Interviewer-administered | 6 | 80 |
| Wang et al. [52] | 2007 | Harbin | 2006 | MSM venue | N/A | Interviewer-administered | 6 | 60 |
| Ruan et al. [53] | 2007 | Beijing | 2005 | N/A | Multiple sampling methods | Interviewer-administered | 6 | 80 |
| Xu et al. [44] | 2010 | Liaoning | 2006 | Recruiting by NGO∗∗ | N/A | Interviewer-administered | 12 | 60 |
| Lau et al. [49] | 2008 | Kunming | 2003–2005 | Multiple recruiting methods | Convenience sampling | Interviewer-administered | 6 | 60 |
| Cao et al. [37] | 2012 | 4 cities | 2008 | Recruiting by NGO | Snowball sampling | Interviewer-administered | 6 | 80 |
| Liao et al. [22] | 2014 | 4 cities in Shandong Province | 2011 | Multiple recruiting methods | N/A | Interviewer-administered | 6 | 70 |
| Tao et al. [28] | 2013 | Beijing | 2010-2011 | Multiple recruiting methods | Multiple sampling methods | Interviewer-administered | 12 | 60 |
| Wu et al. [15] | 2013 | 61 cities | 2008-2009 | N/A | RDS + Snowball sampling | Interviewer-administered | 6 | 90 |
| Guo et al. [36] | 2012 | Beijing | 2009 | Multiple recruiting methods | N/A | Self-administered | 6 | 70 |
| Wang et al. [33] | 2012 | Harbin | 2006–2010 | Community-based | Snowball sampling | Self-administered | 12 | 65 |
| Cao et al. [30] | 2013 | Nanchang | 2011 | Multiple recruiting methods | Multiple sampling methods | Interviewer-administered | 1 week | 60 |
| Li et al. [56] | 2014 | Beijing | 2009–2011 | N/A | RDS | CASI | 12 | 80 |
| Feng et al. [46] | 2010 | Chengdu | N/A | Multiple recruiting methods | Snowball sampling | Interviewer-administered | 6 | 50 |
| Wang et al. [27] | 2013 | Beijing | 2008-2009 | Multiple recruiting methods | Multiple sampling methods | Interviewer-administered | 6 | 80 |
| Zhang et al. [32] | 2012 | Chongqing | 2009 | N/A | RDS | CASI | 6 | 80 |
| Zhang et al. [25] | 2013 | Harbin | 2011 | Recruiting by NGO | N/A | Interviewer-administered | 12 | 60 |
| Cai et al. [23] | 2014 | Shenzhen | 2009–2012 | N/A | Snowball sampling + RDS | Interviewer-administered | 6 | 75 |
| Liu et al. [40] | 2011 | Beijing | N/A | MSM venue | Snowball sampling | Interviewer-administered | 12 | 50 |
| Wang et al. [26] | 2013 | Mianyang | 2011-2012 | N/A | Snowball sampling | Interviewer-administered | 6 | 55 |
| Qu et al. [39] | 2011 | Inner Mongolia | 2010 | Community-based | Snowball sampling | Interviewer-administered | 6 | 60 |
| Xu et al. [45] | 2010 | 4 cities | N/A | N/A | Snowball sampling + RDS | Interviewer-administered | 6 | 70 |
| Xi [38] | 2011 | Hangzhou | 2009-2010 | MSM venue | Snowball sampling | Interviewer-administered | 6 | 50 |
| Chen et al. [42] | 2011 | Lanzhou | 2006–2010 | MSM venue | Snowball sampling | Interviewer-administered | 6 | 50 |
| Li [54] | 2007 | Beijing | 2005 | Multiple recruiting methods | Multiple sampling methods | Interviewer-administered | 6 | 70 |
#N/A: not available, ##RDS: respondent-driven sampling, ∗CASI: computer-assisted self-administered interview, and ∗∗NGO: Non-Governmental Organizations.
3.2. Quantitative Data Synthesis
3.2.1. HIV Prevalence Analysis and Comparison
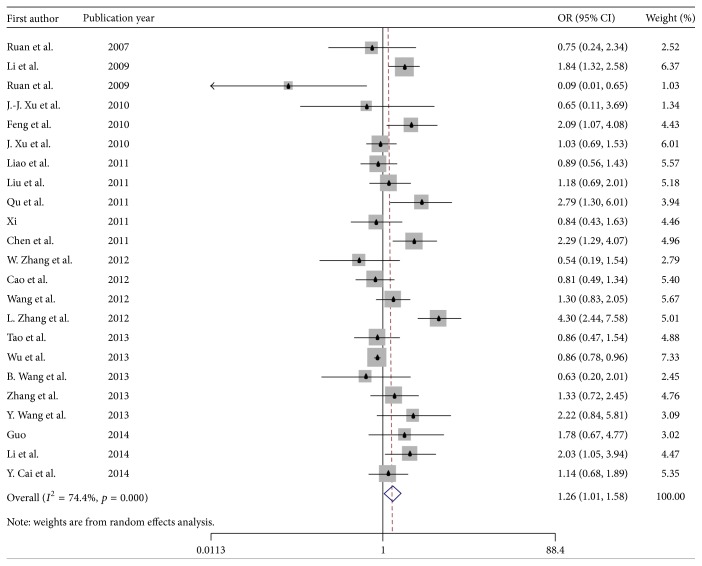
As seen in Table 2, across 23 samples, a significantly higher prevalence of HIV was found among MSMW compared with MSMO (6.6% versus 5.4%, OR = 1.27, 95% CI = 1.01–1.58) (Figure 2). Subgroup analysis by region showed that in the Southwest China, the difference in HIV prevalence between MSMW and MSMO was the highest (14.8% versus 6.7%, OR = 2.43, 95% CI = 1.58–3.72), followed by Northeast China (6.5% versus 5.7%, OR = 1.27, 95% CI = 0.89–1.82), the East China (2.7% versus 5.7%, OR = 0.67, 95% CI = 0.32–1.42), North China (5.7% versus 4.1%, OR = 1.32, 95% CI = 0.89–1.94), and other regions (6.3% versus 6.0%, OR = 1.03, 95% CI = 0.78–1.36). For studies that collected data in 2009 and later, the gap in HIV prevalence between MSMW and MSMO was larger than in other periods (8.3% versus 5.6%, OR = 1.59, 95% CI = 1.08–2.33). The prevalence of HIV for studies recruiting participants through RDS and all other sampling methods was 6.9% versus 6.3%, OR = 1.16, 95% CI = 0.65–2.09 and was 6.7% versus 5.2%, OR = 1.30, 95% CI = 1.05–1.61, respectively.
Table 2.
The odds and prevalence of HIV among MSMW and MSMO by study and design characteristics.
| Category | Subgroup | Comparison group | Number of studies | Prevalence estimate (%) | Heterogeneity | OR and 95% CI | p value | Heterogeneity | ||
|---|---|---|---|---|---|---|---|---|---|---|
| and 95% CI | I 2 (%) | p value | I 2 (%) | p value | ||||||
| Overall | MSMW | 23 | 6.6 (5.3, 7.8) | 89.2 | <0.001 | 1.27 (1.01, 1.58) | 0.018 | 74.4 | <0.001 | |
| MSMO | 23 | 5.4 (4.7, 6.2) | 83.9 | <0.001 | ||||||
|
| ||||||||||
| Regions | Southwest China | MSMW | 4 | 14.8 (9.3, 20.3) | 79.5 | 0.002 | 2.43 (1.58, 3.72) | 0.004 | 53.3 | 0.093 |
| MSMO | 4 | 6.7 (4.0, 9.5) | 83.2 | <0.001 | ||||||
| East China | MSMW | 3 | 2.7 (0.4, 4.9) | 87.4 | <0.001 | 0.67 (0.32, 1.42) | 0.236 | 61.2 | 0.076 | |
| MSMO | 3 | 5.7 (1.7, 9.6) | 89.5 | <0.001 | ||||||
| Northeast China | MSMW | 3 | 6.5 (2.3, 10.7) | 76.1 | 0.015 | 1.27 (0.89, 1.82) | 0.101 | 0.0 | 0.740 | |
| MSMO | 3 | 5.7 (2.3, 9.2) | 73.4 | 0.023 | ||||||
| North China | MSMW | 7 | 5.2 (4.0, 6.5) | 20.0 | 0.277 | 1.32 (0.89, 1.94) | 0.088 | 43.0 | 0.104 | |
| MSMO | 7 | 4.1 (3.1, 5.1) | 48.8 | 0.069 | ||||||
| Several cities from different regions or those that cannot be classified into the above four categories | MSMW | 6 | 6.3 (4.5, 8.2) | 82.3 | <0.001 | 1.03 (0.78, 1.36) | 0.304 | 61.6 | 0.023 | |
| MSMO | 6 | 6.0 (4.8, 7.2) | 72.0 | 0.003 | ||||||
|
| ||||||||||
| Sampling method | RDS | MSMW | 5 | 6.9 (3.8, 10.0) | 95.5 | <0.001 | 1.16 (0.65, 2.09) | 0.218 | 88.9 | <0.001 |
| MSMO | 5 | 6.3 (5.0, 7.6) | 85.4 | <0.001 | ||||||
| All other nonprobability sampling | MSMW | 18 | 6.7 (5.1, 8.3) | 84.8 | <0.001 | 1.30 (1.05, 1.61) | 0.037 | 47.4 | 0.014 | |
| MSMO | 18 | 5.2 (4.2, 6.3) | 83.3 | <0.001 | ||||||
|
| ||||||||||
| Data collection period | Before 2009 | MSMW | 7 | 4.9 (2.8, 6.9) | 94.4 | <0.001 | 0.91 (0.63, 1.32) | 0.103 | 75.1 | <0.001 |
| MSMO | 7 | 5.8 (4.2, 7.4) | 92.6 | <0.001 | ||||||
| 2009 and later | MSMW | 10 | 8.3 (5.9, 10.7) | 71.8 | <0.001 | 1.59 (1.08, 2.33) | <0.001 | 65.3 | 0.002 | |
| MSMO | 10 | 5.6 (4.1, 7.1) | 77.4 | <0.001 | ||||||
| Not reported or cannot be classified into the above two categories | MSMW | 6 | 6.5 (4.6, 8.5) | 75.8 | 0.001 | 1.33 (0.97, 1.84) | 0.376 | 48.8 | 0.082 | |
| MSMO | 6 | 5.0 (3.8, 6.2) | 61.9 | 0.022 | ||||||
|
| ||||||||||
| Data collection method | Interviewer-administered | MSMW | 19 | 6.5 (5.1, 7.9) | 90.5 | <0.001 | 1.21 (0.94, 1.56) | 0.245 | 77.1 | <0.001 |
| MSMO | 19 | 5.6 (4.8, 6.5) | 84.3 | <0.001 | ||||||
| Self-administered | MSMW | 2 | 5.4 (2.8, 8.1) | 23.5 | 0.253 | 1.37 (0.91, 2.08) | 0.211 | 0.0 | 0.567 | |
| MSMO | 2 | 3.9 (2.9, 4.8) | 0.0 | 0.449 | ||||||
| Not reported or cannot be classified into the above two categories | MSMW | 2 | 8.5 (3.4, 13.6) | 72.7 | 0.056 | 1.58 (1.01, 2.50) | 0.030 | 0.0 | 0.354 | |
| MSMO | 2 | 5.7 (0.1, 11.2) | 89.2 | 0.002 | ||||||
Figure 2.
Forest plot of OR pool estimates of HIV infection among MSMW, compared to MSMO.
3.2.2. Possible Explanatory Behavioral Factors for Significant Difference in HIV Infection Risk
As seen in Table 3, for anal sex role with male, MSMW were more likely to have insertive anal intercourse (IAI) and less likely to have receptive anal intercourse (RAI) than MSMO (IAI: 53.2% versus 41.1%, OR = 1.74, 95% CI = 1.26–2.42; RAI: 23.7% versus 38.7%, OR = 0.42, 95% CI = 0.28–0.64). No significant differences were found in condom use between MSMW and MSMO (UAI: 56.7% versus 57.8%, OR = 1.19, 95% CI = 0.99–1.26; UIAI: 63.9% versus 58.3%, OR = 1.19, 95% CI = 0.89–1.60; URAI: 45.9% versus 53.3%, OR = 0.73, 95% CI = 0.50–1.06; UAI with commercial male partner: 53.2% versus 41.1%, OR = 1.07, 95% CI = 0.76–1.50). In comparison with sex partners in the past 6 months, MSMW were significantly more likely to engage in commercial sex than MSMO (18.3% versus 12.2%, OR = 1.56, 95% CI = 1.01–2.42). Yet a marginally significant higher proportion of MSMW have multiple male partners (57% versus 51.9%, OR = 1.19, 95% CI = 0.85–1.67, p = 0.090) and casual male partners (65.3% versus 61.3%, OR = 1.16, 95% CI = 0.85–1.58) in the past 6 months. Additionally, substance use was significantly more frequent among MSMW than MSMO (alcohol use in the past 6 months: 27.1% versus 13.1%, OR = 2.53, 95% CI = 2.14–2.99; illicit drug use in the past 6 months: 5.3% versus 2.5%, OR = 2.09, 95% CI = 1.48–2.95).
Table 3.
The odds and proportion of HIV-related risky behaviors among MSMW and MSMO.
| Behaviors | Number of studies | Comparison group | Prevalence estimate (%) | Heterogeneity | OR and 95% CI | p value | Heterogeneity | ||
|---|---|---|---|---|---|---|---|---|---|
| and 95% CI | I 2 (%) | p value | I 2 (%) | p value | |||||
| Condom use in the past 6 months | |||||||||
| UAI with male | 9 | MSMW | 56.7 (46.2, 67.2) | 94.6 | <0.001 | 1.19 (0.99, 1.26) | 0.123 | 40.7 | 0.096 |
| MSMO | 57.8 (50.4, 65.2) | 95.0 | <0.001 | ||||||
| UIAI with male | 3 | MSMW | 63.9 (57.8, 70.0) | 0 | 0.857 | 1.19 (0.89, 1.60) | 0.101 | 23.2 | 0.272 |
| MSMO | 58.3 (46.2, 70.4) | 94.3 | <0.001 | ||||||
| URAI with male | 3 | MSMW | 45.9 (13.4, 78.4) | 95.1 | <0.001 | 0.73 (0.50, 1.06) | 0.317 | 35.9 | 0.210 |
| MSMO | 53.3 (32.9, 73.8) | 98.0 | <0.001 | ||||||
| UAI with commercial male partner | 3 | MSMW | 53.2 (22.8, 83.5) | 90.1 | <0.001 | 1.07 (0.76, 1.50) | 0.785 | 35.7 | 0.211 |
| MSMO | 41.1 (10.2, 72.6) | 94.7 | <0.001 | ||||||
|
| |||||||||
| Anal sexual role | |||||||||
| Mainly insertive | 8 | MSMW | 53.2 (37.5, 68.9) | 97.9 | <0.001 | 1.74 (1.26, 2.42) | 0.004 | 81.6 | <0.001 |
| MSMO | 41.1 (29.5, 52.8) | 98.4 | <0.001 | ||||||
| Mainly receptive | 8 | MSMW | 23.7 (13.9, 33.4) | 96.8 | <0.001 | 0.42 (0.28, 0.64) | 0.013 | 83.9 | <0.001 |
| MSMO | 38.7 (23.0, 54.5) | 99.2 | <0.001 | ||||||
| Both | 5 | MSMW | 59.4 (53.9, 64.9) | 96.8 | <0.001 | 0.92 (0.69, 1.24) | 0.256 | 62.2 | 0.032 |
| MSMO | 35.8 (20.3, 51.3) | 98.7 | <0.001 | ||||||
|
| |||||||||
| Sex partner in the past 6 months | |||||||||
| Multiple (⩾2) male partners | 5 | MSMW | 57.0 (40.8, 73.2) | 95.3 | <0.001 | 1.19 (0.85, 1.67) | 0.090 | 69.6 | 0.010 |
| MSMO | 51.9 (42.8, 60.9) | 94.7 | <0.001 | ||||||
| Having casual male partners | 4 | MSMW | 65.3 (56.8, 73.7) | 78.6 | 0.003 | 1.16 (0.85, 1.58) | 0.141 | 56.6 | 0.075 |
| MSMO | 61.6 (53.1, 70.1) | 94.5 | <0.001 | ||||||
| Having commercial male partners | 10 | MSMW | 18.3 (11.6, 25.1) | 95.3 | <0.001 | 1.56 (1.01, 2.42) | 0.023 | 86.8 | <0.001 |
| MSMO | 12.2 (8.1, 16.4) | 96.8 | <0.001 | ||||||
|
| |||||||||
| Substance use in the past 6 months | |||||||||
| Alcohol use | 6 | MSMW | 27.1 (15.7, 38.2) | 96.6 | <0.001 | 2.53 (2.14, 2.99) | <0.001 | 33.5 | 0.185 |
| MSMO | 13.1 (7.6, 18.6) | 96.7 | <0.001 | ||||||
| Illicit drug use | 3 | MSMW | 5.3 (4.1, 6.5) | 0 | 0.558 | 2.09 (1.48, 2.95) | <0.001 | 0 | 0.435 |
| MSMO | 2.5 (1.9, 3.1) | 0 | 0.536 | ||||||
3.3. Sensitivity Analysis and Publication Bias
The pooled rates and ORs were not significantly affected in the sensitivity analysis, suggesting that the results were robust. The funnel plot (dots nearly symmetrically distributed) and Egger's test (all p values for Egger's test > 0.05) reflected that there was no evidence of publication bias in any comparison model (data not provided).
4. Discussion
To our knowledge, this is the first systematic review to compare both HIV prevalence and various risk behaviors between Chinese MSMW and MSMO. It provides an insight into the latest HIV epidemic of MSMW and specific HIV transmission risk from MSM to general population and proposes a crucial suggestion for China's health department to make more effective prevention strategy and policy in the future. Building on our earlier research, we integrated the latest extensive 31 additional published pieces of literature and further validated that Chinese MSMW have a significantly higher HIV prevalence than MSMO, which is similar to our previous conducted meta-analysis results [16]. Remarkably, our present systematic review further clarified risk behavioral differences among MSMW and MSMO in China, which have not yet been disclosed before.
The aggregated ORs among MSMW were 1.3 times more likely to be HIV-positive than MSMO, which is quite different from a meta-analysis of American MSM suggesting that HIV prevalence among MSMW is somewhat lower than MSMO (OR = 0.41, 95% CI: 0.31–0.54) [57]. These divergences may be attributed to relatively lower rates of risky behavior of MSMW than MSMO in the United States, such as fewer UAI and URAI exposures. On the contrary, higher rates of commercial sex and substance use were found in Chinese MSMW in present systematic review.
The HIV prevalence among MSMW varies according to geographic differences: the extraordinarily high HIV prevalence of MSMW in the Southwest compared to other regions in China (Southwest China: 12.9%; Northeast China: 6.5%; North China: 5.1%; East China: 2.7%). Due to the fact that Southwest China includes several high HIV prevalence areas in China such as Guangxi and Yunnan [3, 58], MSMW in this region engaged in similar sexual risk behaviors may have higher HIV prevalence than in other regions of China. So targeted measures should be taken, which consider the risk profile of MSMW in high HIV prevalence areas of China in order to curb the spread of HIV.
Moreover, our findings further showed that Chinese MSMW have a high rate of commercial sex in the last 6 months. As MSMW feared exposing their homosexual orientation to their female spouse or partner, some may choose to buy sex from MBs [59]. On the other hand, MBs in China often sell sex to both males and females to increase their income [24]. MBs have become one of the emerging high risk subgroups of MSM communities in recent years [60–62], so higher rate of commercial sex in MSMW was associated with HIV transmission. The current systematic review also estimated that MSMW were 2.1 and 3.0 times more likely to engage in alcohol use than MSMO. Moreover, MSMW more likely use illicit drugs in this study. Such social environments may lead MSMW to hide their sexual orientation by unwillingly engaging in heterosexual relationships, given that they may seek out substance use (alcohol/illicit drugs) in an attempt to modulate pressure from reality [22]. As substance use may relax safer sex norms and increase unprotected anal sex, a higher substance use rate in MSMW may increase the risk of HIV transmission [63–65]. Our findings are consistent with other studies that MSMW prefer insertive anal sex role [28, 30, 31, 34, 57, 66–68], but we failed to find significant differences in condom use with male partners between MSMW and MSMO; hence, insertive anal sex role reducing the risk of HIV transmission may be offset by significant higher rate of commercial sex and using alcohol/illicit drugs.
The findings yielded in this study have some important implications for national HIV prevention and care planning and intervention development. The results suggest that MSMW have composed a significant special subproportion of the population of MSM who are both vulnerable to HIV infection from other higher risk MSM and also in high risk of bridging HIV epidemic to their female partners. However, there are currently no HIV prevention targeted interventions policies for MSMW in China. Given this challenge, we should develop specific prevention strategies targeting MSMW from the following three aspects. First, strategies should focus on increasing HIV/STIs screening programs for MSMW subpopulations to help them to learn their HIV infection status. We could promote and implement VCT or STIs clinic-based interventions to increase the frequency of HIV/STIs screening among MSMW through more frequent calling or sending of text message to remind them with their clinic visits [69]. Second, we should take measure of MSMW on preventing high risk commercial sex and substance use; meanwhile, we should enhance their consciousness of protecting themselves as well as their partners (both male and female). Third, given high risk of HIV infection among MSMW, MSMW's family is also a potential source of HIV discordant couples in China [8, 70–72]. In recent years a number of international studies have shown that the early initiation of antiretroviral therapy (ART) could reduce rates of sexual transmission of HIV-1 and clinical events [73–75], in China; early ART initiation was also reported that may reduce HIV transmission in discordant couples [76]. Hence, early ART initiation for HIV-positive MSMW should also be a good candidate strategy to improve the quality of MSMW's lives and decrease their HIV transmission risk in discordant couples. Additionally, it is essential to actively advocate for the respect and social equality of people with bisexual and homosexual orientations and reduce the social discrimination and family pressures for MSM.
This systematic review and meta-analysis has several important limitations. First, the paucity of existing research did not allow for subgroup analyses of HIV prevalence by race/ethnicity and other demographic differences both within MSMW and compared to MSMO. Second, though we attempted to be as inclusive as possible, our available database searches may have excluded relevant studies from this systematic review and meta-analysis. Third, the majority of included articles of this study recruited participants in urban locations, so rural representation was limited. Fourth, for lack of data from Northwest and other areas in China, it is difficult to reflect the comprehensive national HIV epidemic. Fifth, the results of this study suggest that a higher proportion of commercial sex and substance use among MSMW may be a potentially indicative factor for significantly higher HIV prevalence compared to MSMO, but whether commercial sex and/or substance use significantly moderated HIV prevalence differences between MSMW and MSMO should also be verified in future research.
More emphasis needs to be placed on Chinese MSMW in order to develop more targeted prevention measures for these potentially hidden MSM. Strategies targeting MSMW focused on increasing the frequency of HIV/STIs screening, preventing high risk commercial sex and substance use, encouraging safe sex practices, and actively carrying out early antiretroviral therapy for HIV-positive MSMW; meanwhile, actively advocating for the respect and social equality of people with bisexual and homosexual orientations and reducing the social discrimination and family pressures for MSM could help to slow the spread of HIV/AIDS.
Acknowledgments
The authors appreciate all the researchers whose articles were included in the study. In addition, the authors would like to thank Dr. Xu for reviewing the present paper and providing great guidance. This work was funded in part by Grants from the Mega-Projects of National Science Research for the 12th Five-Year Plan (2012ZX10001006), “Innovation Team Development Programme 2012” of The Ministry of Education, and Key Laboratory Program of Liaoning Education Department (LZ2014038).
Conflict of Interests
The authors declare that they have no conflict of interests.
Authors' Contribution
The work presented here was carried out in collaboration between all authors. All authors read and approved the final paper. The first two authors contributed equally to this meta-analysis. Jun-Jie Xu defined the research theme. Hong-Yi Wang, Ke Yun, and Yong-Ze Li worked on data collection and data abstraction. Hong-Yi Wang and Jun-Jie Xu analysed the data, interpreted the results, and wrote the paper. Hua-Chun Zou, Christiana Meng Zhang, and Kathleen Heather Reilly revised the language. Yong-Jun Jiang, Wen-Qing Geng, Ning Wang, and Hong Shang supplied comments and helped with interpretation of the results.
References
- 1.UNAIDS. HIV/AIDS, Global Report: UNAIDS Report on the Global AIDS Epidemic: 2012. UNAIDS; 2012. [Google Scholar]
- 2.Zhou Y., Li D., Lu D., Ruan Y., Qi X., Gao G. Prevalence of HIV and syphilis infection among men who have sex with men in China: a meta-analysis. BioMed Research International. 2014;2014:12. doi: 10.1155/2014/620431.620431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ministry of Health. 2011 Estimates for the HIV/AIDS Epidemic in China. Joint United Nations Programme on HIV/AIDS; 2011. http://www.unaids.org.cn/pics/20130521161757.pdf. [Google Scholar]
- 4.Ministry of Health. Update on the AIDS/STD epidemic in China and main response in control and prevention in October, 2014. Chinese Journal of AIDS & STD. 2014;20(12):p. 885. [Google Scholar]
- 5.State Council AIDS Working Committee Office (SCAWCO) China 2010 UNGASS Country Progress Report (2008-2009) Beijing, China: Ministry of Health of the People's Republic of China; 2010. [Google Scholar]
- 6.Cao Z., Xu J., Zhang H., et al. Risk factors for syphilis among married men who have sex with men in China. Sexually Transmitted Diseases. 2014;41(2):98–102. doi: 10.1097/OLQ.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 7.Shang H., Xu J., Han X., Spero Li J., Arledge K. C., Zhang L. HIV prevention: bring safe sex to China. Nature. 2012;485(7400):576–577. doi: 10.1038/485576a. [DOI] [PubMed] [Google Scholar]
- 8.Feng L., Ding X., Lu R., et al. High HIV prevalence detected in 2006 and 2007 among men who have sex with men in China's largest municipality: an alarming epidemic in Chongqing, China. Journal of Acquired Immune Deficiency Syndromes. 2009;52(1):79–85. doi: 10.1097/qai.0b013e3181a4f53e. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y., Li L.-L., Zhang G.-G., Fan J., Zhao X.-H., Li K. Analysis on the intention of marriage and the influence factors among unmarried men who have sex with men. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33(10):1031–1035. [PubMed] [Google Scholar]
- 10.Li X., Zhang B., Chu Q., et al. Correlation between AIDS and homosexuals: a study of 2046 male homosexuals in nine major cities of China. The Chinese Journal of Human Sexuality. 2008;17(8):6–10. [Google Scholar]
- 11.Cai Y. M., Pan P., Hong F. C., et al. Survey of KABP on STD/AIDS among male sexual workers in Shenzhen City. China Tropical Medicine. 2007;7(11):2131–2133. [Google Scholar]
- 12.Chow E. P. F., Wilson D. P., Zhang L. What is the potential for bisexual men in China to act as a bridge of HIV transmission to the female population? Behavioural evidence from a systematic review and meta-analysis. BMC Infectious Diseases. 2011;11, article 242 doi: 10.1186/1471-2334-11-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Varghese B., Maher J. E., Peterman T. A., Branson B. M., Steketee R. W. Reducing the risk of sexual HIV transmission: quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use. Sexually Transmitted Diseases. 2002;29(1):38–43. doi: 10.1097/00007435-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Jin F., Jansson J., Law M., et al. Per-contact probability of HIV transmission in homosexual men in Sydney in the era of HAART. AIDS. 2010;24(6):907–913. doi: 10.1097/qad.0b013e3283372d90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu Z., Xu J., Liu E., et al. HIV and syphilis prevalence among men who have sex with men: a cross-sectional survey of 61 cities in China. Clinical Infectious Diseases. 2013;57(2):298–309. doi: 10.1093/cid/cit210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yun K., Xu J. J., Reilly K. H., et al. Prevalence of bisexual behaviour among bridge population of men who have sex with men in China: a meta-analysis of observational studies. Sexually Transmitted Infections. 2011;87(7):563–570. doi: 10.1136/sextrans-2011-050079. [DOI] [PubMed] [Google Scholar]
- 17.Liberati A., Altman D. G., Tetzlaff J., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology. 2009;62 doi: 10.1016/j.jclinepi.2009.06.006.e1-34 [DOI] [PubMed] [Google Scholar]
- 18.Stovold E., Beecher D., Foxlee R., Noel-Storr A. Study flow diagrams in Cochrane systematic review updates: an adapted PRISMA flow diagram. Systematic Reviews. 2014;3, article 54 doi: 10.1186/2046-4053-3-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong W. C. W., Cheung C. S. K., Hart G. J. Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerging Themes in Epidemiology. 2008;5, article 23 doi: 10.1186/1742-7622-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hao W., Xiao S., Liu T., et al. The second National Epidemiological Survey on illicit drug use at six high-prevalence areas in China: prevalence rates and use patterns. Addiction. 2002;97(10):1305–1315. doi: 10.1046/j.1360-0443.2002.00197.x. [DOI] [PubMed] [Google Scholar]
- 21.Higgins J. P. T., Thompson S. G., Deeks J. J., Altman D. G. Measuring inconsistency in meta-analyses. British Medical Journal. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liao M., Kang D., Tao X., et al. Alcohol Use, stigmatizing/discriminatory attitudes, and HIV high-risk sexual behaviors among men who have sex with men in china. BioMed Research International. 2014;2014:8. doi: 10.1155/2014/143738.143738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cai Y., Liu H., Song Y., Hong F. Factors associated with HIV and syphilis infection among men who have sex with men blood donors in Shenzhen. Chinese Journal of Preventive Medicine. 2014;48(2):128–132. [PubMed] [Google Scholar]
- 24.Cai R., Zhao J., Cai W., Chen L., Richardus J. H., de Vlas S. J. HIV risk and prevention behaviors in men who have sex with men and women: a respondent-driven sampling study in Shenzhen, China. AIDS and Behavior. 2014;18(8):1560–1568. doi: 10.1007/s10461-014-0735-x. [DOI] [PubMed] [Google Scholar]
- 25.Zhang L., Zhang D., Yu B., et al. Prevalence of HIV infection and associated risk factors among men who have sex with men (MSM) in Harbin, P. R. China. PLoS ONE. 2013;8(3) doi: 10.1371/journal.pone.0058440.e58440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Y., Li L., Fan J., et al. Investigation on the sexual behavior and HIV infection among MSM in Mianyang City and analysis of the influencing factors. Pratical Preventive Medicine. 2013;20:1166–1169. [Google Scholar]
- 27.Wang B., Li X., Stanton B., Liu Y., Jiang S. Socio-demographic and behavioral correlates for HIV and syphilis infections among migrant men who have sex with men in Beijing, China. AIDS Care. 2013;25(2):249–257. doi: 10.1080/09540121.2012.701714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tao J., Ruan Y., Yin L., et al. Sex with women among men who have sex with men in China: prevalence and sexual practices. AIDS Patient Care and STDs. 2013;27(9):524–528. doi: 10.1089/apc.2013.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chow E. P. F., Jing J., Feng Y., et al. Pattern of HIV testing and multiple sexual partnerships among men who have sex with men in China. BMC Infectious Diseases. 2013;13(1, article 549) doi: 10.1186/1471-2334-13-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cao Y., Li S., Lu L., et al. Comparetive analysis on the characteristics of bisexually-and gay-identified men in Nanchang City. Journal of Preventive Medicine & Public Health. 2013;24:62–66. [Google Scholar]
- 31.Zhang W., Shi P., Shi W., et al. Characteristics of sexual orientation and sexual behavior among men who have sex both with men and women. Acta Medicinae Universitatis Scientiae et Technologiae Huazhong. 2012;41:375–378. [Google Scholar]
- 32.Zhang L., Ding X., Lu R., et al. Predictors of hiv and syphilis among men who have sex with men in a chinese metropolitan city: comparison of risks among students and non-students. PLoS ONE. 2012;7(5) doi: 10.1371/journal.pone.0037211.e37211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang K., Yan H., Liu Y., Leng Z., Wang B., Zhao J. Increasing prevalence of HIV and syphilis but decreasing rate of self-reported unprotected anal intercourse among men who had sex with men in Harbin, China: results of five consecutive surveys from 2006 to 2010. International Journal of Epidemiology. 2012;41(2):423–432. doi: 10.1093/ije/dyr182. [DOI] [PubMed] [Google Scholar]
- 34.She M., Zhang H.-B., Wang J., et al. Investigation of HIV and syphilis infection status and risk sexual behavior among men who have sex with men in four cities of China. Chinese journal of Preventive Medicine. 2012;46(4):324–328. [PubMed] [Google Scholar]
- 35.Han L., Wen Y., Cheng X., et al. Survey on risk factors of HEV infection among man who have sex with man. Chinese Journal of Disease Control and Prevention. 2012;16:586–589. [Google Scholar]
- 36.Guo Y., Li X., Song Y., Liu Y. Bisexual behavior among Chinese young migrant men who have sex with men: implications for HIV prevention and intervention. AIDS Care. 2012;24(4):451–458. doi: 10.1080/09540121.2011.613914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cao Z., Zhang H.-B., She M., et al. Prevalence of HIV infection and sexual behaviors with both men and women among currently married men who have sex with men. Chinese Journal of Epidemiology. 2012;33(5):488–491. [PubMed] [Google Scholar]
- 38.Xi S. Study on AIDS prevention knowledge, behavioral characteristics, HIV infection and its inflnuencing factors among men who have sex with men (MSM) in Hangzhou City [M.S. thesis] Zhejiang, China: Department of Social Medicine & Health Management, College of Public Health, Medical School, Zhejiang University; 2011. [Google Scholar]
- 39.Qu L., Gao Y., Liu J., et al. Prevalence of HIV infection and its associated factors among 805 MSM in inner Mongolia. Practical Preventive Medicine. 2011;18:2081–2083. [Google Scholar]
- 40.Liu Y.-J., Jiang S.-L., Hu Y., Song L., Yu M., Li S.-M. Characteristics of sexual behaviors and infection status of AIDS and other sexually transmitted diseases among men who have sex with men in 2009 in Beijing. Chinese Journal of Preventive Medicine. 2011;45(11):971–974. [PubMed] [Google Scholar]
- 41.Liao M., Kang D., Jiang B., et al. Bisexual behavior and infection with HIV and syphilis among men who have sex with men along the east coast of China. AIDS Patient Care and STDs. 2011;25(11):683–691. doi: 10.1089/apc.2010.0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen J. J., Zhang X. Y., Chen X. Y., et al. The analysis of influence factors of HIV in MSM in Lanzhou. The Chinese Journal of Dermatovenereology. 2011;25(12):954–957. [Google Scholar]
- 43.Bai Y., Feng W. D. HIV related risk sexual behavior among men having sex with men with different sex orientation in Liuzhou. J Prev Med Inf. 2010;26 [Google Scholar]
- 44.Xu J.-J., Zhang M., Brown K., et al. Syphilis and HIV seroconversion among a 12-month prospective cohort of men who have sex with men in Shenyang, China. Sexually Transmitted Diseases. 2010;37(7):432–439. doi: 10.1097/olq.0b013e3181d13eed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu J., Han D.-L., Liu Z., et al. The prevalence of HIV infection and the risk factors among MSM in 4 cities, China. Chinese Journal of Preventive Medicine. 2010;44(11):975–980. [PubMed] [Google Scholar]
- 46.Feng Y., Wu Z., Detels R., et al. HIV/STD prevalence among men who have sex with men in Chengdu, China and associated risk factors for HIV infection. Journal of Acquired Immune Deficiency Syndromes. 2010;53(1):S74–S80. doi: 10.1097/qai.0b013e3181c7dd16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ruan S., Yang H., Zhu Y., et al. Rising HIV prevalence among married and unmarried among men who have sex with men: Jinan, China. AIDS and Behavior. 2009;13(4):671–676. doi: 10.1007/s10461-009-9567-5. [DOI] [PubMed] [Google Scholar]
- 48.Li C.-M., Jia Y.-J., Ding X.-B., Liu J.-B., Xiao Y. HIV infections and heterosexual behaviors among men who have sex with men in Chongqing municipality, China. Chinese Journal of Epidemiology. 2009;30(9):882–886. [PubMed] [Google Scholar]
- 49.Lau J. T. F., Wang M., Wong H. N., et al. Prevalence of bisexual behaviors among men who have sex with men (MSM) in China and associations between condom use in MSM and heterosexual behaviors. Sexually Transmitted Diseases. 2008;35(4):406–413. doi: 10.1097/olq.0b013e318164467f. [DOI] [PubMed] [Google Scholar]
- 50.Ouyang L., Ding X. B., Zhou C., et al. HIV risk sexual behavior among MSM with different sex orientation in Chongqing. South China Journal of Preventive Medicine. 2008;34(2):16–19. [Google Scholar]
- 51.Chen K. Investigation on HIV/AIDS related risk behaviors and infection among men who have sex with men [M.S. thesis] Department of Epidemiology and Health Statistics, School of Public Health, Fujian Medical University; 2008. [Google Scholar]
- 52.Wang L., Tang H., Zhang D., et al. Behavioral features of men who have sex with men with different sexual orientations. Chinese Journal of AIDS & STD. 2007;13:123–126. [Google Scholar]
- 53.Ruan Y., Li D., Li X., et al. Relationship between syphilis and HIV infections among men who have sex with men in Beijing, China. Sexually Transmitted Diseases. 2007;34(8):592–597. doi: 10.1097/01.olq.0000253336.64324.ef. [DOI] [PubMed] [Google Scholar]
- 54.Li X. High risk behaviors and HIV/syphilis prevalence among men who have sex with men in Beijing, China [M.S. thesis] Chinese Center for Disease Control and Prevention; 2007. [Google Scholar]
- 55.Tang H. L. Characteristics of sexual network and HIV/AIDS related risk behaviors among men who have sex with men [M.S. thesis] Chinese Center for Disease Control and Prevention; 2007. [Google Scholar]
- 56.Li X., Lu H., Cox C., et al. Changing the landscape of the HIV epidemic among MSM in China: results from three consecutive respondent-driven sampling surveys from 2009 to 2011. BioMed Research International. 2014;2014:10. doi: 10.1155/2014/563517.563517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Friedman M. R., Wei C., Klem M. L., Silvestre A. J., Markovic N., Stall R. HIV infection and sexual risk among men who have sex with men and women (MSMW): a systematic review and meta-analysis. PLoS ONE. 2014;9 doi: 10.1371/journal.pone.0087139.e87139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yang Y. AIDS epidemic trend in the second-round national comprehensive AIDS prevention and control demonstration zones in Guangxi. Guangxi Medical Journal. 2014;(8):1123–1125. [Google Scholar]
- 59.Solomon S. S., Mehta S. H., Latimore A., Srikrishnan A. K., Celentano D. D. The impact of HIV and high-risk behaviours on the wives of married men who have sex with men and injection drug users: implications for HIV prevention. Journal of the International AIDS Society. 2010;13(supplement 2, article S7) doi: 10.1186/1758-2652-13-s2-s7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lai Y., Cai Y., Song Y., et al. HIV/syphilis infection and high risk behaviors among men who have sex with men previous to be money boys. China Tropical Medicine. 2013;13(6):680–683. [Google Scholar]
- 61.Liu S., Zhao J., Rou K., et al. A Survey of condom use behaviors and HIV/STI prevalence among venue-based money boys in Shenzhen, China. AIDS and Behavior. 2012;16(4):835–846. doi: 10.1007/s10461-011-9978-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nehl E. J., He N., Lin L., et al. Drug use and sexual behaviors among MSM in China. Substance Use & Misuse. 2015;50(1):123–136. doi: 10.3109/10826084.2014.962048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ding Y., He N., Zhu W., Detels R. Sexual risk behaviors among club drug users in Shanghai, China: prevalence and correlates. AIDS and Behavior. 2013;17(7):2439–2449. doi: 10.1007/s10461-012-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Guo Y., Li X., Stanton B. HIV-related behavioral studies of men who have sex with men in China: a systematic review and recommendations for future research. AIDS and Behavior. 2011;15(3):521–534. doi: 10.1007/s10461-010-9808-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.He Q., Wang Y., Lin P., et al. High prevalence of risk behaviour concurrent with links to other high-risk populations: a potentially explosive HIV epidemic among men who have sex with men in Guangzhou, China. Sexually Transmitted Infections. 2009;85(5):383–390. doi: 10.1136/sti.2009.035808. [DOI] [PubMed] [Google Scholar]
- 66.Maulsby C., Sifakis F., German D., Flynn C. P., Holtgrave D. HIV risk among men who have sex with men only (MSMO) and men who have sex with men and women (MSMW) in Baltimore. Journal of Homosexuality. 2013;60(1):51–68. doi: 10.1080/00918369.2013.735938. [DOI] [PubMed] [Google Scholar]
- 67.Beyrer C., Trapence G., Motimedi F., et al. Bisexual concurrency, bisexual partnerships, and HIV among Southern African men who have sex with men. Sexually Transmitted Infections. 2010;86(4):323–327. doi: 10.1136/sti.2009.040162. [DOI] [PubMed] [Google Scholar]
- 68.Phillips A. E., Lowndes C. M., Boily M. C., et al. Men who have sex with men and women in Bangalore, South India, and potential impact on the HIV epidemic. Sexually Transmitted Infections. 2010;86(3):187–192. doi: 10.1136/sti.2009.038216. [DOI] [PubMed] [Google Scholar]
- 69.Zou H., Fairley C. K., Guy R., et al. Automated, computer generated reminders and increased detection of gonorrhoea, chlamydia and syphilis in men who have sex with men. PLoS ONE. 2013;8(4) doi: 10.1371/journal.pone.0061972.e61972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang B., Li X., Chu Q., et al. A survey of HIV/AIDS related behaviors among 2250 MSM in nine major cities of China. Chinese Journal of AIDS & STD. 2008;14:541–547. [Google Scholar]
- 71.He Q., Wang Y., Lin P., et al. Potential bridges for HIV infection to men who have sex with men in Guangzhou, China. AIDS and Behavior. 2006;10(7):S17–S23. doi: 10.1007/s10461-006-9125-3. [DOI] [PubMed] [Google Scholar]
- 72.Choi K.-H., Gibson D. R., Han L., Guo Y. High levels of unprotected sex with men and women among men who have sex with men: a potential bridge of HIV transmission in Beijing, China. AIDS Education and Prevention. 2004;16(1):19–30. doi: 10.1521/aeap.16.1.19.27721. [DOI] [PubMed] [Google Scholar]
- 73.Cohen M. S., Chen Y. Q., McCauley M., et al. Prevention of HIV-1 infection with early antiretroviral therapy. The New England Journal of Medicine. 2011;365(6):493–505. doi: 10.1056/nejmoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pao D., Pillay D., Fisher M. Potential impact of early antiretroviral therapy on transmission. Current Opinion in HIV & AIDS. 2009;4(3):215–221. doi: 10.1097/coh.0b013e328329c5ca. [DOI] [PubMed] [Google Scholar]
- 75.Sáez-Cirión A., Bacchus C., Hocqueloux L., et al. Post-treatment HIV-1 controllers with a long-term virological remission after the interruption of early initiated antiretroviral therapy ANRS VISCONTI Study. PLoS Pathogens. 2013;9(3) doi: 10.1371/journal.ppat.1003211.e1003211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.He N., Duan S., Ding Y., et al. Antiretroviral therapy reduces HIV transmission in discordant couples in rural Yunnan, China. PLoS ONE. 2013;8(11) doi: 10.1371/journal.pone.0077981.e77981 [DOI] [PMC free article] [PubMed] [Google Scholar]