Abstract
OBJECTIVE
We evaluated pregnancy outcomes, maternal and fetal/neonatal, during the Treatment Options for type 2 Diabetes in Adolescents and Youth (TODAY) study.
RESEARCH DESIGN AND METHODS
The TODAY study was a randomized controlled trial comparing three treatment options for youth with type 2 diabetes. Informed consent included the requirement for contraception, including abstinence; this was reinforced at each visit. Following informed consent, self-reported data related to the mother’s prenatal care and delivery and the infant’s health were retrospectively collected. When permitted, maternal medical records and infant birth records were reviewed.
RESULTS
Of the 452 enrolled female participants, 46 (10.2%) had 63 pregnancies. Despite continued emphasis on adequate contraception, only 4.8% of the pregnant participants reported using contraception prior to pregnancy. The mean age at first pregnancy was 18.4 years; the mean diabetes duration was 3.17 years. Seven pregnancies were electively terminated; three pregnancies had no data reported. Of the remaining 53 pregnancies, 5 (9.4%) resulted in early pregnancy loss, and 7 (13%) resulted in loss with inadequate pregnancy duration data. Two pregnancies ended in stillbirth, at 27 and 37 weeks, and 39 ended with a live-born infant. Of the live-born infants, six (15.4%) were preterm and eight (20.5%) had a major congenital anomaly.
CONCLUSIONS
Despite diabetes-specific information recommending birth control and the avoidance of pregnancy, 10% of the study participants became pregnant. Pregnancies in youth with type 2 diabetes may be especially prone to result in congenital anomalies. Reasons for the high rate of congenital anomalies are uncertain, but may include poor metabolic control and extreme obesity.
Introduction
Type 2 diabetes was originally considered a disease of adulthood. However, in the last several decades, the prevalence of type 2 diabetes has increased in youth, most likely related to increases in childhood obesity (1). In 2009, the SEARCH for Diabetes in Youth Study found that the percentage of diabetes in youth 15–19 years of age attributable to type 2 diabetes in the U.S. ranged from 5.5% to 80% (2), depending on race/ethnicity and region of the country. With the increase in type 2 diabetes in youth, an increase in the number of pregnancies complicated by type 2 diabetes is anticipated, including an expected increase in these pregnancies in adolescents.
Type 1 and type 2 diabetes and gestational diabetes mellitus, particularly when there is poor metabolic control, are all known to be associated with increased complications, both in the mother and the neonate (3,4). These pregnancies may also result in adverse long-term metabolic consequences for the offspring from developmental programming effects of maternal diabetes and obesity (5,6). In addition, pregnancies in healthy girls that occur during the adolescent years are already considered high risk because of increased maternal and fetal/neonatal complications (7). Therefore, pregnancies occurring in adolescents with type 2 diabetes would be expected to be at especially high risk. However, despite the rising prevalence of pediatric type 2 diabetes, data on rates and outcomes of teenage pregnancy among girls with type 2 diabetes are limited. Such data are critical to understanding how to best care for these youth and their offspring.
The Treatment Options for type 2 Diabetes in Adolescents and Youth (TODAY) study was a multicenter clinical trial with a broad racial/ethnic and geographic representation in the U.S. and the largest intervention study in youth with type 2 diabetes to date. The TODAY cohort offers, therefore, an opportunity to assess pregnancy rates and outcomes across the spectrum of individuals with youth-onset type 2 diabetes. The rationale, design, and methods (8); baseline characteristics of the cohort (9); and primary outcome (10) of the TODAY study have been previously reported. The purpose of this article is to report the pregnancy rates, maternal complications, pregnancy outcomes, and fetal/neonatal outcomes in the female TODAY participants and place these outcomes in the larger context of what is known about pregnancies in young women with diabetes and teenage pregnancy in general.
Research Design and Methods
The TODAY study was a National Institutes of Health–sponsored, three-group, randomized controlled trial to assess the efficacy of treatment options for type 2 diabetes in youth. In summary, the TODAY cohort included 699 youths with type 2 diabetes, defined according to American Diabetes Association criteria, who had the following characteristics: age range 10–17 years, obese or overweight (BMI >85th percentile), islet cell antibody negative, C-peptide positive, type 2 diabetes duration of <2 years, glycosylated hemoglobin (HbA1c) <8.0%, and received no diabetes medications other than metformin (MET). TODAY participants were randomized 1:1:1 to receive MET alone; MET plus rosiglitazone (ROSI); or MET plus an intensive family-based lifestyle program (TODAY Lifestyle Program) aimed at improving eating habits, increasing activity level, and weight reduction. The MET and ROSI participants, family, and the study staff were double blinded. The primary end point of the TODAY study was “treatment failure,” defined as HbA1c >8.0% consecutively for a 6-month period or the sustained need for insulin therapy for 3 months after initiating insulin therapy for treatment of acute metabolic decompensation.
Because of the potential use of ROSI, a pregnancy class C medication, the TODAY study protocol and consent form specified that all female participants either used “an acceptable method of birth control,” including abstinence, or they would stop receiving study medication. In addition, the study protocol specified that all subjects receive standard diabetes education, including, in female participants, counseling before conception to defer pregnancy until the HbA1c was under 6% and to plan all pregnancies under medical supervision. A pregnancy test was performed in female participants at every study visit (i.e., every 2 months in year 1 and every 3 months for the remainder of the study). If a study participant was found to be pregnant, the administration of study medications was immediately stopped, and the participant was referred for obstetrical care from a maternal-fetal medicine specialist. Study outcomes were not tracked during pregnancy or lactation, but resumed after the pregnancy and lactation were completed.
Four hundred fifty-two (64.7%) of the enrolled subjects were female, and nearly all were in either Tanner stage IV or V at the time of randomization. Since contraception was a universal recommendation for girls in the TODAY study, only limited data about pregnancies were obtained prospectively. When it was recognized that pregnancy incidence was higher than anticipated, we retrospectively collected self-reported data from the TODAY participants about their pregnancy and its outcome, including any maternal or infant complications. In addition, permission was sought from participants to obtain the mothers’ obstetrical records and the infants’ birth records for abstraction into standardized data collection forms. Maternal questionnaires reporting pregnancy health and the infant’s health were provided by the participants for 60 of 63 known pregnancies. Mothers’ records were made available for the 53 pregnancies with known outcomes and not electively terminated, and infant records were available in all 39 live-born infants. Records were available in both of the stillborn infants. This report presents the data for all pregnancies that began after randomization (starting in July 2004) and were completed by the end of the randomized controlled portion of the TODAY trial (February 2011). Participants were followed on average for 3.8 years.
For pregnancies resulting in a live birth, gestational age was classified as early preterm (27 to <34 weeks), late preterm (34–36 weeks), or term (≥37 weeks). Birth weight was classified as large for gestational age (LGA) (>90th percentile), small for gestational age (SGA) (<10th percentile), or appropriate for gestational age using U.S. National Reference Standards (11,12). Birth weight was also classified as very low birth weight (<1,500 g), low birth weight (1,500–2,499 g), normal weight (2,500–3,999 g), or macrosomic (>4,000 g) using Centers for Disease Control and Prevention standards.
Statistical Analysis
Descriptive statistics reported are median, minimum, maximum, quartiles, and percentages. Subgroup comparisons were made using the Kruskal-Wallis test for continuous variables and the Fisher exact test or χ2 test for categorical variables. P values <0.05 are considered statistically significant. No adjustment was made for multiple comparisons, and results should be considered descriptive and exploratory.
Results
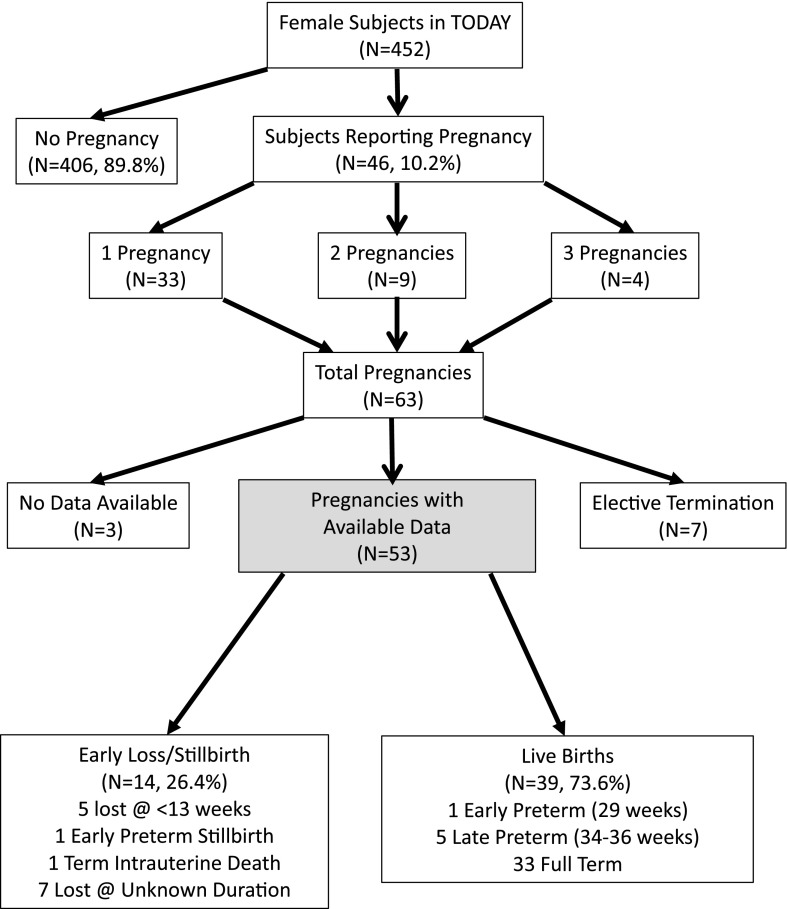
Of the 452 female participants enrolled in the TODAY study, 46 (10.2%) had 63 pregnancies. Of these, 33 participants (71%) had a single pregnancy, 9 (19.5%) had two pregnancies, and 4 (8.7%) had three pregnancies (Fig. 1). No information was available on the seven pregnancies that were electively terminated or on the three participants who were lost to follow-up. Of the remaining 53 pregnancies, there were 14 pregnancy losses; 5 of these were early pregnancy losses or miscarriages, and 9 had inadequate pregnancy duration data. There were 39 live births, 1 at 29 weeks, 5 late preterm deliveries, and 33 term births (Fig. 1).
Figure 1.
Breakdown of pregnancies reported by young women in the TODAY study. The shaded box represents the pregnancies on which results are reported herein.
A comparison of the TODAY female participants who did and did not experience a pregnancy is shown in Table 1. Those who became pregnant were older at randomization (15 vs. 13 years of age, P < 0.0001), and, at the time of pregnancy, they were more likely to be living away from their parent’s home (P = 0.008) and were more likely to have a lower household income (P = 0.03). Other demographic characteristics, including ethnic composition, parental education, diabetes duration, BMI, smoking history, TODAY treatment group, HbA1c at baseline, and the percent of those reaching the primary end point of HbA1c persistently >8%, were not different between those reporting a pregnancy and those who did not (Table 1). There was no significant difference in the pregnancy rate across racial/ethnic groups (Table 1).
Table 1.
Characteristics of female participants with reported pregnancies (N = 46) compared with female participants not reporting pregnancy (N = 406)
| Characteristics | Pregnancy reported (N = 46) | No pregnancy reported (N = 406) | P value* |
|---|---|---|---|
| Pregnancies reported | |||
| One pregnancy reported | 33 (71.74) | ||
| Two pregnancies reported | 9 (19.57) | ||
| Three pregnancies reported | 4 (8.70) | ||
| Age at randomization | 15 (13, 17) | 13 (12, 15) | <0.0001 |
| Duration of diabetes at baseline (months) | 6 (4, 11) | 6 (4, 10) | NS |
| Race/ethnicity | NS | ||
| American Indian | 6 (13.04) | 24 (5.91) | |
| Black non-Hispanic | 17 (36.96) | 141 (34.73) | |
| Hispanic | 17 (36.96) | 153 (37.68) | |
| White non-Hispanic | 5 (10.87) | 81 (19.95) | |
| Asian non-Hispanic | 1 (2.17) | 7 (1.72) | |
| Parents in household | 0.0081 | ||
| Lives with neither parent | 11 (24.44) | 34 (8.59) | |
| Lives with mother only | 18 (40.00) | 188 (47.47) | |
| Lives with father only | 3 (6.67) | 14 (3.54) | |
| Lives with both parents | 13 (28.89) | 160 (40.40) | |
| Parent education | NS | ||
| Less than HS education | 18 (40.00) | 98 (24.62) | |
| HS, business, tech education | 6 (13.33) | 106 (26.63) | |
| Some college education | 15 (33.33) | 128 (32.16) | |
| College degree | 6 (13.33) | 66 (16.58) | |
| Household income | 0.0314 | ||
| <$25,000 | 22 (52.38) | 148 (40.44) | |
| $25,000–49,999 | 17 (40.48) | 126 (34.43) | |
| >$49,999 | 3 (7.14) | 92 (25.14) | |
| Treatment group | NS | ||
| MET only | 14 (30.43) | 132 (32.51) | |
| MET plus ROSI | 15 (32.61) | 137 (33.74) | |
| MET plus TLP | 17 (36.96) | 137 (33.74) | |
| Baseline HbA1c (%) | 6.00 (5.50, 6.90) | 5.90 (5.50, 6.50) | NS |
| Baseline HbA1c (mmol/mol) | 42 (37, 52) | 41 (37, 52) | NS |
| Ever smoked | 19 (41.30) | 127 (31.28) | NS |
Values are reported as frequencies (%) or median (25th percentile, 75th percentile), unless otherwise indicated. HS, high school; TLP, TODAY Lifestyle Program.
*From Kruskal-Wallis test for continuous variables with medians presented and χ2 for categorical variables.
The pregnancy demographics, management, and outcomes are shown in Tables 2 and 3. The median maternal age was 18.4 years at the time of the first pregnancy, 20.1 years at the time of the second pregnancy, and 22.3 years at the time of the third pregnancy (Table 2). Age at pregnancy was not associated with pregnancy outcome (data not shown). The pregnancies were first identified at a median of 6.2 weeks after the last menstrual period, which is consistent with frequent pregnancy tests performed during the trial. Only 3 participants (5%) reported using contraception prior to the pregnancy, while 45 (75%) reported they had not used contraception prior to the pregnancy. In addition, only eight participants (13.3%) recalled receiving counseling before conception.
Table 2.
Maternal pregnancy demographics and pregnancy care and outcomes (N = 60 with data provided)
| Characteristics | Maternal pregnancy demographics and pregnancy care (N = 60 pregnancies) |
|---|---|
| Maternal age (years) | |
| First pregnancy | 18.4 (14.3, 16.5, 19.3, 21.7) |
| Second pregnancy | 20.1 (16.7, 18.6, 21.5, 23.1) |
| Third pregnancy | 22.3 (18.3, 20.1, 23.1, 23.4) |
| Duration of diabetes at first pregnancy (months) | 38 (29, 51) |
| Interval between pregnancies (months) | 19.6 (13.0, 25.5) |
| Gestational age when pregnancy noted (weeks) | 6.2 (4.9, 7.9) |
| Using contraception | |
| Yes | 3 (5) |
| No | 45 (75) |
| Did not provide information | 12 (20) |
| Reported receiving preconception counseling | |
| Yes | 8 (13.3) |
| No | 40 (66.7) |
| Missing | 12 (20.0) |
| BMI closest to conception* (N = 46) | 35.2 (20.3, 31.0, 39.7, 50.2) |
| HbA1c closest to conception (%)** (N = 46) | 7.0 (5.1, 5.9, 8.9, 13.6) |
| HbA1c closest to conception (mmol/mol)** (N = 46) | 53 (32, 41, 74, 125) |
| HbA1c closest to delivery (%)*** (N = 47) (exclude known terminations) | 6.3 (5.1. 5.6, 8.2, 12.1) |
| HbA1c closest to delivery (mmol/mol)*** (N = 47) (exclude known terminations) | 45 (32, 38, 66, 109) |
| Highest HbA1c during pregnancy (N = 35) (excludes known terminations) | |
| <6.5% (<48 mmol/mol) | 13 (37.1) |
| 6.5–7.5% (48–58 mmol/mol) | 5 (14.3) |
| 7.5–8% (58–64 mmol/mol) | 4 (11.4) |
| ≥8% (≥58 mmol/mol) | 13 (37.1) |
| Reported receiving prenatal care | |
| Yes | 39 (73.6) |
| No | 5 (9.4) |
| Missing | 9 (17.0) |
| Mother’s medical records available (N = 53) (excludes known terminations) | |
| Yes | 35 (66.0) |
| No | 18 (34.0) |
| Infant’s medical records available (N = 41) (includes only live births and 2 stillbirths) | |
| Yes | 26 (63.4) |
| No | 15 (36.6) |
Values are given as the median (minimum, 25th percentile, 75th percentile, and maximum), median (25th percentile and 75th percentile), or frequency (%).
*Median 46 days (minimum 1 day, 25th percentile 29 days, 75th percentile 223 days, and maximum 1,510 days) from conception.
**Median 44 days (minimum 1 day, 25th percentile 29 days, 75th percentile 223 days, and maximum 1,892 days) from conception.
***Median 189 days (minimum 4 days, 25th percentile 45 days, 75th percentile 359 days, and maximum 1,720 days) from delivery.
Table 3.
Pregnancy outcomes (N = 53), excludes voluntary terminations (7) and no data reported (3)
| Characteristics | Frequency (%) |
|---|---|
| Duration of pregnancy | |
| <13 weeks; 7, 8, 9, 10, and 12 weeks | 5 (9.4) |
| 13–26 weeks | 0 (0) |
| 27–33 weeks; 27-week stillbirth, live birth 29 weeks with congenital anomalies | 2 (3.8) |
| 34–36 weeks; 5 live births, 1 with congenital anomalies | 5 (9.4) |
| ≥37 weeks; 1 stillbirth, 33 live births, 6 with congenital anomalies | 34 (64.2) |
| Pregnancy loss, no data on pregnancy duration | 7 (13.2) |
| Of the pregnancies ending in the 3rd trimester (N = 41), % live births | 39 (95.1) |
| Birth weight category (live births and weight available N = 37) | |
| LGA (90th percentile or higher according to Harriet Lane*) | 8 (21.6) |
| SGA (10th percentile or lower according to Harriet Lane*) | 2 (5.5) |
| Birth weight category (live births and weight available N = 37) | |
| <1,500 g | 0 (0) |
| 1,500–2,499 g | 3 (8.1) |
| ≥2,500 g | 27 (73.0) |
| ≥4,000 g | 7 (18.9) |
| Congenital anomalies (live births only N = 39) | 8 (20.5) |
| Types of congenital anomalies | |
| Cardiac | 4 (50.0) |
| Other | 4 (50.0) |
The median BMI recorded closest to conception was 35.2 kg/m2, the range was 20.3–50.2 kg/m2, and 18.6% of participants had BMI >40 kg/m2 (Table 2). The median HbA1c closest to conception was 7.0% (53 mmol/mol), and the range was 5.1–13.6% (32–125 mmol/mol). The median gestational age at these HbA1c levels was 6.2 weeks (Table 2). The median HbA1c closest to the date of delivery was 6.3% (45 mmol/mol), and the range was 5.1–12.1% (32–109 mmol/mol), although the number of participants with available HbA1c relatively close to delivery was limited. HbA1c values during pregnancy, available in only 35 pregnancies (55.6%), showed that the highest HbA1c recorded was <6.5% in 37.1%, >6.5% in 62.8%, >7.5% in 48.5%, and >8% in 37.1% (Table 2).
The majority of participants (39 [73.6%]) reported receiving prenatal care, but 9 (17.0%) did not provide information about prenatal care (Table 2). Those reporting prenatal care were more likely to have a term, live-born infant than those who reported no prenatal care or did not provide this information (P = 0.0002) (Supplementary Table 1). The two women reporting a stillborn infant both reported receiving prenatal care.
In the 53 pregnancies that were not electively terminated and on which data were available, there were 14 pregnancy losses (26.4%) and 39 live births (Table 3). Of the 39 live births, 33 were term births (Table 3). The stillbirth at 27 weeks had a prior genetic quad screen test that was positive for an elevated maternal serum α fetoprotein level, but the examination report at delivery was not available. The pregnancy that resulted in an intrauterine death at 37 weeks was complicated by maternal morbid obesity and hypertension, as well as poor glycemic control (HbA1c >8%). Autopsy findings in this stillbirth suggested that the cause of death was a thrombosis of one umbilical artery and the umbilical vein resulting in acute fetal circulatory compromise.
Birth weights were available for 37 of the 39 live-born infants (Table 3). Of these, eight infants (21.6%) were LGA (>90th percentile) and/or macrosomic (≥4,000 g), and 2 infants (5.4%) were SGA (<10th percentile).
Of the 44 women reporting on medication use during pregnancy, 6.8% reported taking MET, 72.7% reported taking insulin, and none reported taking the study medication, ROSI, or a statin or an ACE inhibitor. Twelve women (27.3%) reported taking other, nonstudy medications during the pregnancy, including one taking methyldopa for hypertension and two taking oral micronized progesterone.
Data describing maternal and newborn complications derived from 48 pregnancies with available information about complications are shown in Supplementary Tables 2 and 3. Thirteen women required hospitalization during the pregnancy other than for delivery of the infant. Four mothers had preeclampsia. In addition, 5 women had protein excretion of ≥300 mg/g creatinine, and 10 women had hypertension during the pregnancy; in 4 of those with hypertension, the hypertension was present before pregnancy, and all 4 of those with preeclampsia had hypertension prior to pregnancy. Another three women had urinary albumin levels of 30 to <300 mg/g creatinine, which may reflect increased albumin excretion associated with pregnancy. Only six participants had retinal photographs taken before their first pregnancy. Of these, one participant had mild nonproliferative diabetic retinopathy at 4.75 years duration of diabetes; the others had no retinopathy. Twenty-nine participants had retinal photography after their first pregnancy. Of those, eight participants (27.6%) had mild nonproliferative diabetic retinopathy and the others had no retinopathy.
Nine (23%) of the 39 live-born infants required a prolonged hospitalization, that is, a longer hospitalization than the mother. The eight infants with congenital anomalies accounted for most of the prolonged hospitalizations. Six infants (16.7%) had hypoglycemia, three (8.3%) had respiratory distress syndrome, and one (2.8%) had hypocalcemia. None had shoulder dystocia.
Strikingly, among the 39 live births, there were 8 (20.5%) with major congenital anomalies (Table 3). These anomalies included four cardiac anomalies and four other anomalies (polycystic kidney disease, microcephaly, cleft palate, and jejunal atresia). (See Supplementary Table 4 for the available details of the congenital anomalies.) Congenital anomalies were not reported for miscarriages or stillbirths. In the full-term pregnancies, live births without a congenital anomaly (a desirable outcome, n = 27) were compared with those ending in a miscarriage, stillbirth, preterm delivery, or an infant with a congenital anomaly (an undesirable outcome; n = 26); there was no significant difference in the HbA1c closest to conception (median 7.5% [range 5.1–13.6%], median 58 mmol/mol [range 32–125 mmol/mol] vs. 6.9% [range 5.2–11.9%], median 52 mmol/mol [range 33–107 mmol/mol]) or in the HbA1c closest to delivery (and after delivery) (median 6.2% [range 5.2–12.1%], [median 44 mmol/mol [range 33–109 mmol/mol] vs. 6.4% [range 5.1–11.9%], median 46 mmol/mol [range 32–107 mmol/mol]). There was a significant difference in desirable outcomes across assigned treatment groups (P = 0.027), with those assigned to the ROSI-plus-MET arm having a higher rate of desirable outcomes (data not shown). None of the participants reported taking ROSI during their pregnancies. There was no significant difference between glycemic control in pregnancies resulting in a live birth (n = 39) versus those resulting in a miscarriage or stillbirth (n = 14, data not shown). In the pregnancies with HbA1c data available within 8 weeks of conception and resulting in the birth of a child with a congenital anomaly (n = 5), the median HbA1c was 6.3% (range 5.6–11.9% [median 45 mmol/mol, range 38–107 mmol/mol]) compared with the median HbA1c 7.6% (range 5.2–13.6 [median 60 mmol/mol, range 33–125 mmol/mol]) in those without a congenital anomaly (n = 21). There was no significant difference in pregnancy outcome when stratified by a maternal BMI <35 kg/m2 vs. ≥35 kg/m2 (data not shown). Using other BMI cutoff thresholds (25, 30, or 40 kg/m2) did not change this result. Finally, 50% of women with unsuccessful pregnancies reported current or prior smoking, whereas only 29.6% of those with successful pregnancies reported smoking; however, this difference was not statistically significant (P = 0.1296).
Conclusions
This report summarizes pregnancy frequency and outcomes in adolescents and young adults with type 2 diabetes in the TODAY study and reveals that, despite a universal recommendation for contraception or abstinence, 10.2% of female participants experienced a pregnancy during the mean 3.8 years of study participation. Importantly, these adolescents and young women had poor pregnancy outcomes, with 26.4% of pregnancies ending in a miscarriage, stillbirth, or intrauterine death, and 20.5% of the live-born infants having a major congenital anomaly.
The pregnancy rate of 10.2% is consistent with the reported teen pregnancy rate in the U.S. during the time of the TODAY trial (13,14). In the TODAY trial, contraception or abstinence was specifically stated as being necessary for participation, and this was explained during the informed consent process. The importance of contraceptive use as well as the importance of delaying pregnancy until the HbA1c was <6% was again explained prior to randomization and was emphasized verbally at each subsequent visit. Thus, the very low number of pregnant TODAY study participants who reported using contraception prior to conception (4.8%) is of great concern. It is of particular concern that only eight of the participants with a pregnancy (13.3%) reported remembering that they had received diabetes-specific counseling on the importance of using adequate contraception during the TODAY trial. An improved understanding of the reasons for ongoing pregnancy risk in teens, despite counseling on contraceptive use and the risk to both the mother and the fetus of a pregnancy complicated by poorly controlled type 2 diabetes, is an important area for continued study (15,16). Past data suggest that perceived side effects of contraception, difficulty in obtaining contraception, an unrealistic plan to abstain from sexual activity, and, importantly, the lack of motivation to postpone childbirth all contribute to infrequent use of contraception among adolescents (17,18). The use of long-acting reversible contraception (LARC) could be considered in youth who are at high risk for pregnancy, especially in those also at high risk for discontinuation of oral contraceptive use (19,20). Further, the finding that almost 30% of those with one pregnancy during the TODAY study had a subsequent pregnancy is consistent with the current literature and suggests that postpartum use of LARC should be recommended (20,21). Our experience with a 10.2% pregnancy rate and poor pregnancy outcomes indicates an urgent need for effective contraception educational programs directed at teens and young women with type 2 diabetes. This includes information about LARC as well as more general education about the effects of obesity and diabetes on the health of the offspring.
The pregnancy complication rate among the TODAY youth is similar to that reported in the literature in adult women with either type 2 or type 1 diabetes, including the rate of late-term pregnancy loss. A large study from England, Wales, and Northern Ireland (3) and a study from the Netherlands (4) reported perinatal infant mortality to be 3–5% in woman of all ages with diabetes, including those with relatively well-controlled type 2 diabetes; this is four times that of the general population and similar to the rate of stillbirths (3.7%) that we report. However, the rate of major anomalies seen in the TODAY study (20.5%) was much higher than the 4.6% reported in adult women from the U.K. (3). Glycemic control, especially in the 3 months prior to conception and the first trimester of pregnancy, is important in preventing congenital anomalies (22). HbA1c within the normal range during this time has been shown to decrease the rate of congenital anomalies in offspring of women with diabetes to one that is indistinguishable from that of the general population (23). While 25% of the TODAY study participants with HbA1c reported within this time frame had HbA1c <6.0%, most of the remainder had significantly higher levels, including 25% with HbA1c ≥9%. These elevated HbA1c levels could at least partly explain the increased rate of congenital anomalies. Although there was no significant difference in congenital anomalies when pregnancies were analyzed by HbA1c levels within 8 weeks of conception, the number of TODAY study participants with pregnancies and congenital anomalies is relatively small. Our small sample size, as well as a high prevalence of other maternal comorbidities associated with congenital anomalies, including obesity and lower socioeconomic status, does not allow us to determine whether poor glycemic control was associated with the high rate of congenital anomalies in our population.
Increased maternal BMI to 35–40 kg/m2, even without associated diabetes, was recently reported (24) to be associated with a stillbirth and fetal death rate two to four times higher than expected. Half of the pregnant TODAY study participants had BMI >35 kg/m2, and 18.6% had BMI >40 kg/m2. Obesity has also been associated with an increase in congenital anomalies, including central nervous system, gastrointestinal, and palatal defects (25). One study (26) documented an improvement in maternal and neonatal outcomes following bariatric surgery. Although we did not see an association of BMI ≥35 kg/m2 with an increase in congenital anomalies or fetal deaths compared with maternal BMI <35 kg/m2, this may be due to small pregnancy numbers. Smoking also increases the odds of congenital anomalies in obese women (25). Overall, 41% of the TODAY study pregnant youth reported a history of smoking, with 50% of those with unsuccessful pregnancy outcomes reporting being current or prior smokers compared with 29.6% of those with successful pregnancies. In addition, 40% of the participants reporting pregnancy had parents with less than a high school education, and 52.4% were from families with a household income of <$25,000 per year. Therefore, obesity, smoking, poor socioeconomic status, and poor glycemic control may have all contributed to the high rate of congenital anomalies.
Although teen pregnancy has been reported to be associated with adverse pregnancy outcomes (7), not all studies agree. A report from Ontario, Canada, found lower levels of family income and education in teen pregnancies as well as increased levels of smoking and substance abuse (27). The TODAY study did not formally assess subjects for substance abuse other that at the time of screening. In the report from Ontario (27), the rates of preterm birth and fetal death were not different from those of individuals 20–35 years old; however, infants of teens had increased rates of admission to the neonatal intensive care unit for preterm birth. In the TODAY study, fetal loss was not associated with age, but this analysis may have been limited by the small sample size and relatively narrow age range of the participants.
In addition to the individual and family trauma of a pregnancy loss or the birth of a child with a congenital anomaly, a major concern for public health planning is the health impact of poorly controlled maternal type 2 diabetes on the offspring (5). Studies (28–30) have shown that the offspring of women who are overweight and obese, as well as women with poorly controlled diabetes, are at higher risk for future obesity, diabetes, and other characteristics of the metabolic syndrome in later childhood and as adults. This fetal programming effect is thought to be secondary to epigenetic changes and direct influences on metabolic pathways, adipocyte development, hypothalamic appetite regulatory pathways, mitochondrial function, and changes in pancreatic, hepatic, and nephron development (5,6,31).
To decrease the risks of obesity and metabolic syndrome in the offspring of women with type 2 diabetes, we need better ways to achieve weight loss and glycemic control, especially in youth. These are very difficult goals to accomplish and are often not possible with the currently available therapy (10). Glucose control before conception is also important to decrease the risks of defects in organogenesis during the 4–6 weeks after conception. This study and others remind us that adolescents may not yet be capable of making fully informed and healthy decisions about the appropriate timing of conception (18). Physicians caring for adolescents with type 2 diabetes should be continually aware of the need to help teens understand the importance of optimizing the timing of pregnancy to ensure a healthy pregnancy and healthy baby. Ongoing and recurring counseling about the importance of birth control and postponing pregnancy until appropriate glycemic control is established is an important component of caring for adolescent girls with diabetes.
This study is limited by the retrospective collection of much of the pregnancy-associated data. An additional limitation to the study is that some teens and young women did miss one or more study visits and then returned for study visits more regularly. When a participant returned for regular study visits, they were asked about pregnancies and contraception during the time away from the study. Thus, we think it is unlikely that a completed pregnancy occurred during this time without our knowledge, but an early termination or loss may have been unreported by those with regular study visit attendance as well as those missing study visits.
In the observational extension of the TODAY trial, data on new pregnancies are being collected prospectively. Further studies are greatly needed to provide data about pregnancy outcomes and the long-term health of children and youth born to young women with type 2 diabetes.
Supplementary Material
Article Information
Acknowledgments. The TODAY Study Group thanks the following companies for donations in support of the efforts of the study: Becton, Dickinson and Company; Bristol-Myers Squibb; Eli Lilly and Company; GlaxoSmithKline; LifeScan, Inc.; Pfizer; and Sanofi. The authors also thank the American Indian partners associated with the clinical center located at the University of Oklahoma Health Sciences Center, including members of the Absentee Shawnee Tribe, Cherokee Nation, Chickasaw Nation, and Choctaw Nation of Oklahoma, and the Oklahoma City Area Indian Health Service for their participation and guidance.
The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the respective Tribal and Indian Health Service Institution Review Boards or their members.
Funding. This work was completed with funding from the National Institute of Diabetes and Digestive and Kidney Diseases and the National Institutes of Health Office of the Director (OD) through grants U01-DK-61212, U01-DK-61230, U01-DK-61239, U01-DK-61242, and U01-DK-61254; from the National Center for Research Resources General Clinical Research Centers Program grants M01-RR-00036 (Washington University School of Medicine in St. Louis), M01-RR00043-45 (Children’s Hospital Los Angeles), M01-RR00069 (University of Colorado Denver), M01-RR00084 (Children’s Hospital of Pittsburgh), M01-RR01066 (Massachusetts General Hospital), M01-RR00125 (Yale University), and M01-RR14467 (University of Oklahoma Health Sciences Center); and from the National Center for Research Resources Clinical and Translational Science Awards UL1-RR-024134 (Children’s Hospital of Philadelphia), UL1-RR-024139 (Yale University), UL1-RR-024153 (Children’s Hospital of Pittsburgh), UL1-RR-024989 (Case Western Reserve University), UL1-RR-024992 (Washington University in St. Louis), UL1-RR-025758 (Massachusetts General Hospital), and UL1-RR-025780 (University of Colorado Denver).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. G.J.K. and N.H.W. researched data and wrote the article. L.P. researched data and reviewed and edited the article. K.J.N., R.S.G., and S.M.W. researched data, contributed to discussion, and reviewed and edited the article. L.A.B. and B.L. contributed to discussion and reviewed and edited the article. L.P. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented at the International Diabetes Federation's 2015 World Diabetes Congress, Vancouver, Canada, 30 November–4 December 2015.
Footnotes
Clinical trial reg. no. NCT00081328, clinicaltrials.gov.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc15-1206/-/DC1.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Centers for Disease Control and Prevention. Fast facts on diabetes: national diabetes fact sheet, 2011 [Internet], 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Available from http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed 30 June 2014
- 2.Dabelea D, Mayer-Davis EJ, Saydah S, et al.; SEARCH for Diabetes in Youth Study . Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311:1778–1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macintosh MC, Fleming KM, Bailey JA, et al. . Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: population based study. BMJ 2006;333:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Groen B, Links TP, van den Berg PP, et al. Similar adverse pregnancy outcome in native and nonnative Dutch women with pregestational type 2 diabetes: a multicentre retrospective study. ISRN Obstet Gynecol 2013;2013:361435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barbour LA. Changing perspectives in pre-existing diabetes and obesity in pregnancy: maternal and infant short- and long-term outcomes. Curr Opin Endocrinol Diabetes Obes 2014;21:257–263 [DOI] [PubMed] [Google Scholar]
- 6.Heerwagen MJ, Miller MR, Barbour LA, Friedman JE. Maternal obesity and fetal metabolic programming: a fertile epigenetic soil. Am J Physiol Regul Integr Comp Physiol 2010;299:R711–R722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ozalp S, Tanir HM, Sener T, Yazan S, Keskin AE. Health risks for early (< or =19) and late (> or =35) childbearing. Arch Gynecol Obstet 2003;268:172–174 [DOI] [PubMed] [Google Scholar]
- 8.Zeitler P, Epstein L, Grey M, et al.; TODAY Study Group . Treatment Options for type 2 Diabetes in Adolescents and Youth: a study of the comparative efficacy of metformin alone or in combination with rosiglitazone or lifestyle intervention in adolescents with type 2 diabetes. Pediatr Diabetes 2007;8:74–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Copeland KC, Zeitler P, Geffner M, et al.; TODAY Study Group . Characteristics of adolescents and youth with recent-onset type 2 diabetes: the TODAY cohort at baseline. J Clin Endocrinol Metab 2011;96:159–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zeitler P, Hirst K, Pyle L, et al.; TODAY Study Group . A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med 2012;366:2247–2256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics 2010;125:e214–e224 [DOI] [PubMed] [Google Scholar]
- 12.Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol 1996;87:163–168 [DOI] [PubMed] [Google Scholar]
- 13.Mathews TJ, Sutton PD, Hamilton BE, Ventura SJ. State disparities in teenage birth rates in the United States. NCHS Data Brief 2010;46:1–8 [PubMed] [Google Scholar]
- 14.Sayegh MA, Castrucci BC, Lewis K, Hobbs-Lopez A. Teen pregnancy in Texas: 2005 to 2015. Matern Child Health J 2010;14:94–101 [DOI] [PubMed] [Google Scholar]
- 15.Solomon-Fears C. Teenage pregnancy prevention: statistics and programs. Washington, DC, Congressional Research Service [Internet], 2014. Available from http://fas.org/sgp/crs/misc/RS20301.pdf. Accessed 23 May 2015
- 16.Daley AM. What influences adolescents’ contraceptive decision-making? A meta-ethnography. J Pediatr Nurs 2014;29:614–632 [DOI] [PubMed] [Google Scholar]
- 17.Richards MJ, Sheeder J. Adolescents: their futures and their contraceptive decisions. J Pediatr Adolesc Gynecol 2014;27:301–305 [DOI] [PubMed] [Google Scholar]
- 18.Stevens-Simon C, Kelly L, Singer D, Nelligan D. Reasons for first teen pregnancies predict the rate of subsequent teen conceptions. Pediatrics 1998;101:E8. [DOI] [PubMed] [Google Scholar]
- 19.Secura GM, Madden T, McNicholas C, et al. . Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med 2014;371:1316–1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001-2008. Am J Public Health 2014;104(Suppl. 1):S43–S48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tocce KM, Sheeder JL, Teal SB. Rapid repeat pregnancy in adolescents: do immediate postpartum contraceptive implants make a difference? Am J Obstet Gynecol 2012;206:481.e1–e7 [DOI] [PubMed] [Google Scholar]
- 22.Kitzmiller JL, Block JM, Brown FM, et al. . Managing preexisting diabetes for pregnancy: summary of evidence and consensus recommendations for care. Diabetes Care 2008;31:1060–1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guerin A, Nisenbaum R, Ray JG. Use of maternal GHb concentration to estimate the risk of congenital anomalies in the offspring of women with prepregnancy diabetes. Diabetes Care 2007;30:1920–1925 [DOI] [PubMed] [Google Scholar]
- 24.Aune D, Saugstad OD, Henriksen T, Tonstad S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. JAMA 2014;311:1536–1546 [DOI] [PubMed] [Google Scholar]
- 25.Watkins ML, Rasmussen SA, Honein MA, Botto LD, Moore CA. Maternal obesity and risk for birth defects. Pediatrics 2003;111:1152–1158 [PubMed] [Google Scholar]
- 26.Vrebosch L, Bel S, Vansant G, Guelinckx I, Devlieger R. Maternal and neonatal outcome after laparoscopic adjustable gastric banding: a systematic review. Obes Surg 2012;22:1568–1579 [DOI] [PubMed] [Google Scholar]
- 27.Fleming N, Ng N, Osborne C, et al. . Adolescent pregnancy outcomes in the province of Ontario: a cohort study. J Obstet Gynaecol Can 2013;35:234–245 [DOI] [PubMed] [Google Scholar]
- 28.Whitaker RC. Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics 2004;114:e29–e36 [DOI] [PubMed] [Google Scholar]
- 29.Catalano PM, Farrell K, Thomas A, et al. . Perinatal risk factors for childhood obesity and metabolic dysregulation. Am J Clin Nutr 2009;90:1303–1313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Catalano PM, McIntyre HD, Cruickshank JK, et al.; HAPO Study Cooperative Research Group . The Hyperglycemia and Adverse Pregnancy Outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care 2012;35:780–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patti ME. Intergenerational programming of metabolic disease: evidence from human populations and experimental animal models. Cell Mol Life Sci 2013;70:1597–1608 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.