Abstract
Purpose:
To find out the current physiotherapy practices in Intensive Care Unit (ICU) across Maharashtra.
Materials and Methods:
Study design was exploratory cross-sectional survey. Questionnaires were sent to the physiotherapists working in hospitals across Maharashtra state, India. Four weeks for completion of questionnaire was given in an attempt to ensure good response rates.
Result:
Of 200, 73 questionnaires were received representing a 36% response rate. The study revealed that 76% of the respondents were bachelors qualified, 15% were masters in physiotherapy with only 4% specialized in cardio-respiratory physiotherapy; 82% had <5 years experience in ICU. Almost 19% had not at all attended any seminars/workshops related to ICU management while 61% attended up to three within last 2 years. The availability of a physiotherapist during the night was affirmed by 63%, 58% responded initiation of physiotherapy to be “always physician referred” and 39% mentioned “physiotherapist initiated.” Almost 80% performed chest wall techniques, 86% positioning, 27% postural drainage, 5% manual hyperinflation, 12% application of nebulizer, and 56% bedsores management. Only 5% reported involvement in ventilator setting, 11% had their opinion sought before weaning from ventilator, 29% practiced noninvasive ventilation, 11% were involved in decision-making for extubation and 44% reported involvement in patient family education.
Conclusion:
The study showed that physiotherapists among the responding ICUs surveyed lack in experience and updated knowledge. Physician reference is necessary to initiate physiotherapy and there exists no established criteria for physiotherapy treatment in ICU. All physiotherapists were routinely involved in chest physiotherapy, mobilization, and positioning.
Keywords: Hospitals across Maharashtra, Intensive Care Units, physiotherapy practices
Introduction
Physical therapy is concerned with identifying and maximizing quality of life and movement potential within the spheres of promotion, prevention, treatment/intervention, habilitation and rehabilitation.[1] A physiotherapist assesses, plan and implement rehabilitative programs that improve or restore human motor function, maximize movement ability, relieve pain syndrome and treat or prevent physical challenges associated with injuries, disease and other impairments.[2]
An Intensive Care Unit (ICU) is a specially staffed and equipped hospital ward dedicated to the management of patients with life-threatening illnesses, injuries or complications. Role and responsibility of physiotherapist have been poorly defined in ICU. It was mentioned that they should be included in ICU team.[3] As per the recommendations of European Respiratory Society and European Society of Intensive Care Medicine (ESICM), there is a need to standardize pathways for clinical decision-making and education, and define the professional profile of ICU physiotherapists in more detail.[4] The aims of any physiotherapy program in the critical care areas is to apply advanced, cost-effective therapeutic modalities to decrease the patient's dependency on the ventilator, to improve residual function, to prevent the need for new hospitalizations and to improve the patient's quality of life.[5]
Factors influencing physiotherapy practices in Indian ICUs include awareness of techniques, availability of equipment, training or education of the physiotherapist, physiotherapist to patient ratio, presence of respiratory therapists, cultural differences, attitude of other professionals toward physiotherapy, evidence-based practice (EBP) considerations, medical management of the patient (such as sedation practices, setting ventilator parameters, and inclination for early tracheostomy), open versus closed ICUs, and case-mix of unit.[6]
The physiotherapy practices in ICUs historically include positioning, mobilization, manual hyperinflation, chest manipulation, suctioning, breathing and limb exercises, postural drainage.[7] Physiotherapy treatment, when started early, prevents weaning delay, limited mobility and total dependence on the ventilator. Therefore, weaning process and physiotherapy are two major interventions to speed up the patient's recovery.[8]
The outcome of physiotherapy treatment in ICU may vary with the degree to which physiotherapy services are available and the specific tasks that are performed by physiotherapists in the ICU. There is need to establish current physiotherapy practices in ICU. The objective of this study was to evaluate qualification of physiotherapists, hospital infrastructure available for physiotherapists, and the current physiotherapy practices in ICUs of hospitals across the state of Maharashtra, India.
Materials and Methods
Study design
An exploratory cross-sectional survey was carried out in multispecialty hospitals across Maharashtra state.
Participants
Physiotherapists working in ICUs in the hospitals having more than 10 ICU beds were recruited for the study. Physiotherapist with <1-year of experience in ICU were excluded.
Procedure
The study was approved by the Institutional Ethical Committee at Tilak Maharashtra Vidyapeeth Pune. Experts in the field of cardiorespiratory physiotherapy were consulted, and a questionnaire was prepared. A pilot study was done on 10 physiotherapists working in multispeciality hospitals. Postpilot study a few changes were made and a questionnaire was finalized with appropriate modifications.
Total 50 multispecality hospitals from 10 cities across Maharashtra state were shortlisted randomly from the National Accreditation Board of Hospital and Healthcare Providers and Medical Council of India websites. Questionnaires were mailed to the head of the physiotherapy department of shortlisted hospitals. Physiotherapists working in ICU were requested to fill the questionnaire and revert via mail. Aim and objectives of the study were clearly stated in the cover letter attached to the questionnaire. The respondents were made clear that the identity of the participants will not be disclosed and the information gathered would be used for research purpose and informed written consents from the participating institutions were obtained. The questionnaire included hospital information (number of beds in hospital and ICU beds), therapist profile (qualification, experience, and hours of working) and role of physiotherapists in ICU (chest manipulation, positioning, mobilization, and postural drainage, application of nebulizer etc.). A period of 4 weeks was given for completion of a questionnaire in an attempt to ensure good response rates.
Results
Of 200, 73 questionnaires were received (36% response rate).
Table 1 indicates responders details such as a total number of ICU beds and availability of physiotherapist during the night. This survey included private, government, and semi-government hospitals. Among the respondents, 68% were from private hospitals, 27% from government, and 4% from semi-government hospitals. It was found that 63% of physiotherapists were available during the night, with 49% as a resident and 13% as an “on-call physiotherapist” and about 36% physiotherapist responded that there is no therapist available during the night. Table 2 indicates physiotherapist's profile that includes the age, qualification, years of experience, hours of working, average number of patients treated, and seminar attended.
Table 1.
Responders’ details
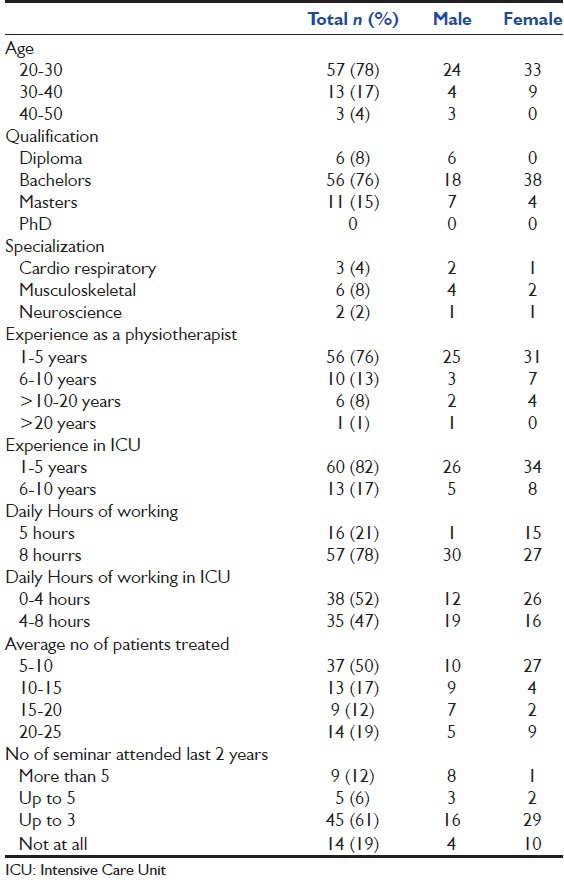
Table 2.
Physiotherapists’ profile
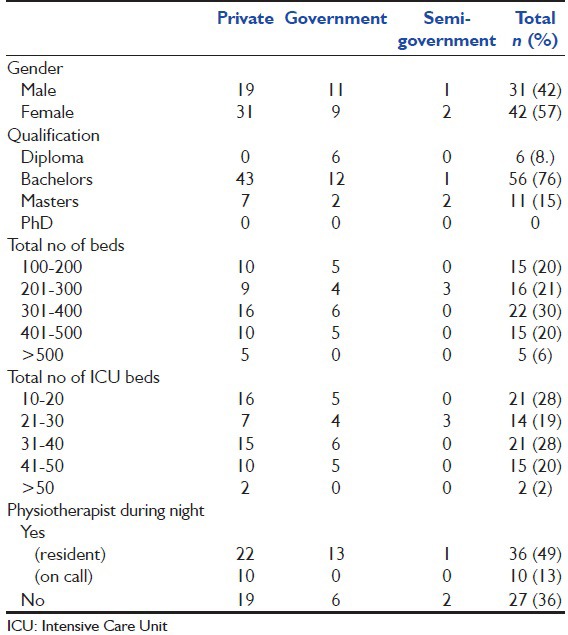
Figure 1 indicates the physiotherapy practices which involve patient screening and assessment, ventilator setting, physiotherapy techniques, and the role of physiotherapist during extubation. Majority of respondents (80%) performed chest wall techniques, 86% positioning, 61% joint mobilization, 27% postural drainage, 5% manual hyperinflation, 19% closed suctioning, 50% open suctioning, 12% application of nebulizer pre- and post-treatment, and 56% management of bedsores. It was noted that 91% physiotherapist always go through medical/investigations reports and 95% physiotherapist assess vital parameters before treatment. Only 44% physiotherapists were involved in patient and family education regarding the condition and prognosis of the patient's health.
Figure 1.
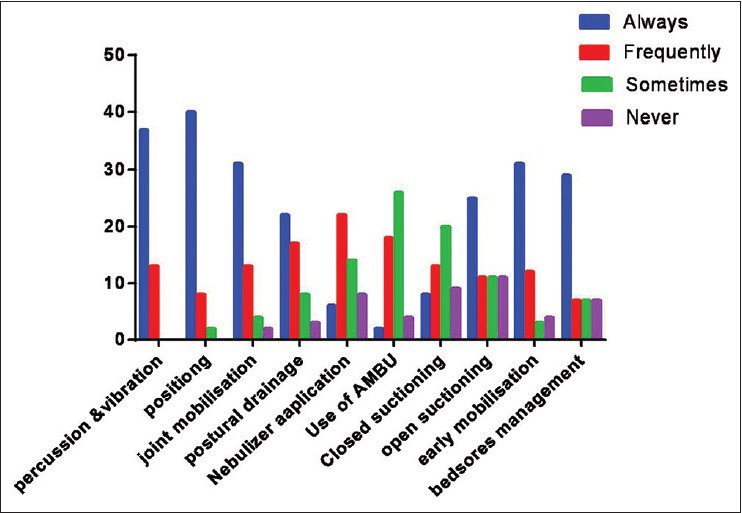
Physiotherapy techniques
Discussion
This study was done to establish current physiotherapy practices in ICU across Maharashtra state, India. It was observed that the physiotherapists working in ICU vary in qualification, experience, clinical knowledge, and skills. In this survey, it was observed that 78% of the respondents were aged between 20 and 30 years while 82% had <5 years of ICU experience. While assessing qualification of physiotherapists working in ICU, it was observed that 76% of the respondents were bachelors and 15% masters in physiotherapy. These results contrast with the survey conducted by Kumar et al. in 2007[8] who reported that 59% were postgraduate qualified physiotherapist working in ICU.
Regular update of knowledge and skills, continuing medical education (CME) carries prime importance as far as ICU management is concerned. However, in this survey, it was found that almost 19% of physiotherapists have not at all attended any seminars/workshops/CME related to ICU management while 61% attended up to three seminars, 6% attended up to five and only 12% attended more than five seminars within last 2 years.
According to this survey, 49% of ICUs had a resident physiotherapist, and 13% had “on-call” service available during the night. The survey conducted by Kumar et al.[8] showed that 24% of ICUs had a resident physiotherapist available on-site during the night, and 79% of physiotherapists were available on-call. Norrenberg and Vincent[9] have reported that 34% had a physiotherapist available during the night in Europe, whereas 83% physiotherapist indicated the availability of on-call service during night in South Africa[10] while Chaboyer et al.[11] reported that 90% of ICUs in Australia had physiotherapists available during the week, and 25% had “on-call” service only on weekends.
While assessing the referral system being practiced in ICUs, 58% of the respondents mentioned it to be “always physician referred” and 39% responded to be physiotherapist initiated, whereas, only 58% respondents mentioned that there is “established criteria” for the initiation of physiotherapy in ICU. The referral for physiotherapy varied with the referring professional, their interest, understanding and interaction with the physiotherapist, their ideas and concepts about physiotherapy. The survey conducted by Shimpi et al.[12] reported that 95.5% of doctors from all the groups made referrals to physiotherapy, but only 12.2% did not include a medical diagnosis as they expected the physiotherapists to diagnose and decide the patient's treatment. This suggests that although the role of the physiotherapist in ICU is increasing, the referral appears to be largely physician initiated.
EBP is the explicit use of current best evidence in making decisions about the care of individual patients and is a concept of growing importance for physiotherapy. According to our study, 53% respondents practiced EBP for decision-making or planning the treatment. In a survey conducted by Akinbo et al. in Nigeria[13] 98% responded that EBP improves the quality of patient care, 99% mentioned that they needed to increase the use of evidence in their daily practice and 88% believed that evidence helps in decision-making.
While assessing physiotherapy practice pattern in ICU, it was observed that majority of physiotherapists (80%) always performed chest wall techniques. Kumar et al.[8] in his multicenter survey found that 91% physiotherapists performed chest wall techniques in India, 79% in Australia[11] and 98% in Europe.[10] Physiotherapist plays a vital role in the clearance of secretions during weaning process. The potential roles of the physiotherapist in weaning a patient from invasive ventilation to spontaneously breathing includes numerous techniques that are based on expertise and knowledge. These roles involve the decision-making such as when weaning should begin, weaning strategies, mode of ventilation, and whether use of noninvasive ventilation (NIV) is appropriate.
European Society of Intensive Care Medicine (ESICM) has recommended that “therapist-driven weaning protocols” can be implemented dependent on physician staffing in the ICU, and respiratory muscle training should be considered in patients with respiratory muscle weakness and weaning failure.[4] It was observed that 5% of the respondents were always involved in setting ventilator parameters while 11% opinions were always taken before weaning a patient from the mechanical ventilator. Only 11% respondants were involved in decision-making in extubation, 25% performed suctioning during extubation, and 29% always applied NIV. Kumar et al.[8] reported that 10% of respondents were involved in setting ventilator parameters and 18% were involved in weaning. In Europe,[10] 12% of physiotherapist played an active role in the adjustment of mechanical ventilation, 22% in weaning from mechanical ventilation, and 25% in extubations.
In this survey, 44% physiotherapists were always involved in “patient and family education” and generating awareness regarding the disease conditions and their prognosis. A good interaction between physiotherapist and patient may reduce patient anxiety and discomfort, thus, enhancing patient cooperation.
Overall in this survey, diversities were observed in physiotherapy practices within hospitals across Maharashtra state, India. This diversity needs to be explored by future study for variables such as physiotherapist's qualification, years of experience, attendance of seminars, type of hospital, referral system, availability of physiotherapist during night and preferred physiotherapy techniques.
Since the number of participants and the response rate were low, the results should be validated by a larger study ensuring higher response. Prompts or reminders to participants would have resulted in better response rate. Studies should also be carried out generating information on the hospital policies for physiotherapy practicesin the ICUs. The effectiveness of physiotherapy in ICUs should be evaluated considering diversities in physiotherapy practice.
Conclusion
This survey showed that physiotherapist among the responding ICUs surveyed lack in experience and updated knowledge. Physician reference is necessary to initiate physiotherapy, and there exist no established criteria for physiotherapy treatment in ICU. All physiotherapists were routinely involved in chest wall techniques, mobilization, and positioning.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank all the hospitals and participant physiotherapists for their contribution in this study.
References
- 1.World Confederation for Physical Therapy. Policy Statement: Description of Physical Therapy. 2011. [Last accessed on 2015 Aug 10]. Available from: http://www.wcpt.org/policy/ps-descriptionPT .
- 2.Classification of Health Workforce Statistics, World Health Organization. [Last accessed on 2015 Aug 21]. Available from: http://www.who.int/hrh/statistics/Health_workers_classification.pdf .
- 3.Stiller K. Physiotherapy in intensive care: Towards an evidence-based practice. Chest. 2000;118:1801–13. doi: 10.1378/chest.118.6.1801. [DOI] [PubMed] [Google Scholar]
- 4.Gosselink R, Bott J, Johnson M, Dean E, Nava S, Norrenberg M, et al. Physiotherapy for adult patients with critical illness: Recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med. 2008;34:1188–99. doi: 10.1007/s00134-008-1026-7. [DOI] [PubMed] [Google Scholar]
- 5.Clini E, Ambrosino N. Early physiotherapy in the respiratory Intensive Care Unit. Respir Med. 2005;99:1096–104. doi: 10.1016/j.rmed.2005.02.024. [DOI] [PubMed] [Google Scholar]
- 6.Bhat A, Chakravarthy K, Rao BK. Chest physiotherapy techniques in neurological Intensive Care Units of India: A survey. Indian J Crit Care Med. 2014;18:363–8. doi: 10.4103/0972-5229.133890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones AY, Hutchinson RC, Oh TE. Chest physiotherapy practice in Intensive Care Units in Australia, the UK and Hong Kong. Physiother Theory Pract. 1992;8:39–47. [Google Scholar]
- 8.Kumar JA, Maiya AG, Pereira D. Role of physiotherapists in Intensive Care Units of India: A multicenter survey. Indian J Crit Care Med. 2007;11:198–203. [Google Scholar]
- 9.Norrenberg M, Vincent JL. A profile of European Intensive Care Unit physiotherapists. European Society of Intensive Care Medicine. Intensive Care Med. 2000;26:988–94. doi: 10.1007/s001340051292. [DOI] [PubMed] [Google Scholar]
- 10.Van Aswegen H, Potterton J. A pilot survey of the current scope of practice of South African physiotherapists in Intensive Care Units. South Afr J Physiother. 2000;61:17–21. [Google Scholar]
- 11.Chaboyer W, Gass E, Foster M. Patterns of chest physiotherapy in Australian Intensive Care Units. J Crit Care. 2004;19:145–51. doi: 10.1016/j.jcrc.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 12.Shimpi A, Writer H, Shyam A, Dabadghav R. Role of physiotherapy in India – A cross-sectional survey to study the awareness and perspective among referring doctors. J Med Thesis. 2014;2:11–5. [Google Scholar]
- 13.Akinbo S, Odebiyi D, Okunola T, Aderoba O. Evidence-based practice: Knowledge, attitudes and beliefs of physiotherapists in Nigeria. Internet J Med Inform. 2008;4:2. [Google Scholar]


