Abstract
Fat embolism syndrome (FES) typically consists of a triad of neurological, pulmonary, and cutaneous symptoms. There exist few case reports of FES involving central nervous system (CNS) only without pulmonary involvement. In most of such cases, CNS involvement is partial, and patients recover fully neurologically within days. We report a rare and unusual case of massive cerebral fat embolism that led to brain death in trauma patient.
Keywords: Brain death, fat embolism, trauma
Introduction
Subclinical fat embolism is common in trauma patients with long bone and pelvic fractures, but not all cases of fat embolism progress to fat embolism syndrome (FES). The incidence of FES is around 3–4%.[1] FES is characterized by various central nervous system, respiratory, cutaneous, and hematological manifestations. The neurological symptoms can be focal or diffuse,[2] and most of the times exist with respiratory symptoms. There are only few reports of FES without pulmonary involvement, and in most of the cases, it is reversible with dramatic recovery. There exists only one report in which fat embolism led to brain death. We report a case of massive cerebral fat embolism (CFE) leading to brain death without clinical pulmonary involvement.
Case Report
A 26-year-old male presented to our Emergency Department after sustaining road traffic accident with complaints of pain and deformity in the right leg and abrasion over the forehead. He had no history of loss of consciousness, ENT bleed, vomiting, or convulsion. He was conscious, oriented with normal breathing and was hemodynamically stable but tachycardic. Initial resuscitation with fluids and blood was done. As per protocol, computed tomography (CT) head was done, which was normal. X-ray of the right lower limb revealed a closed segmental fracture shaft of the femur, fracture both bones right leg, and fracture of the 1st and 2nd distal phalanx for which closed traction was applied. He had no other injuries and was shifted to ward.
Twelve hours later, he became agitated and restless for which he was given some sedation in the ward. Few hours later, the patient became drowsy not responding verbally to commands. His Glasgow Coma Scale (GCS) decreased to E3V1M5. Arterial blood gas (ABG) was done which did not show any abnormalities (pH - 7.45, PCo2-31 mmHg, PO2-211 mmHg, Na - 132 mEq/l, K - 3.5 mEq/l, glucose - 164 mg/dl, HCO3-23.6, BE - 2.5, on face mask), and he was shifted to Intensive Care Unit (ICU). In ICU, the patient developed generalized tonic clonic convulsions. Intravenous midazolam was given, and he was immediately intubated and connected to ventilator. CT scan head was repeated which did not show any abnormality [Figure 1]. Conservative management was continued, and external fixator was applied for fracture femur. Twenty-four hours later, fine petechial rash developed in his upper chest and axilla. Bilateral lower conjunctival petechiae were also present. Urine analysis revealed no fat globules, and GCS deteriorated to E1VTM2. Pupils were dilated but reacting to light. ABG analysis did not show hypoxemia or electrolyte abnormalities. Conservative management continued with the suspicion of fat embolism. Six hours later, the patient suddenly deteriorated to E1VTM1 with absent brainstem reflexes. Magnetic resonance imaging (MRI) brain was done, which revealed massive fat embolism [Figure 2] and bilateral internal carotid artery flow cut-off [Figure 3]. The patient was declared brain dead after positive apnea test.
Figure 1.
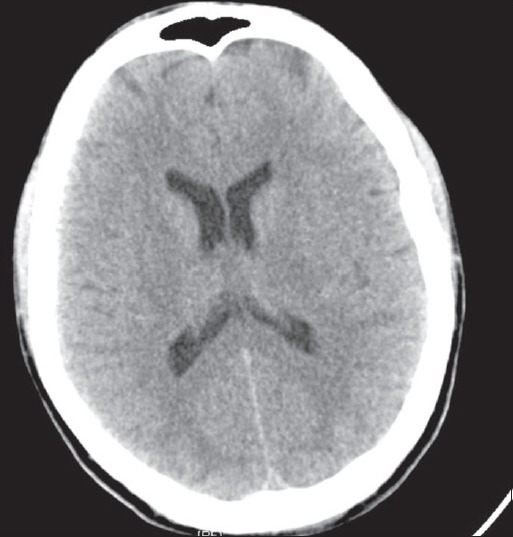
Normal computed tomography scan brain
Figure 2.
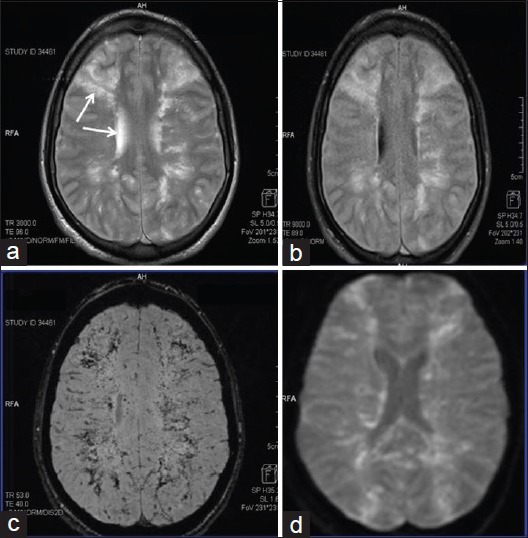
(a and b) T2-weighted and fluid, attenuated inversion recovery sequences show illdefined hyperintensity seen involving bilateral superficial and deep white matter with periventricular confluences, blooming on susceptibility weighted images (c) and restricted diffusion on diffusion-weighted images (d) suggestive of fat embolism
Figure 3.
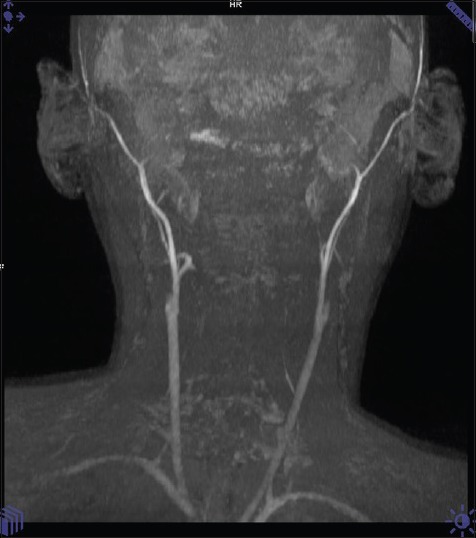
Diffuse cerebral edema present with nonvisualization of intracranial Internal carotid artery and its branches consistent with brain death
Discussion
FES is a severe posttraumatic complication usually associated with long bone or pelvic fractures. Features of fat embolism become typically apparent 24–72 h after trauma,[3,4] but in some cases, early manifestation occurs. Diagnosis of FES is difficult and requires high amount of suspicion, based on history and classical triad of hypoxemia, neurological symptoms, and petechial rash. These petechiae occur in only 20–50% of patients and resolve quickly. Gurd's and Wilson's criteria are often used to make diagnosis. It consists of major and minor criteria.
Major criteria
Respiratory insufficiency
Cerebral involvement
Petechial rash.
Minor criteria
Tachycardia
Fever
Jaundice
Retinal changes
Renal changes
Microglobulinemia
Thrombocytopenia
Elevated erythrocyte sedimentation rate
Anemia.
One major and four minor criteria must be present to formally diagnose FES.
Neurological manifestations of FES initially manifests as agitated delirium but may progress to stupor, seizures, or coma.[5] In our case, the patient started having neurological features within 16 h of trauma. He became initially agitated, restless and then developed generalized tonic clonic seizure, following a period of reduced level of consciousness. There was no hypoxemia, but diagnosis was facilitated by typical petechial rash in the axilla, chest, and conjunctiva.
Generally, CT scan brain is normal in patients with isolated CFE. Magnetic resonance imaging is more sensitive and demonstrates multiple small hyperintense, intracerebral lesions.[6] In our case also, CT scan brain was normal, and MRI showed extensive cortical and brain stem fat embolism which led to brain death. There are few differential diagnosis of disseminated hyperintense lesions on T2-weighted scans which include diffuse axonal injury, areas of vasogenic edema associated with microinfarcts, and demyelinating diseases[6] which were ruled out by history and clinical scenario, in our case.
Most patients with FES show good recovery. Residual neurological deficits range from cognitive dysfunction, subtle personality changes to memory loss, and sometimes focal deficits. The mortality ranges from 5% to 15% and is usually secondary to pulmonary involvement.[7] CFE without pulmonary involvement has been described earlier also, but none of the cases deteriorated to brain death due to embolism. Bracco et al.[8] reported a case of massive cerebral embolism in which the patient remained comatose until 6 months but had normal brainstem reflexes. Walshe et al.[9] also reported a case of CFE causing brain death, but the mechanism of sudden brainstem coning in their case was different. They had used large doses of acetazolamide for raised intraocular pressure which led to metabolic acidosis and compensatory hypocapnia. Unexpected normocapnia during weaning precipitated coning in their patient. The patient, in our case, was normocapnic on ventilator throughout.
Management of FES requires early immobilization of fracture, symptomatic management of respiratory, cardiovascular, and neurological abnormalities. External fixator was applied for immobilization in our case, but there was rapid evolution of FES, and the patient deteriorated to brain death due to massive cerebral embolism.
This case presents the fact that not all the neurological complications in fat embolism are reversible and can be as drastic as brain death. Moreover, it also reinforces the fact that any neurological symptoms in trauma patient with long bone fractures should raise the suspicion of fat embolism, and fixation of the fractures should be done as early as possible to prevent such complication.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Parisi DM, Koval K, Egol K. Fat embolism syndrome. Am J Orthop (Belle Mead NJ) 2002;31:507–12. [PubMed] [Google Scholar]
- 2.Bardana D, Rudan J, Cervenko F, Smith R. Fat embolism syndrome in a patient demonstrating only neurologic symptoms. Can J Surg. 1998;41:398–402. [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta A, Reilly CS. Fat embolism. Contin Educ Anaesth Crit Care Pain. 2007;7:148–51. [Google Scholar]
- 4.Jorens PG, Van Marck E, Snoeckx A, Parizel PM. Nonthrombotic pulmonary embolism. Eur Respir J. 2009;34:452–74. doi: 10.1183/09031936.00141708. [DOI] [PubMed] [Google Scholar]
- 5.Metting Z, Rödiger LA, Regtien JG, van der Naalt J. Delayed coma in head injury: Consider cerebral fat embolism. Clin Neurol Neurosurg. 2009;111:597–600. doi: 10.1016/j.clineuro.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Parizel PM, Demey HE, Veeckmans G, Verstreken F, Cras P, Jorens PG, et al. Early diagnosis of cerebral fat embolism syndrome by diffusion-weighted MRI (starfield pattern) Stroke. 2001;32:2942–4. [PubMed] [Google Scholar]
- 7.Mellor A, Soni N. Fat embolism. Anaesthesia. 2001;56:145–54. doi: 10.1046/j.1365-2044.2001.01724.x. [DOI] [PubMed] [Google Scholar]
- 8.Bracco D, Favre JB, Joris R, Ravussin A. Fatal fat embolism syndrome: A case report. J Neurosurg Anesthesiol. 2000;12:221–4. doi: 10.1097/00008506-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Walshe CM, Cooper JD, Kossmann T, Hayes I, Iles L. Cerebral fat embolism syndrome causing brain death after long-bone fractures and acetazolamide therapy. Crit Care Resusc. 2007;9:184–6. [PubMed] [Google Scholar]


