Abstract
Recurrent extensive ocular surface squamous neoplasia (OSSN) with orbital invasion can be successfully managed with external radiotherapy using electrons resulting in eye and vision salvage. We report a case of right eye recurrent OSSN in an immunocompetent adult Indian male, with extensive orbital involvement. The patient had two previous surgical excisions with recurrent disease. At this stage, conventionally exenteration is considered the treatment modality. However, he was treated with 5040 cGy radiotherapy (15eV electrons) resulting in complete disease regression. At the end of 3 years follow-up, the patient was disease free, maintained a vision of 20/25, with mild dry eye, well-managed with topical lubricants. Extensive OSSN with orbital invasion does not always need exenteration. External beam electron radiotherapy provides a noninvasive cure with organ and vision salvage and should be considered in extensive OSSN not amenable to simple excision biopsies. Long-term studies to evaluate the effect of radiation on such eyes are suggested.
Keywords: Electron beam, ocular surface squamous neoplasia, radiotherapy
Ocular surface squamous neoplasia (OSSN) encompasses corneal and conjunctival squamous cell proliferations ranging from squamous dysplasia to carcinoma in situ to invasive carcinoma. Simple excision biopsy, with adequate margins and alcohol kerato-epitheliectomy, clear margin of 4 mm from tumor border, careful handling of carcinomatous tissue to avoid seeding, and use of triple freeze-thaw has been the conventional recommended technique with more than 95% success rates. Brachytherapy is also a good option for cases with localized scleral involvement. However, recent literature confirms the effectiveness of noninvasive techniques such as chemotherapy in the majority of the lesions.[1] The treatment options for extensive, recurrent OSSN with orbital invasion (American Joint Committee on Cancer [AJCC] T4) remain largely unchanged with exenteration being most widely acceptable and recommended option. We report a case of invasive recurrent OSSN managed using external radiotherapy with electrons resulting in eye and vision salvage with complete disease cure. To the best of our knowledge based on literature search, this radiation technique has not been used before for similar extensive OSSN with orbital extension.
Case Report
A 30-year-old Indian male presented with recurrent fleshy growth involving the conjunctiva and cornea of the right eye over last 3 months. The same lesion was previously excised twice over the last 4 years elsewhere. On examination, his visual acuity in the right eye was 20/25. The central cornea was clear; the peripheral 2 mm of the cornea was opaque. A pink fleshy growth involved the entire bulbar conjunctiva with extension up to the inferior fornix and extended 7 clock hours from 3 o’clock to 10 o’clock position [Fig. 1]. Rest of the ocular examination was unremarkable. There was no regional lymphadenopathy. Computerized tomography showed a hyperdense diffuse mass anteriorly involving the outer coats of the right eye, extending beyond the equator into the orbit. There was no intraocular or intraconal extension. The AJCC grading of the lesion was T4a N0 M0. He was not immunocompromised or having HIV infection.
Figure 1.
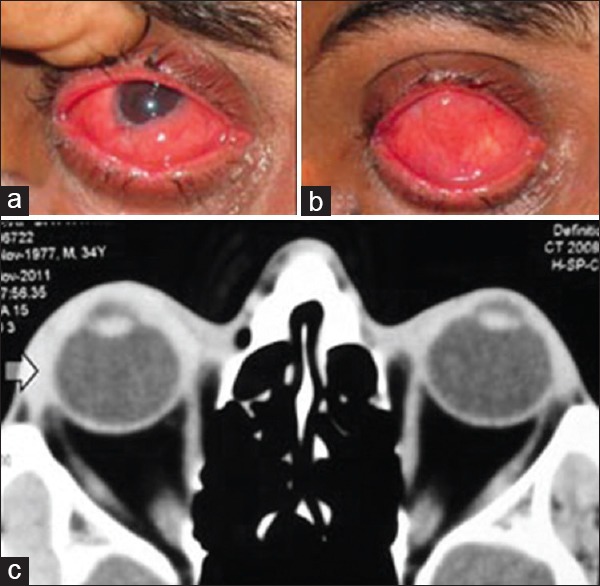
Extensive ocular surface squamous neoplasia of right eye involving (a) 7 clock hours of limbus (b) including the inferior fornix (as seen on upgaze) (c) orbital soft tissue with a postequatorial component as seen on computed tomography scan orbits, axial view
Incision biopsy was performed to confirm the histological diagnosis of OSSN. Diffuse infiltrative scleral involvement with extension into anterior orbit was present at 3 o’clock to 6 o’clock position for about 10 mm from the limbus. This was obvious even during the surgical procedure and complete excision with margins was not feasible. Still most of the clinically evident, gross lesion was excised. Considering his young age and good vision in his eye, exenteration was deferred, and radiation treatment was planned for conservation of eye and vision. Two weeks after surgery, the patient was treated with 15 MeV electrons external beam radiotherapy with linear accelerator to reach a cumulative dose of 5040 cGy in 28 fractions over 5½ weeks to the right eye. Radiation was given to the entire socket with 1 cm margin beyond the orbital rim using single head on field technique with custom made lead cut out defining the field of radiation and corneal shielding. During treatment, there was mild epiphora and conjunctivitis (acute reactions) which were self-limiting and subsided within 3 weeks of treatment completion.
At 3 months follow-up, the disease showed complete clinical and radiological regression. At 4 years follow-up, the patient had no recurrence and maintained a visual acuity of 20/25 [Fig. 2]. The patient developed mild dry eye that was well-controlled on topical lubricants. No other long-term radiation-induced side effects were noted until now. The patient has been advised annual follow-ups to evaluate for disease recurrence and long-term radiation-induced side effects, especially retinopathy.
Figure 2.
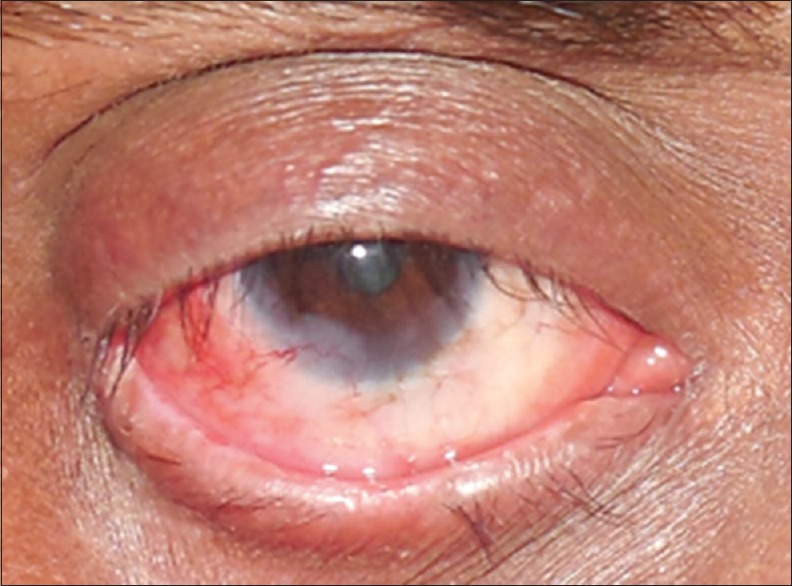
Complete disease regression after radiotherapy at 2 years follow-up
Discussion
The clinical spectrum of OSSN is varied, ranging from localized limbal disease to extensive orbital involvement. For lesions confined to the conjunctiva, excision biopsy with clear margins is recommended. In case of residual disease involving the sclera, adjuvant, topical chemotherapy like mitomycin C, 5-fluorouracil, or plaque brachytherapy is employed.[1] Topical chemotherapy causes long-term toxicity to the epithelium. More recently, noninvasive techniques such as topical and subconjunctival interferon have been employed as the first line treatment for OSSN confined to the conjunctiva.[2] They are better tolerated than the conventional chemotherapeutic agents. There is no definitive guideline in literature regarding superiority of one adjuvant modality versus other (chemotherapy, interferon, or radiotherapy).
However, in case of extensive OSSN with orbital invasion (AJCC T4), the conventionally accepted treatment remains exenteration. This leads to removal of eye with loss of vision and profound psychosocial implications due to the disfigurement and loss of self-esteem, and this may not always be amenable to rehabilitation easily by prosthesis.
Radiation as an adjuvant treatment after surgery has been described in various forms for OSSN, which includes protons, brachytherapy, orthovoltage external radiation, and stereotactic radiotherapy. Proton external radiotherapy has been recently used in three patients with OSSN, described in two case reports; showing encouraging results.[3,4] However, the nonavailability, cost effectiveness, and long-term outcome data in routine practice still remain a significant limitation.[5] In one report, orthovoltage radiotherapy for medial canthal basal cell carcinomas has been proven to be effective but is unavailable in the most modern radiotherapy centers in India.[6] Brachytherapy can be an excellent alternative in cases restricted to the ocular coats, especially when there is residual scleral disease after primary excision.[7] However, in the current case, the tumor involved the anterior orbit as well, and moreover, the central corneal was free from disease. So attempting to plaque, such a lesion would not be feasible, as orbital extension would be shielded by the plaque itself. There would also be issues with higher doses on surface leading to more scarring and scleral thinning in an already compromised sclera with multiple previous surgeries and infiltrative disease itself. Hence, brachytherapy would not have been a suitable option for the current case.
Electrons are the special particulate type of radiation which deliver high dose of ionizing radiation to the tumor without much damage to surrounding tissues. The dosimetric advantage of electrons over photons is well described for superficial tumors. Unlike photons, electrons will have very minimal exit dose beyond the tumor, and so side effects to the other eye and brain behind the treated eye are avoided.[8] These are advantages similar to those expected with the use of protons. Proton radiation delivers more three-dimensional conformal dose than electrons, especially sparing lens and posterior eye structures. Thought was given to consider the stereotactic radiation, but considering diffuse involvement of outer coats of more than half of the eye, with application of required margins in radiotherapy treatment planning; the treatment volume would have practically covered the entire eye. Stereotactic radiotherapy, however, precise, always has exit dose to consider that would cause more damage to the normal structures (including contralateral eye and brain). Electrons have the inherent capacity of treating the surface with no exit dose. Hence, in cases such as these, electrons fare better over stereotactic radiotherapy by avoiding the collateral damage that would have been caused by exit dose. Furthermore, electron radiotherapy is inexpensive and more widely available, as compared to stereotactic radiotherapy or protons. Hence in superficial tumors such as OSSN with extensive orbital involvement, electron therapy may be comparable to proton beam therapy and has an advantage of wider availability and low cost without compromising outcomes.
Although electrons have been traditionally used for all superficial tumors and adequate long-term data is available regarding dosimetry and safety; this is a first report in best of our knowledge describing successful use for OSSN.[8] The only long-term side effect seen in this patient was dry eye, which is being effectively managed with tear substitution alone.
External radiotherapy using electrons is an effective treatment option for invasive orbital OSSN. It helps to preserve the eye and vision while providing excellent disease control and cosmesis. The side effects of radiotherapy using electrons are minimal. However, long-term studies involving larger number of patients are recommended to look into the efficacy and side effect profile in detail.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nanji AA, Sayyad FE, Karp CL. Topical chemotherapy for ocular surface squamous neoplasia. Curr Opin Ophthalmol. 2013;24:336–42. doi: 10.1097/ICU.0b013e3283622a13. [DOI] [PubMed] [Google Scholar]
- 2.Shields CL, Kaliki S, Kim HJ, Al-Dahmash S, Shah SU, Lally SE, et al. Interferon for ocular surface squamous neoplasia in 81 cases: Outcomes based on the American Joint Committee on Cancer classification. Cornea. 2013;32:248–56. doi: 10.1097/ICO.0b013e3182523f61. [DOI] [PubMed] [Google Scholar]
- 3.El-Assal KS, Salvi SM, Rundle PA, Mudhar HS, Rennie IG. Treatment of invasive ocular surface squamous neoplasia with proton beam therapy. Eye (Lond) 2013;27:1223–4. doi: 10.1038/eye.2013.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramonas KM, Conway RM, Daftari IK, Crawford JB, O’Brien JM. Successful treatment of intraocularly invasive conjunctival squamous cell carcinoma with proton beam therapy. Arch Ophthalmol. 2006;124:126–8. doi: 10.1001/archopht.124.1.126. [DOI] [PubMed] [Google Scholar]
- 5.Gornall J. Proton beam therapy: More than a leap of faith? BMJ. 2012;345:e4917. doi: 10.1136/bmj.e4917. [DOI] [PubMed] [Google Scholar]
- 6.Krema H, Herrmann E, Albert-Green A, Payne D, Laperriere N, Chung C. Orthovoltage radiotherapy in the management of medial canthal basal cell carcinoma. Br J Ophthalmol. 2013;97:730–4. doi: 10.1136/bjophthalmol-2012-302991. [DOI] [PubMed] [Google Scholar]
- 7.Arepalli S, Kaliki S, Shields CL, Emrich J, Komarnicky L, Shields JA. Plaque radiotherapy in the management of scleral-invasive conjunctival squamous cell carcinoma: An analysis of 15 eyes. JAMA Ophthalmol. 2014;132:691–6. doi: 10.1001/jamaophthalmol.2014.86. [DOI] [PubMed] [Google Scholar]
- 8.Hogstrom KR, Almond PR. Review of electron beam therapy physics. Phys Med Biol. 2006;51:R455–89. doi: 10.1088/0031-9155/51/13/R25. [DOI] [PubMed] [Google Scholar]


