Sir,
Primary pancreatic hydatid cyst is a rare entity; the presentation as an asymptomatic pancreatic space-occupying lesion is even rarer. Caused by Echinococcus granulosus, the disease is prevalent in the Mediterranean region, Africa, South America, Australia, and the Middle East. We report two cases of pancreatic hydatid cyst that presented as pancreatic mass.
The first case was of a 48-year-old man who was diagnosed with pancreatic space-occupying lesion since last 10 years, and was kept on a follow-up. The patient was asymptomatic. Ultrasound showed a pancreatic cyst suggestive of infective etiology. Subsequently, an endoscopic ultrasound (EUS)-guided fine-needle aspiration (FNA) was done.
The second case was of a 35-year-old woman who presented with a history of low-grade fever since 2 months, and ultrasound showed a pancreatic cystic mass.
Microscopic examination of Giemsa stained smear of both the cases in low power examination showed a necrotic background with dispersed laminated membranes [Figures 1a and b]. On careful evaluation on higher power, there were hooklets and scolices. Scolices were seen with attached two rows of hooklets [Figure 1c]. These were also appreciated in periodic acid-Schiff (PAS) and Grocott silver stains [Figures 1c and d, 2a and b]. Additionally, Ziehl-Neelsen (ZN) and PAS stain tests were done to rule out the possibility of tuberculosis and any other fungal infection. A diagnosis of primary hydatid cyst of pancreas was given.
Figure 1.
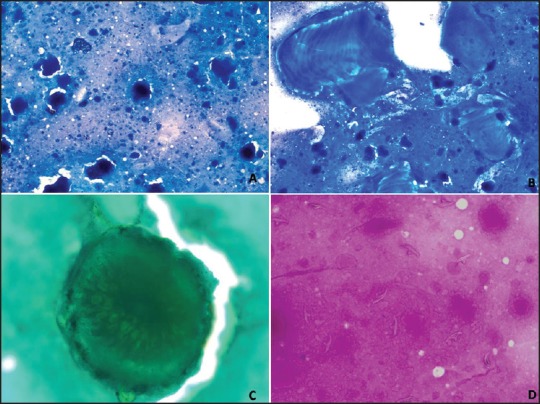
(Case 1): (a) Smear shows a necrotic background (Giemsa, ×100); (b) Laminated membrane of hydatid cyst. (Giemsa, ×400); (c) Scolex with rows of hooklets. (Gomori methnamine silver stain, ×1000); (d) Dispersed hooklets. (Periodic-acid Schiff stain, ×400)
Figure 2.
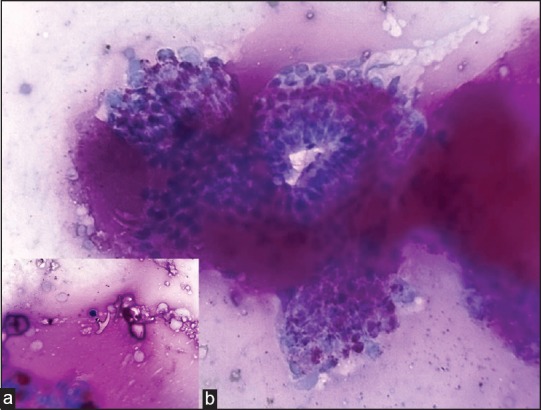
(Case 2): (a) Monolayered epithelial sheets with mucin. (Periodicacid Schiff stain, ×400); (b) Hooklets attached to mucin lakes. (Periodic-acid Schiff stain, ×1000)
There are only two cases of cytological diagnosis of hydatid cyst in pancreas reported in indexed journals. We report these two cases to highlight the importance of EUS-guided FNAC in diagnosing infective cystic lesion that mimic a neoplastic process otherwise.
Hydatid cyst is an infective disease of humans and animals seen more commonly in some specific geographic regions of the world. The primary route of human infection is the ingestion of E. granulosus eggs through consumption of vegetables that are contaminated with dog feces. While liver involvement is the most common manifestation, pancreatic hydatid cyst has been reported in 0.25-0.75% of the cases.[1] The head of the pancreas is the most common location (57%), followed by the corpus (24%) and the tail (19%).[2,3] Possible sources of infestation include hematogenous dissemination, local spread via pancreaticobiliary ducts, and peripancreatic lymphatic invasion.[2,3]
Preoperative diagnosis of pancreatic hydatid cyst is difficult as it may be mistaken for pseudocysts, cystadenocarcinoma, and congenital or post-traumatic cysts.[4] Hydatid cyst should be considered a differential diagnosis of pancreatic cystic lesions.
EUS has emerged as an effective technique to gain access to retroperitoneal organs such as pancreas. EUS-guided FNA has increased the probability to identify hydatid cyst in the pancreas that has been considered a rare site so far. This is an effective and safe procedure for diagnosing pancreatic lesions, be it malignant or benign.[5]
EUS findings alone has limitations regarding definitive diagnosis; however, fluid aspiration can help in differentiating malignant cystic lesions.
Cytological evaluation of EUS-guided FNA emerges as an important diagnostic tool, preventing unnecessary surgical intervention. Precaution for anaphylaxis and spread of protoscolices can be taken timely.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Brown RA, Millar AJ, Steiner Z, Krige JE, Burkimsher D, Cywes S. Hydatid cyst of the pancreas — a case report in a child. Eur J Pediatr Surg. 1995;5:121–3. doi: 10.1055/s-2008-1066184. [DOI] [PubMed] [Google Scholar]
- 2.Ozmen MM, Moran M, Karakahya M, Coskun F. Recurrent acute pancreatitis due to a hydatid cyst of the pancreatic head: A case report and review of the literature. JOP. 2005;6:354–8. [PubMed] [Google Scholar]
- 3.Jai SR, El Hattabi K, Bensardi F, Chehab F, Khaiz D, Bouzidi A. Primary hydatid cyst of the pancreas causing obstructive jaundice. Saudi J Gastroenterol. 2007;13:191–3. doi: 10.4103/1319-3767.36752. [DOI] [PubMed] [Google Scholar]
- 4.Lemmer ER, Krige JE, Price SK, Girdwood AH. Hydatid cyst in the head of the pancreas with obstructive jaundice. J Clin Gastroenterol. 1995;20:136–8. doi: 10.1097/00004836-199503000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Baghbanian M, Shabazkhani B, Ghofrani H, Forutan H, Dariani N, Farahvash M, et al. Efficacy of endoscopic ultrasound guided fine needle aspiration in patients with solid pancreatic neoplasms. Saudi J Gastroenterol. 2012;18:358–63. doi: 10.4103/1319-3767.103426. [DOI] [PMC free article] [PubMed] [Google Scholar]


