Abstract
Introduction:
Tubal blockage is one of the most common causative factors for female barrenness. It accounts for about 25-35% of female infertility. It is very difficult to manage, as the treatment choices for it are only tubal re-constructive surgery and in vitro fertilization (IVF). On the other hand, there is not established any reliable Ayurvedic treatment for the tubal blockage. It is the need of the time to establish an efficient and cost-effective therapy for this problem.
Aim:
To evaluate the efficacy of Yavakshara Taila Uttarabasti in fallopian tubal blockage.
Materials and Methods:
Patients of childbearing age with active marital life of 1 year or more, having complaint of failure to conceive with at least one fallopian tube blockage were selected. Total 19 patients were registered with 42.11% unilateral and 57.89% bilateral tubal blockage. Yavakshara Taila (5 ml) Intrauterine Uttarabasti was given for 6 days (with interval of 3 days in between), after completion of menstrual cycle for two consecutive cycles.
Results:
The tubal patency was found in 68.75% of patients and conception was achieved in 6.25% of patients.
Conclusion:
Yavakshara Taila Uttarabasti an effective procedure for treating tubal blockage with no apparent evidence of complication.
Keywords: Fallopian tube blockage, hysterosalpingography, Uttarabasti, Yavakshara Taila
Introduction
Infertility is the failure to conceive (regardless of cause) after 1 year of unprotected intercourse. It affects approximately 10–15% of reproductive-aged couples.[1] Among responsible factors of female infertility, the tubal blockage is the second highest affecting around 25–35% of population[2] and difficult to treat. The management alternatives for it are only tubal reconstructive surgeries and in vitro fertilization but is available in a very few infertility clinics in developing countries that are not easily accessible. The probability of ectopic pregnancy and other complications are also associated.
The tubal blockage has been considered as Vata predominant Tridoshaja condition, whereas Vata causes Sankocha[3] (constriction), Kapha induces Shopha (swelling), while Pitta causes Paka[4] (inflammation). The drug assumed to be effective in removing the blockage of fallopian tube should possess Tridoshaghna properties mainly Vata-Kapha Shamaka (alleviating Vata-Kapha). Local administration of any drug with Sukshma, Laghu (light), Sara (capable of flowing and permeating through), Vyavayi, Vikasi, Pramathi Guna, Katu Vipaka, and Ushna (hot) Virya can be assumed to have effective role in removing tubal blockage and in restoring the tubal functions by reaching up to the minute channels.
Considering this, Yavakshara Taila was selected in present clinical trial. Yavakshara Taila contents Yavakshara[5] and Tila Taila[6] (sesame oil), which are having similar properties. Yavakshara is considered as Garbhaprada (fertility creating) and effective in Artavanasha (amenorrhea) and is indicated for internal administration.[7] Kshara Taila which is mentioned for Stree Roga Adhikara[8] and Karna Rogadhikara[9] is being practiced for intrauterine tubal blockage in some parts of India.
Considering this, it is planned to evaluate the efficacy of Yavakshara Taila Uttarbasti in tubal blockage.
Materials and Methods
Total 19 patients attending the outpatient department of Stree Roga and Prasooti Tantra, fulfilling the criteria for inclusion were registered irrespective of caste, religion, etc. Informed written consent of the patients was taken before including into the study. The present clinical trial was open labeled single arm study. The study was approved by the Institutional Ethics Committee (No. PGT/7-A/Ethics/2011-12/2087; Dt. 05/09/2011) and registered in Clinical Trial Registry of India (No. CTRI/2013/03/003500).
Diagnostic criteria
Based on hysterosalpingography (HSG) or sonosalpingography (SSG) report with unilateral or bilateral tubal blockage.
Inclusion criteria
Patients of childbearing age (between 19 and 38 years) having complaints of failure to conceive due to tubal blockage were selected on the diagnostic basis of HSG.
Exclusion criteria
Patients with any possibility of active urogenital infections, history of excessive menstruation, suffering from any chronic disease, hepatitis B, sexually transmitted diseases, human immunodeficiency virus (HIV), other contagious diseases etc., were excluded.
Investigations
Serological tests for HIV, hepatitis B surface antigen (Australia antigen for hepatitis B) and Venereal Disease Research Laboratory test were carried out in all the patients before starting the course of treatment
Transvaginal sonography was done before treatment to rule out any pelvic pathology.
Routine hematological and urine investigations were carried out to rule out underlying other pathologies
Treatment protocol
Patients undergoing treatment were given Snehana (oleation) with Bala Taila,[10] followed by Nadi Sveda (fomentation) with water steam on the lower abdomen, back and lower limbs, before administration of Uttarabasti. For sterilization of peri-vaginal part Yoni Prakshalana (vaginal douche)with Panchavalkala Kvatha[11] (decoction) was performed. The procedure was carried out in the operation theater with all aseptic precautions. Patients were made to lie in the lithotomy position, external genital region was cleaned with antiseptic solution, vagina and cervix were visualized with the help of Sim's speculum and anterior vaginal wall retractor. The anterior lip of cervix was held with the help of Allis’ forceps. The uterine sounding was done. The Uttarabasti cannula, already attached with 5 ml syringe filled with Yavakshara Taila was passed in to the uterine cavity after making head low position. The drug was pushed above the level of internal os with constant and gentle force, and then the patient was advised to lie in head low position for 2 h. Thereafter, the lower abdomen was fomented with hot water bag. Uttarabasti of Yavakshara Taila was given in 5 ml dose for 6 days with an interval of 3 days in between,[12] in one cycle (after cessation of menses), for two consecutive cycles.
Precautions
During the course of Uttarabasti, patients were asked to avoid spicy diet and prohibit coitus.
Assessment of complications
Lower abdominal pain and per vaginal bleeding were the most apparent complaints during and after the procedure. It was considered as a complication, only if it is very much disturbing the patient. Any type of features of urogenital infection during and after the procedure were also considered as a complication.
Criteria for assessment
For assessment of therapy, HSG was repeated to check the patency of unilateral or bilateral block after the cessation of menstruation in the third cycle.
Follow-up study
A follow-up study for pregnancy or any late complications was carried out for 2 months after the completion of treatment. Any new complaint appeared during follow-up period related to study was also noted.
Observations and Results
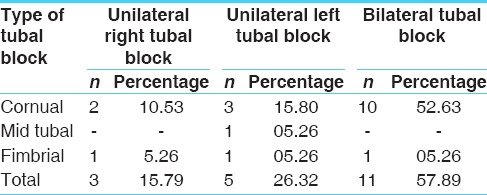
Total 19 patients were registered in the study and 16 could complete the treatment. Three drop outs are due to migration. Unilateral tubal blockage was observed in 42.11% and bilateral in 57.89% of the patients before treatment. In unilateral tubal blockage, 15.79% patients had right tubal block, out of them 10.53% had cornual and 5.26% had fimbrial tubal block; while 26.32% patients had left tubal block, out of them 15.8% had cornual, 5.26% had mid tubal and fimbrial tubal blockage each. In bilateral tubal blockage, 52.63% patients had cornual, and 5.26% patients had mid tubal blockage [Table 1].
Table 1.
Sites of tubal blockage (n=19)
In Prakriti Parikshana, 57.89% patients had Vata-Pitta type, 31.58% had Vata-Kapha type, and 10.53% patients had Kapha-Pitta type of Prakriti. In sexual history, maximum patients (78.95%) reported satisfactory sexual life, 21.05% reported unsatisfactory sex history and 26.32% patients reported associated problems like dyspareunia, etc. A history of pelvic inflammatory disease (PID) was noted in 26.32% of patients. A history of tuberculosis noted in one patient. Other tubal anomalies like hydrosalphinx observed in 2.36% of the patient.
While analyzing the clinical manifestations during and after the procedure of Uttarabasti, pain was reported by 18.75% patients with <1 h duration with tolerating capacity. Per vaginal bleeding (in spotting amount) was reported by 12.5% of patients.
In effect of therapy, out of 16 completed patients tubal patency was observed in 11 patients that is, the tubal block was removed in 68.75% patients. Among 5 patients who could not achieve tubal patency during the study period, two cases were found to have a history of PID, and 3 patients had chronicity of the history with 14 years.
The X-ray of patients with a cornual block before treatment and spillage after treatment are depicted in Figure 1a and b. Other X-rays of the bilateral fimbrial block, right cornual block before treatment and spillage after treatment are depicted in Figures 2 and 3 respectively.
Figure 1.
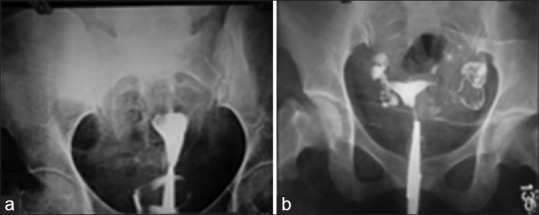
Case 1: Bilateral cornual block (a) before treatment, (b) after treatment
Figure 2.
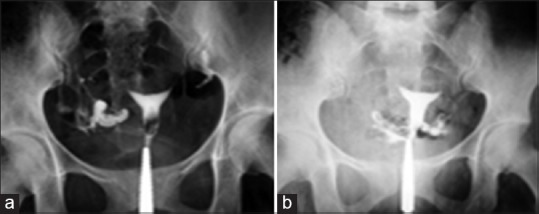
Case 2: Bilateral fimbrial block (a) before treatment, (b) after treatment
Figure 3.
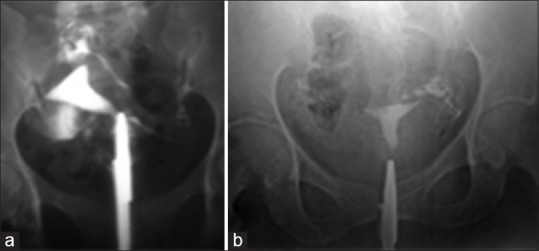
Case 3: Right cornual block (a) before treatment, (b) after treatment
In the follow-up period, conception was achieved in one patient. Anovulation was persisting in 5 patients; irregular uterine cavity in one patient. Male factor was observed in 5 patients in whom tubal block was cleared but no conception occurred within the follow-up period of 2 months.
Discussion
It has been established that in only 40% of the cases of tubal blockage, a previous history of PID has been found, and in 60% of the patients, it has not been possible to elicit the history of PID, although it is the most important etiological factor of tubal blockage.[13] It is supported by the fact that, 26.32% of the patients in this study had a history of PID. A history of tuberculosis which is considered as an important etiological factor of infertility due to tubal block has been found in one patient. It suggests that this disease has become less prevalent in the population than previously.
Not much significant difference was observed in unilateral and bilateral tubal blockage. The incidence of unilateral and bilateral tubal blockage in the present study shows the prevalence of both the conditions high in the society [Table 1]. Yet unilateral blockage is also important to give due consideration, because, it reduces the possibility of conception. Moreover, the condition becomes worse, if another patent tube is abnormal. Much authentic data are not available on the incidence of unilateral and bilateral tubal blockage. Hence, it is difficult to co-relate. The most prevalent site of blockage was cornual [Figures 1a and 3a]. This data supports the established fact that proximal (cornual) tubal block is the most common. Proximal tubal occlusion is mostly due to an inflammatory phenomenon, secondary to an ascending sexually transmitted disease, puerperal infection, or septic abortion. It may also be associated to salpingitis isthmica nodusa, endometriosis, tubal polyposis, or other rare causes of endosalpingitis.[14] Other tubal anomalies observed in the present study with 02.63% hydrosalpinx. Maximum patients had the history of satisfactory sexual life. 21.05% patients had an unsatisfactory sexual life due to certain male factors like erectile dysfunction or premature ejaculation, etc. The complaint of dyspareunia, that is 26.32% of patients is also significant in patients with infertility and tubal blockage. Dyspareunia can be due to vaginal infection or vaginismus. The cases with any types of reproductive tract infections were already excluded from the study. Hence, the cases found with the history of superficial dyspareunia might be due to vaginismus, which is psychological.
Analyzing the clinical manifestations during procedure of Uttarabasti, only 18.75% of the patients complained lower abdominal pain within tolerating capacity, which may be due to contractile response of uterus to remove the blockage from the site of obstruction. It is assumed that obstruction from the blockage site will be removed with the Lekhana property of Ushna-Tikshna drugs and also by the contractile response of uterus. The contractile response was confirmed by the lower abdominal pain, which was a common complaint after the procedure. No patient had excessive or fresh bleeding after this procedure. Slight bleeding reported may be due to the removal of the inner uterine as well as tubal lining by the Ushna-Tikshna and Lekhana properties of the drug. Symptoms of genitourinary infection and oil embolism were not reported during and after the procedure and even in the follow-up period in any patient. It may be due to the potent anti-inflammatory and anti-infective effect of Tila Taila. This proves the intrauterine Uttarabasti as a safe therapeutic measure against tubal blockage. None of the major adverse reaction was observed during or post procedure.
Probable mode of action of intrauterine Uttarabasti on tubal blockage
While analyzing the effect of Uttarabasti on tubal blockage, highly significant results show the potency of the drugs used and also the efficacy of Uttarabasti. It is clear that its action on various disorders is in two ways, local as well as systemic. In case of tubal blockage, this effect seems to be more local than systemic. Tila Taila is Vranashodhaka, Vranapachaka and Krimighna. In addition, its specific action also helps in Garbhashayashodhana and Yonishulaprashamana. These properties indicate towards its antiseptic as well as anti-inflammatory actions. Its Vyavayi and Vikasi Guna show its potency to enter in minute channels and spread easily. Thus the best medium for any drug to reach in tubal cavity and remove the blockage.[6,15,16,17]
Yavakshara[5] had Vata-Kapha Shamaka and Aampachaka action. It also has Gulmanashana and Kaphanissaraka Karma. Further, any of the Kshara is said to be the best for checking the recurrence. It helps in scraping of obstructing substance and also removes the endometrial lining of tubes and uterus. It removes the fibrosed and damaged endometrium and promotes its rejuvenation. Thus, this management not only removes the blockage but also creates an environment conducive for inside the intrauterine implantation.
On evaluation of the cases in which the conception did not occur even after the block was removed; it was found that 9 patients had other potent factors accounting for infertility such as anovulation, irregular uterine cavity, male factor, etc.
Conclusion
The results suggest that Yavakshara Taila Uttarabasti is a safe and efficacious measure in the management of infertility due to tubal blockage. Chances of complications during this procedure are negligible if proper antiseptic and aseptic care is taken before, during and after the procedure. Conception within follow-up period shows high chances of pregnancy if other factors of infertility are managed. Hence, it can be said that Uttarabasti may replace microsurgeries in the management of tubal infertility in near future.
Financial support and sponsorship
IPGT and RA, Gujarat Ayurved University, Jamnagar, Gujarat, India.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Puscheck EE. Lucidi RS, editor. [Last cited on 2013 Mar 02]. Available from: http://www.emedicine.medscape.com/article/274143-overview#aw2aab6b3 .
- 2.Dutta DC. Infertility. In: Konar H, editor. Textbook of Gynaecology. 5th ed. Ch. 16. Delhi: New Central Book Agency; 2009. p. 222. [Google Scholar]
- 3.Sharma H, editor. Reprint ed. Varanasi: Chaukhamba Sanskrit Sansthan; 2009. Kashyapa Samhita of Vriddha Jivaka, Sutrasthana, Ch. 27, Ver. 30.31; p. 42. [Google Scholar]
- 4.Acharya JT, editor. Reprint ed. Varanasi: Chaukhamba Surbharati Prakashana; 2012. Sushruta Samhita of Sushruta, Sutrasthana, Ch.17, Ver. 7; p. 83. [Google Scholar]
- 5.Mishra BS, editor. 11th ed. Varanasi: Chaukhambha Prakashana; 2007. Bhavaprakasha Nighantu of Shree Bhava Mishra, Haritakyadi Varga, Ver.252-255; p. 163. [Google Scholar]
- 6.Mishra BS, editor. 11th ed. Varanasi: Chaukhambha Prakashana; 2007. Bhavaprakasha Nighantu of Shree Bhava Mishra, Taila Varga, Ver.2-7; p. 779. [Google Scholar]
- 7.Mishra SN, editor. Reprint ed. Varanasi: Chaukhamba Orientalia; 2003. Rasamanjari of Acharya Shalinatha, Ch.9, Ver. 52-54. [Google Scholar]
- 8.Shah NC. Bharata Bhaishajya Ratanakara, Part 5th. Ahmedabad: Unjha Ayurveda Pharmacy; 1937. pp. 533–4. [Google Scholar]
- 9.Shastri AD, editor. 1st ed. Varanasi: Chaukhambha Prakashana; 2011. Bhaishajya Ratnavali of Govind Das Sen, Ch.62, Ver. 18-22; p. 976. [Google Scholar]
- 10.Paradakar HS. Reprint ed. Varanasi: Chaukhamba Surbharati Prakashana; 2011. Ashtanga Hridaya of Vagbhata, Chikitsasthana, Ch.21, Ver. 73-81; p. 727. [Google Scholar]
- 11.Tripathi B, editor. Sharangadhara Samhita of Sharangdharacharya, Madhyama Khanda Ch.2, Ver. 149. 6th ed. Varanasi: Chaukhambha Surabharati Prakashana; 2005. p. 155. [Google Scholar]
- 12.Acharya JT, editor. Charaka Samhita of Agnivesha, Siddhisthana, Ch.9, Ver. 69. Reprint ed. Varanasi: Chaukhamba Surbharati Prakashana; 2011. p. 721. [Google Scholar]
- 13.Insler V, Lunenfeld B. Infertility: Male and Female. 2nd ed. Edinburgh: Churchill Livingstone; 1993. p. 253. [Google Scholar]
- 14.Insler V, Lunenfeld B. Infertility: Male and Female. 2nd ed. Edinburgh Churchill Livingstone; 1993. p. 25. [Google Scholar]
- 15.Mishra BS, editor. Bhavaprakasha Nigantu of Shree Bhava Mishra, Dhanya Varga. 11th ed. Ver. 2-7. Varanasi: Chaukhambha Prakashana; 2007. p. 652. [Google Scholar]
- 16.1st ed. New Delhi: Ministry of Health and Family Welfare, Dept. of ISM, and H, Govt. of India (API, 4e); 1999. Anonymous. The Ayurvedic Pharmacopeia of India, Part 1, Vol. IV; pp. 195–96. [Google Scholar]
- 17.Acharya JT, editor. Sushruta Samhita of Sushruta, Sutrasthana. Reprint ed. Ch. 45, Ver. 112. Varanasi: Chaukhamba Surbharati Prakashana; 2012. p. 205. [Google Scholar]


