Abstract
Purpose:
To determine the prevalence and causes of blindness and visual impairment (VI) in Yazd, central Iran.
Methods:
This population-based, cross-sectional study was performed on adults aged 40–80 years, residing in Yazd district, in 2010–2011. Eligible subjects were selected using cluster random sampling. Each participant underwent an interview and complete ophthalmologic examination. Blindness and VI were defined as best-corrected visual acuity (VA) <3/60 and < 6/18 in the better eye, respectively.
Results:
Out of 2,320 eligible individuals, 2,098 participated in the study (90.4% response rate), of whom, 2,023 subjects completed all evaluations. The standardized prevalence of blindness and VI were 0.7% (95% confidence interval [CI], 0.3–1.0%) and 4.4% (95% CI, 3.3–5.4%), respectively which was significantly associated with older age (odd ratio [OR] = 3.2, 95% CI: 1.9–5.2 and OR = 3.1, 95% CI: 2.3–4.2, respectively) and female sex (OR = 3.6, 95% CI: 1.1–12.3 and OR = 1.7, 95% CI: 1.2–2.5, respectively). The proportion of avoidable causes of blindness and VI were 92.9% (95% CI: 80.0-100.0%) and 76.6% (95% CI: 69.2-85.0%), respectively. Major causes of blindness were diabetic retinopathy (50.0%), glaucoma (21.4%) and cataracts (14.3%) whereas main causes of VI were cataracts (41.5%), diabetic retinopathy (17.0%) and age-related macular degeneration (13.8%).
Conclusions:
Diabetic retinopathy, glaucoma, cataract and age-related macular degeneration were the leading causes of blindness and VI in Yazd, most of which are avoidable. Planning for prevention of blindness is highly recommended to decrease the proportion of avoidable blindness.
Keywords: Blindness, Community Health Planning, Iran, Prevalence
INTRODUCTION
Visual impairment (VI) is a major health problem worldwide.[1] According to the World Health Organization (WHO) estimations, 285 million visually impaired people lived in the world in 2010 which included 39 million blind people and 246 million subjects with low vision.[2] Visual problems impose large costs on the society.[3] Nowadays, living standards have been improved in most communities, but the prevalence of avoidable blindness remains significantly high in many countries. Almost 80% of global VI is treatable or preventable.[1] Cataracts and uncorrected refractive errors have been accounted as the leading causes of VI, and the major cause of blindness is cataract.[2]
Data on the prevalence and causes of VI and blindness is required to plan programs for eliminating avoidable blindness and VI. About 90% of the world's visually impaired subjects, live in developing countries.[1,4]
A number of studies have reported the prevalence of VI and blindness in Iran, but no population-based study data is available from central Iran.[5,6,7,8,9] This population-based study was performed in Yazd district to determine the prevalence and causes of VI and blindness in the central region of Iran.
METHODS
This population-based cross-sectional study was conducted in 2010–2011 on adults aged 40–80 years in both urban and rural area of Yazd district. Yazd is located in central Iran and has an estimated population of 526,000 people according to the 2006 national census. The study adhered to the Declaration of Helsinki and was approved by the Ethics Committee at Shahid Beheshti University of Medical Sciences. All eligible subjects signed an informed consent.
The study protocol has been reported in detail previously.[10] In brief, a final sample of 2,023 individuals who belonged to 58 clusters each, containing 40 subjects were selected applying multistage systematic cluster sampling method and with probability proportional to size strategy.
Three trained health teams performed subject recruitment by house-to-house visits. Demographic information was collected using a questionnaire, including age, sex, level of education, past ocular and medical history. Individuals were invited to an equipped eye clinic within a week.
Ophthalmic Examination
At the eye clinic, participants underwent a comprehensive eye evaluation. After visual acuity (VA) measurement and refraction, an expert ophthalmologist performed ocular examination including intraocular pressure measurement, gonioscopy, anterior segment examination and anterior chamber depth assessment. The lens and optic disc were examined after dilating the pupil.
A trained optometrist performed stereoscopic fundus photography following pupil dilation in all participants and after laser peripheral iridotomy in subjects with an occludable angle. Visual fields of all participants were tested before dilation.
Visual Acuity Testing
Visual acuity was determined using an NIDEK chart projector (CPe670, 20/10–20/400; Nidek Co., Gamagori, Japan) with tumbling E letters at 4 m distance by an experienced optometrist. An Individual, who could not read the largest E letters on the chart was tested for counting fingers, hand motion and light perception. Uncorrected VA and best-corrected VA were evaluated separately for each eye. Refraction was performed using a Topcon KR 8000 automated refractometer (Topcon Co., Tokyo, Japan). If autorefraction was not possible, objective retinoscopy and subjective refraction would be tried.
Definitions
Blindness was defined as VA <3/60 (20/400, 1.3 LogMar) with best correction in the better eye, and low vision was defined as VA <6/18 (20/60, 0.5 LogMar) but equal to or better than 3/60 (20/400, 1.3). VI (included blindness and low vision) was defined as best-corrected VA <6/18 (20/60, 0.5 LogMar) in the better eye. Moderate visual impairment (MVI) and severe visual impairment (SVI) were classified as best-corrected VA <6/18–6/60 and VA <6/60–3/60, respectively.[11]
Cataract density was scored using the grading system of the Age-Related Eye Disease Study.[12] Glaucoma was diagnosed using the International Society of Geographical and Epidemiological Ophthalmology classification.[13] Diabetic Retinopathy was assessed by masked grading of stereoscopic fundus photographs using the Early Treatment Diabetic Retinopathy Study definitions[14] and Severity of Diabetic Retinopathy was classified according to the International Clinical Diabetic Retinopathy Disease Severity Scale.[15] Age-related macular degeneration (ARMD) was evaluated based on the International ARMD Epidemiological Study Group.[16] All clinical and paraclinical data were evaluated separately and construed by the study team based on the above definitions and archived in a computer database at the Ophthalmic Research Center.
The principle cause of VI or blindness was determined by a reading group which consisted of three retinal and three glaucoma subspecialists with acceptable inter- and intra-reliabilities (based on a Kappa test) according to clinical history and examination of the better eye.[17]
If VA improved to 20/60 or better with optical correction, refractive error was considered as the main cause of blindness or VI. In case there was more than one cause for VI and blindness, the most treatable or preventable one was assessed as the main cause of VI and blindness.
Statistical Analysis
Statistical analysis was performed using STATA software version 12.0 (State Corp LP, College Station, TX, USA). The prevalence of VI and blindness was calculated and standardized for age and sex in Yazd based on the 2006 national census. Multiple multinomial logistic regression models were applied to investigate the association between VI and blindness with age, sex, area of residence and education. In analyses, we regarded the cluster effect of sampling for calculating 95% confidence intervals (95% CIs) by multilevel models. In this analysis, we considered two levels (for subject results) and three levels (for eye results). P value less than 0.05 were considered as statistically significant.
RESULTS
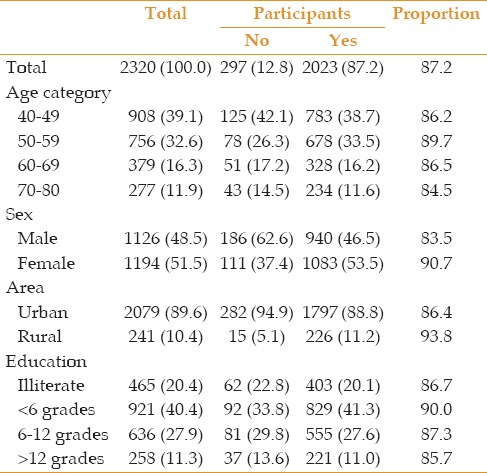
Among 2,320 eligible people, 2,098 subjects participated in the study (response rate, 90.4%) and VA data was available for 2,023 (87.2%) individuals. Mean age in the study population was 59.8 ± 6.8 years consisting of 55.5% (1,083) female subjects. Table 1 demonstrates demographics of the study population.
Table 1.
Demographic data of study population and participants in the Yazd Eye Study
The prevalence of blindness and VI were 0.7% (95% CI, 0.3–1.0%) and 4.9% (95% CI, 3.3–5.4%), respectively. These values were higher in female subjects. Table 2 shows the prevalence of VI, blindness and low vision in Yazd district population. Figure 1 displays the cumulative age and sex stratified distribution of blindness, MVI and SVI, suggesting that the severity of visual abnormalities was greater in older individuals and women. VI was more prevalent in older subjects and increased with each decade of older age (odd ratio [OR] =3.1, 95% CI: 2.3–4.2%, P < 0.0001) and was also associated with female gender (OR = 1.7, 95% CI: 1.2–2.5, P = 0.008). Similarly, blindness was associated with each decade of older age (OR = 3.2, 95% CI: 1.9–5.2%, P < 0.0001) and female gender (OR = 3.6, 95% CI: 1.1–12.3%, =0.041). Area of residence or education was not significantly associated with VI and blindness. However, low vision was more prevalent among rural residents (OR = 2.3, 95% CI: 1.2–4.2%, P = 0.009) [Table 3].
Table 2.
Prevalence of VI, blindness and low vision based on best corrected visual acuity
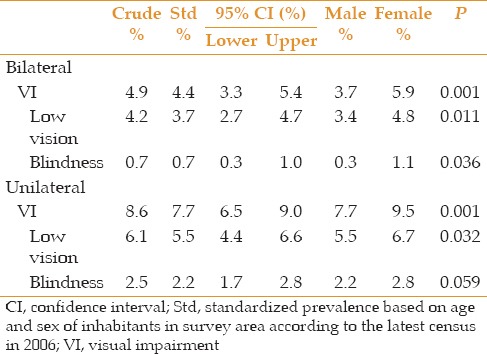
Figure 1.
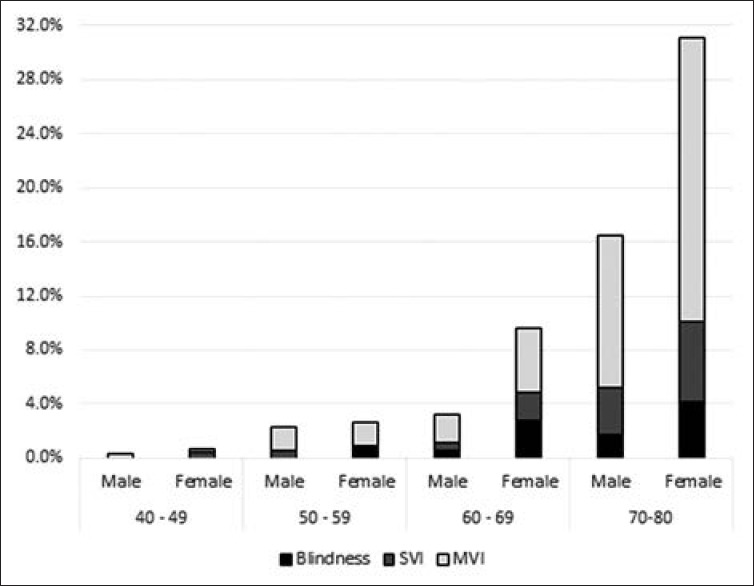
Cumulative age and sex distribution for moderate visual impairment (MVI), severe visual impairment (SVI) and blindness in Yazd Eye Study. Blindness = visual acuity <3/60, MVI = visual acuity <6/18 - 6/60; SVI = visual acuity < 6/60 - 3/60.
Table 3.
Distribution and comparison of VI, blindness and low vision by age, sex, area and education in the Yazd Eye Study
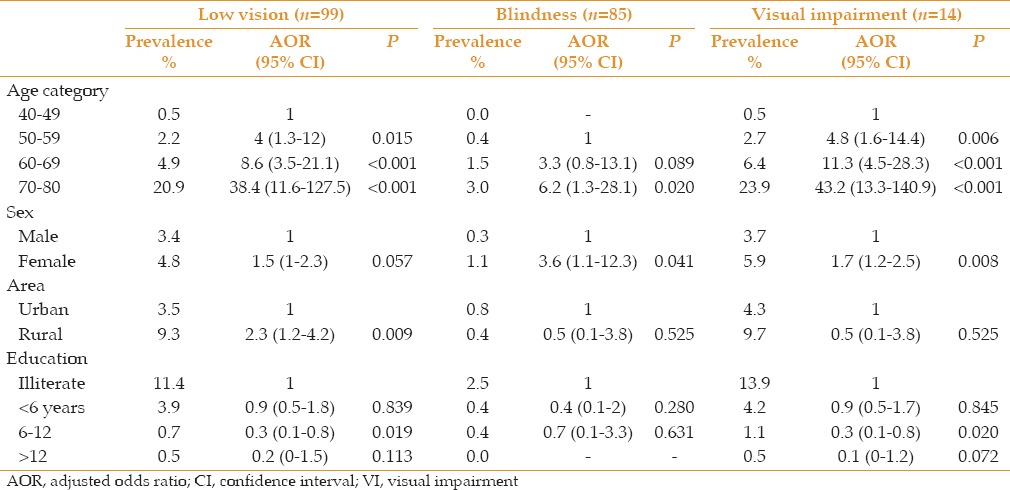
Table 4 presents major causes of blindness and VI. Based on best-corrected visual acuity (BCVA), the leading causes of blindness were diabetic retinopathy (50%) followed by glaucoma (21.4%) and cataracts (14.3%). Major causes of VI were cataracts (41.5%), diabetic retinopathy (17%) and age-related macular degeneration (ARMD, 13.8%). Most causes of blindness and VI were avoidable; 92.9% (95% CI: 80–100%) and 76.6% (95% CI: 69.2–85%), respectively [Figure 2]. Causes of blindness were curable and preventable in 14.3% (95% CI: 0–33.4%) and 78.6% (95% CI: 56.7–100%) of cases, while causes of VI were curable or preventable in 44.7% (95% CI: 34.8–53.8%) and 31.9% (95% CI: 22.7–43%) of cases, respectively.
Table 4.
Main causes of bilateral blindness and VI based on best corrected VA in the Yazd Eye Study
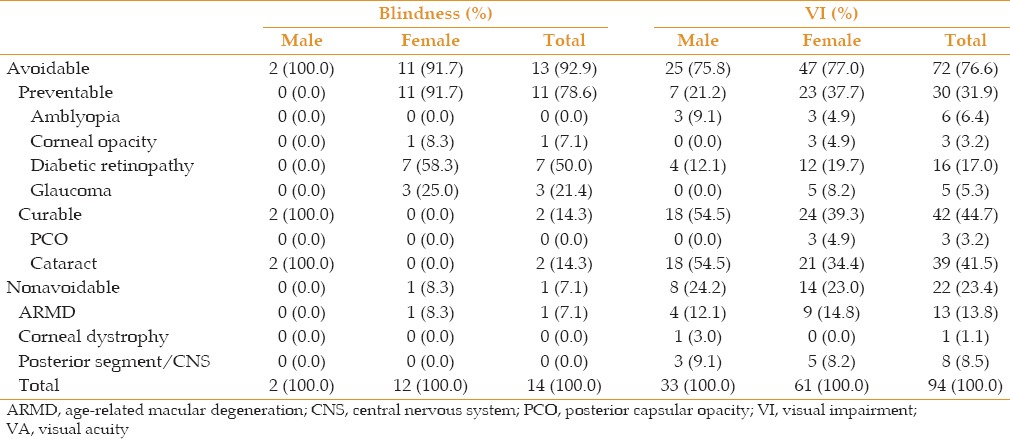
Figure 2.
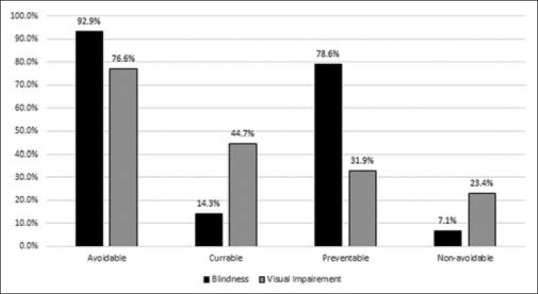
Distribution of avoidable and non-avoidable causes of blindness and visual impairment in the Yazd Eye Study.
DISCUSSION
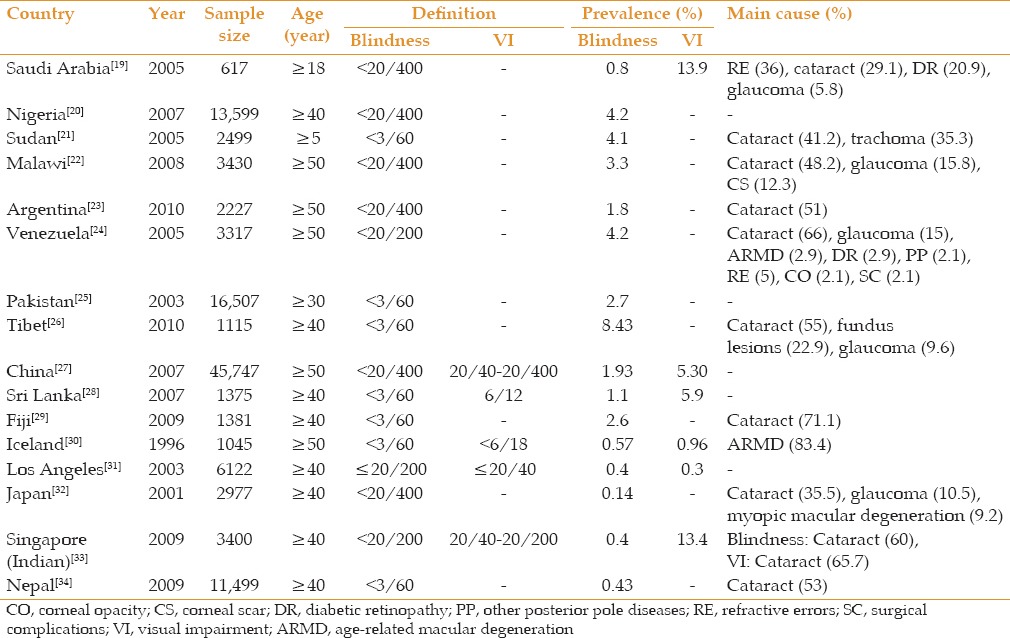
The present study highlighted cataracts, diabetic retinopathy and ARMD as the leading causes of VI in Yazd district. The current study is the first survey on the prevalence and causes of VI in the central region of Iran. The standardized prevalence of blindness and VI among adults aged 40 to 80 years was 0.7% and 4.4%, respectively. These figures are comparable to those from Eastern Mediterranean countries.[18] The prevalence of blindness in our study was close to that reported from Saudi Arabia[19] and relatively lower than Africa (Nigeria,[20] Sudan,[21] Malawi)[22] Latin America (1.1% in Argentina to 4.2% in Venezuela)[23,24], Middle East region (Pakistan),[25] some Asian countries (Tibet,[26] China,[27] Sri Lanka[28]) and the Western Pacific region (Fiji).[29] In comparison with the current study, studies conducted in Iceland,[30] Los Angeles,[31] Japan[32] and the Indian population of Singapore[33] revealed lower rates of blindness and VI [Table 5].
Table 5.
Prevalence of blindness, visual impairment and their causes in some population based studies
Previous Iranian studies from Varamin (≥50 years, 1.33%),[5] Khuzestan (>5 years, 1.3%)[9] and Zahedan (≥10 years, 0.79%)[8] have reported higher rates of blindness and VI, whereas Tehran (0.28%)[6] and Shahroud (0.3%)[7] studies demonstrated lower rates. Although the overall rate of blindness seems lower in Tehran, this rate was much higher (2.8%) in people aged >60 years. Tehran Eye Study evaluated all age groups, and the Shahroud study invited subjects aged 40–64 years whereas in our study individuals 40 to 80 years of age were included. Moreover, the study populations of Tehran and Shahroud studies were urban residents of the cities, while the population of Yazd Eye Study belonged to both urban and rural areas.
The prevalence of blindness and VI were significantly associated with older age and female gender in the current study. The majority of diseases leading to blindness and VI occur in older subjects. The longer life expectancy of female subjects together with less access to healthcare as compared to male individuals may increase the probability of being visually impaired or blind in women. This finding was supported by several studies.[7,8,20,25,27] However, some studies showed this association only in older subjects.[9,29,33,35,36,37] There are also exceptions. Rapid assessment of avoidable blindness findings from Malawi demonstrated a higher prevalence of blindness in men as compared to women.[22] This trend was explained by poor outcomes after ocular surgery in that region, because in Malawi, men had more access to cataract surgery than women. The higher prevalence of low vision in rural areas probably indicates that rural residents have improper access to eye care services and/or less knowledge about eye health. This finding was in agreement with the Pakistan eye study.[25] On the other hand, some other studies reported that rural/urban domicile is not a risk factor for blindness, VI or low vision.[9,20,29]
Refractive errors have been accounted as a primary cause of VI and blindness in recent studies based on presenting VA.[5,6,9,19,36,38] Another report from the current study database has reported prevalence of refractive errors in Yazd district.[39] Based on uncorrected visual acuity, refractive errors were the main cause of VI and blindness in our study (85% and 47%, respectively).
In contrast to other studies from other regions of Iran and most developing countries, diabetic retinopathy was the main cause of blindness in the present study. Although our analysis was done based on BCVA and we therefore bypassed refractive errors as the main cause of blindness, we did not expect diabetic retinopathy to be a major cause of blindness in Yazd; however, this finding is probably due to the large number of diabetic patients in the region. Screening programs and public education should be seriously performed to prevent and monitor diabetes mellitus in Yazd.
Glaucoma is the second cause of blindness worldwide[2] and some developed countries, such as Japan and Germany, have reported glaucoma as the second cause of VI.[35,40] It has been estimated that half of the world's population with glaucoma reside in Asia.[41] A previous report from this population based survey demonstrated that 4.4% of Yazd population were affected with glaucoma.[17] According to the present paper, glaucoma was recognized as the second leading cause of blindness. Since glaucoma leads to irreversible blindness, early diagnosis of the disease is essential to prevent vision loss.
Several studies in Africa, Asia and Latin America have reported cataracts as the principal cause of blindness and VI.[5,6,7,8,9,21,23,26,33,36,37] Cataracts account for half of the blindness despite the fact that the condition is curable.[2,18] Cataracts were the third leading cause of blindness in our study. The large number of patients with diabetic retinopathy in Yazd district most likely led to underrepresentation of cataracts as a major cause of blindness. Improving disease awareness through regular check-ups and enhancing the cataract surgery coverage will avoid related blindness.
In Western populations, age-related macular degeneration has been the main cause of blindness and VI in white people,[21,30] whereas cataracts, diabetic retinopathy and glaucoma are major causes in black people.[21] In the current study, ARMD was the third cause of VI.
Trachoma was not a leading cause of visual disability in the current study, however it was recognized as the second cause of blindness in Eastern Mediterranean countries.[18] In some African countries, trachoma has been almost as common as cataracts and considered as the leading cause of blindness and VI.[21] According to previous studies in Iran, VI and blindness are no longer attributed to corneal disorders.[5,6,7,9]
In the current study, we employed BCVA to define blindness and VI, thus the role of refractive errors as a prevalent avoidable cause of VI could not be estimated. Nevertheless, the proportion of avoidable causes of blindness and VI were 92.9% (95% CI: 80–100%) and 76.6% (95% CI: 69.2–85%), respectively. The large proportion of preventable causes of blindness (78.6%; 95% CI: 56.7–100%) in this study, suggests that educational programs may increase community awareness and accordingly encourage proper behaviors for prevention of blindness. Furthermore, 44.7% (95% CI: 34.8–53.8%) of VI causes were curable. Among treatable causes, cataracts had the greatest share in VI.
The limitation of our study was not considering presenting VA in defining blindness and VI. On the other hand, the high response rate (90.4%), including participants from both urban and rural areas, and applying fundus images are advantages of this study.
In summary, the overall prevalence of blindness and VI was 0.7% and 4.4%, respectively in Yazd district. Major causes of blindness were diabetic retinopathy, glaucoma and cataracts. The main causes of VI were cataracts followed by diabetic retinopathy and ARMD. Educational and screening programs for early detection, follow-up and management of diabetic retinopathy, glaucoma and cataract at the community level are required to eliminate blindness in central Iran. In addition, since the proportion of blindness and irreversible low vision was considerable, it may be recommended that low vision and rehabilitation services be assessed in this district and in case of inadequacy, get improved.
Financial Support and Sponsorship
Research and Technology Department of the Ministry of Health.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Shahid Sadoughi University of Medical Sciences in Yazd for organizing the logistics of the survey and would like to thank Dr. Mehdi Tavakoli for his insightful comments.
REFERENCES
- 1.Geneva, Switzerland: Wold Health Organization; 2009-2013. Wrold Health Organization. Action Plan for the Prevention of Avoidable Blindness and Visual Impairment. [Google Scholar]
- 2.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–618. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 3.Holden BA. Blindness and poverty: A tragic combination. Clin Exp Optom. 2007;90:401–403. doi: 10.1111/j.1444-0938.2007.00217.x. [DOI] [PubMed] [Google Scholar]
- 4.Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–851. [PMC free article] [PubMed] [Google Scholar]
- 5.Rajavi Z, Katibeh M, Ziaei H, Fardesmaeilpour N, Sehat M, Ahmadieh H, et al. Rapid assessment of avoidable blindness in Iran. Ophthalmology. 2011;118:1812–1818. doi: 10.1016/j.ophtha.2011.01.049. [DOI] [PubMed] [Google Scholar]
- 6.Fotouhi A, Hashemi H, Mohammad K, Jalali KH. Tehran Eye Study. The prevalence and causes of visual impairment in Tehran: the Tehran Eye Study. Br J Ophthalmol. 2004;88:740–745. doi: 10.1136/bjo.2003.031153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hashemi H, Khabazkhoob M, Emamian MH, Shariati M, Fotouhi A. Visual impairment in the 40- to 64-year-old population of Shahroud, Iran. Eye (Lond) 2012;26:1071–1077. doi: 10.1038/eye.2012.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shahriari HA, Izadi S, Rouhani MR, Ghasemzadeh F, Maleki AR. Prevalence and causes of visual impairment and blindness in Sistan-va-Baluchestan Province, Iran: Zahedan Eye Study. Br J Ophthalmol. 2007;91:579–584. doi: 10.1136/bjo.2006.105734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feghhi M, Khataminia G, Ziaei H, Latifi M. Prevalence and causes of blindness and low vision in khuzestan province, Iran. J Ophthalmic Vis Res. 2009;4:29–34. [PMC free article] [PubMed] [Google Scholar]
- 10.Katibeh M, Ziaei H, Pakravan M, Dehghan MH, Ramezani A, Amini H, et al. The Yazd Eye Study-A population-based survey of adults aged 40-80 years: Rationale, study design and baseline population data. Ophthalmic Epidemiol. 2013;20:61–69. doi: 10.3109/09286586.2012.744844. [DOI] [PubMed] [Google Scholar]
- 11.10th Revision. Geneva: WHO; 1993. World Health Organization. International Statistical Classification of Diseases, Injuries and Causes of Death. [Google Scholar]
- 12.Sperduto RD, Clemons TE, Lindblad AS, Ferris FL, 3rd Age-Related Eye Disease Study Research Group. Cataract classification using serial examinations in the age-related eye disease study: Age-related eye disease study report no 24. Am J Ophthalmol. 2008;145:504–508. doi: 10.1016/j.ajo.2007.10.024. [DOI] [PubMed] [Google Scholar]
- 13.Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–242. doi: 10.1136/bjo.86.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grading diabetic retinopathy from stereoscopic color fundus photographs – An extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:786–806. [PubMed] [Google Scholar]
- 15.Wilkinson CP, Ferris FL, 3rd, Klein RE, Lee PP, Agardh CD, Davis M, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110:1677–1682. doi: 10.1016/S0161-6420(03)00475-5. [DOI] [PubMed] [Google Scholar]
- 16.Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv Ophthalmol. 1995;39:367–374. doi: 10.1016/s0039-6257(05)80092-x. [DOI] [PubMed] [Google Scholar]
- 17.Pakravan M, Yazdani S, Javadi MA, Amini H, Behroozi Z, Ziaei H, et al. A population-based survey of the prevalence and types of glaucoma in central Iran: The Yazd eye study. Ophthalmology. 2013;120:1977–1984. doi: 10.1016/j.ophtha.2013.02.029. [DOI] [PubMed] [Google Scholar]
- 18.Tabbara KF. Blindness in the eastern Mediterranean countries. Br J Ophthalmol. 2001;85:771–775. doi: 10.1136/bjo.85.7.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Shaaln FF, Bakrman MA, Ibrahim AM, Aljoudi AS. Prevalence and causes of visual impairment among Saudi adults attending primary health care centers in northern Saudi Arabia. Ann Saudi Med. 2011;31:473–480. doi: 10.4103/0256-4947.84624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kyari F, Gudlavalleti MV, Sivsubramaniam S, Gilbert CE, Abdull MM, Entekume G, et al. Prevalence of blindness and visual impairment in Nigeria: The National Blindness and Visual Impairment Study. Invest Ophthalmol Vis Sci. 2009;50:2033–2039. doi: 10.1167/iovs.08-3133. [DOI] [PubMed] [Google Scholar]
- 21.Ngondi J, Ole-Sempele F, Onsarigo A, Matende I, Baba S, Reacher M, et al. Prevalence and causes of blindness and low vision in southern Sudan. PLoS Med. 2006;3:e477. doi: 10.1371/journal.pmed.0030477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalua K, Lindfield R, Mtupanyama M, Mtumodzi D, Msiska V. Findings from a rapid assessment of avoidable blindness (RAAB) in Southern Malawi. PLoS One. 2011;6:e19226. doi: 10.1371/journal.pone.0019226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Furtado JM, Lansingh VC, Carter MJ, Milanese MF, Peña BN, Ghersi HA, et al. Causes of blindness and visual impairment in Latin America. Surv Ophthalmol. 2012;57:149–177. doi: 10.1016/j.survophthal.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 24.Salomao SR, Cinoto RW, Berezovsky A, Araujo-Filho A, Mitsuhiro MR, Mendieta L, et al. Prevalence and causes of vision impairment and blindness in older adults in Brazil: The Sao Paulo Eye Study. Ophthalmic Epidemiol. 2008;15:167–175. doi: 10.1080/09286580701843812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jadoon MZ, Dineen B, Bourne RR, Shah SP, Khan MA, Johnson GJ, et al. Prevalence of blindness and visual impairment in Pakistan: The Pakistan National Blindness and Visual Impairment Survey. Invest Ophthalmol Vis Sci. 2006;47:4749–4755. doi: 10.1167/iovs.06-0374. [DOI] [PubMed] [Google Scholar]
- 26.Wang GQ, Bai ZX, Shi J, Luo S, Chang HF, Sai XY. Prevalence and risk factors for eye diseases, blindness, and low vision in Lhasa, Tibet. Int J Ophthalmol. 2013;6:237–241. doi: 10.3980/j.issn.2222-3959.2013.02.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhao J, Ellwein LB, Cui H, Ge J, Guan H, Lv J, et al. Prevalence of vision impairment in older adults in rural China: The China nine-province survey. Ophthalmology. 2010;117:409–416. doi: 10.1016/j.ophtha.2009.11.023. 416.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Edussuriya K, Sennanayake S, Senaratne T, Marshall D, Sullivan T, Selva D, et al. The prevalence and causes of visual impairment in central Sri Lanka the Kandy Eye study. Ophthalmology. 2009;116:52–56. doi: 10.1016/j.ophtha.2008.08.034. [DOI] [PubMed] [Google Scholar]
- 29.Ramke J, Brian G, Maher L, Qalo Qoqonokana M, Szetu J. Prevalence and causes of blindness and low vision among adults in Fiji. Clin Experiment Ophthalmol. 2012;40:490–496. doi: 10.1111/j.1442-9071.2011.02749.x. [DOI] [PubMed] [Google Scholar]
- 30.Gunnlaugsdottir E, Arnarsson A, Jonasson F. Prevalence and causes of visual impairment and blindness in Icelanders aged 50 years and older: The Reykjavik Eye Study. Acta Ophthalmol. 2008;86:778–785. doi: 10.1111/j.1755-3768.2008.01191.x. [DOI] [PubMed] [Google Scholar]
- 31.Varma R, Ying-Lai M, Klein R, Azen SP Los Angeles Latino Eye Study Group. Prevalence and risk indicators of visual impairment and blindness in Latinos: The Los Angeles Latino Eye Study. Ophthalmology. 2004;111:1132–1140. doi: 10.1016/j.ophtha.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 32.Iwase A, Araie M, Tomidokoro A, Yamamoto T, Shimizu H, Kitazawa Y, et al. Prevalence and causes of low vision and blindness in a Japanese adult population: The Tajimi Study. Ophthalmology. 2006;113:1354–1362. doi: 10.1016/j.ophtha.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 33.Zheng Y, Lavanya R, Wu R, Wong WL, Wang JJ, Mitchell P, et al. Prevalence and causes of visual impairment and blindness in an urban Indian population: The Singapore Indian Eye Study. Ophthalmology. 2011;118:1798–1804. doi: 10.1016/j.ophtha.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 34.Thapa SS, Berg RV, Khanal S, Paudyal I, Pandey P, Maharjan N, et al. Prevalence of visual impairment, cataract surgery and awareness of cataract and glaucoma in Bhaktapur district of Nepal: The Bhaktapur Glaucoma Study. BMC Ophthalmol. 2011;11:2. doi: 10.1186/1471-2415-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nakamura Y, Tomidokoro A, Sawaguchi S, Sakai H, Iwase A, Araie M. Prevalence and causes of low vision and blindness in a rural Southwest Island of Japan: The Kumejima study. Ophthalmology. 2010;117:2315–2321. doi: 10.1016/j.ophtha.2010.03.043. [DOI] [PubMed] [Google Scholar]
- 36.Budenz DL, Bandi JR, Barton K, Nolan W, Herndon L, Whiteside-de Vos J, et al. Blindness and visual impairment in an urban West African population: The Tema Eye Survey. Ophthalmology. 2012;119:1744–1753. doi: 10.1016/j.ophtha.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li J, Zhong H, Cai N, Luo T, Li J, Su X, et al. The prevalence and causes of visual impairment in an elderly Chinese Bai ethnic rural population: The Yunnan minority eye study. Invest Ophthalmol Vis Sci. 2012;53:4498–4504. doi: 10.1167/iovs.12-9429. [DOI] [PubMed] [Google Scholar]
- 38.You QS, Xu L, Yang H, Wang YX, Jonas JB. Five-year incidence of visual impairment and blindness in adult Chinese the Beijing Eye Study. Ophthalmology. 2011;118:1069–1075. doi: 10.1016/j.ophtha.2010.09.032. [DOI] [PubMed] [Google Scholar]
- 39.Ziaei H, Katibeh M, Solaimanizad R, Hosseini S, Gilasi HR, Golbafian F, et al. Prevalence of refractive errors; the yazd eye study. J Ophthalmic Vis Res. 2013;8:227–236. [PMC free article] [PubMed] [Google Scholar]
- 40.Finger RP, Fimmers R, Holz FG, Scholl HP. Prevalence and causes of registered blindness in the largest federal state of Germany. Br J Ophthalmol. 2011;95:1061–1067. doi: 10.1136/bjo.2010.194712. [DOI] [PubMed] [Google Scholar]
- 41.Wong TY, Loon SC, Saw SM. The epidemiology of age related eye diseases in Asia. Br J Ophthalmol. 2006;90:506–511. doi: 10.1136/bjo.2005.083733. [DOI] [PMC free article] [PubMed] [Google Scholar]


